Published online Feb 28, 2022. doi: 10.35713/aic.v3.i1.1
Peer-review started: November 9, 2021
First decision: December 13, 2021
Revised: December 31, 2021
Accepted: February 20, 2022
Article in press: February 20, 2022
Published online: February 28, 2022
Processing time: 107 Days and 11.2 Hours
Artificial intelligence (AI) is defined as the digital computer or computer-controlled robot's ability to mimic intelligent conduct and crucial thinking commonly associated with intelligent beings. The application of AI technology and machine learning in medicine have allowed medical practitioners to provide patients with better quality of services; and current advancements have led to a dramatic change in the healthcare system. However, many efficient applications are still in their initial stages, which need further evaluations to improve and develop these applications. Clinicians must recognize and acclimate themselves with the developments in AI technology to improve their delivery of healthcare services; but for this to be possible, a significant revision of medical education is needed to provide future leaders with the required competencies. This article reviews the potential and limitations of AI in healthcare, as well as the current medical application trends including healthcare administration, clinical decision assistance, patient health monitoring, healthcare resource allocation, medical research, and public health policy development. Also, future possibilities for further clinical and scientific practice were also summarized.
Core Tip: In this review, we explored the potential of powerful artificial intelligence (AI) for a more comprehensive application in the healthcare setting. Moreover, we also pointed out the demerits and problems in the current application of AI in medicine.
- Citation: Hung CM, Shi HY, Lee PH, Chang CS, Rau KM, Lee HM, Tseng CH, Pei SN, Tsai KJ, Chiu CC. Potential and role of artificial intelligence in current medical healthcare. Artif Intell Cancer 2022; 3(1): 1-10
- URL: https://www.wjgnet.com/2644-3228/full/v3/i1/1.htm
- DOI: https://dx.doi.org/10.35713/aic.v3.i1.1
McCarthy, one of the core founders of artificial intelligence (AI), defined AI as the science and engineering of making intelligent machines[1]. AI has come a long way since its conception in 1956[2]. AI research aims to establish a capable system with intelligence to overcome the Turing test, demonstrating intelligent behavior identical to humans. For the next 60 years, this specialty encountered several episodes of excitement and frustration with nearly no advancement. However, in 2010, deep learning achieved marked improvements. This achievement is a type of machine learning (ML) with multiple layers of nodes among the input and output layers, resulting in artificial neural networks capable of establishing excellent development in recognizing speech, classifying an image, and translating context[3].
AI has been applied to analyze complex and big data to deliver outputs beyond human input in diverse healthcare backgrounds[4]. Davenport et al[5] advocated that AI systems would not extensively take over human clinical professionals but would amplify their patient care achievements. In other words, the concept of professional advice from a digital helper is not better than the clinician, but the fusion and application of ML into clinical medicine would enhance accurate healthcare delivery[6]. Rather than traditional robotics, AI applications in current healthcare mainly affect clinicians and medical institutions accessing enormous data sets of crucial clinical knowledge. A scheme of medical information for patient care could use sophisticated algorithms to give real-time analysis[7], including diagnosis, management strategies and prognosis, recurrence and survival rates, and information collection rates of millions of patients, geographical distributions, and countless and sometimes interconnected health status of oncologic patients. This advanced computing power of AI can detect and analyze large and small trends from the available information, and even forecast through ML designed to classify possible health prognoses.
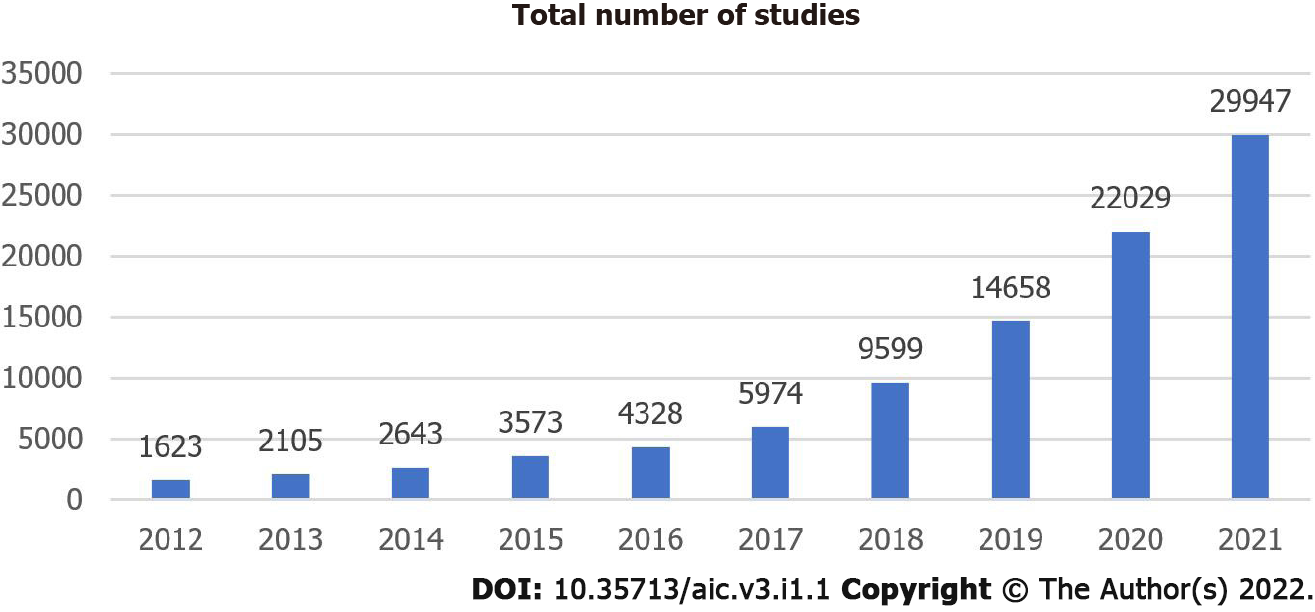
The importance of AI technology in medical healthcare provision and study is increasingly becoming apparent[8]. There is a rapid growth trend of related publications on this topic in the form of academic articles from medical professionals (Figure 1). Specialists have emphasized the effectiveness and capability of AI-empowered healthcare provision. Recently, more countries and private institutions have invested in this technological progress[9]. In addition, the United States Food and Drug Administration (FDA) has enthusiastically promoted AI-empowered instruments in the medical market[10].
