Published online Dec 26, 2017. doi: 10.13105/wjma.v5.i6.167
Peer-review started: August 4, 2017
First decision: September 7, 2017
Revised: September 21, 2017
Accepted: October 29, 2017
Article in press: October 29, 2017
Published online: December 26, 2017
Processing time: 145 Days and 2.8 Hours
To investigate the influence of complete and incomplete revascularization (ICR) in patients with multivessel coronary artery disease undergoing coronary artery bypass or percutaneous coronary intervention.
We searched PubMed using the keywords “complete revascularization”, “incomplete revascularization”, “coronary artery bypass”, and “percutaneous coronary intervention”. We selected randomized controlled studies (RCT) and observational studies only for review. The main outcomes of interest were mortality, myocardial infarction (MI) and repeat revascularization. We identified further studies by hand searching relevant publications and included those that met with the inclusion criteria in our final analysis and performed a systematic review.
Ten studies were identified, including 13327 patients of whom, 8053 received complete revascularization and 5274 received ICR. Relative to ICR, CR was associated with lower mortality (RR: 0.755, 95%CI: 0.66 to 0.864, P = 0.765, I2 = 0.0%), lower rates of MI (RR: 0.759, 95%CI: 0.615 to 0.937, P = 0.091, I2 = 45.1%), lower rates of MACCE (RR: 0.731, 95%CI: 0.668 to 0.8, P = 0.453, I2 = 0.0%) and reduced rates of repeat coronary revascularization (RR: 0.691, 95%CI: 0.541 to 0.883, P = 0.0, I2 = 88.3%).
CR is associated with lower rates of adverse outcomes. CR can be used as a standard in the choice of any particular revascularization strategy.
Core tip: Completeness of revascularization has been documented to have lesser adverse post-operative/post-procedural outcomes as compared to incomplete revascularization (ICR). We conduct a systematic review with meta-analysis to analyze the outcomes in patients undergoing CR vs ICR, using any or both techniques. Ten studies were identified, including 13327 patients of whom, 8053 received CR and 5274 received ICR. CR is associated with lower rates of mortality, MI, repeat coronary revascularization procedures, and MACCE. Sub-group analysis also showed reduced rates of adverse events. CR can be used as an aim for any myocardial revascularization procedure.
- Citation: Auchoybur ML, Chen X. Complete revascularization reduces adverse outcomes in patients with multivessel coronary artery disease. World J Meta-Anal 2017; 5(6): 167-176
- URL: https://www.wjgnet.com/2308-3840/full/v5/i6/167.htm
- DOI: https://dx.doi.org/10.13105/wjma.v5.i6.167
Complete revascularization arose from early studies on coronary artery bypass grafting (CABG) surgery whereby some studies demonstrated that patients who were completely revascularized enjoyed a mortality benefit over those who were incompletely revascularized[1-3]. Data from the coronary artery surgery study (CASS) registry show that patients with multi-vessel coronary artery disease (CAD) and severe angina that received three or more grafts had better survival relative to patients who received one or two grafts[4]. Although CR is often easier to achieve with CABG than with percutaneous coronary intervention (PCI), with recent developments in percutaneous transluminal coronary angioplasty procedures, such as the new era of drug eluting stents (DES), the previous barriers of PCI in the treatment of multi-vessel disease are no longer insurmountable, and favorable outcomes have been recorded across multiple centers using this revascularization approach[5].
Different established standards are used to determine the degree of completeness of revascularization. Conventionally, perfusion districts are divided into three areas according to the supply of the coronary artery branches namely the left anterior descending (LAD), the left circumflex (LCX) and the right coronary artery (RCA). The most commonly used definition across studies is the (1) anatomical definition, and was used in 90% of the studies included in our meta-analysis. According to this definition, CR has been achieved if all diseased arterial segments with a vessel size (greater/equal to 1.5 mm for a graft and 2.0-2.25 mm for a stent) with at least one significant stenosis greater than or equal to 50% receive a graft or a stent. A second definition of CR is (2) numerical whereby the number of distal anastomoses is greater or equal to the number of diseased coronary segments/systems and was used in 10% of the studies included in our meta-analysis. Other definitions include the (3) functional definition whereby all ischemic myocardial territories are grafted (or stented); areas of old infarction with no viable myocardium are not required to be perfused, the (4) score-based definition whereby the stenosis in different vessels is scored and different weights are given to different vessels according to number of myocardial segments supplied (A residual score of 0 is usually considered equivalent to CR) and the (5) physiology-based definition whereby all coronary lesions with fractional flow reserve of less than equal to 0.75-0.80 receive a graft or stent.
