Copyright
©2012 Baishideng Publishing Group Co.
World J Gastroenterol. Nov 14, 2012; 18(42): 6005-6017
Published online Nov 14, 2012. doi: 10.3748/wjg.v18.i42.6005
Published online Nov 14, 2012. doi: 10.3748/wjg.v18.i42.6005
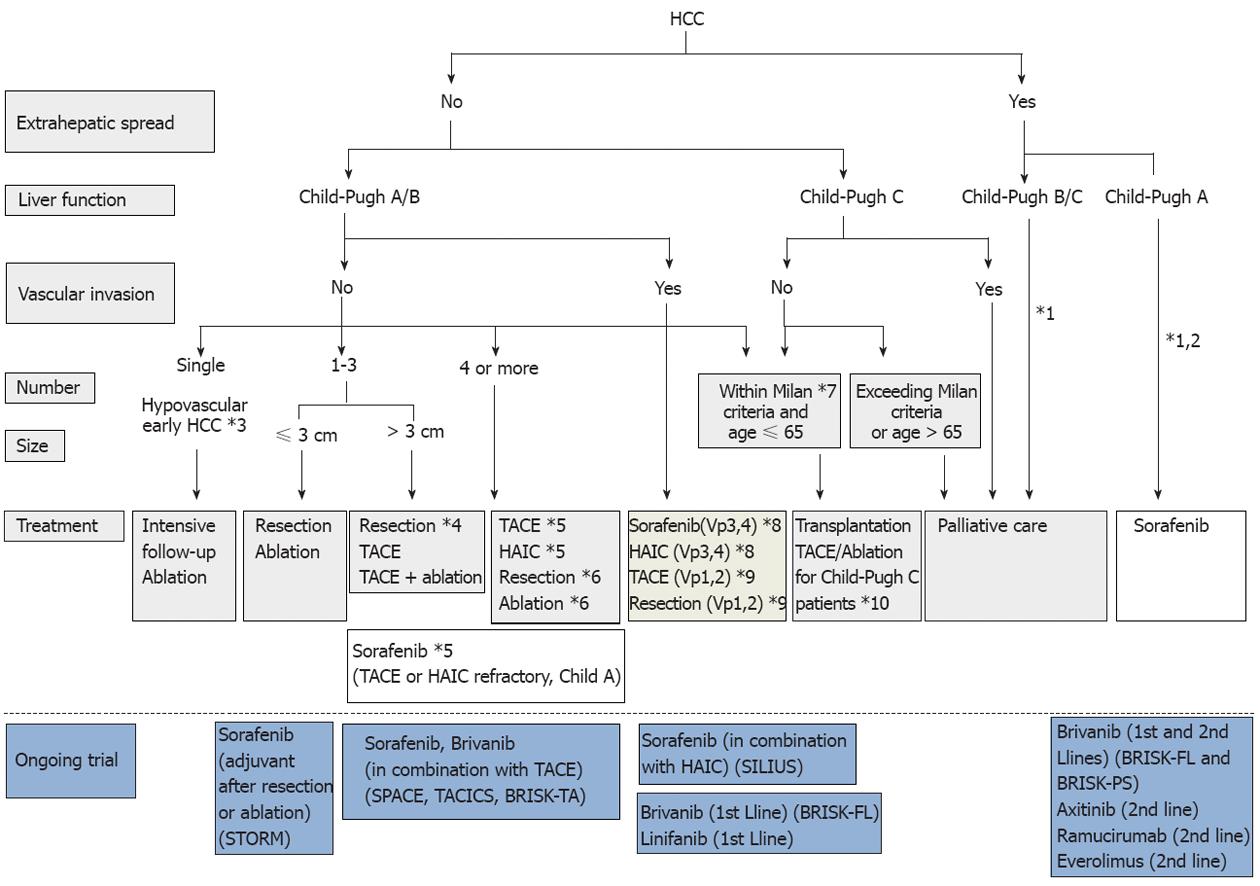
Figure 7 Consensus-based treatment algorithm for hepatocellular carcinoma proposed by Japan Society of Hepatology, revised in 2010.
(Cited and modified from Kudo et al[67] with permission.) *1: Treatment should be performed as if extrahepatic spread is negative, when extrahepatic spread is not considered as a prognostic factor in Child-Pugh class A/B patients; *2: Sorafenib is the first choice of treatment in this setting as a standard of care; *3: Intensive follow-up observation is recommended for hypovascular nodules by the Japanese Evidence-Based Clinical Practice Guidelines. However, local ablation therapy is frequently performed in the following cases: (1) when the nodule is diagnosed pathologically as early hepatocellular carcinoma (HCC); (2) when the nodules show decreased uptake on Gd-EOB-MRI, or (3) when the nodules show decreased portal flow by CTAP, since these nodules frequently progress to advanced HCC; *4: Even for HCC nodules exceeding 3 cm in diameter, transcatheter arterial chemoembolization (TACE) in combination with ablation is frequently performed when resection is not indicated; *5: TACE is the first choice of treatment in this setting. Hepatic arterial infusion chemotherapy (HAIC) using an implanted port is also recommended for TACE-refractory patients. The regimen for this treatment is usually low-dose FP [5-fluorouracil (5-FU) + CDDP] or intra-arterial 5-FU infusion combined with systemic interferon therapy. Sorafenib is also recommended for TACE or HAIC-refractory patients with Child-Pugh class A liver function; *6: Resection is sometimes performed when more than 4 nodules are detected. Ablation is sometimes performed in combination with TACE; *7: Milan criteria: Tumor size ≤ 3 cm and tumor number ≤ 3, or solitary tumor ≤ 5 cm. Even when liver function is good (Child-Pugh A/B), transplantation is sometimes considered for frequently recurring HCC patients; *8: Sorafenib and HAIC are recommended for HCC patients with major portal invasion such as Vp3 (portal invasion in the 1st portal branch) or Vp4 (portal invasion in the main portal branch); *9: Resection and TACE are frequently performed when portal invasion is minor, such as Vp1 (portal invasion in the 3rd or more peripheral portal branch) or Vp2 (portal invasion in the 2nd portal branch); *10: Local ablation therapy or subsegmental TACE is performed even for Child-Pugh C patients when transplantation is not indicated when there is no hepatic encephalopathy, no uncontrollable ascites, and a low bilirubin level (< 3.0 mg/dL). However, it is regarded as an experimental treatment because there is no evidence of a survival benefit in Child-Pugh C patients. A prospective study is necessary to clarify this issue.
- Citation: Kudo M. Signaling pathway/molecular targets and new targeted agents under development in hepatocellular carcinoma. World J Gastroenterol 2012; 18(42): 6005-6017
- URL: https://www.wjgnet.com/1007-9327/full/v18/i42/6005.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i42.6005