Published online Jul 31, 2019. doi: 10.13105/wjma.v7.i7.350
Peer-review started: April 22, 2019
First decision: June 10, 2019
Revised: June 13, 2019
Accepted: July 26, 2019
Article in press: July 26, 2019
Published online: July 31, 2019
Processing time: 102 Days and 19.1 Hours
Recurrent Clostridium difficile infection (CDI) in children can be difficult to manage and may represent an unidentified underlying pathology. Recurrence can be frequently encountered in immunodeficiency disorders and inflammatory bowel disease (IBD).
To report cases of a select population of children with recurrent CDI who are immunocompetent and do not have an identified IBD and examine the potential for any underlying risk factors, disease course and disease outcome.
Review of charts for children aged 1-21 years with recurrent CDI referred to see pediatric gastroenterology service was performed. All subjects with known immunosuppression or IBD were excluded. Subjects were followed for at least 24 mo.
Twelve children seen consecutively were identified. All patients were treated with antibiotic courses for CDI prior to their referral. Five out of 12 patients had an underlying pathology that was not previously identified, including eosinophilic colitis and IBD. CDI symptoms resolved after treatment of underlying colitis without the need to target therapy for CDI. There were 9 patients that failed antibiotic treatment of CDI and required fecal microbiome transplant, which was safe and highly effective in preventing recurrence (100% efficacy). The gut microbial changes after fecal transplant were characterized by a remarkable and durable increase in diversity and in abundance of Bacteroides.
Pediatric patients with frequent recurrence of CDI may have an unidentified underlying gastrointestinal pathology that may warrant further investigation by a specialist who can identify these diseases and help optimize management. Many of these children may benefit from fecal microbial transplant which appears to be a safe, highly effective therapy that results in long term changes in the gut microbiome.
Core tip: Children with recurrent Clostridium difficile infection who do not have known immunodeficiency or inflammatory bowel disease deserve a thorough workup as many may have an underlying gastrointestinal disease.
- Citation: Chu A, Michail S. Pediatric recurrent Clostridium difficile infections in immunocompetent children: Lessons learned from case reports of the first twelve consecutive patients. World J Meta-Anal 2019; 7(7): 350-357
- URL: https://www.wjgnet.com/2308-3840/full/v7/i7/350.htm
- DOI: https://dx.doi.org/10.13105/wjma.v7.i7.350
The incidence of Clostridium difficile infections (CDI) in both adults and pediatrics is increasing[1-5]. CDI can result in a spectrum of disorders that ranges from carrier and asymptomatic state to causing significant morbidity and even mortality[6]. Infants frequently test positive but are asymptomatic[7]. Part of the rise in CDI could be from increasing testing among infants, which needs to be done with caution given the high prevalence of asymptomatic colonization in young infants[7]. There is also a higher incidence of colonization and colitis with C. difficile in pediatric inflammatory bowel disease (IBD) compared to adult IBD as well as patients with celiac disease[8].
There have been multiple studies showing correlation between certain risk factors predisposing to the development of CDI. Risk factors such as acid suppressing agents, especially H2 receptor antagonists, exposure to antibiotics and immunosuppressants, comorbidities such as cancer, cystic fibrosis and IBD, and hospitalization have been known to increase the incidence of CDI for some time[1,9]. These studies are charged with the task of understanding the risk for developing the infection in general, however, there is a paucity of studies that describe a select population of children that have recurrence of this infection. While community acquired CDI is more common in pediatrics than adults, recurrent CDI is not common in children[10]. A study by Kociolek in 2015[11] showed an association between recurrent CDI and malignancy and IBD. The study identified thirty children with recurrent infection and demonstrated that the majority of these subjects (19 subjects or 63%) have malignancy, underwent solid organ transplant or have IBD.
In this study, we aimed to understand CDI in a very unique population of children who are not immunocompromised and do not have any identified IBD. This study describes important discoveries of unidentified underlying gastrointestinal conditions which may not be recognized unless the child is adequately evaluated by a specialist in the field. The study also describes the success, and the durable gut microbial changes after fecal microbial transplant in this population. These discoveries contribute to the successful outcome in management of these subjects by identifying and addressing the underlying disease.
