Published online Oct 28, 2021. doi: 10.13105/wjma.v9.i5.455
Peer-review started: March 30, 2021
First decision: July 30, 2021
Revised: August 14, 2021
Accepted: October 20, 2021
Article in press: October 20, 2021
Published online: October 28, 2021
Processing time: 211 Days and 18.7 Hours
Severe acute respiratory syndrome coronavirus-2 is a novel coronavirus strain that causes pneumonia and acute respiratory distress syndrome along with other morbidities, collectively known as coronavirus disease 2019 (COVID-19) disease. There has been widespread discussion about the psychological impact of COVID-19 particularly on children and adolescents. There have been overarching negative effects with regards to decreased physical activity, more screen time, increasingly unhealthy diets, and irregularities in sleep/wake schedules. This, coupled with disruptions in ongoing mental health treatment and associated support structures, has caused unprecedented declines in the emotional and psychosocial wellbeing of children and adolescents. This review aims to systematically review the literature to provide a general overview of the ways in which COVID-19 has affected common psychiatric illnesses in children and adolescents. The included articles in all subsections concluded that symptoms of these common childhood psychiatric disorders have generally been exacerbated by the COVID-19 pandemic. This review indicates that quarantine and the consequent isolation have had multiple significant and consistent negative implications on the mental health of children and adolescents. Our study indicates that there should be increased vigilance among providers and families to mitigate the negative psychological effects that the COVID-19 pandemic has on children with common childhood psychiatric disorders.
Core Tip: The included articles in all subsections concluded that symptoms of these common childhood psychiatric disorders have generally been exacerbated by the coronavirus disease 2019 (COVID-19) pandemic. Our study indicates that there should be increased vigilance among pediatricians and families to mitigate the negative psychological effects that the COVID-19 pandemic has on children with common childhood psychiatric disorders. This calls out for pediatricians, psychiatrists, and all providers alike to remain cognizant of these effects and work collaboratively towards measures to reduce the psychological impact of COVID-19.
- Citation: Balaram K, Ahmed M, Marwaha R. Review of the effects of SARS-CoV2 infection and COVID-19 on common pediatric psychiatric illnesses. World J Meta-Anal 2021; 9(5): 455-461
- URL: https://www.wjgnet.com/2308-3840/full/v9/i5/455.htm
- DOI: https://dx.doi.org/10.13105/wjma.v9.i5.455
Severe acute respiratory syndrome coronavirus-2 (SARS-CoV2), is a novel coronavirus strain that causes pneumonia and acute respiratory distress syndrome along with other morbidities, collectively known as coronavirus disease 2019 (COVID-19) disease[1]. The World Health Organization declared SARS-CoV2 infection to be a global pandemic in March 2020. As of February 2021, there are upwards of 110 million cases of SARS-CoV2 infection worldwide with over 28 million cases and 500000 total deaths documented in the United States. In addition to significant medical impact, there has also been a profound psychologic impact because of the pandemic, particularly among vulnerable populations. There has been widespread discussion about the psychological impact of COVID-19 particularly on children and adolescents[2].
Since the start of the pandemic, the transition to online-based education, increasing school closures, and the alteration of normal adolescent social activities have caused an unmitigated disruption in the lives of children[2]. In general, the greatest impacts appear to be losses in areas of daily routine, institutional support structures, and social connection[2]. Though these effects are generally attributed to the cessation of in-person learning in schools, it is generally assumed that there have been overarching detrimental effects with regards to decreased physical activity, more TV and screen time, increasingly unhealthy diets, and irregularities in sleep/wake schedules[2].
This, coupled with disruptions in ongoing mental health treatment and associated support structures, has caused unprecedented declines in the emotional and psychosocial wellbeing of children and adolescents[2].
This review aims to systematically review the literature to provide a general overview of the ways in which COVID-19 has affected common psychiatric illnesses in children and adolescents.