Due to procedural difficulties associated with each technique (CABG and PCI), complete revascularization is not always achieved. Previous studies have tried to assess the outcomes following incomplete revascularization (ICR). However, since there is no specific definition for ICR, which is essentially defined as “failure to achieve complete revascularization”, it lacks objectivity as it relies on post-procedural classification of CR by the treating surgeon/physician. The SYNTAX trial, which used a more accurate method to determine the completeness of revascularization (patients were categorized as incompletely revascularized when the number of diseased segments that were treated did not match the heart team decision), and the BARI trial reported no increase in adverse outcomes in incompletely revascularized patients.
There is discrepancy between the results of different studies concerning the superiority of CR over ICR. In our meta-analysis, we aim to determine whether CR, is associated with improved post-procedural outcomes. In a subgroup analysis, we also investigate the mid/long-term outcomes of CR, along with outcomes in a > 60 years old patient population.
We identified four types of studies on the PubMed database: Randomized controlled trials, observational studies, controlled clinical trials and clinical trials. The study was conducted in March 2016, using the keywords “coronary artery bypass”, “percutaneous coronary intervention”, “complete revascularization”, “incomplete revascularization”. The total number of records identified was fifty-four. We limited our search to the specific above-mentioned study types. Six of these studies met with our inclusion criteria. Through Hand-search (a methodological approach previously validated), we searched through journals related to our subject-matter and identified relevant studies and also searched the latter’s references. An additional four manuscripts were selected using the above-mentioned method[6]. A total of ten studies were included in our final analysis.
We included two types of studies in our meta-analysis, namely randomized controlled trials and observational studies in which: (1) Patients with multi-vessel CAD were enrolled for either CABG or PCI; (2) the outcomes of interest between CR and ICR were compared using any of the definitions of CR (see introduction for definitions of CR used); and (3) the outcomes included the primary outcome of interest and/or the secondary outcomes. We excluded studies in which: (1) multiple grafts were used for treatment of multi-vessel CAD without any reference to CR and/or ICR; (2) PCI was used for the treatment in the setting of ST-elevation acute myocardial infarction (MI); (3) outcomes of interest were not reported unless there was reference to CR and ICR; (4) the patients included were undergoing repeat CABG surgery; and (5) the sample size was small (< 100 patients).
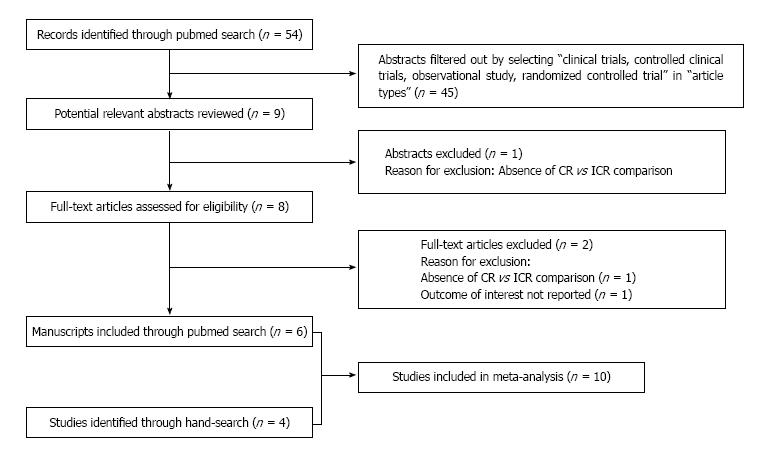
Our initial search using the keywords: Complete revascularization, ICR, coronary artery bypass, PCI yielded fifty-four citations on PubMed. Using the filter for article types, we selected clinical trials, controlled clinical trials, observational studies and randomized controlled trials only. Of the fifty-four citations, nine citations remained, and the abstracts from these nine citations were reviewed. Of these, one abstract was excluded due to absence of comparison between complete and ICR. The remaining eight full text manuscripts were reviewed for eligibility. Of these eight manuscripts, six met with our inclusion criteria. We hand-searched references cited in relevant publications and an additional four manuscripts that fit our inclusion criteria were included. A total of ten studies were selected and included in this meta-analysis (Figure 1).