Institutional Review Board (IRB) approval was obtained to study pediatric patients with recurrent CDI, defined as two or more distinct episodes of CDI associated with diarrhea or bloody diarrhea who were referred for evaluation to pediatric gastro-enterology service. Subjects younger than one year and older than twenty-one years of age were excluded. All subjects with known immunosuppression or IBD prior to referral were excluded. Subjects had been followed up for at least one year.
The 16S bacterial DNA region from stool DNA and negative controls were amplified by PCR using a shared forward primer 806rB (CAAGCAGAAGACGGCATACGAGATAGTCAGCCAGCCGGACTACNVGGGTWTCTAAT) for all samples, while each sample had its own unique identifying reverse primer, which were modified from the original 515F-806R primer pairs. All samples were pooled and sequenced using custom sequencing primers; R1 (TATGGTAATTGTGTGYCAGCMGCCGCGGTAA), R2 (AGTCAGCCAGCCGGACTACNVGGGTWTCTAAT) and Index (AATGATACGGCGACCACCGAGATCTACACGCT). Paired-end sequencing (2 × 150bp) using Illumina MiSeq Reagent Kit v2 flowcell was performed on an Illumina MiSeq System.
Reads were de-multiplexed using QIIME v1.9.1. Statistical analyses were performed using the “phyloseq” (v1.20.0) package in the R statistical environment.
Twelve consecutive children were identified that fit the criteria described above. Children averaged 7.5 years of age (range 1-17 years). All children were treated with at least one course of metronidazole and one course of enteral vancomycin prior to referral. Nine children were exposed to antibiotic therapy prior to their first CDI. Three children had multiple antibiotic courses including amoxicillin. The most common single antibiotic course prior to CDI was amoxicillin as well. Three children did not receive antimicrobials prior to their first CDI. Two of the three children who did not receive antibiotics prior to their first CDI, were found to have an underlying gastrointestinal disease. The identification of the underlying disease changed the management of these patients. Five of the 12 children were previously healthy. The remaining children had different co-morbidities as described in Table 1 without a known history of colitis or immunodeficiency prior to referral. There were 9 patients that failed antibiotic treatment of CDI and required fecal microbiome transplant (FMT), which ultimately relieved CDI symptoms. Of these nine patients, 4 had a gastrostomy or gastrojejunostomy tube (Table 1), seven had history of antibiotic use, and 3 had history of acid suppressants.
| Age of onset (yr) | Gender | # of CDIs | Medications | Co-morbidities | Devices | Prior hosp | Final diagnosis |
| 8.6 | F | > 5 | PPI, EES, multiple antibiotics course including amoxicillin | DD, BPD | GT | Yes | Eosinophilic colitis |
| 1.17 | M | > 5 | History of ranitidine, multiple antibiotic courses including amoxicillin | 36 wk prematurity, SGA, GERD, cleft lip | GJT | Yes | |
| 7 | M | > 5 | Erythromycin | CP, multiple orthopedic surgeries | GT | Yes | Lactase deficiency |
| 10 | F | 3 | Amoxicillin-clavulanate | None | None | No | |
| 3 | F | > 5 | PPI, multiple antibiotics courses including amoxicillin | DD, renal disease, recurrent pneumonia | GT | Yes | |
| 9 | M | 3 | None | ASD | none | No | IBD proctitis |
| 17 | M | 4 | PPI, clindamycin | CP, DD | GT | Yes | |
| 12 | M | > 5 | None | None | None | No | Eosinophilic esophagitis and lactase deficiency |
| 4 | F | 4 | Amoxicillin-clavulanate | History of UTI, hydronephrosis | None | Yes | |
| 2 | M | 4 | Amoxicillin | None | None | No | Lactase deficiency |
| 2 | M | 3 | None | None | None | No | |
| 14 | F | 3 | Cephalosporin | None | None | Yes |
After a thorough gastrointestinal workup, two patients were found to have eosinophilic disease, one subject had eosinophilic colitis and another subject had eosinophilic esophagitis. The child with eosinophilic colitis was placed exclusively on crystalline amino acid formula which resulted in resolution and prevention of any further CDI even after future exposure to antimicrobial therapy. One patient was found to have IBD proctitis, and CDI resolved after treatment of IBD. There were three subjects diagnosed with lactase deficiency.
