Published online Oct 28, 2022. doi: 10.35712/aig.v3.i4.96
Peer-review started: June 7, 2022
First decision: July 14, 2022
Revised: July 30, 2022
Accepted: September 13, 2022
Article in press: September 13, 2022
Published online: October 28, 2022
Processing time: 142 Days and 15.2 Hours
Artificial intelligence (AI) evolved many years ago, but it gained much advance
Core Tip: Globally, hepatocellular carcinoma is a major cause of illness and fatality. Although substantial progress has been made in the treatment strategy for hepatocellular carcinoma, managing it is still a major issue. Artificial intelligence in the area of gastroenterology, especially in hepatology, is particularly useful for various investigations of hepatocellular carcinoma because it is a commonly found tumor and has specific radiological features that enable diagnostic procedures without the requirement of histological study. Artificial intelligence is utilized to diagnose, curative and prediction goals.
- Citation: Mokhria RK, Singh J. Role of artificial intelligence in the diagnosis and treatment of hepatocellular carcinoma. Artif Intell Gastroenterol 2022; 3(4): 96-104
- URL: https://www.wjgnet.com/2644-3236/full/v3/i4/96.htm
- DOI: https://dx.doi.org/10.35712/aig.v3.i4.96
Hepatocellular carcinoma (HCC) is a malignancy of the liver that is very lethal. It is the most commonly found primary adult liver malignancy. Worldwide it is the third most common cause of cancer-related death[1]. According to the American Cancer Society, 42810 new liver and intrahepatic cholangiocarcinoma cases were detected in 2020, of which 30160 died[2]. Surgery (liver transplantation and resection) is the backbone of HCC treatment and is the only possible treatment option. Delamination or removal is an alternative treatment for small tumors. In addition, intra-arterial treatment and chemotherapy can control the disease to some extent[1]. In addition, HCC has certain radiological features that do not require histological examination for diagnosis. Therefore, the analysis and interpretation of diagnostic imaging procedures are not always easy as it changes during the disease course. The same applies to diagnosis/prognosis and treatment response, as they are influenced by numerous factors.
Artificial intelligence (AI) is the computer simulation of the human intelligence process. The concept of AI emerged in the 1950s[3], but only a few years ago it made real progress. It has been used in a variety of industries, i.e. image and natural language processing. In the field of medicine, AI is becoming increasingly significant. The utilization of AI is rapidly expanding and is increasingly useful in understanding gastrointestinal diseases[4-6]. The phrase “artificial intelligence” refers to a group of computer programs that attempt to mimic human brain capabilities, i.e. learning and problem-solving.
AI has evolved into a separate discipline called machine learning (ML). ML examines data to develop algorithms that can recognize distinct behavior forms and confirm predictive models. ML focuses on developing mathematical models that assist machines in making predictions or judgments without being explicitly programmed. Various ML techniques, for instance, support vector machines (SVM), artificial neural networks (ANNs), classification, and regression trees, seem to be employed in various investigations in the medical discipline[7]. Deep learning (DL) has emerged as an emerging paradigm of ML for developing multilayered neural network algorithms, and approaches like convolutional neural network (CNN), an ANN multilayer, have been widely accepted and used in radiological image analysis[8,9].
In a nutshell, ML is a core branch of AI, and DL is used to implement it. The use of ML and DL to forecast the risk of gastric cancer has been successful[10]. Figure 1 shows the correlation between AI, ML, and DL.
There are limitations in using AI in various areas of medicine. Looking back on many studies and applications of irrelevant databases having biases can influence the truthfulness of AI. Therefore, it is essential to design a bias-free, proposed, well-designed multicenter collaborative study, and various important aspects, such as economics, medical professional regulation, and ethical reviews, should not be ignored. Various terms associated with AI in this minireview are given in Table 1.
| Term | Definition |
| AI | The utilization of computers and associated techniques to mimic the sharp attitude and critical approach of humans |
| ML | It is a branch of AI and computer science that concerns the usage of data and algorithms to mimic the means that human beings ascertain and step by step upgrading its precision |
| ANN | It is a computational model in accordance with the structure and functions of biological neural networks. ANNs employ a nonlinear function to a loaded sum of inputs and model relations among them |
| CNN | It is a deep learning neural network intended to process structured arrays of data, i.e. radiological images |
| Deep learning | A branch of ML that tries to mimic the human brain and has the ability to gather data and do predictions with remarkable precision |
| AUC | AUC is an approach applied in ML to assess many used models to find out which have the higher performance |
| Accuracy | AI and ML technology employ algorithms to analyze data and perform predictions on the basis of such data. Although studies report that AI programs may regularly achieve accuracy levels of at least 95% and AI programs cannot verify the veracity of the data being examined, the overall accuracy is typically lower yet still higher than 80% |
| C-index (c-statistic) | It is an algorithm performance metric that takes values between 0 and 1 and explains how well the model fits the data |
The utility of AI can enhance diagnostic procedures in the area of liver cancer. CNN in the form of multilayered ANN is interlinked, and whole input data passes through every layer before being transformed to give output data. It is a more advanced version of DL that has its own learning capacity. Ultrasound (US) tests, abdominal computed tomography (CT), magnetic resonance imaging (MRI) of the abdomen, positron emission tomography (PET), and histology can benefit from CNN.
