Copyright
©2014 Baishideng Publishing Group Inc.
World J Hepatol. Aug 27, 2014; 6(8): 580-595
Published online Aug 27, 2014. doi: 10.4254/wjh.v6.i8.580
Published online Aug 27, 2014. doi: 10.4254/wjh.v6.i8.580
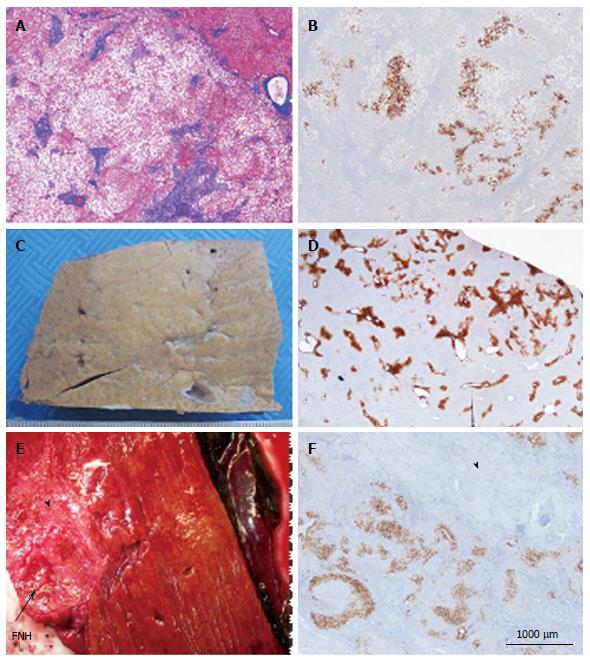
Figure 4 Other aspects (steatotic, pre-focal nodular hyperplasia, regressing focal nodular hyperplasia).
A, B: Woman born in 1959; heavy alcohol consumption, tobacco; hepatomegaly, no evidence for cirrhosis on liver function tests, virus negative. Computed tomography scan: nodule 3.5 cm and others (1.5, 0.3 and 0.8 cm). No firm radiological diagnosis: ?focal nodular hyperplasia (FNH)/hepatocellular adenoma (HCA)/HCC, left hepatectomy in 2001. A: Masson’s trichrome - the nodule is composed of benign steatotic hepatocytes separated by fibrous bands. Steatosis is not a rare event in FNH. B: Glutamine synthase (GS) immunostaining - anastomosed GS positive areas, favoring the diagnosis of steatotic FNH. The diagnosis of FNH remains doubtful, however. In this case, the diagnoses of HNF1A mutated HCA, inflammatory HCA, β-HCA and β-IHCA were ruled out (specific IHC markers were negative). The diagnosis of unclassified HCA cannot, however, be ruled out. Molecular analysis is necessary to confirm the diagnosis. C, D: Woman born in 1950; abdominal pain: gallbladder lithiasis; Magnetic resonance imaging (MRI): 2.5 cm nodule, probably an HCA. Left hepatectomy plus cholecystectomy in 2000. C: Fixed specimen - subcapsular, not well defined nodule barely visible, clearer than the surrounding liver. D: GS immunostaining - the positive perivenular areas are slightly but significantly larger than in the surrounding normal liver; this aspect is interpreted as a “pre-FNH” without fibrosis and nodulation. Pre FNH is probably not a rare entity but to-day there is no consensus concerning its denomination[9]. This type of lesion has been named in congenital vascular abnormalities such as Rendu-Osler disease. E, F: Woman born in 1948; intrahepatic hemorrhagic rupture of a large nodule of segment VII in 2009. MRI favors HCC, additional 4 nodules known since 2005 and interpreted as FNH. Size of the FNH nodule resected with the HCC has decreased significantly. Right hepatectomy (HCC + 1 additional not identified nodule, previously known as FNH). E: Fresh specimen: close to the hemorrhagic HCC, a 4 cm hard white/brown nodule, under the capsule (arrow), with irregular surface. F: GS immunostaining: limited positive areas (map-like pattern) surrounded by large areas of dense fibrous tissue (arrowhead). All these features are interpreted as a regressing FNH. This interpretation needs to be confirmed by additional cases.
- Citation: Sempoux C, Balabaud C, Bioulac-Sage P. Pictures of focal nodular hyperplasia and hepatocellular adenomas. World J Hepatol 2014; 6(8): 580-595
- URL: https://www.wjgnet.com/1948-5182/full/v6/i8/580.htm
- DOI: https://dx.doi.org/10.4254/wjh.v6.i8.580