In this study, the potentials of AI, its application in different fields of healthcare, and its current limitations will be discussed. Furthermore, we also investigated the advantages of clinicians over AI in clinical work and suggest different ways of cooperating with AI effectively.
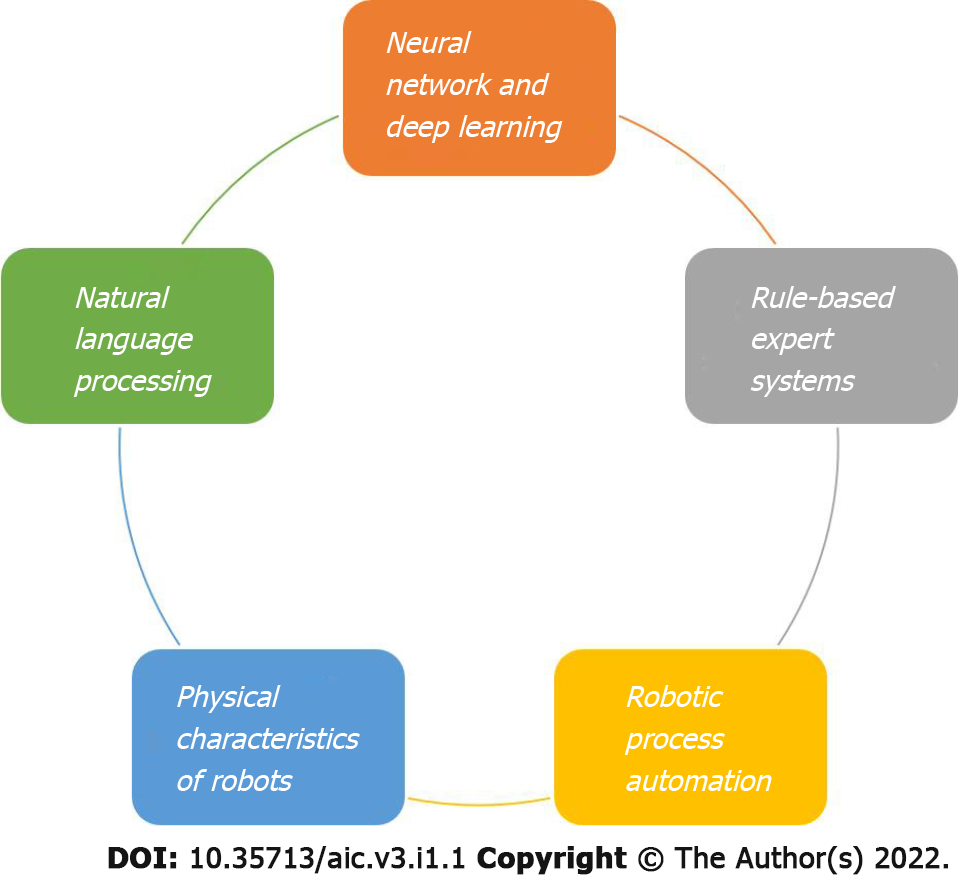
AI is a collection of technologies consisting of abilities that could be applied in healthcare. Some particular AI technologies are paramount to healthcare (Figure 2).
Neural networks and deep learning are essential to ML, a statistical technology for fitting models to data and 'learning' by training models with data. The neural networks technology has been available since the 1960s for categorization applications[11]. A standard neural network comprises many simple, connected processors called neurons, each producing a sequence of real-valued activations[12]. It imitates the process of how neurons manage signals. It can determine if one person would suffer from a specific disease in his or her life. It views the disease based on the inputs, outputs, and weights of variables or parameters related to the inputs with outputs.
Deep learning is the most complicated form of ML, which involves neural network models with different levels of parameters to predict prognosis. Each character in a deep learning model usually has limited implications for clinical professionals. In other words, the explanation of the model's prognosis may be very challenging to interpret. Nowadays, the typical utilization of deep learning in healthcare involves the recognition of possibly cancerous lesions in radiologic imaging[13]. Currently, it is commonly applied to detect clinically specific features in imaging data, which is easily neglected by the human eye[14].
Since the 1950s, AI researchers have strived to make sense of human language. Natural language processing aims to program machines to interpret human language as humans do. It comprises speech recognition, word analysis, sentence translation, and other intentions based on human language. Statistical natural language processing is related to deep learning neural networks. It has also contributed to increased recognition accuracy. A natural language processing system can duplicate patient interactions and operate conversational AI[15]. Furthermore, it has succeeded in scaling up partial roles of clinical decision-making, developing tools to stratify risks, and even identifying possible surgical complications from clinical records[16], and performing patient triage by identifying syndromes[17].
Expert systems could automatically alert patients and provide instructions according to the telemonitoring data. This is expected to increase patient self-care and improve clinical management[18].
In the 1980s, expert systems related to the ‘if-then’ rules were the primary technique for AI. Human experts and knowledge engineers were required to build up a set of guides in a specific knowledge domain. In the healthcare aspect, they were extensively applied to assist in making clinical decisions. This system consisted of an expert system and a statistical analysis system linked to a patient database[19]. They have been used for the past decades, but are more extensively used nowadays[20]. However, they are proposed to be replaced by more advanced ML algorithms, possibly because of their static nature. As these expert systems are applied to clinical use, this demerit becomes accentuated by the rapid generation rate of new knowledge, the regional differences related to the expression of many diseases, and the change rate of patient demographics and disease incidence in the future[19].