The data was extracted by Merveesh L Auchoybur using standardized extraction forms. Extracted information included study design, method of revascularization and definition of CR used by each study, follow-up time, patient characteristics pre-operatively, and outcomes relevant to this meta-analysis. The subjects were divided into two groups, namely the complete revascularization group for those subjects who received complete revascularization and the ICR group for those subjects who were not completely revascularized. In studies where complete revascularization through CABG and PCI were reported separately, the sum total of completely revascularized patients was used for the complete revascularization group and the remaining patients were added to the ICR group.
The primary outcome used in this systematic study was all-cause mortality. Secondary outcomes were MI and repeat revascularization. Major adverse cardiovascular and cerebral events were also analyzed where present.
In this meta-analysis, both χ2 based Q-statistic test and I2 test were considered to assess the heterogeneity across studies, and P-value less than or equal to 0.05 was considered significant. I2 is a description of the variation present across studies that is due to heterogeneity instead of chance (I2 value less than 50% indicates no or little heterogeneity)[7]. Weighted relative risk (RR) and its 95% confidence interval were calculated to evaluate the effect size. A fixed effect model using Mantel-Haenszel method were used to combine values from studies when heterogeneity was absent, otherwise, a random-effects model using the DerSimonian and Laird method was used[8]. Egger’s test and inverted funnel plots were utilized to provide a diagnosis of publication bias[9]. Automatic “zero cell” correction was used for studies with no events for a particular outcome. All analyses were performed using Stata version 11.1 software (Stata, College Station, TX, United States). All statistical evaluations were made assuming a two-sided test with a significance level of 0.05, unless stated otherwise.
The list of the ten studies that met with our inclusion criteria are listed in Table 1. Of the studies included, four were RCTs and six were non-RCTs. All the RCTs reported both CABG and PCI as revascularization strategies. Of the six non-RCTs included, three reported PCI, two reported both CABG and PCI simultaneously, and one reported CABG only. Of the studies comprising our analysis, nine use an anatomical definition of CR and one uses a numerical definition of CR. The current analysis includes 13327 patients of whom, 8053 (60.4%) received complete revascularization (CR) and 5274 (39.6%) received ICR. The mean age of the patients undergoing CR was 63.6 years, 20.5% had diabetes mellitus, 39.8% had suffered from previous MI, 43.5% had hypertension (Table 2). The mean age of the patients undergoing ICR was 65.1 years, 22.4% had diabetes mellitus, 46.1% had previously suffered from MI, and 52.6% had hypertension (Table 3). The mean follow-up time of the patients was 4.9 years.