One of the children treated with FMT, experienced a change in disease phenotype from C. difficile colitis that required hospitalization for bloody diarrhea with endoscopic confirmation of C. difficile colitis, to an asymptomatic C. difficile colonizer for 12 mo, followed by loss of colonization. No further CDI treatment was required despite the use of antimicrobial therapy for respiratory infection after FMT. From the FMT safety perspective, one subject developed transient fever for one day but was otherwise asymptomatic. Another subject developed bloating on the day of FMT. No serious adverse events were seen related to FMT.
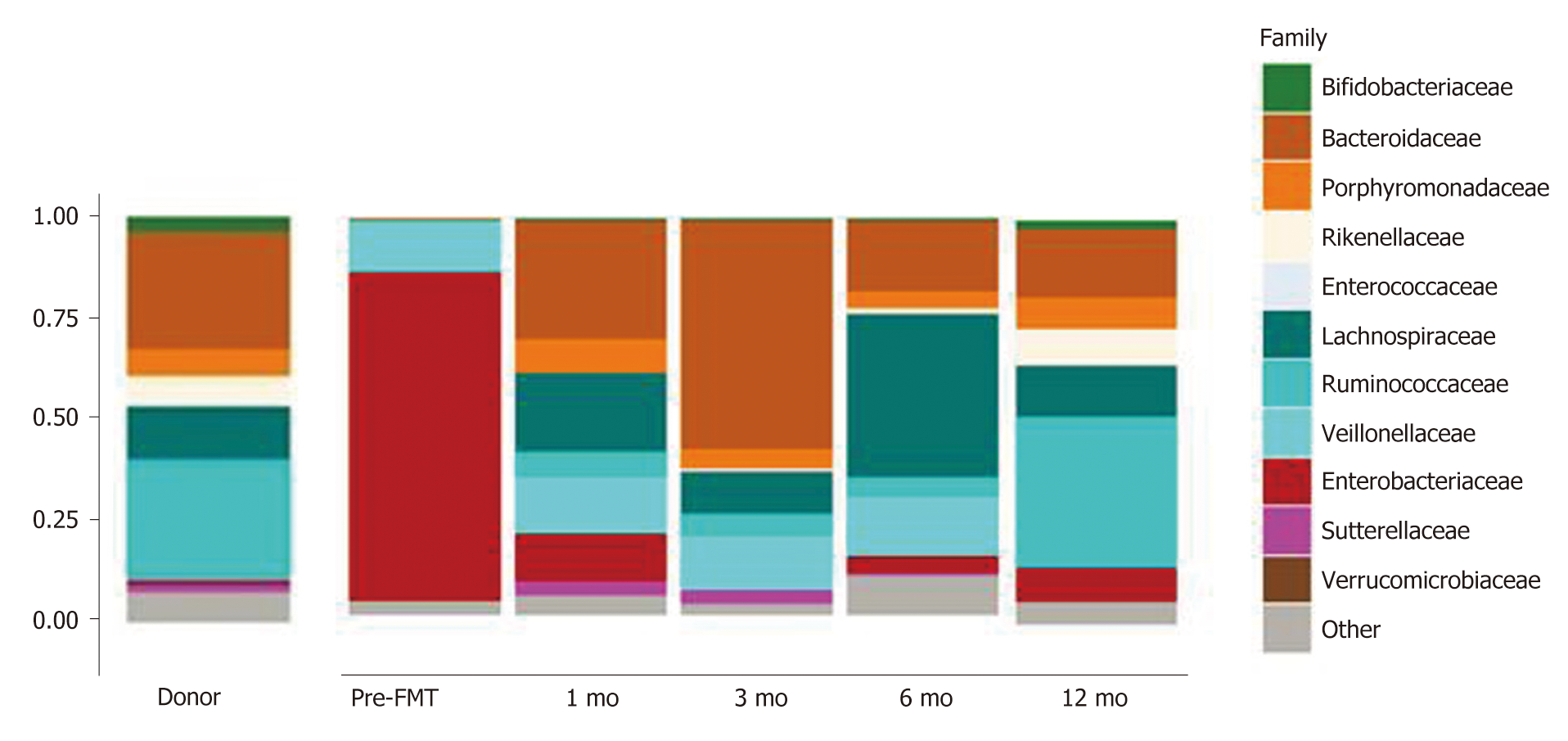