Physical robots are well-known for performing repetitive and precise pre-defined work, such as elevating, locating, welding, or collecting objects during hospital supply delivery. Since the 1980s, there has been an incremental development of minimally invasive surgeries. However, this was limited by the complexity of surgery due to the technical constraint of traditional laparoscopic instruments. Robotic technology provides a 3-dimensional view of the operating field, allows filtering of physiological tremor, and permits greater precision and control through its articulated arms. These advantages offer solutions to the limitation of traditional laparoscopic instruments[21]. The United States initially approved robot-assisted surgery in 2000. Robots empower the surgeons and provide a clearer vision to perform accurate and minimally invasive surgery resulting in smaller surgical wounds[22]. Robotic-assisted prostatectomy, cystectomy, pyeloplasty, nephrectomy, and partial nephrectomy are all becoming increasingly common techniques used by surgeons[23]. Moreover, robots are becoming more intelligent, as other AI facilities are being installed in the operating systems. Of course, dominant decision-making is still made by humans during surgery.
“Automation” is defined as the application of robotics, AI, ML, machine vision, and similar emerging and mature digital technologies to allow human work to be substituted by robots[24]. This technique executes structured digital works for organizational goals. Robotic process automation involves mere computer programs on servers. It hinges on a set of work assignments, business guidelines, and a ‘presentation layer’ combination with information systems to mimic a semi-intelligent system operator. In the medical field, it is usually applied to perform repetitive work, e.g., updating patient records or billing, extracting data from images into transactional systems, etc[25].
According to the study by Willis et al[26], many forms of automation already exist in the healthcare setting. Not only do they increase the productivity of human employees, but they also do not remove human tasks entirely. Automation has even unexpectedly created more work for the medical staff. Although automation has allowed humans to process tasks more efficiently, it has resulted in more administrative work.
During the global health emergency related to coronavirus disease 19 (COVID-19), experts have worked day and night to explore new technologies to mitigate the pandemic. Due to this, the trend of AI application in healthcare has grown rapidly[9], and has involved the development of sophisticated algorithms to perform complicated work efficiently and effectively[27]. Recent research has shown that AI could greatly enhance COVID-19 screening, diagnostics, and prediction, resulting in better scale-up, a timely response, a more reliable and efficient outcome. Furthermore, it was found that sometimes it outperforms humans in certain healthcare tasks[28].
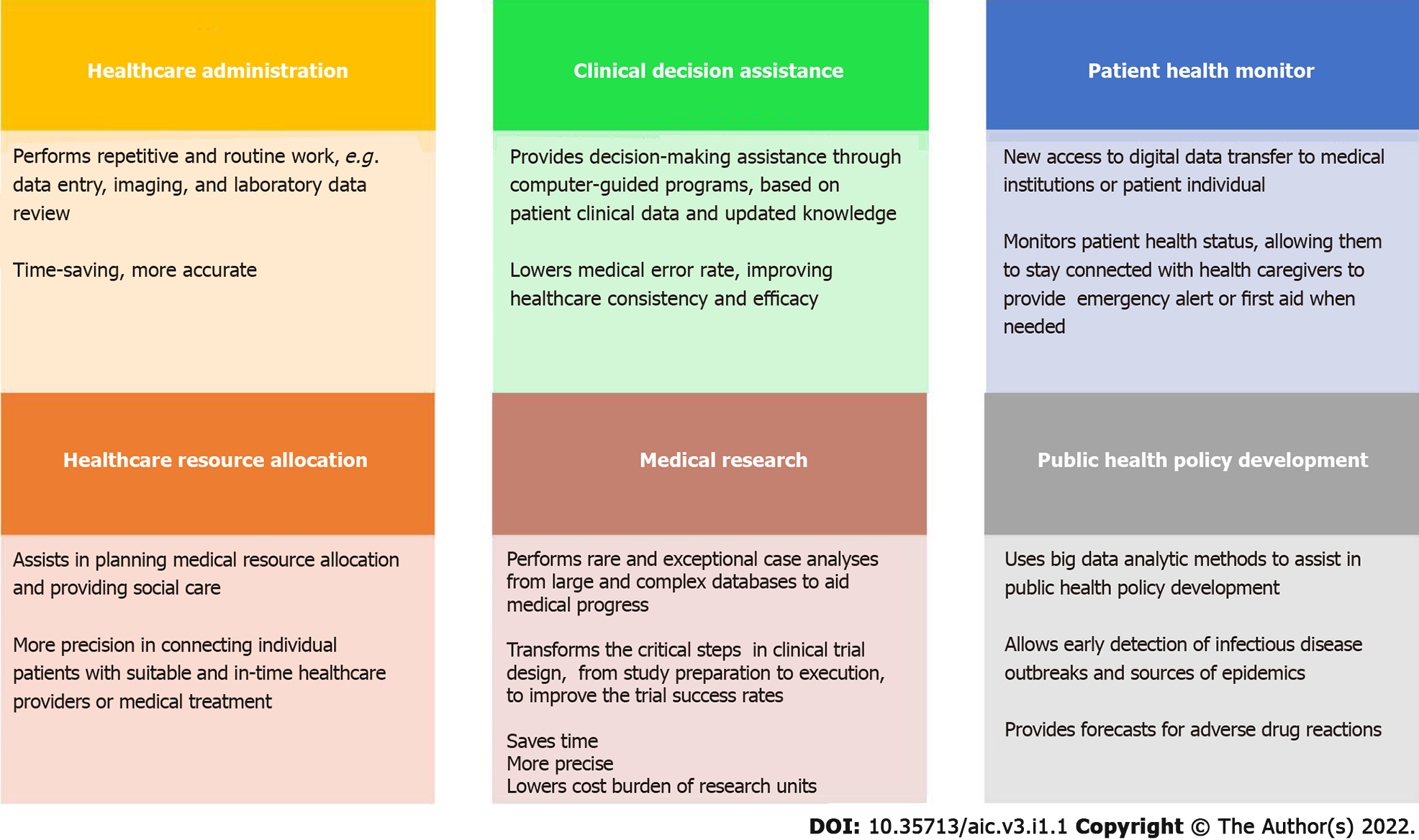
In summary, AI-empowered healthcare delivery exerts a significant impact on healthcare administration, clinical decision assistance, patient health monitoring, healthcare resource allocation, medical research, and public health policy development (Figure 3).