| Ref. | Type of search | Method of revascularization | Study design | Year | Definition of CR used | Follow-up (yr) |
| Bell et al[24] | Hand | PCI | Post hoc analysis, non-RCT | 1990 | Anatomical | 2.2 |
| Approach/catherine Mclellan et al[25] | Hand | PCI | Post hoc analysis, non-RCT | 2005 | Anatomical | 9 |
| ARTS II/Sarno et al[26] | PubMed | CABG/PCI | Post hoc analysis, non-RCT | 2010 | Anatomical | 5 |
| ARTS trial/van den Brand et al[14] | PubMed | CABG/PCI | Post hoc analysis, RCT | 2002 | Anatomical | 1 |
| SYNTAX trial/Farooq et al[27] | PubMed | CABG/PCI | Post hoc analysis, RCT | 2013 | Anatomical | 4 |
| BARI/Bourassa et al[28] | PubMed | CABG/PCI | Post hoc analysis, RCT | 1999 | Anatomical | 5 |
| Bourassa et al[29] | Hand | PTCA | Post hoc analysis, non-RCT | 1998 | Anatomical | 9 |
| Head et al[30] | PubMed | CABG/PCI | Post hoc analysis, RCT | 2012 | Anatomical | 3 |
| BARI 2D/Schwartz et al[31] | PubMed | CABG/PCI | Post hoc analysis, non-RCT | 2012 | Numerical | 5.3 |
| Mohammadi et al[32] | Hand | CABG | Post hoc analysis, non-RCT | 2012 | Anatomical | 5.4 ± 3.0 |
| Ref. | Prevalence of CR (%) | Mean age (yr) | Previous MI | No previous MI | Diabetes | No diabetes | Hypertension | No hypertension |
| Bell et al[24] | 41.0 | 60.0 | 122 | 234 | 46 | 319 | 148 | 217 |
| Approach/catherine Mclellan et al[25] | 66.9 | 62.1 | 802 | 506 | 244.6 | 1063.4 | 725.94 | 582.06 |
| ARTS II/Sarno et al[26] | 72.5 | 61.5 | 149 | 688 | 163 | 674 | 440 | 397 |
| ARTS trial/van den Brand et al[14] | 77.2 | 61.0 | 385 | 498 | 143.93 | 739.07 | - | |
| SYNTAX trial/Farooq et al[27] | 61.8 | 65.3 | 521 | 1088 | 429.6 | 1179.4 | 759.45 | 849.55 |
| BARI/Bourassa et al[28] | 65.4 | 61.3 | 612 | 584 | 204.52 | 991.48 | 578.86 | 617.14 |
| Bourassa et al[29] | 17.4 | 56.6 | 62 | 70 | 15.05 | 116.95 | 55.97 | 76.03 |
| Head et al[30] | 59.9 | 64.9 | 328 | 713 | 300 | 438 | 702 | 356 |
| BARI 2D/Schwartz et al[31] | 37.9 | 61.21 | - | - | - | |||