HCC develops in cirrhotic livers most of the time but not always. Clinical practice recommendations advocate routine abdominal US in hepatic cirrhosis patients. This approach is used for detecting lesions that occupy space. US is the primary machine for detecting hepatic disease and fresh lesions. Though, analysis of images is not straightforward and can be subject to interobserver variations.
To review the fundamental disorder, Bharti et al[11] established an ANN model that discriminated various phases of hepatic infection by analyzing US images: normal liver, chronic liver disease, cirrhosis, and HCC. Further, this model’s accuracy was found to be 96.6%[11]. An algorithm to analyze US images was developed by Liu et al[12]. Liu et al[12] preferred the liver capsule to detect the existence of cirrhosis, even at an early stage when radiological findings are not clearly visible. By investigating the morphology of the liver capsule, Liu et al[12] predicted the presence or absence of cirrhosis with an area under the curve (AUC) of 0.968.
The human output is defined when it comes to identifying liver lesions from US images. Schmauch et al[13] developed a DL approach that could reveal and label benign and malignant space-occupying liver lesions. This system requires acceptance. It has the potential to improve the diagnostic yield of US and inform clinicians about potentially malignant lesions[13].
To improve the ability of contrast-enhanced US (C-US) for the detection of cancer-related characteristics, the use of AI has been utilized. Guo et al[14] confirmed how applying DL to the behavior of liver lesions observed on C-US in three phases (arterial, portal, and late) improved the accuracy, sensitivity, and specificity of the investigation undertaken.
When an US reveals a fresh liver lesion, further imaging procedures, primarily dynamic contrast-enhanced CT or MRI, are used to get an accurate diagnosis. In dynamic CT or MRI scans, the radiological behavior of liver lesions can be used to characterize the lesion. If CT scans of liver nodules reveal unclear behavior, then lesion biopsy is prescribed as per the recommendation of the European Association for the Study of the Liver guidelines[15]. As suggested by the American Association for the Study of Liver Diseases guidelines[16], there is the possibility of non-detection of a malignant lesion involved during the procedure or during close follow-up. A study was performed on 178 patients with cirrhosis and liver nodules by Mokrane et al[17], and they were unable to differentiate between neoplastic and non-neoplastic lesions in these patients, hence requiring a biopsy. On doing a biopsy, 77% of the lesions were malignant. By applying DL techniques, the AUC for classifying nodules as HCC or non-HCC was 0.70. By analyzing the output of three-layered ANN, Yasaka et al[18] with the help of contrast-enhanced CT classified liver masses into five groups: A (cholangiocarcinoma, hepatocholangiocarcinoma, or metastasis); B (other malignant tumors, i.e. cholangiocarcinoma, hepatocholangiocarcinoma, or metastasis); C (ambiguous masses, dysplastic nodules, or early HCC, and benign masses other than cysts or haemangiomas); D (haemangiomas); and E (cysts).
Assessing tumor load could be beneficial for detecting tumor relapse in follow-up CT scans. Vivanti et al[19] proposed an automated detecting procedure for recurrence on the basis of early manifestation of the tumor, its CT behavior, baseline tumor load/mass quantification, and follow-up. With an accuracy of 86%, this approach demonstrated a higher proportion of true positives in detecting tumor relapse.
The usefulness of liver segmentation in assessing lesions in the liver and managing good treatment is critical. Li et al[20] developed a CNN that could cause the segmentation of liver tumors on the basis of CT images having an accuracy of 82.67% ± 1.43%, which is better than existing approaches, allowing for more appropriate treatment planning.
The use of CNN in MRI has also been investigated. Hamm et al[21] prepared and verified a CNN-based DL approach that identified MRI liver lesions with 92% accuracy, 92% sensitivity, and 98% specificity with a mean computation time of 5.6 milliseconds.
Further research has used more MRI sequences, risk components, and clinical information of the patient to create an automated classification method that classifies hepatic lesions as adenoma, cyst, haemangioma, HCC, and metastasis, having sensitivity/specificity of 0.80/0.78, 0.93/0.93, 0.84/0.82, 0.73/0.56, and 0.62/0.77 respectively[22].