AI could save time, which the clinical staff could use to care for patients, by performing repetitive and routine work, such as data entry, imaging, and laboratory data review[2]. The connection of ML algorithms with digital medical records could help clinical staff and administrators gain accurate patient data[29]. The accuracy and speed of data searches could be refined using ML and concept-based information retrieval systems. AI has already been applied to identify diseases even in the early stages. For example, AI-assisted diagnosis of breast cancer has significant advantages over those without AI assistance. It helps radiologists act as a second interpreter during data interpretation and patient screening. According to the American Cancer Society, it also reduces false-positive diagnosis rates, eliminating the need for unnecessary biopsy and lowering medical expenses[30]. It can finish reviewing and reporting the findings in just a few seconds. Although innovative methods have been established to diagnose and distinguish breast cancer, none of those methods could identify all cancer patients.
Clinical decision assistance systems are computer-guided programs that assist clinicians in their decision-making based on patient clinical data and updated knowledge[31]. AI is a powerful tool that lowers the medical error rate and improves healthcare consistency and efficacy.
The trend of AI application in clinical decision assistance is rising tremendously. For example, the case number of the COVID-19 global pandemic has overcome current medical facilities and obligated the clinical professionals, patients, and families to make crucial determinations based on limited information and within a short time. ML methods have been previously applied to assist in making clinical decisions. There is currently a demand for ML-supported decisions based on acquired vital signs, laboratory data, prescription orders, and complications from caring for previous patients. In clinical practice, AI-related precision medicine can predict patients' most suitable treatment protocols based on different patient characteristics and the treatment context[32]. AI can also make individualized treatment protocols for patients based on the large-scale database and updated information[33]. In addition, it is expected to guide inexperienced hospital frontline and healthcare providers to perform appropriately with ample evidence under emergent situations[34].
The popularity of smartphones and monitoring instruments has brought new access to digital data transfer to medical institutions. Using digital medical records also empowers the AI to monitor patient health status[29]. Through AI, patients with chronic diseases could be better informed about their health and stay connected with their health caregivers. Furthermore, AI-assisted home health monitoring instruments and techniques help low functioning and elderly patients to keep connected to assure that emergency medical technicians can immediately provide first aid when needed[35].
AI systems are also capable of following patient prognosis. For example, the National Institutes of Health has created the AiCure app to monitor medication used by patients. Moreover, those with hypertension or diabetes could benefit from AI’s ability to track their health status through its clinically validated sensors and devices, effectively driving self-management[35]. Technology applications and apps boost more suitable actions in individuals and push one to follow a healthier lifestyle. In other words, it puts people in control of their health and well-being.
Many governments use AI to plan medical resource allocation and provide social care services. AI could connect individual patients with suitable healthcare providers who could satisfy their needs based on their allocated medical budget.
Furthermore, AI could also design a specific treatment protocol and suggest more effective resource use for every patient[36]. For example, clinicians could identify potential risk factors associated with obesity using statistics, ML, and data visualization methods. AI systems can generate automated, personalized, contextual, and behavioral recommendations for obese patients during body weight control, including the suggestion of bariatric surgery, if indicated[37].
Shi et al[38] and Shi et al[39] used an artificial neural network model for predicting the 5-year mortality after surgery for hepatocellular carcinoma using the administrative claims data obtained from the Taiwan Bureau of National Health Insurance (BNHI). Their studies demonstrated that surgeon volume was the most crucial factor influencing 5-year mortality, followed by hospital volume and Charlson co-morbidity index. These parameters could be addressed in preoperative and postoperative healthcare consultations to educate the patients for better recovery and prognosis after hepatocellular carcinoma surgery. In addition, the government could also adjust the policy of healthcare resource allocation in hepatocellular carcinoma surgery with the aid of the AI-empowered analysis results of the BNHI database.
Clinicians could use AI to analyze rare and exceptional cases from large and complex databases faster and more precisely than previously[40]. AI could also search for related scientific studies and information from the literature and combine different data to aid in medical progress[41]. In clinical trials, inappropriate patient selection and recruiting techniques, paired with ineffective patient monitoring and coaching could lead to high trial failure rates. AI can transform the critical steps of a clinical trial design, from study preparation to execution, to improve the trial success rates, thus lowering the cost burden of the research units[42]. It is expected to select the most precise patient data for relevant clinical studies and establish a database with a large population for more studies in the future.
Kiely et al[43] applied real-world data to screen for idiopathic pulmonary arterial hypertension, and the initial report was published in 2019. Their initial AI analysis algorithm has been used to provide a lower-cost screening at a significant population level, facilitate earlier diagnosis, and improve diagnostic rates and patient outcomes.
There was no reliably effective vaccine or specific drug invented for COVID-19 until the end of September 2020. Specialists have proposed several vaccines and drugs for COVID-19 by utilizing AI-based approaches. For example, the Harvard T.H. Chan School of Public Health and the Human Vaccines Project declared that they are using AI models to accelerate vaccine development by utilizing state-of-the-art techniques in epidemiology, immune monitoring, and network biology to explain effective immunity in older populations[44,45].
Nowadays, many medical and health-related institutions use AI to assist in the early detection of infectious disease outbreaks and sources of epidemics[46]. Moreover, AI could also forecast adverse drug reactions, which causes about 6.5% of hospital admissions in the UK[47]. This indicates that AI could use big data analytic methods to assist in public health policy development.
