Copyright
©The Author(s) 2021.
World J Hepatol. Jan 27, 2022; 14(1): 80-97
Published online Jan 27, 2022. doi: 10.4254/wjh.v14.i1.80
Published online Jan 27, 2022. doi: 10.4254/wjh.v14.i1.80
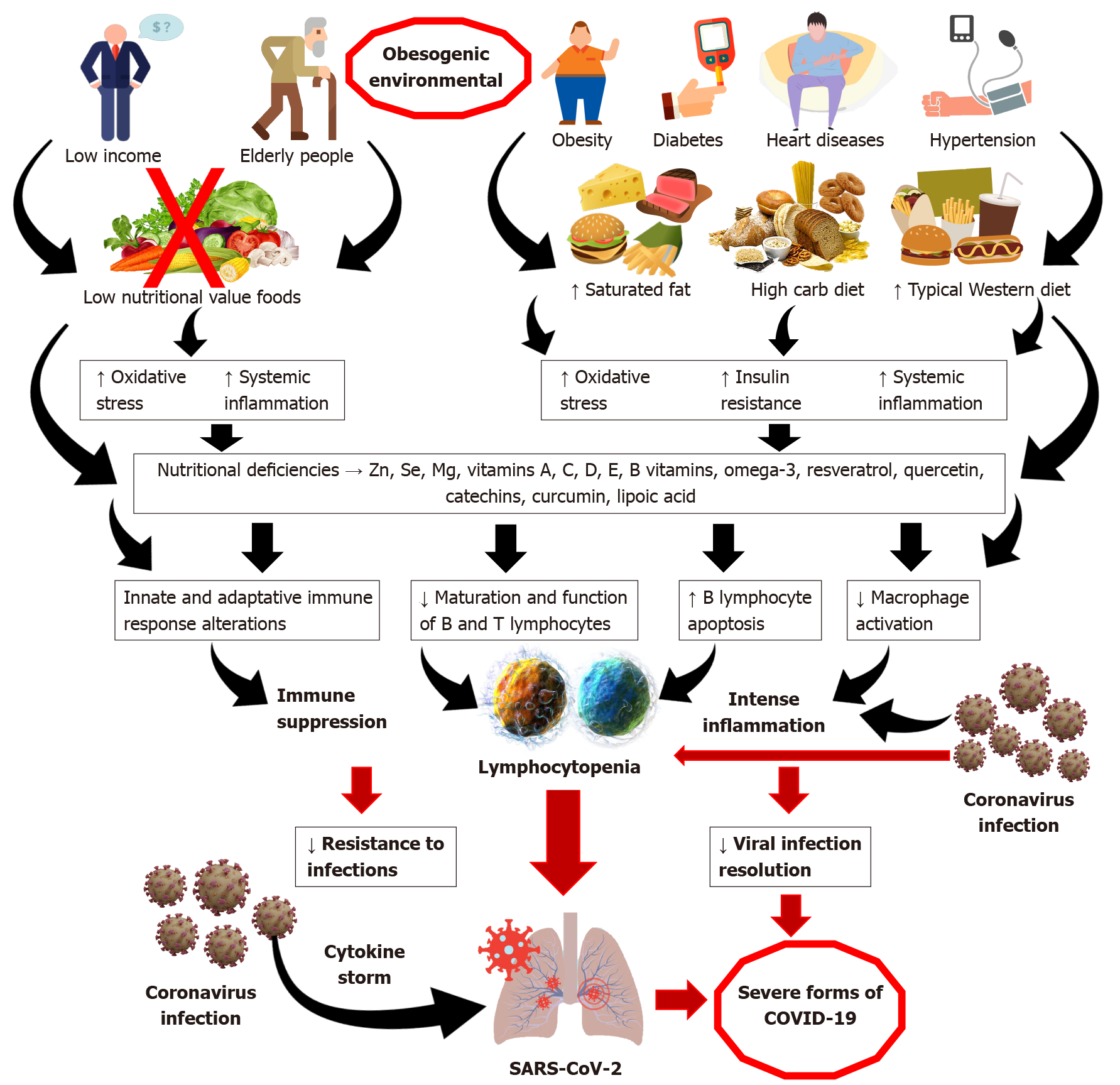
Figure 1 Health, diet and lifestyle practices associated with clinical outcomes in SARS-CoV-2 infection.
Individuals suffering with systemic inflammatory background associated with overweight, obesity, diabetes, heart disease and hypertension, and chronic liver disease, as well as elderly individuals, are more susceptible to develop the most severe forms of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. Chronic consumption of typical westernised diets (WD) diets, which are rich in saturated fat, carbohydrates with high glycaemic index, and low in fresh fruits and vegetables, is relatively common amongst individuals who present worsened clinical outcomes. A typical WD dietary pattern features low nutritional value, facilitating deficiencies of vitamins, minerals, polyunsaturated fatty acids and bioactive compounds such as resveratrol, quercetin, catechins, curcumin and lipoic acid, amongst others. Nutritional deficit can facilitate the exacerbation of oxidative stress, inflammation and insulin resistance, with consequent disturbances in the innate and adaptive immune response, resulting in suppression of the immune response and greater susceptibility to infections. Coronavirus infection is usually associated with a “cytokine storm”, intense inflammation, leukopenia and lymphocytopenia. Individuals with preestablished pro-inflammatory background and impaired immune system due to poor diet are at greater risk of evolving more rapidly to the more severe forms of SARS-CoV-2 infection[12,37,81]. SARS-CoV-2: Severe acute respiratory syndrome coronavirus 2; COVID-19: Coronavirus disease 2019.
- Citation: de Jesus RP, de Carvalho JF, de Oliveira LPM, Cunha CM, Alves TCHS, Vieira STB, Figueiredo VM, Bueno AA. Metabolic and nutritional triggers associated with increased risk of liver complications in SARS-CoV-2. World J Hepatol 2022; 14(1): 80-97
- URL: https://www.wjgnet.com/1948-5182/full/v14/i1/80.htm
- DOI: https://dx.doi.org/10.4254/wjh.v14.i1.80