Preis et al[23] used a neural network to study hepatic intake of fluorodeosyglucose 18F along with data from the patient and clinical details to assess the results of 18F-FDG PET/CT (Fluorine 18 fluorodeosyglucose positron emission tomography/computed tomography). Preis et al[23] obtained higher sensitivity and specificity to find malignancy of the liver, which remained unrevealed visibly. This method can help the radiologist in the analysis of PET.
Even for experienced pathologists, determining the histopathological categorization of a liver lesion and distinction of tumor strain is critical to planning the treatment and prognosis assessment of the disease. Kiani et al[24] were concerned with the histopathological distinction between HCC and cholangiocarcinoma and employed AI to assist pathologists.
Others reported how a deep CNN can perform an automatic identification of HCC and discriminate normal tissue from malignant tissue as well as identify key biological predictors, utilizing previous histopathological images of HCC[25].
The specific biological variance among HCC patients hampers evidence-based clinical assessment among all patients. Hence, for optimizing treatment techniques and measuring the results, powerful standardized risk classification tools are required. AI has the potential to play a significant role in the treatment of HCC in this area. The majority of studies about the applicability of AI in HCC treatment are focused on analyzing specific tumor attributes, i.e. radiological, histological, or genetic traits, or combining clinical data to estimate treatment response. Therefore, patients will be able to be better selected for certain treatment alternatives.
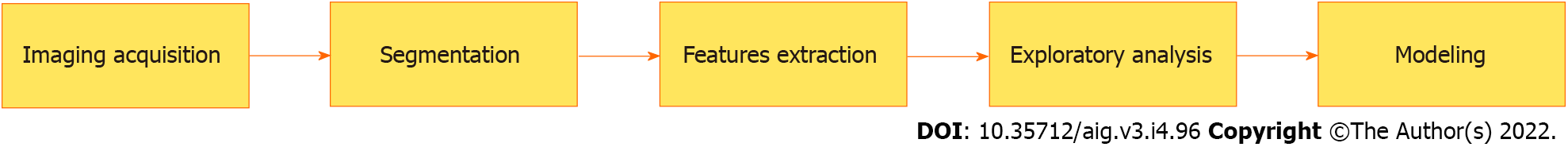
The examination and remedy measure of HCC is generally performed with imaging facilities i.e. C-US, CT, and MRI following investigation of assured tumor characteristics, i.e. vascularization or behavior after the addition of a contrasting substance[26]. These attributes are amenable to biases after analysis by radiologists, along with the absence of high-resolution dimensional images. Recently an advanced technology has emerged in the area of radiology and cancer which is known as radiomics[27]. This technology extracts a large amount of significant data from the radiological images and links this data with the related biological system. The study of complete data with AI software can give effective and accurate reports for proper diagnosis and prognosis[27,28]. Figure 2 shows various stages of radiomics where AI can play a role.
The early reappearance of the tumor following operative removal is due to an unsatisfactory prognostic process. The recognition of clinical cases before surgical operation with more risk of relapse is essential to escape irrelevant treatment. Various computer models help to analyze specific tumor markers/ features and assist in the prognosis of the risk of relapse before operative procedures. These models also help in the assessment of survival after surgical removal.
Vascular microinvasion (VMI) is a self-sufficient prognostic component of relapse. VMI is linked with poor outcomes following tumor excision[29]. The accessibility of data regarding VMI preoperatively can be of high use. The radiological approach presently used in medical practice does not give a fair diagnosis.
Several studies explain radiomic signatures that presume the status of VMI preoperatively on the basis of contrast-enhanced CT[30,31] or MRI[32]. These techniques include exposure to radiation, are hard to execute, and are expensive. In a recent study, Dong et al[33] used grayscale US images based on radiomic algorithms to proceed with radiomic signatures in the prediction of VMI. By using radiomic techniques, Ji et al[34] developed prognostic models for relapse after excision surgery for assessing contrast-enhanced CT images and had a C-index value of 0.633-0.699. These models could be utilized for providing an individualized risk stratification for managing HCC individually.
ML techniques help in assessing survival after surgical resection as observed in many studies[35-37]. Recently, more advanced DL models helped in assessing survival after surgical resection on the basis of digitalized histological images of tumors.