When AI applications are deployed mainly in high-income countries, their use in low-income regions remains relatively nascent. However, AI systems in such low-income countries could support healthcare management in several ways. First, medical expert systems can assist clinicians in disease diagnosis and treatment plan selection, as performed in developed countries. AI could act as a human clinician in initial disease diagnosis in poor communities if one is not readily available. The sick could then be transferred to a suitable institution with the relevant medical resources. Furthermore, AI has already been used to forecast the disease model and delay its spread in epidemic situations worldwide, even in resource-poor regions[48].
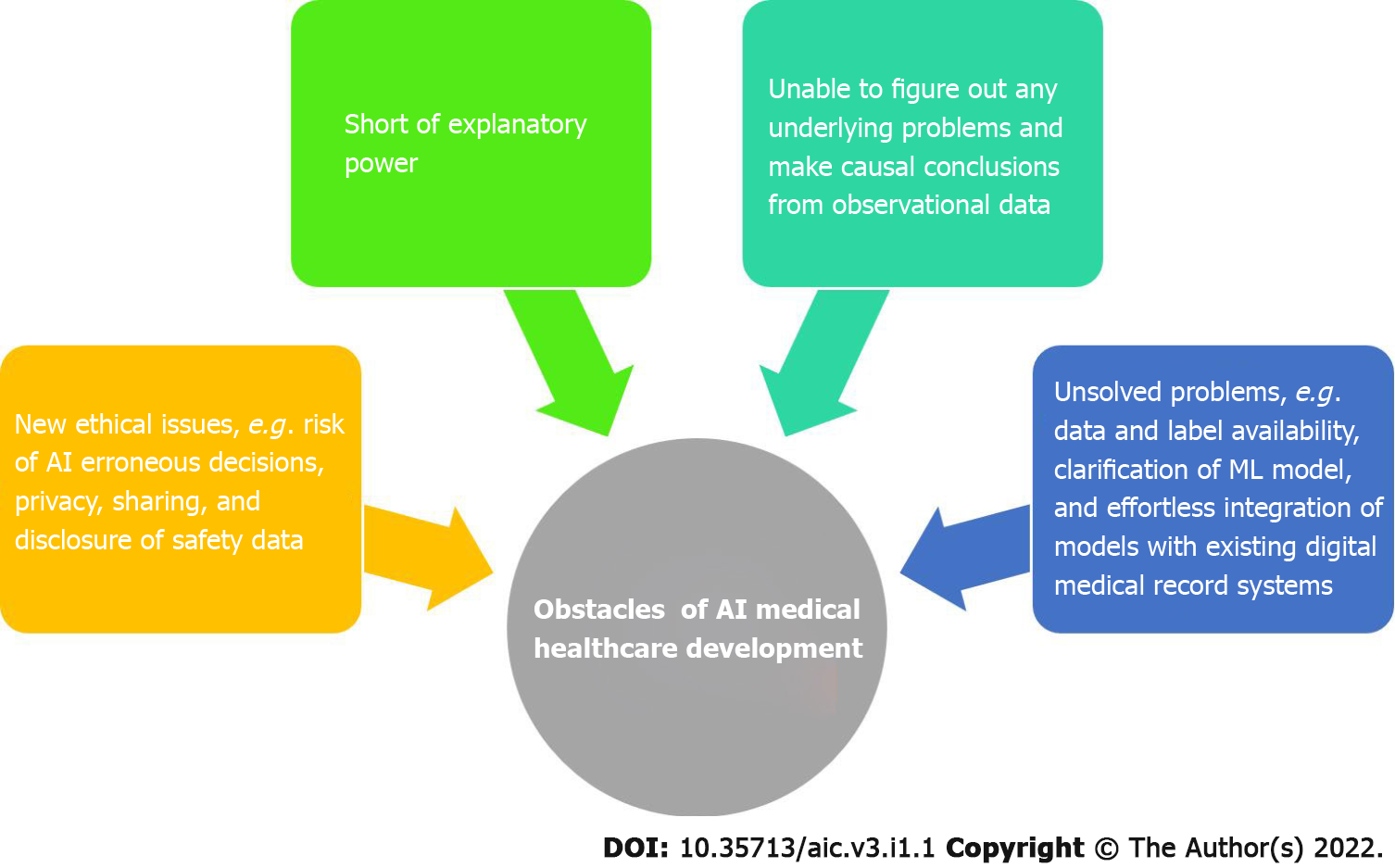
Deep learning is short in explanatory power; deep neural networks cannot interpret how a diagnosis is made, and prejudice characteristics are difficult to identify[7]. This means that ML cannot determine underlying problems and is unable to make causal conclusions from observational data. Algorithms are efficient in outcome prediction, but predictors are not causes[49]. Furthermore, there are still problems that need to be solved, such as data and label availability, clarification of the ML model, and effortless integration of these models with existing digital medical record systems[50].
With the advent of AI development, new ethical issues have also been encountered after it intervened in medical practice, e.g., risk of erroneous decisions by AI, responsibility of using AI in support decision-making, difficulties in confirmation of AI outputs, constitutive data biases in AI system training, sensitive data security crisis, assurance of public trust in AI medical interventions, and the possibility of AI being used for malicious goals[51]. Among these issues, privacy, sharing, and disclosure of safety data relating to AI applications must be strengthened and solved first (Figure 4).