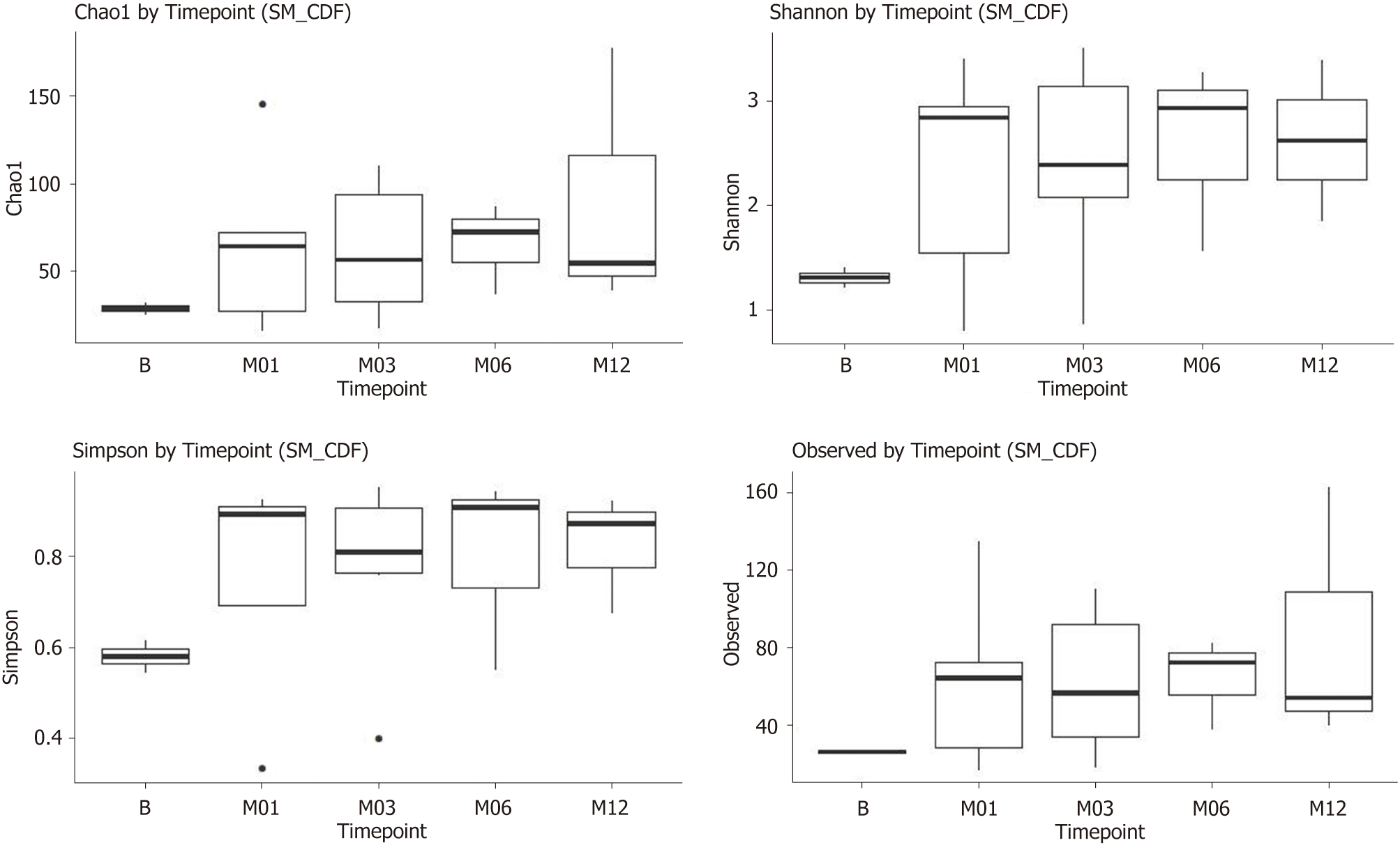
Gut microbial profiles were examined before and after fecal transplant and compared to the donor profile. Children with recurrent CDI had very low abundance of Bacteroidaceae (Figure 1) prior to fecal transplant as well as low diversity of microorganisms compared to healthy donor (1.3 = 0.2 vs 3.2 + 0.4, Shannon diversity index, P = 0.031). After fecal transplant, the fecal microbial profile diversity improved. This phenomenon seemed to be durable for the twelve months following fecal transplant (Figure 2). Similarly, Bacteroidaceae became quite abundant after fecal transplant and this effect was seen over twelve months (Figure 1).