According to Barcelona Clinical Liver Cancer (BCLC) classification, transcatheter arterial chemoembolization (TACE) exists as the preferred option for the treatment of intermediary B stage HCC[38]. The right choice of patients who can get benefit from this treatment is critical in order to minimize superfluous investigations that can lead to unfavorable side effects and waste healthcare resources. Studies based on AI approaches have been created as a trial to infer the feedback of TACE treatment and facilitate the proper selection of patients. The majority of the studies rely on image analysis, but some studies have also utilized genomic signatures. Morshid et al[39] developed an automatic ML algorithm that predicted TACE response using a mixture of quantitative CT image attributes and pretreatment patient clinical data. They obtained a prediction accuracy rate of 74.2% while working on combining the Barcelona Clinic Liver Cancer stage and quantitative image characteristics instead of applying the Barcelona Clinic Liver Cancer stage alone. Peng et al[40] used CT scans from 789 patients from three separate hospitals to verify a DL model for predicting TACE response. They were able to predict complete responses with an accuracy of 84% and an AUC of 0.97. Liu et al[41] developed and verified a DL radiomics-based C-US approach as a result of a quantitative assessment of C-US cine recordings. They demonstrated a high level of reproducibility and an AUC of 0.93 (95% confidence interval: 0.80-0.98) for predicting TACE reaction.
Further research has combined MRI and clinical data with ML approaches to predict TACE response. Abajian et al[42] worked on 36 patients who had an MRI prior to TACE. They built a response prediction model with 78.0% accuracy, 62.5% sensitivity, and 82% specificity.
The efficacy of TACE has also been tested by a post-treatment survival analysis of patients. Mähringer-Kunz et al[43] designed an ANN with every variable of main traditional prediction scores to produce a survival prediction model following TACE (ART[44], ABCR[45], and SNACOR[46]). With an AUC of 0.77, 78% sensitivity, and 81% specificity, they expected a 1-year survival rate that was better than the conventional scores.
Although radiomics have been used in the majority of investigations estimating the usage of AI to examine TACE. Some have also looked at genetic analysis to predict TACE response. Ziv et al[47] analyzed genetic mutations by applying SVM algorithms to look for tumor responses following TACE. However, this study involved a small number of cases.
Radiofrequency ablation has also been studied as a treatment for HCC in its early stages[38]. Liang et al[48] used SVM to create a prognostic model of HCC relapse. They investigated 83 HCC cases that had undergone radiofrequency ablation and secured an AUC of 0.69, 67% sensitivity, and 86% specificity. From this data, they could recognize patients with a greater chance of relapse.
Apart from the use of any therapy, AI approaches have been used to predict the overall survival of HCC patients. The observations by Dong et al[49] were based on current information on the relationship between anomalies in DNA methylation and HCC[50-52]. They employed ML techniques (SVM) for the evaluation of DNA methylation data from 377 HCC samples and created three risk groups to expect complete survival and achieved a mean 10-fold cross-validation score of 0.95.
To illustrate the effectiveness of AI for medical assistance, further research is required that compares the output of medical staff with AI assistance vs experts lacking AI assistance. These studies should target elements linked to curing and prognosis (for instance, identifying ambiguous hepatic wounds, the existence of vascular invasion, and the reaction to percutaneous treatments) to analyze liver masses and explore HCC. Additional significant points are the utilization of AI for interpretation of HCC behavior in cirrhotic and non-cirrhotic patients, in the differential diagnosis of primary and metastatic liver lesions[53], and particularly in the clinical detection of cholangiocarcinoma, which is difficult to differentiate from HCC with existing approaches and has distinct treatment methods from HCC. Simultaneously, healthcare providers must be trained for the integration of AI into everyday practice in the area of liver cancer.
AI has guided the detection of HCC (on the basis of premalignant variations, imaging, and biomarkers) as a result of its capability to examine huge datasets and combine data effectively. The perspective of AI techniques is immense in every stage in the handling of HCC, e.g., from early diagnosis to treatment options and prognostic and therapeutic response prognosis. These methods could promote accurate and personalized medicine to assist clinical practice and better utilize healthcare resources. Numerous datasets (radiological images or pathologic data) could be utilized individually or in conjunction for accuracy better than that of conventional statistical means. Moreover, AI-based approaches can also assist in lowering interobserver variance while studying images and leads to standardization.
The outcomes from many studies endorse the consolidation of the ML models with clinical/pathologic data and created clinical scores or biomarkers. Biomarkers detected by the incorporation of several ‘-omics’ datasets lead to the recognition of a biochemical tumor signature, which revolutionizes HCC detection in the near future.
One of the most significant advancements in recent years has been the utilization of AI technologies in medicine. It will almost certainly grow in popularity as a result of its utility in processing and analyzing massive amounts of available data. However, we should be attentive that there are some limitations that may reduce its acceptability and application in the medical field. Medical professionals need to understand the genuine value of AI and recognize the necessity for it to coexist with the essential requirement for human assessment. Regardless of the significant advancements, it is critical to ensure that medical protocols remain completely transparent.