AI cannot replace the clinician’s role in healthcare because it intrinsically lacks articulation and cannot generate insights[4]. However, AI could assuredly assist in making better clinical decisions and even provide more accurate judgment in specific healthcare fields[52]. ML has already alleviated much of the workload of radiologists and anatomical pathologists in many medical institutions due to its massive imaging database, accompanied by advanced innovation in computer vision. With rapid progress in AI performance, machine accuracy can overcome that of humans[53]. The expanding availability of healthcare databases and the fast progression of big data analytic methods have led to the success and popularity of AI applications in the healthcare field. In addition, powerful AI techniques can discover new clinical information hidden in the extensive database, further assisting clinical decision-making[54-56]. However, there are no universally applicable healthcare rules. AI must be complemented with clinician confirmation in many instances. Furthermore, the clinician-patient relationship is guided by associative thinking and could affect real-life treatment decisions. The impact of psychosocial and emotional factors on disease prognosis falls outside the AI scope, which should always be considered. Thus, most AI experts believe that a blend of human experience and digital augmentation should be the natural settling point for AI in healthcare (Table 1).
| Human factors | AI factors |
| Clinicians could regard their patient as a fellow mortal, vulnerable being and gain detailed knowledge of the patient's disease related to their lives | AI continually coordinates new knowledge and perfects itself more rapidly than humans do |
| Clinicians know about social relationships and norms and could establish a genuinely intimate and empathetic connection with their patients | Automation of routine work could save time, such as documentation, administrative reporting, or even triaging images |
| The clinician-patient relationship could be guided by human associative thinking and affect real-life treatment strategies | AI could provide reliable diagnosis and treatment strategies, issue reminders for medication, provide precise analytics for pathology and images, and predict overall health according to the current medical database and patient information |
| The impact of psychosocial and emotional factors on disease prognosis and patient compliance could benefit from a good and close clinician-patient relationships | AI could provide simple mental health assistance via chatbot, monitor patient health, and predict disease progression |
Clinical medicine always requires professional staff to manage enormous amounts of data, from patient physiologic information to laboratory and imaging results. The capability of this complex management has separated excellent clinicians from others. AI has been regarded as an essential tool for clinicians in their daily practice. The increased application of AI technologies does not lower the value of face-to-face interaction with patients. On the contrary, because of AI, it is expected that clinicians would move toward the tasks that uniquely need social skills such as empathy, persuasion, and big-picture integration. Integrating the human clinician’s 'hardware' with the AI’s 'software' could provide an ideal healthcare delivery that exceeds what either could do alone. Perhaps the experts who refuse to apply AI technology in their clinical practice would be regarded as non-professional in the next decade.
Provenance and peer review: Invited article; externally peer reviewed.
Peer-review model: Single blind
Specialty type: Health care sciences and services
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Dabbakuti JRKKK, Hanada E, Wang P S-Editor: Liu JH L-Editor: Webster JR P-Editor: Liu JH
| 1. | Laï MC, Brian M, Mamzer MF. Perceptions of artificial intelligence in healthcare: findings from a qualitative survey study among actors in France. J Transl Med. 2020;18:14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 150] [Cited by in RCA: 115] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 2. | Ahuja AS. The impact of artificial intelligence in medicine on the future role of the physician. PeerJ. 2019;7:e7702. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 153] [Cited by in RCA: 281] [Article Influence: 46.8] [Reference Citation Analysis (0)] |
| 3. | The Lancet. Artificial intelligence in health care: within touching distance. Lancet. 2017;390:2739. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 69] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 4. | Ellahham S, Ellahham N, Simsekler MCE. Application of Artificial Intelligence in the Health Care Safety Context: Opportunities and Challenges. Am J Med Qual. 2020;35:341-348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 33] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 5. | Davenport T, Kalakota R. The potential for artificial intelligence in healthcare. Future Healthc J. 2019;6:94-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1432] [Cited by in RCA: 1124] [Article Influence: 187.3] [Reference Citation Analysis (0)] |
| 6. | Char DS, Shah NH, Magnus D. Implementing Machine Learning in Health Care - Addressing Ethical Challenges. N Engl J Med. 2018;378:981-983. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 793] [Cited by in RCA: 651] [Article Influence: 93.0] [Reference Citation Analysis (0)] |
| 7. | Tarassenko L, Watkinson P. Artificial intelligence in health care: enabling informed care. Lancet. 2018;391:1260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Ramesh AN, Kambhampati C, Monson JR, Drew PJ. Artificial intelligence in medicine. Ann R Coll Surg Engl. 2004;86:334-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 310] [Cited by in RCA: 390] [Article Influence: 18.6] [Reference Citation Analysis (0)] |
| 9. | He J, Baxter SL, Xu J, Zhou X, Zhang K. The practical implementation of artificial intelligence technologies in medicine. Nat Med. 2019;25:30-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 597] [Cited by in RCA: 947] [Article Influence: 157.8] [Reference Citation Analysis (0)] |
| 10. | Harvey HB, Gowda V. How the FDA Regulates AI. Acad Radiol. 2020;27:58-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 57] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 11. | Shahid N, Rappon T, Berta W. Applications of artificial neural networks in health care organizational decision-making: A scoping review. PLoS One. 2019;14:e0212356. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 346] [Cited by in RCA: 149] [Article Influence: 24.8] [Reference Citation Analysis (0)] |