In adults, a recent meta-analysis showed age > 65 years, additional antibiotic use during follow-up, use of proton-pump inhibitors (PPIs), and renal insufficiency were most frequently associated with recurrent CDI[12]. There have been a few pediatric studies that describe risk factors for CDI in pediatric patients as well[1,9,11,13]. Underlying chronic medical condition, recent antibiotic use (specifically cephalosporins as described by Crews et al[13]), acid-suppressing agents, gastrointestinal feeding device, and past or prolonged hospitalization increase the risk of developing CDI in pediatrics[1,9,13]. There is a paucity of data in the literature that focuses on recurrent infections. Kociolek et al[11] described a cohort of children who have recurrent CDI and found that the majority have malignancy or solid organ transplant, or IBD (n = 19, or 63%). Although there have been studies implicating IBD and immunosuppression increasing children’s susceptibility to CDI[4,8], to our knowledge, no studies have directly linked recurrent CDI to undiagnosed underlying gastrointestinal disease.
With regards to antibiotic use in children who developed recurrent CDI, most of the children in our study received amoxicillin therapy, in contrast to the study by Crews et al[13] that showed more exposure to cephalosporins. Most children (two thirds), who did not receive antimicrobials prior to their first CDI were found to have an underlying gastrointestinal disease which was only identified when a work up was performed after referral to specialist. The authors recognize the limitation of the findings due to the small overall number of subjects in this sub-population.
Perhaps over one third of infants younger than 12 mo are colonized with C. difficile[14]. The rate of colonization then drops to 15% between ages 1-8 years and then 5% after age 8 years, similar to the rate in adults[14]. Due to the high rate of colonization in infants, patients under 12 mo of age were excluded from this study.
Five of the twelve children in our cohort had a gastrostomy or a jejunostomy feeding tube, which are known to be associated with an increased risk of acquiring C. difficile, in adults and children[14-16]. This is likely due to spore contamination of equipment or formula, or use of formula that promotes C. difficile growth in the gut[14,15,17]. Most of the children in our study have been hospitalized in the past, which again would expose them to an environment that could harbor C. difficile spores and increasing their risk of acquiring C. difficile[14,18].
While there are many medical conditions known to predispose pediatric patients to CDI, such as hematopoietic stem cell transplant, IBD, cancer, fungal infections, and human immunodeficiency virus infection[14], those co-morbidities are diagnosed prior to the onset of CDI. In our study, 5 out of 12 patients had underlying pathology that was not previously identified. There have been many single study reports of other medical conditions that are associated with CDI[14], such as cystic fibrosis[19], Hirschsprung’s[20], and Henoch-Schonlein purpura[21]. In our study, two patients had eosinophilic disease, which has not been described in prior studies as an association or risk factor for CDI. The discovery and treatment of an underlying colitis, namely eosinophilic colitis and IBD proctitis, resulted in prompt resolution of the recurrence of CDI.
Three of the twelve subjects were diagnosed with lactase deficiency by disaccharidase assay. Since there is overlap in symptoms with CDI and lactase deficiency, namely diarrhea and abdominal pain, the discovery and treatment of lactase deficiency allowed optimizing management and more appropriate assignment of symptoms to the correct underlying disease. However, as expected, management of lactase deficiency did not result in resolution of CDI recurrence. FMT in both subjects resulted in prompt resolution of symptoms.
All the subjects receiving FMT had resolution of symptoms for at least one year. One subject became an asymptomatic colonizer of C. difficile after FMT. The colonization was seen for 12 mo followed by resolution of colonization.
FMT in this patient population appeared to be highly effective and safe. Fecal transplant resulted in improved gut microbial diversity and abundance of Bacteroides, which appeared to be durable and seen to persist for at least twelve months. The overall numbers are small and more research will be necessary to confirm these observations.
In this subset population, it is recommended that children with recurrent CDI who do not have immunodeficiency or identified IBD be evaluated by a provider who can investigate the presence of an underlying gastrointestinal disease. In about one third of these subjects, a gastrointestinal disorder may be discovered that can impact the management of recurrent infection.
In conclusion, there are likely risk factors that are still unknown that can predispose to CDI. Pediatric patients that have more than one episode of CDI recurrence have an increased likelihood of underlying gastrointestinal pathology especially if there has been no prior use of antimicrobials and should be investigated so that proper treatment can be offered. Fecal microbial transplant is a highly effective and safe therapy for these children and results in durable changes in the gut microbiome.