The authors would like to thank Dr. Jitender Bhardwaj, Assistant Professor, Zoology Department, Kurukshetra University, Kurukshetra, Haryana, India, and Sh. Ram Narayan, Lecturer (English), Government High School, Karsa Dod, Karnal, Haryana, India for timely support.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: India
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Lu G, China; Wan Y, China S-Editor: Liu JH L-Editor: Filipodia P-Editor: Liu JH
| 1. | Vitale A, Trevisani F, Farinati F, Cillo U. Treatment of Hepatocellular Carcinoma in the Precision Medicine Era: From Treatment Stage Migration to Therapeutic Hierarchy. Hepatology. 2020;72:2206-2218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 124] [Article Influence: 24.8] [Reference Citation Analysis (0)] |
| 2. | Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70:7-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12667] [Cited by in RCA: 15282] [Article Influence: 3056.4] [Reference Citation Analysis (4)] |
| 4. | Reismann J, Romualdi A, Kiss N, Minderjahn MI, Kallarackal J, Schad M, Reismann M. Diagnosis and classification of pediatric acute appendicitis by artificial intelligence methods: An investigator-independent approach. PLoS One. 2019;14:e0222030. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 47] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 5. | Reichling C, Taieb J, Derangere V, Klopfenstein Q, Le Malicot K, Gornet JM, Becheur H, Fein F, Cojocarasu O, Kaminsky MC, Lagasse JP, Luet D, Nguyen S, Etienne PL, Gasmi M, Vanoli A, Perrier H, Puig PL, Emile JF, Lepage C, Ghiringhelli F. Artificial intelligence-guided tissue analysis combined with immune infiltrate assessment predicts stage III colon cancer outcomes in PETACC08 study. Gut. 2020;69:681-690. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 84] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 6. | Maeda Y, Kudo SE, Mori Y, Misawa M, Ogata N, Sasanuma S, Wakamura K, Oda M, Mori K, Ohtsuka K. Fully automated diagnostic system with artificial intelligence using endocytoscopy to identify the presence of histologic inflammation associated with ulcerative colitis (with video). Gastrointest Endosc. 2019;89:408-415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 163] [Article Influence: 27.2] [Reference Citation Analysis (0)] |
| 7. | Kaul V, Enslin S, Gross SA. History of artificial intelligence in medicine. Gastrointest Endosc. 2020;92:807-812. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 310] [Article Influence: 62.0] [Reference Citation Analysis (1)] |
| 8. | Briceño J. Artificial intelligence and organ transplantation: challenges and expectations. Curr Opin Organ Transplant. 2020;25:393-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 9. | Yang YJ, Bang CS. Application of artificial intelligence in gastroenterology. World J Gastroenterol. 2019;25:1666-1683. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 211] [Cited by in RCA: 160] [Article Influence: 26.7] [Reference Citation Analysis (5)] |
| 10. | Taninaga J, Nishiyama Y, Fujibayashi K, Gunji T, Sasabe N, Iijima K, Naito T. Prediction of future gastric cancer risk using a machine learning algorithm and comprehensive medical check-up data: A case-control study. Sci Rep. 2019;9:12384. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 63] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 11. | Bharti P, Mittal D, Ananthasivan R. Preliminary Study of Chronic Liver Classification on Ultrasound Images Using an Ensemble Model. Ultrason Imaging. 2018;40:357-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 34] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 12. | Liu X, Song JL, Wang SH, Zhao JW, Chen YQ. Learning to Diagnose Cirrhosis with Liver Capsule Guided Ultrasound Image Classification. Sensors (Basel). 2017;17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 59] [Cited by in RCA: 64] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 13. | Schmauch B, Herent P, Jehanno P, Dehaene O, Saillard C, Aubé C, Luciani A, Lassau N, Jégou S. Diagnosis of focal liver lesions from ultrasound using deep learning. Diagn Interv Imaging. 2019;100:227-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 101] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 14. | Guo LH, Wang D, Qian YY, Zheng X, Zhao CK, Li XL, Bo XW, Yue WW, Zhang Q, Shi J, Xu HX. A two-stage multi-view learning framework based computer-aided diagnosis of liver tumors with contrast enhanced ultrasound images. Clin Hemorheol Microcirc. 2018;69:343-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 71] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 15. | European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J Hepatol. 2018;69:182-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5593] [Cited by in RCA: 6013] [Article Influence: 859.0] [Reference Citation Analysis (3)] |