| 12. | Schmidhuber J. Deep learning in neural networks: an overview. Neural Netw. 2015;61:85-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9280] [Cited by in RCA: 3955] [Article Influence: 359.5] [Reference Citation Analysis (0)] |
| 13. | Hosny A, Parmar C, Quackenbush J, Schwartz LH, Aerts HJWL. Artificial intelligence in radiology. Nat Rev Cancer. 2018;18:500-510. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1552] [Cited by in RCA: 1848] [Article Influence: 264.0] [Reference Citation Analysis (2)] |
| 14. | Vial A, Stirling D, Field M, Ros M, Ritz C, Carolan M, Holloway L, Miller AA. The role of deep learning and radiomic feature extraction in cancer-specific predictive modelling: a review. Transl Cancer Res. 2018;7:803-816. [RCA] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 73] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 15. | Nadkarni PM, Ohno-Machado L, Chapman WW. Natural language processing: an introduction. J Am Med Inform Assoc. 2011;18:544-551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 514] [Cited by in RCA: 508] [Article Influence: 39.1] [Reference Citation Analysis (0)] |
| 16. | Murff HJ, FitzHenry F, Matheny ME, Gentry N, Kotter KL, Crimin K, Dittus RS, Rosen AK, Elkin PL, Brown SH, Speroff T. Automated identification of postoperative complications within an electronic medical record using natural language processing. JAMA. 2011;306:848-855. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 207] [Cited by in RCA: 235] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 17. | Chapman WW, Christensen LM, Wagner MM, Haug PJ, Ivanov O, Dowling JN, Olszewski RT. Classifying free-text triage chief complaints into syndromic categories with natural language processing. Artif Intell Med. 2005;33:31-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 76] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 18. | Seto E, Leonard KJ, Cafazzo JA, Barnsley J, Masino C, Ross HJ. Developing healthcare rule-based expert systems: case study of a heart failure telemonitoring system. Int J Med Inform. 2012;81:556-565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 52] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 19. | Hughes CA, Gose EE, Roseman DL. Overcoming deficiencies of the rule-based medical expert system. Comput Methods Programs Biomed. 1990;32:63-71. [PubMed] [DOI] [Full Text] |
| 20. | Kulikowski CA. Beginnings of Artificial Intelligence in Medicine (AIM): Computational Artifice Assisting Scientific Inquiry and Clinical Art - with Reflections on Present AIM Challenges. Yearb Med Inform. 2019;28:249-256. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 63] [Cited by in RCA: 48] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 21. | Rassweiler JJ, Autorino R, Klein J, Mottrie A, Goezen AS, Stolzenburg JU, Rha KH, Schurr M, Kaouk J, Patel V, Dasgupta P, Liatsikos E. Future of robotic surgery in urology. BJU Int. 2017;120:822-841. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 126] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 22. | Wang P, Su YJ, Jia CY. Current surgical practices of robotic-assisted tissue repair and reconstruction. Chin J Traumatol. 2019;22:88-92. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 23. | Saglam R, Muslumanoglu AY, Tokatlı Z, Caşkurlu T, Sarica K, Taşçi Aİ, Erkurt B, Süer E, Kabakci AS, Preminger G, Traxer O, Rassweiler JJ. A new robot for flexible ureteroscopy: development and early clinical results (IDEAL stage 1-2b). Eur Urol. 2014;66:1092-1100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 94] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 24. | Grewal D, Motyka D, Levy M. The evolution and future of retailing and retailing education. J Mark Educ. 2018;40:85-93. [DOI] [Full Text] |
| 25. | Hussain A, Malik A, Halim MU, Ali AM. The use of robotics in surgery: a review. Int J Clin Pract. 2014;68:1376-1382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 81] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 26. | Willis M, Duckworth P, Coulter A, Meyer ET, Osborne M. The Future of Health Care: Protocol for Measuring the Potential of Task Automation Grounded in the National Health Service Primary Care System. JMIR Res Protoc. 2019;8:e11232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 27. | Islam MM, Poly TN, Alsinglawi B, Lin LF, Chien SC, Liu JC, Jian WS. Application of Artificial Intelligence in COVID-19 Pandemic: Bibliometric Analysis. Healthcare (Basel). 2021;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 21] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 28. | Khan M, Mehran MT, Haq ZU, Ullah Z, Naqvi SR, Ihsan M, Abbass H. Applications of artificial intelligence in COVID-19 pandemic: A comprehensive review. Expert Syst Appl. 2021;185:115695. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 65] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 29. | Rieke N, Hancox J, Li W, Milletarì F, Roth HR, Albarqouni S, Bakas S, Galtier MN, Landman BA, Maier-Hein K, Ourselin S, Sheller M, Summers RM, Trask A, Xu D, Baust M, Cardoso MJ. The future of digital health with federated learning. NPJ Digit Med. 2020;3:119. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 608] [Cited by in RCA: 682] [Article Influence: 136.4] [Reference Citation Analysis (0)] |
| 30. | Sadoughi F, Kazemy Z, Hamedan F, Owji L, Rahmanikatigari M, Azadboni TT. Artificial intelligence methods for the diagnosis of breast cancer by image processing: a review. Breast Cancer (Dove Med Press). 2018;10:219-230. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 38] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 31. | Montani S, Striani M. Artificial Intelligence in Clinical Decision Support: a Focused Literature Survey. Yearb Med Inform. 2019;28:120-127. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 72] [Cited by in RCA: 54] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 32. | Lee SI, Celik S, Logsdon BA, Lundberg SM, Martins TJ, Oehler VG, Estey EH, Miller CP, Chien S, Dai J, Saxena A, Blau CA, Becker PS. A machine learning approach to integrate big data for precision medicine in acute myeloid leukemia. Nat Commun. 2018;9:42. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 113] [Cited by in RCA: 143] [Article Influence: 20.4] [Reference Citation Analysis (0)] |
| 33. | Reddy S, Fox J, Purohit MP. Artificial intelligence-enabled healthcare delivery. J R Soc Med. 2019;112:22-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 150] [Article Influence: 21.4] [Reference Citation Analysis (0)] |