Childhood recurrent Clostridium difficile infections (CDI) may be difficult to control and may represent an unknown underlying pathology. Recurrence often occurs in immunodeficiency disorders and inflammatory bowel disease (IBD).
There have been multiple studies showing correlation between certain risk factors predisposing to the development of CDI. Risk factors such as acid suppressing agents, especially H2 receptor antagonists, exposure to antibiotics and immunosuppressants, comorbidities such as cancer, cystic fibrosis and IBD, and hospitalization have been known to increase the incidence of CDI for some time. These studies are charged with the task of understanding the risk for developing the infection in general, however, there is a paucity of studies that describe a select population of children that have recurrence of this infection. While community acquired CDI is more common in pediatrics than adults, recurrent CDI is not common in children.
The main objectives of this report are understanding CDI in a very unique population of children who are not immunocompromised and do not have any identified IBD. This study describes important discoveries of unidentified underlying gastrointestinal conditions which may not be recognized unless the child is adequately evaluated by a specialist in the field. The study also describes the success, and the durable gut microbial changes after fecal microbial transplant in this population. These discoveries contribute to the successful outcome in management of these subjects by identifying and addressing the underlying disease.
Pediatric patients with recurrent CDI, defined as two or more distinct episodes of CDI associated with diarrhea or bloody diarrhea who were referred for evaluation to pediatric gastro-enterology service were identified. Subjects younger than one year and older than twenty-one years of age were excluded. All subjects with known immunosuppression or IBD prior to referral were excluded. Subjects had been followed up for at least one year.
We have observed 12 children in succession. All patients received CDI antibiotics prior to referral. Five of the 12 patients had previously undiscovered potential pathologies, including eosinophilic colitis and IBD. After the treatment of basal colitis, the symptoms of CDI disappear and there is no need for CDI treatment. Nine patients required fecal microbial transplantation for antibiotic CDI failure, which is safe and effective (100% efficacy) for preventing recurrence. Intestinal microbial changes following fecal transplantation are characterized by a significant and sustained increase in diversity and the abundance of Bacteroides.
Children with recurrent CDI deserve a through gastrointestinal workup as they may frequently have an underlying disease which can contribute to the management of the condition. When medical therapy fails in this population, fecal microbial transplant is a safe and durable therapy. Children with recurrent CDI may have unidentified gastrointestinal disease contributing to the recurrence of the infection. Children with recurrent clostridium difficile frequently have an unidentified gastrointestinal disorder, which when identified and addressed, can help with management of clostridium difficile recurrence.
Children with recurrent CDI need a thorough gastrointestinal workup to optimize their care and management. Future research should focus on individualized medicine and targeting underlying disease on a case by case basis.
Manuscript source: Unsolicited Manuscript
Specialty type: Medicine, research and experimental
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Matowicka-Karna J, Trifan A S-Editor: Dou Y L-Editor: A E-Editor: Liu JH
| 1. | Brown KE, Knoderer CA, Nichols KR, Crumby AS. Acid-Suppressing Agents and Risk for Clostridium difficile Infection in Pediatric Patients. Clin Pediatr (Phila). 2015;54:1102-1106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 2. | Deshpande A, Pant C, Anderson MP, Donskey CJ, Sferra TJ. Clostridium difficile infection in the hospitalized pediatric population: increasing trend in disease incidence. Pediatr Infect Dis J. 2013;32:1138-1140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 44] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 3. | Pant C, Deshpande A, Gilroy R, Olyaee M, Donskey CJ. Rising Incidence of Clostridium difficile Related Discharges among Hospitalized Children in the United States. Infect Control Hosp Epidemiol. 