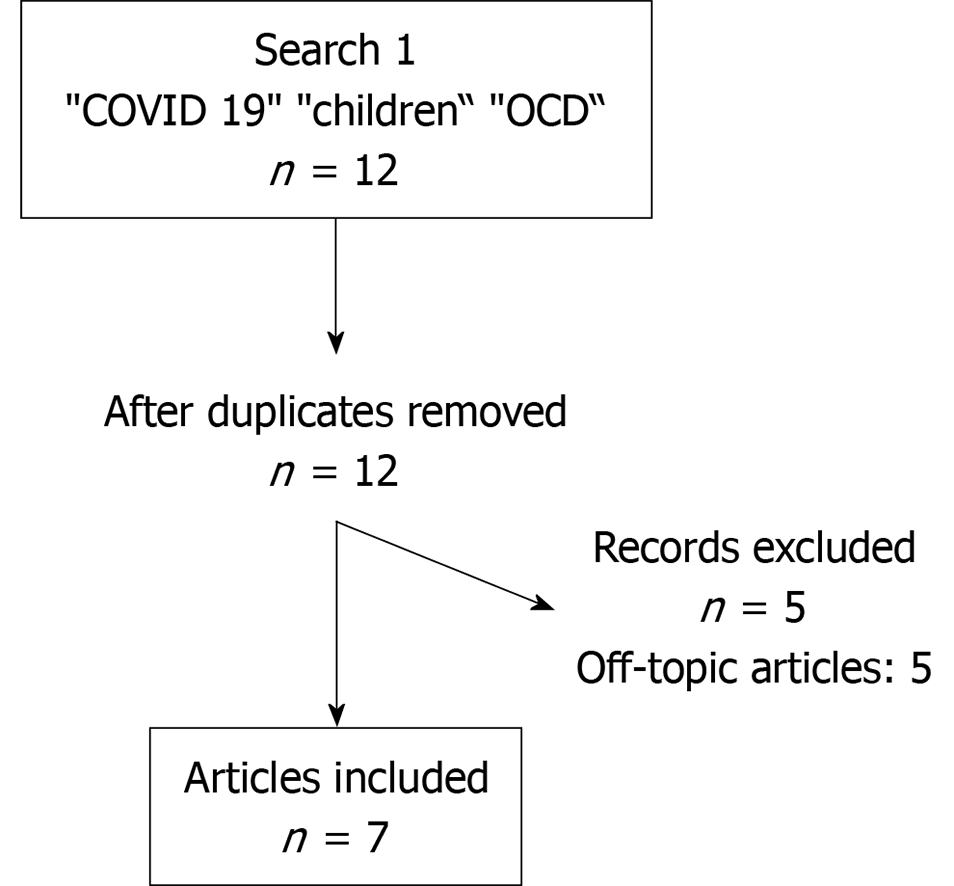
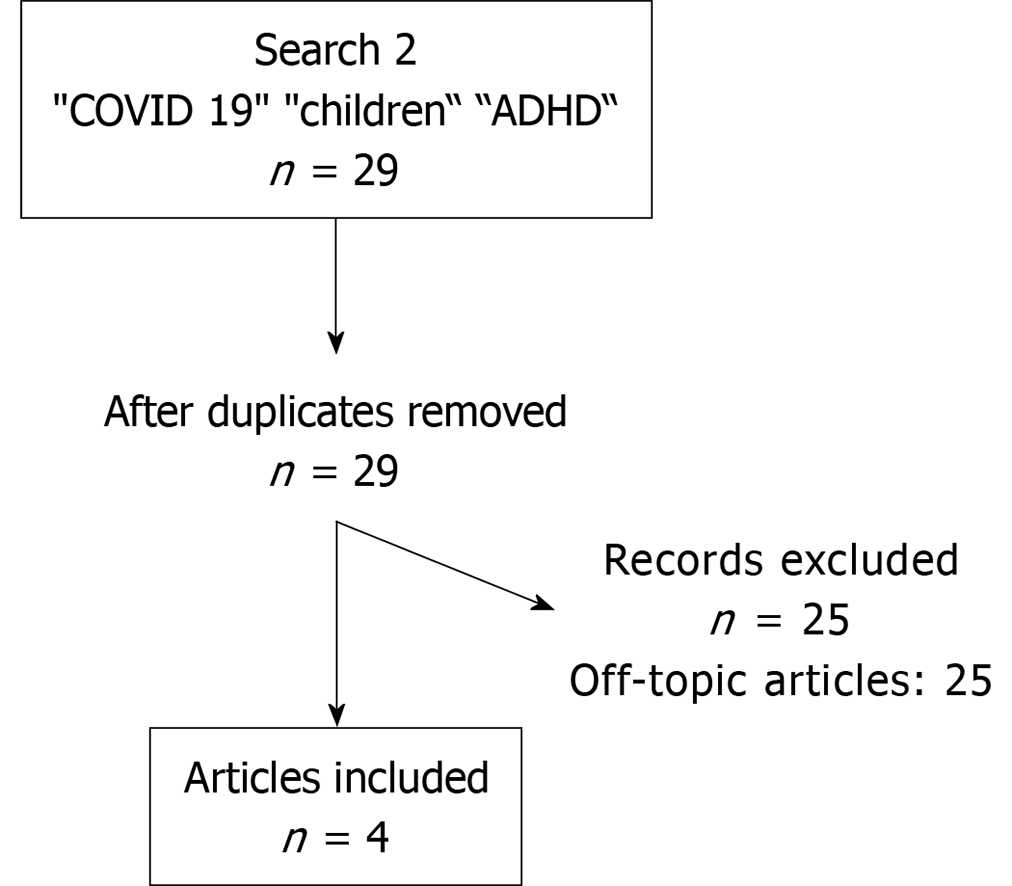
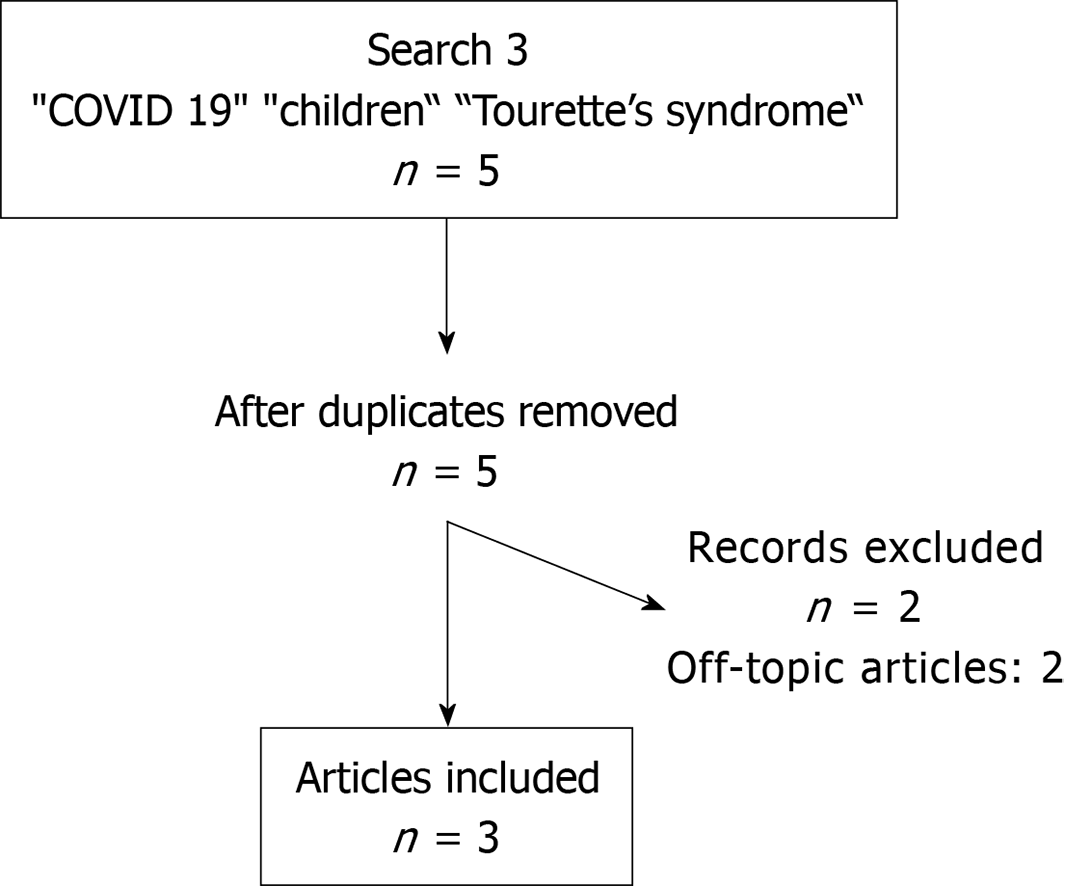
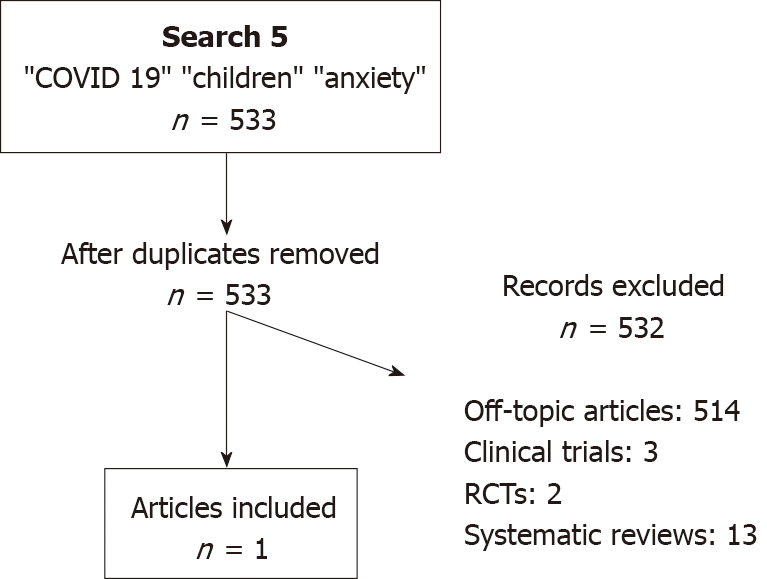
For this review, we performed multiple literature searches of PubMed, Cochrane and PsycInfo to find articles (Figures 1-5). The first search used the keywords "COVID 19," "children," and "OCD," the second search used the keywords "COVID 19," "children," and "ADHD," the third search used the keywords "COVID 19," "children," and "Tourette’s syndrome,” the fourth search used the keywords "COVID 19," "children," and "depression," and the fifth search used the keywords "COVID 19," "children," and "anxiety.” The search was not initially restricted by study design or language but was limited to articles published between January 1 to December 31, 2020. Review articles published in or translated to English were included. Full-text references cited in these articles were also researched for additional relevant studies. The inclusion criteria were on-topic articles discussing the effect of COVID-19 on common pediatric psychiatric disorders. The exclusion criteria were any study designs that were case reports, surveys, or study protocols, or articles that were considered to be off topic.
A total of 12 articles were identified through a literature search. There were no clinical trials, randomized controlled trials or meta-analysis that were identified. After excluding articles that were off-topic, seven articles remained for inclusion (Figure 1).