| 16. | Heimbach JK, Kulik LM, Finn RS, Sirlin CB, Abecassis MM, Roberts LR, Zhu AX, Murad MH, Marrero JA. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology. 2018;67:358-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2107] [Cited by in RCA: 3008] [Article Influence: 429.7] [Reference Citation Analysis (3)] |
| 17. | Mokrane FZ, Lu L, Vavasseur A, Otal P, Peron JM, Luk L, Yang H, Ammari S, Saenger Y, Rousseau H, Zhao B, Schwartz LH, Dercle L. Radiomics machine-learning signature for diagnosis of hepatocellular carcinoma in cirrhotic patients with indeterminate liver nodules. Eur Radiol. 2020;30:558-570. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 124] [Article Influence: 24.8] [Reference Citation Analysis (0)] |
| 18. | Yasaka K, Akai H, Abe O, Kiryu S. Deep Learning with Convolutional Neural Network for Differentiation of Liver Masses at Dynamic Contrast-enhanced CT: A Preliminary Study. Radiology. 2018;286:887-896. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 293] [Cited by in RCA: 389] [Article Influence: 48.6] [Reference Citation Analysis (0)] |
| 19. | Vivanti R, Szeskin A, Lev-Cohain N, Sosna J, Joskowicz L. Automatic detection of new tumors and tumor burden evaluation in longitudinal liver CT scan studies. Int J Comput Assist Radiol Surg. 2017;12:1945-1957. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 50] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 20. | Li W, Jia F, Hu Q. Automatic Segmentation of Liver Tumor in CT Images with Deep Convolutional Neural Networks. J Comput Commun. 2015;3:146-151. [RCA] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 155] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 21. | Hamm CA, Wang CJ, Savic LJ, Ferrante M, Schobert I, Schlachter T, Lin M, Duncan JS, Weinreb JC, Chapiro J, Letzen B. Deep learning for liver tumor diagnosis part I: development of a convolutional neural network classifier for multi-phasic MRI. Eur Radiol. 2019;29:3338-3347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 205] [Article Influence: 34.2] [Reference Citation Analysis (0)] |
| 22. | Jansen MJA, Kuijf HJ, Veldhuis WB, Wessels FJ, Viergever MA, Pluim JPW. Automatic classification of focal liver lesions based on MRI and risk factors. PLoS One. 2019;14:e0217053. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 46] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 23. | Preis O, Blake MA, Scott JA. Neural network evaluation of PET scans of the liver: a potentially useful adjunct in clinical interpretation. Radiology. 2011;258:714-721. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 24. | Kiani A, Uyumazturk B, Rajpurkar P, Wang A, Gao R, Jones E, Yu Y, Langlotz CP, Ball RL, Montine TJ, Martin BA, Berry GJ, Ozawa MG, Hazard FK, Brown RA, Chen SB, Wood M, Allard LS, Ylagan L, Ng AY, Shen J. Impact of a deep learning assistant on the histopathologic classification of liver cancer. NPJ Digit Med. 2020;3:23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 181] [Cited by in RCA: 158] [Article Influence: 31.6] [Reference Citation Analysis (0)] |
| 25. | Liao H, Xiong T, Peng J, Xu L, Liao M, Zhang Z, Wu Z, Yuan K, Zeng Y. Classification and Prognosis Prediction from Histopathological Images of Hepatocellular Carcinoma by a Fully Automated Pipeline Based on Machine Learning. Ann Surg Oncol. 2020;27:2359-2369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 37] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 26. | Villanueva A. Hepatocellular Carcinoma. N Engl J Med. 2019;380:1450-1462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2066] [Cited by in RCA: 3150] [Article Influence: 525.0] [Reference Citation Analysis (37)] |
| 27. | Gillies RJ, Kinahan PE, Hricak H. Radiomics: Images Are More than Pictures, They Are Data. Radiology. 2016;278:563-577. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4541] [Cited by in RCA: 5506] [Article Influence: 611.8] [Reference Citation Analysis (3)] |
| 28. | Lambin P, Leijenaar RTH, Deist TM, Peerlings J, de Jong EEC, van Timmeren J, Sanduleanu S, Larue RTHM, Even AJG, Jochems A, van Wijk Y, Woodruff H, van Soest J, Lustberg T, Roelofs E, van Elmpt W, Dekker A, Mottaghy FM, Wildberger JE, Walsh S. Radiomics: the bridge between medical imaging and personalized medicine. Nat Rev Clin Oncol. 2017;14:749-762. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1825] [Cited by in RCA: 3532] [Article Influence: 441.5] [Reference Citation Analysis (0)] |