2016;37:104-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 4. | Nylund CM, Goudie A, Garza JM, Fairbrother G, Cohen MB. Clostridium difficile infection in hospitalized children in the United States. Arch Pediatr Adolesc Med. 2011;165:451-457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 143] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 5. | Khanna S, Baddour LM, Huskins WC, Kammer PP, Faubion WA, Zinsmeister AR, Harmsen WS, Pardi DS. The epidemiology of Clostridium difficile infection in children: a population-based study. Clin Infect Dis. 2013;56:1401-1406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 170] [Cited by in RCA: 165] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 6. | Davidovics ZH, Michail S, Nicholson MR, Kociolek LK, Pai N, Hansen R, Schwerd T, Maspons A, Shamir R, Szajewska H, Thapar N, de Meij T, Mosca A, Vandenplas Y, Kahn SA, Kellermayer R; and the FMT Special Interest Group of the North American Society of Pediatric Gastroenterology Hepatology, Nutrition, the European Society for Pediatric Gastroenterology Hepatology, Nutrition. Fecal Microbiota Transplantation for Recurrent Clostridium difficile Infection and Other Conditions in Children: A Joint Position Paper From the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition. J Pediatr Gastroenterol Nutr. 2019;68:130-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 89] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 7. | Sammons JS, Toltzis P. Pitfalls in Diagnosis of Pediatric Clostridium difficile Infection. Infect Dis Clin North Am. 2015;29:465-476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 8. | Hourigan SK, Chirumamilla SR, Ross T, Golub JE, Rabizadeh S, Saeed SA, Elson CO, Kelly CP, Carroll KC, Oliva-Hemker M, Sears C. Clostridium difficile carriage and serum antitoxin responses in children with inflammatory bowel disease. Inflamm Bowel Dis. 2013;19:2744-2752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 60] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 9. | Samady W, Pong A, Fisher E. Risk factors for the development of Clostridium difficile infection in hospitalized children. Curr Opin Pediatr. 2014;26:568-572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | McFarland LV, Ozen M, Dinleyici EC, Goh S. Comparison of pediatric and adult antibiotic-associated diarrhea and Clostridium difficile infections. World J Gastroenterol. 2016;22:3078-3104. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 120] [Cited by in RCA: 107] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 11. | Kociolek LK, Palac HL, Patel SJ, Shulman ST, Gerding DN. Risk Factors for Recurrent Clostridium difficile Infection in Children: A Nested Case-Control Study. J Pediatr. 2015;167:384-389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 12. | Deshpande A, Pasupuleti V, Thota P, Pant C, Rolston DD, Hernandez AV, Donskey CJ, Fraser TG. Risk factors for recurrent Clostridium difficile infection: a systematic review and meta-analysis. Infect Control Hosp Epidemiol. 2015;36:452-460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 177] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 13. | Crews JD, Anderson LR, Waller DK, Swartz MD, DuPont HL, Starke JR. Risk Factors for Community-associated Clostridium difficile-associated Diarrhea in Children. Pediatr Infect Dis J. 2015;34:919-923. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 14. | Pant C, Deshpande A, Altaf MA, Minocha A, Sferra TJ. Clostridium difficile infection in children: a comprehensive review. Curr Med Res Opin. 2013;29:967-984. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 37] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 15. | Bliss DZ, Johnson S, Savik K, Clabots CR, Willard K, Gerding DN. Acquisition of Clostridium difficile and Clostridium difficile-associated diarrhea in hospitalized patients receiving tube feeding. Ann Intern Med. 1998;129:1012-1019. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 233] [Cited by in RCA: 204] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 16. | Yokohama S, Aoshima M, Asama T, Shindo J, Maruyama J. Clostridium difficile-associated enteric disease after percutaneous endoscopic gastrostomy. J Gastroenterol. 2009;44:121-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | O'Keefe SJ. Tube feeding, the microbiota, and Clostridium difficile infection. World J Gastroenterol. 2010;16:139-142. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 59] [Cited by in RCA: 58] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 18. | Morinville V, McDonald J. Clostridium difficile-associated diarrhea in 200 Canadian children. Can J Gastroenterol. 2005;19:497-501. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 50] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 19. | Pohl JF, Patel R, Zobell JT, Lin E, Korgenski EK, Crowell K, Mackay MW, Richman A, Larsen C, Chatfield BA. Clostridium difficile Infection and Proton Pump Inhibitor Use in Hospitalized Pediatric Cystic Fibrosis Patients. Gastroenterol Res Pract. 2011;2011:345012. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 20. | Thomas DF, Fernie DS, Bayston R, Spitz L, Nixon HH. Enterocolitis in Hirschsprung's disease: a controlled study of the etiologic role of Clostridium difficile. J Pediatr Surg. 1986;21:22-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 48] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 21. | Boey CC, Ramanujam TM, Looi LM. Clostridium difficile-related necrotizing pseudomembranous enteritis in association with Henoch-Schonlein purpura. J Pediatr Gastroenterol Nutr. 1997;24:426-429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 0.5] [Reference Citation Analysis (0)] |