Though the mean age of onset for those with obsessive-compulsive disorder (OCD) is 19.5 years, childhood onset does occur and generally persists throughout adulthood[3]. According to the diagnostic and statistical manual of mental disorders, 5th edition, 25% of males have onset of symptoms before age 10. Characterized by obsessions and compulsions, OCD can present with a varying combination of symptoms including intrusive and persistent unwanted thoughts, repetitive checking, fears of contamination, feelings of worry and disgust, and repetitive behaviors or patterns of behaviors that an individual is compelled to perform[4,5]. In general, symptoms of OCD are exacerbated by acute stressors, such as trauma.
Due to the COVID-19 pandemic, children and adolescents who are susceptible to OCD are most likely to be affected[6]. There were several studies that concluded that children and adolescents diagnosed with OCD experienced a considerable worsening of their symptoms[6-10]. One particular study concluded that this significant worsening was most prevalent in those with an earlier age of symptom onset and in those with a family history of attention deficit hyperactivity disorder (ADHD)[7]. Another study also identified a substantial increase in contamination fears and cleaning or washing obsessions due to general fears of exposure to infection brought on by the pandemic[8,9]. Contrastingly, there has also been widespread advocacy of infection control measures, such as frequent handwashing, and dissemination of information on avoiding exposure/contamination. These measures may actually lead to those suffering from severe OCD symptoms to feel less stigmatization over their cleansing obsessions[9,10]. They may instead feel more acceptance over their symptoms, as their fears become well-founded and “real” and their ritualized behaviors became generally widespread and even encouraged[9,10]. Therapeutic interventions, such as cognitive behavioral therapy, are designed to achieve symptomatic relief by targeting behaviors like excessive hand washing and intrusive thoughts of contamination. This can lead to a cognitive dissonance in those with OCD as the COVID-19 pandemic has led to a widespread and public campaign to encourage these behaviors.
A total of 29 articles were identified through a literature search. There were no clinical trials, randomized controlled trials or meta-analysis that were identified. After excluding articles that were off-topic, four articles remained for inclusion (Figure 2).
ADHD, characterized by persistent patterns of inattention and/or hyperac
A total of five articles were identified through a literature search. There were no clinical trials, randomized controlled trials or meta-analysis that were identified. After excluding articles that were off-topic, three articles remained for inclusion (Figure 3).
Public health measures aimed at controlling the spread of the COVID-19 pandemic have led to some changes in the symptomatic presentation of Tourette’s disorder[15-17]. The advent of online learning and social distancing measures have decreased the social burden of tics, and resulting psychological distress, felt by children in school and other learning environments[16]. In contrast, several other non-obscene socially inappropriate tics - such as spitting, coughing, sneezing, or inability to maintain interpersonal distance with touching – have become more socially unacceptable[15]. This can lead to increased anxiety and distress in children with these symptoms who may feel undue pressure to modify or control these behaviors[15]. This increased anxiety can lead to a secondary increase in tic symptoms[15]. In general, children with Tourette’s disorder were observed to have overall clinical decline with either a worsening of existing symptoms or a resurgence of previously-controlled symptoms[15-17].
A total of 378 articles were identified through a literature search by using the keywords “COVID,” “depression,” and “children.” There were two clinical trials, two meta-analysis, and eleven systematic reviews. There were no randomized controlled trials that were identified. The clinical trials were excluded as they were off topic. The systematic reviews were excluded due to the overlap from within the meta-analyses. After excluding articles that were off-topic, two meta-analyses remained for inclusion (Figure 4).
A total of 533 articles were identified through a literature search by using the keywords “COVID,” “anxiety,” and “children.” There were three clinical trials, four meta-analysis, two randomized controlled trials, and thirteen systematic reviews. The clinical trials were excluded as they were off topic. The randomized controlled trials were excluded as they were not pertinent to the population subgroup of our review and dealt with the ailments in the adult population. The systematic reviews were excluded due to the overlap from within the meta-analyses. After excluding articles that were off-topic, one meta-analysis remained for inclusion (Figure 5).