| 29. | Erstad DJ, Tanabe KK. Prognostic and Therapeutic Implications of Microvascular Invasion in Hepatocellular Carcinoma. Ann Surg Oncol. 2019;26:1474-1493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 286] [Article Influence: 47.7] [Reference Citation Analysis (0)] |
| 30. | Ma X, Wei J, Gu D, Zhu Y, Feng B, Liang M, Wang S, Zhao X, Tian J. Preoperative radiomics nomogram for microvascular invasion prediction in hepatocellular carcinoma using contrast-enhanced CT. Eur Radiol. 2019;29:3595-3605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 162] [Article Influence: 27.0] [Reference Citation Analysis (1)] |
| 31. | Xu X, Zhang HL, Liu QP, Sun SW, Zhang J, Zhu FP, Yang G, Yan X, Zhang YD, Liu XS. Radiomic analysis of contrast-enhanced CT predicts microvascular invasion and outcome in hepatocellular carcinoma. J Hepatol. 2019;70:1133-1144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 278] [Cited by in RCA: 490] [Article Influence: 81.7] [Reference Citation Analysis (0)] |
| 32. | Zhou W, Zhang L, Wang K, Chen S, Wang G, Liu Z, Liang C. Malignancy characterization of hepatocellular carcinomas based on texture analysis of contrast-enhanced MR images. J Magn Reson Imaging. 2017;45:1476-1484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 88] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 33. | Dong Y, Zhou L, Xia W, Zhao XY, Zhang Q, Jian JM, Gao X, Wang WP. Preoperative Prediction of Microvascular Invasion in Hepatocellular Carcinoma: Initial Application of a Radiomic Algorithm Based on Grayscale Ultrasound Images. Front Oncol. 2020;10:353. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 28] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 34. | Ji GW, Zhu FP, Xu Q, Wang K, Wu MY, Tang WW, Li XC, Wang XH. Machine-learning analysis of contrast-enhanced CT radiomics predicts recurrence of hepatocellular carcinoma after resection: A multi-institutional study. EBioMedicine. 2019;50:156-165. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 154] [Cited by in RCA: 143] [Article Influence: 23.8] [Reference Citation Analysis (0)] |
| 35. | Ho WH, Lee KT, Chen HY, Ho TW, Chiu HC. Disease-free survival after hepatic resection in hepatocellular carcinoma patients: a prediction approach using artificial neural network. PLoS One. 2012;7:e29179. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 57] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 36. | Chiu HC, Ho TW, Lee KT, Chen HY, Ho WH. Mortality predicted accuracy for hepatocellular carcinoma patients with hepatic resection using artificial neural network. ScientificWorldJournal. 2013;2013:201976. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 32] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 37. | Shi HY, Lee KT, Lee HH, Ho WH, Sun DP, Wang JJ, Chiu CC. Comparison of artificial neural network and logistic regression models for predicting in-hospital mortality after primary liver cancer surgery. PLoS One. 2012;7:e35781. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 84] [Cited by in RCA: 79] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 38. | Forner A, Reig M, Bruix J. Hepatocellular carcinoma. Lancet. 2018;391:1301-1314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2800] [Cited by in RCA: 4075] [Article Influence: 582.1] [Reference Citation Analysis (6)] |
| 39. | Morshid A, Elsayes KM, Khalaf AM, Elmohr MM, Yu J, Kaseb AO, Hassan M, Mahvash A, Wang Z, Hazle JD, Fuentes D. A machine learning model to predict hepatocellular carcinoma response to transcatheter arterial chemoembolization. Radiol Artif Intell. 2019;1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 81] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 40. | Peng J, Kang S, Ning Z, Deng H, Shen J, Xu Y, Zhang J, Zhao W, Li X, Gong W, Huang J, Liu L. Residual convolutional neural network for predicting response of transarterial chemoembolization in hepatocellular carcinoma from CT imaging. Eur Radiol. 2020;30:413-424. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 69] [Cited by in RCA: 120] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 41. | Liu D, Liu F, Xie X, Su L, Liu M, Kuang M, Huang G, Wang Y, Zhou H, Wang K, Lin M, Tian J. Accurate prediction of responses to transarterial chemoembolization for patients with hepatocellular carcinoma by using artificial intelligence in contrast-enhanced ultrasound. Eur Radiol. 