| 34. | Debnath S, Barnaby DP, Coppa K, Makhnevich A, Kim EJ, Chatterjee S, Tóth V, Levy TJ, Paradis MD, Cohen SL, Hirsch JS, Zanos TP; Northwell COVID-19 Research Consortium. Machine learning to assist clinical decision-making during the COVID-19 pandemic. Bioelectron Med. 2020;6:14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 60] [Cited by in RCA: 43] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 35. | Hazarika I. Artificial intelligence: opportunities and implications for the health workforce. Int Health. 2020;12:241-245. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 63] [Cited by in RCA: 67] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 36. | Whitelaw S, Mamas MA, Topol E, Van Spall HGC. Applications of digital technology in COVID-19 pandemic planning and response. Lancet Digit Health. 2020;2:e435-e440. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 625] [Cited by in RCA: 372] [Article Influence: 74.4] [Reference Citation Analysis (0)] |
| 37. | Chatterjee A, Gerdes MW, Martinez SG. Identification of Risk Factors Associated with Obesity and Overweight-A Machine Learning Overview. Sensors (Basel). 2020;20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 82] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 38. | Shi HY, Lee KT, Wang JJ, Sun DP, Lee HH, Chiu CC. Artificial neural network model for predicting 5-year mortality after surgery for hepatocellular carcinoma: a nationwide study. J Gastrointest Surg. 2012;16:2126-2131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 24] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 39. | Shi HY, Lee KT, Lee HH, Ho WH, Sun DP, Wang JJ, Chiu CC. Comparison of artificial neural network and logistic regression models for predicting in-hospital mortality after primary liver cancer surgery. PLoS One. 2012;7:e35781. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 84] [Cited by in RCA: 79] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 40. | Brasil S, Pascoal C, Francisco R, Dos Reis Ferreira V, Videira PA, Valadão AG. Artificial Intelligence (AI) in Rare Diseases: Is the Future Brighter? Genes (Basel). 2019;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 69] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 41. | O'Mara-Eves A, Thomas J, McNaught J, Miwa M, Ananiadou S. Using text mining for study identification in systematic reviews: a systematic review of current approaches. Syst Rev. 2015;4:5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 308] [Cited by in RCA: 308] [Article Influence: 30.8] [Reference Citation Analysis (0)] |
| 42. | Harrer S, Shah P, Antony B, Hu J. Artificial Intelligence for Clinical Trial Design. Trends Pharmacol Sci. 2019;40:577-591. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 256] [Article Influence: 42.7] [Reference Citation Analysis (0)] |
| 43. | Kiely DG, Doyle O, Drage E, Jenner H, Salvatelli V, Daniels FA, Rigg J, Schmitt C, Samyshkin Y, Lawrie A, Bergemann R. Utilising artificial intelligence to determine patients at risk of a rare disease: idiopathic pulmonary arterial hypertension. Pulm Circ. 2019;9:2045894019890549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 34] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 44. | Kaushik AC, Raj U. AI-driven drug discovery: A boon against COVID-19? AI Open. 2020;1:1-4. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 45. | Shinde GR, Kalamkar AB, Mahalle PN, Dey N, Chaki J, Hassanien AE. Forecasting Models for Coronavirus Disease (COVID-19): A Survey of the State-of-the-Art. SN Comput Sci. 2020;1:197. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 194] [Cited by in RCA: 101] [Article Influence: 20.2] [Reference Citation Analysis (0)] |
| 46. | Doshi R, Falzon D, Thomas BV, Temesgen Z, Sadasivan L, Migliori GB, Raviglione M. Tuberculosis control, and the where and why of artificial intelligence. ERJ Open Res. 2017;3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (1)] |
| 47. | Jamal S, Goyal S, Shanker A, Grover A. Predicting neurological Adverse Drug Reactions based on biological, chemical and phenotypic properties of drugs using machine learning models. Sci Rep. 2017;7:872. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 62] [Cited by in RCA: 34] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 48. | Wahl B, Cossy-Gantner A, Germann S, Schwalbe NR. Artificial intelligence (AI) and global health: how can AI contribute to health in resource-poor settings? BMJ Glob Health. 2018;3:e000798. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 170] [Cited by in RCA: 231] [Article Influence: 33.0] [Reference Citation Analysis (0)] |
| 49. | Kleinberg J, Ludwig J, Mullainathan S, Obermeyer Z. Prediction Policy Problems. Am Econ Rev. 2015;105:491-495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 234] [Cited by in RCA: 83] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 50. | Goldstein BA, Navar AM, Pencina MJ, Ioannidis JP. Opportunities and challenges in developing risk prediction models with electronic health records data: a systematic review. J Am Med Inform Assoc. 2017;24:198-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 392] [Cited by in RCA: 501] [Article Influence: 55.7] [Reference Citation Analysis (0)] |
| 51. | Gerke S, Minssen T, Cohen G. Ethical and legal challenges of artificial intelligence-driven healthcare. Artificial Intelligence in Healthcare. 2020;295-336. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 102] [Cited by in RCA: 227] [Article Influence: 45.4] [Reference Citation Analysis (0)] |
| 52. | Jiang F, Jiang Y, Zhi H, Dong Y, Li H, Ma S, Wang Y, Dong Q, Shen H. Artificial intelligence in healthcare: past, present and future. Stroke Vasc Neurol. 2017;2:230-243. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1189] [Cited by in RCA: 1407] [Article Influence: 175.9] [Reference Citation Analysis (0)] |
| 53. | Obermeyer Z, Emanuel EJ. Predicting the Future - Big Data, Machine Learning, and Clinical Medicine. N Engl J Med. 2016;375:1216-1219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1493] [Cited by in RCA: 1625] [Article Influence: 180.6] [Reference Citation Analysis (0)] |
| 54. | Murdoch TB, Detsky AS. The inevitable application of big data to health care. JAMA. 2013;309:1351-1352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1052] [Cited by in RCA: 794] [Article Influence: 66.2] [Reference Citation Analysis (0)] |
| 55. | Kolker E, Özdemir V, Kolker E. How Healthcare Can Refocus on Its Super-Customers (Patients, n = 1) and Customers (Doctors and Nurses) by Leveraging Lessons from Amazon, Uber, and Watson. OMICS. 2016;20:329-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 56. | Dilsizian SE, Siegel EL. Artificial intelligence in medicine and cardiac imaging: harnessing big data and advanced computing to provide personalized medical diagnosis and treatment. Curr Cardiol Rep. 2014;16:441. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 222] [Cited by in RCA: 193] [Article Influence: 17.5] [Reference Citation Analysis (0)] |