Both anxiety and depression are major ailments amongst the youth that are often under-reported and under-recognized. Data by SAMHSA, or the Substance Abuse and Mental Health Services Administration, shows that the overall prevalence of depression for adolescents aged 12 to 18 is 13.1% as opposed to 7.1% for adults. Similarly, the rates are 31.9% and 19.1% when it comes to anxiety amongst adolescents, and adults respectively. This means that the relative prevalence of these disorders already remains higher amongst the adolescents as compared to adults.
COVID-19 and its consequent effects have further negatively impacted the mental health of children and adolescents. Multiple studies have shown that social isolation and the resultant loneliness were associated with increased risk of both depression and anxiety[18-25]. Anxiety was seen to be more prevalent amongst children maintaining quarantine, and this was thought to be likely mostly due to loss of primary caregiver’s job, financial instability leading to a dearth in provision of basic amenities[22]. It was also noted that the time period of isolation was more important for symptomatology of mental health ailments than the severity of isolation[23].
The studies noted certain interesting factors. There was seen to be a mild difference between the sexes as well, with loneliness being more strongly associated with social anxiety in boys and depression in girls[23]. Certain primary school students who viewed COVID-19 as a serious disease had increased anxiety and somatic symptoms[2]. One study mentioned that children who practiced social distancing for fear of getting infected were predisposed to anxiety disorders. The same study also mentioned that children who engaged in social distancing secondary to peer pressure had a higher likelihood of depression[24]. This illustrates a thought-provoking difference in symptoms based upon the motivator for social distancing in the first place. Interestingly an age-related difference was also discernible in certain study populations. High school children reported higher number and severity of symptoms of anxiety and depression as compared to their primary and middle school counterparts[24,25]. Certain salient causes of increased depression levels in the study population were also noticed such as internet/smartphone addiction and affected friends/family members in the past.
On the contrary a few of the factors protective towards depression were lesser time spent on the internet, adequate coping mechanisms, increased exercise time, and having a sibling[19,20]. It should come as no surprise that the pandemic meant more children/adolescents, and adults alike ended up spending increased time on the internet and lesser time outdoors. Similarly, children and adolescents with worry and fear about COVID-19 had higher rates of depression, whereas remaining optimistic amidst these times had the opposite effect[2].
The included articles in all subsections concluded that symptoms of these common childhood psychiatric disorders have generally been exacerbated by the COVID-19 pandemic. This was primarily attributed to the restricting quarantining regulations and the public fear of SARS-CoV2 infection. For instance, the routine learning schedule implemented at public schools that had helped to provide structure to children with ADHD have been lost while quarantining at home. This in turn led to worsening ADHD symptoms and behaviors. The public fear of COVID-19 and the widespread encouragement of frequent handwashing have both exacerbated contamination fears in those with OCD experience and worsened repetitive sanitizing behaviors. While children with Tourette’s Disorder may have experienced less psychosocial distress over their tics by being away from school, they may still face difficulties with controlling symptoms because of increased anxiety over their tic behaviors breaking social-distancing rules.
This review portends that quarantine and the consequent isolation have had multiple significant and consistent negative implications on the mental health of children and adolescents. The stigmata of these consequences can be detected even months later beyond quarantine[25]. In general, a lack of vigilance and treatment for pandemic-associated effects on childhood psychiatric disorders may propagate significantly negative and refractory long-term sequelae into adulthood. Our study indicates that there should be increased vigilance among clinicians and families to mitigate the negative psychological effects that the COVID-19 pandemic has on children with common childhood psychiatric disorders. This calls for pediatricians, psychiatrists, and all healthcare providers alike to remain cognizant of these effects and work collaboratively towards measures to reduce the psychological impact of this already menacing physical ailment.