2020;30:2365-2376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 94] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 42. | Abajian A, Murali N, Savic LJ, Laage-Gaupp FM, Nezami N, Duncan JS, Schlachter T, Lin M, Geschwind JF, Chapiro J. Predicting Treatment Response to Image-Guided Therapies Using Machine Learning: An Example for Trans-Arterial Treatment of Hepatocellular Carcinoma. J Vis Exp. 2018;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 43. | Mähringer-Kunz A, Wagner F, Hahn F, Weinmann A, Brodehl S, Schotten S, Hinrichs JB, Düber C, Galle PR, Pinto Dos Santos D, Kloeckner R. Predicting survival after transarterial chemoembolization for hepatocellular carcinoma using a neural network: A Pilot Study. Liver Int. 2020;40:694-703. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 36] [Article Influence: 7.2] [Reference Citation Analysis (2)] |
| 44. | Sieghart W, Hucke F, Pinter M, Graziadei I, Vogel W, Müller C, Heinzl H, Trauner M, Peck-Radosavljevic M. The ART of decision making: retreatment with transarterial chemoembolization in patients with hepatocellular carcinoma. Hepatology. 2013;57:2261-2273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 269] [Article Influence: 22.4] [Reference Citation Analysis (0)] |
| 45. | Adhoute X, Penaranda G, Naude S, Raoul JL, Perrier H, Bayle O, Monnet O, Beaurain P, Bazin C, Pol B, Folgoc GL, Castellani P, Bronowicki JP, Bourlière M. Retreatment with TACE: the ABCR SCORE, an aid to the decision-making process. J Hepatol. 2015;62:855-862. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 125] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 46. | Kim BK, Shim JH, Kim SU, Park JY, Kim DY, Ahn SH, Kim KM, Lim YS, Han KH, Lee HC. Risk prediction for patients with hepatocellular carcinoma undergoing chemoembolization: development of a prediction model. Liver Int. 2016;36:92-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 61] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 47. | Ziv E, Yarmohammadi H, Boas FE, Petre EN, Brown KT, Solomon SB, Solit D, Reidy D, Erinjeri JP. Gene Signature Associated with Upregulation of the Wnt/β-Catenin Signaling Pathway Predicts Tumor Response to Transarterial Embolization. J Vasc Interv Radiol. 2017;28:349-355.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 48. | Liang JD, Ping XO, Tseng YJ, Huang GT, Lai F, Yang PM. Recurrence predictive models for patients with hepatocellular carcinoma after radiofrequency ablation using support vector machines with feature selection methods. Comput Methods Programs Biomed. 2014;117:425-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 31] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 49. | Dong RZ, Yang X, Zhang XY, Gao PT, Ke AW, Sun HC, Zhou J, Fan J, Cai JB, Shi GM. Predicting overall survival of patients with hepatocellular carcinoma using a three-category method based on DNA methylation and machine learning. J Cell Mol Med. 2019;23:3369-3374. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 50. | Xu RH, Wei W, Krawczyk M, Wang W, Luo H, Flagg K, Yi S, Shi W, Quan Q, Li K, Zheng L, Zhang H, Caughey BA, Zhao Q, Hou J, Zhang R, Xu Y, Cai H, Li G, Hou R, Zhong Z, Lin D, Fu X, Zhu J, Duan Y, Yu M, Ying B, Zhang W, Wang J, Zhang E, Zhang C, Li O, Guo R, Carter H, Zhu JK, Hao X, Zhang K. Circulating tumour DNA methylation markers for diagnosis and prognosis of hepatocellular carcinoma. Nat Mater. 2017;16:1155-1161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 478] [Cited by in RCA: 628] [Article Influence: 78.5] [Reference Citation Analysis (0)] |
| 51. | Villanueva A, Portela A, Sayols S, Battiston C, Hoshida Y, Méndez-González J, Imbeaud S, Letouzé E, Hernandez-Gea V, Cornella H, Pinyol R, Solé M, Fuster J, Zucman-Rossi J, Mazzaferro V, Esteller M, Llovet JM; HEPTROMIC Consortium. DNA methylation-based prognosis and epidrivers in hepatocellular carcinoma. Hepatology. 2015;61:1945-1956. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 266] [Cited by in RCA: 324] [Article Influence: 32.4] [Reference Citation Analysis (0)] |
| 52. | Yeh CC, Goyal A, Shen J, Wu HC, Strauss JA, Wang Q, Gurvich I, Safyan RA, Manji GA, Gamble MV, Siegel AB, Santella RM. Global Level of Plasma DNA Methylation is Associated with Overall Survival in Patients with Hepatocellular Carcinoma. Ann Surg Oncol. 2017;24:3788-3795. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 53. | Azer SA. Deep learning with convolutional neural networks for identification of liver masses and hepatocellular carcinoma: A systematic review. World J Gastrointest Oncol. 2019;11:1218-1230. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 70] [Cited by in RCA: 51] [Article Influence: 8.5] [Reference Citation Analysis (4)] |