Manuscript source: Invited manuscript
Specialty type: Psychiatry
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Bianchi F S-Editor: Liu M L-Editor: A P-Editor: Liu M
| 1. | Coronavirus Update (Live). 111200037 Cases and 2461503 Deaths from COVID-19 Virus Pandemic – Worldometer. 2021 Feb 28 [cited 28 February 2021]. Available from: https://www.worldometers.info/coronavirus. |
| 2. | Nearchou F, Flinn C, Niland R, Subramaniam SS, Hennessy E. Exploring the Impact of COVID-19 on Mental Health Outcomes in Children and Adolescents: A Systematic Review. Int J Environ Res Public Health. 2020;17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 183] [Cited by in RCA: 320] [Article Influence: 64.0] [Reference Citation Analysis (0)] |
| 3. | American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington D.C., 2013. |
| 4. | Bokor G, Anderson PD. Obsessive-compulsive disorder. J Pharm Pract. 2014;27:116-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 41] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 5. | Ji G, Wei W, Yue KC, Li H, Shi LJ, Ma JD, He CY, Zhou SS, Zhao Z, Lou T, Cheng J, Yang SC, Hu XZ. Effects of the COVID-19 Pandemic on Obsessive-Compulsive Symptoms Among University Students: Prospective Cohort Survey Study. J Med Internet Res. 2020;22:e21915. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 58] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 6. | Darvishi E, Golestan S, Demehri F, Jamalnia S. A Cross-Sectional Study on Cognitive Errors and Obsessive-Compulsive Disorders among Young People During the Outbreak of Coronavirus Disease 2019. Act Nerv Super (2007). 2020;1-6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 7. | Nissen JB, Højgaard DRMA, Thomsen PH. The immediate effect of COVID-19 pandemic on children and adolescents with obsessive compulsive disorder. BMC Psychiatry. 2020;20:511. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 59] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 8. | Tanir Y, Karayagmurlu A, Kaya İ, Kaynar TB, Türkmen G, Dambasan BN, Meral Y, Coşkun M. Exacerbation of obsessive compulsive disorder symptoms in children and adolescents during COVID-19 pandemic. Psychiatry Res. 2020;293:113363. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 88] [Cited by in RCA: 107] [Article Influence: 21.4] [Reference Citation Analysis (0)] |
| 9. | Schwartz-Lifshitz M, Basel D, Lang C, Hertz-Palmor N, Dekel I, Zohar J, Gothelf D. Obsessive compulsive symptoms severity among children and adolescents during COVID-19 first wave in Israel. J Obsessive Compuls Relat Disord. 2021;28:100610. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 10. | Jelinek L, Moritz S, Miegel F, Voderholzer U. Obsessive-compulsive disorder during COVID-19: Turning a problem into an opportunity? J Anxiety Disord. 2021;77:102329. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 60] [Cited by in RCA: 67] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 11. | McGrath J. ADHD and Covid-19: current roadblocks and future opportunities. Ir J Psychol Med. 2020;37:204-211. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 40] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 12. | Shah R, Raju VV, Sharma A, Grover S. Impact of COVID-19 and Lockdown on Children with ADHD and Their Families-An Online Survey and a Continuity Care Model. J Neurosci Rural Pract. 2021;12:71-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 50] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 13. | Bobo E, Lin L, Acquaviva E, Caci H, Franc N, Gamon L, Picot MC, Pupier F, Speranza M, Falissard B, Purper-Ouakil D. How do children and adolescents with Attention Deficit Hyperactivity Disorder (ADHD) experience lockdown during the COVID-19 outbreak? Encephale. 2020;46:S85-S92. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 72] [Cited by in RCA: 91] [Article Influence: 18.2] [Reference Citation Analysis (0)] |
| 14. | Cortese S, Asherson P, Sonuga-Barke E, Banaschewski T, Brandeis D, Buitelaar J, Coghill D, Daley D, Danckaerts M, Dittmann RW, Doepfner M, Ferrin M, Hollis C, Holtmann M, Konofal E, Lecendreux M, Santosh P, Rothenberger A, Soutullo C, Steinhausen HC, Taylor E, Van der Oord S, Wong I, Zuddas A, Simonoff E; European ADHD Guidelines Group. ADHD management during the COVID-19 pandemic: guidance from the European ADHD Guidelines Group. Lancet Child Adolesc Health. 2020;4:412-414. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 118] [Cited by in RCA: 138] [Article Influence: 27.6] [Reference Citation Analysis (0)] |
| 15. | Robertson MM, Eapen V, Rizzo R, Stern JS, Hartmann A. Gilles de la Tourette Syndrome: advice in the times of COVID-19. F1000Res. 2020;9:257. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 16. | Graziola F, Garone G, Di Criscio L, Grasso M, Curatolo P, Vigevano F, Capuano A. Impact of Italian lockdown on Tourette's syndrome patients at the time of the COVID-19 pandemic. Psychiatry Clin Neurosci. 2020;74:610-612. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 17. | Conte G, Baglioni V, Valente F, Chiarotti F, Cardona F. Adverse Mental Health Impact of the COVID-19 Lockdown in Individuals With Tourette Syndrome in Italy: An Online Survey. Front Psychiatry. 2020;11:583744. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 18. | Panda PK, Gupta J, Chowdhury SR, Kumar R, Meena AK, Madaan P, Sharawat IK, Gulati S. Psychological and Behavioral Impact of Lockdown and Quarantine Measures for COVID-19 Pandemic on Children, Adolescents and Caregivers: A Systematic Review and Meta-Analysis. J Trop Pediatr. 2021;67. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 240] [Cited by in RCA: 358] [Article Influence: 71.6] [Reference Citation Analysis (0)] |
| 19. | Duan L, Shao X, Wang Y, Huang Y, Miao J, Yang X, Zhu G. An investigation of mental health status of children and adolescents in china during the outbreak of COVID-19. J Affect Disord. 2020;275:112-118. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 471] [Cited by in RCA: 542] [Article Influence: 108.4] [Reference Citation Analysis (0)] |
| 20. | Hou TY, Mao XF, Dong W, Cai WP, Deng GH. Prevalence of and factors associated with mental health problems and suicidality among senior high school students in rural China during the COVID-19 outbreak. Asian J Psychiatr. 2020;54:102305. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 59] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 21. | Pisano L, Galimi D, Cerniglia L. A qualitative report on exploratory data on the possible emotional/behavioral correlates of Covid-19 Lockdown in 4-10 years children in Italy. 2020 Preprint. Available from: PsyArxiv. [DOI] [Full Text] |
| 22. | Saurabh K, Ranjan S. Compliance and Psychological Impact of Quarantine in Children and Adolescents due to Covid-19 Pandemic. Indian J Pediatr. 2020;87:532-536. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 199] [Cited by in RCA: 209] [Article Influence: 41.8] [Reference Citation Analysis (1)] |
| 23. | Loades ME, Chatburn E, Higson-Sweeney N, Reynolds S, Shafran R, Brigden A, Linney C, McManus MN, Borwick C, Crawley E. Rapid Systematic Review: The Impact of Social Isolation and Loneliness on the Mental Health of Children and Adolescents in the Context of COVID-19. J Am Acad Child Adolesc Psychiatry. 2020;59:1218-1239.e3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1638] [Cited by in RCA: 1366] [Article Influence: 273.2] [Reference Citation Analysis (0)] |
| 24. | Oosterhoff B, Palmer CA, Wilson J, Shook N. Adolescents' Motivations to Engage in Social Distancing During the COVID-19 Pandemic: Associations With Mental and Social Health. J Adolesc Health. 2020;67:179-185. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 237] [Cited by in RCA: 259] [Article Influence: 51.8] [Reference Citation Analysis (0)] |
| 25. | Imran N, Aamer I, Sharif MI, Bodla ZH, Naveed S. Psychological burden of quarantine in children and adolescents: A rapid systematic review and proposed solutions. Pak J Med Sci. 2020;36:1106-1116. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 104] [Cited by in RCA: 103] [Article Influence: 20.6] [Reference Citation Analysis (0)] |