| Mohammadi et al[32] | 82.1 | 82.1 | 224 | 167 | 107.92 | 283.08 | 286.21 | 104.79 |
| Ref. | Prevalence of CR (%) | Mean age (yr) | Previous MI | No previous MI | Diabetes | No diabetes | Hypertension | No hypertension |
| Bell et al[24] | 41.0 | 60.0 | 122 | 234 | 46 | 319 | 148 | 217 |
| Approach/catherine Mclellan et al[25] | 66.9 | 62.1 | 802 | 506 | 244.6 | 1063.4 | 725.94 | 582.06 |
| ARTS II/Sarno et al[26] | 72.5 | 61.5 | 149 | 688 | 163 | 674 | 440 | 397 |
| ARTS trial/van den Brand et al[14] | 77.2 | 61.0 | 385 | 498 | 143.93 | 739.07 | - | |
| SYNTAX trial/Farooq et al[27] | 61.8 | 65.3 | 521 | 1088 | 429.6 | 1179.4 | 759.45 | 849.55 |
| BARI/Bourassa et al[28] | 65.4 | 61.3 | 612 | 584 | 204.52 | 991.48 | 578.86 | 617.14 |
| Bourassa et al[29] | 17.4 | 56.6 | 62 | 70 | 15.05 | 116.95 | 55.97 | 76.03 |
| Head et al[30] | 59.9 | 64.9 | 328 | 713 | 300 | 438 | 702 | 356 |
| BARI 2D/Schwartz et al[31] | 37.9 | 61.21 | - | - | - | |||
| Mohammadi et al[32] | 82.1 | 82.1 | 224 | 167 | 107.92 | 283.08 | 286.21 | 104.79 |
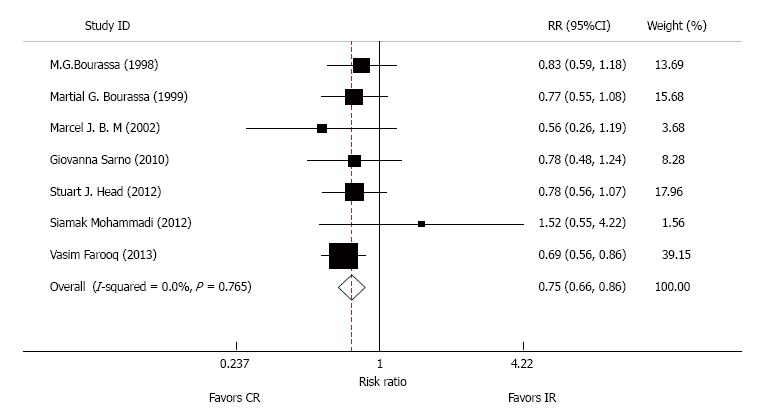
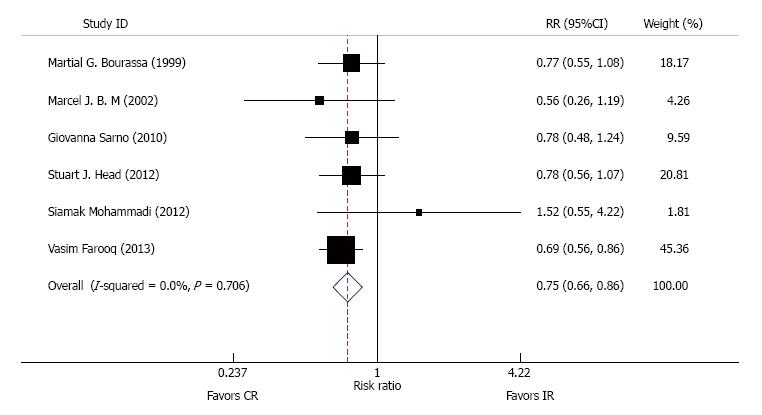
Of the ten studies included, eight reported mortality and were used for this analysis. CR is associated with reduced overall mortality relative to ICR (RR: 0.755, 95%CI: 0.66 to 0.864, P = 0.765, I2 = 0.0%) (Figure 2). In a subgroup analysis: Mid-term follow-up of < 5 years shows that CR has lower mortality (RR: 0.710, 95%CI: 0.595 to 0.847, P = 0.701, I2 = 0.0%). Long-term follow-up of > 5 years is associated with reduced mortality (RR: 0.824, 95%CI: 0.669 to 1.016, P = 0.660, I2 = 0.0%). In the age group of > 60 years, CR is associated with reduced mortality (RR: 0.742, 95%CI: 0.641 to 0.859, P = 0.706, I2 = 0.0%) (Figure 3).
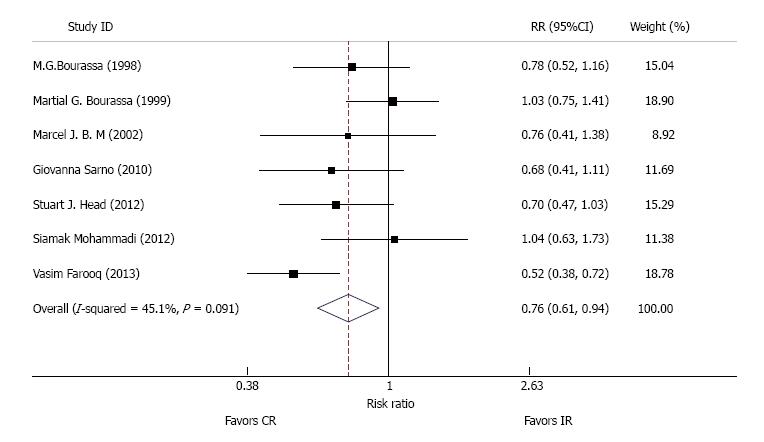
Of the ten studies, seven reported MI and were used for this analysis. CR is associated with reduced rates of post-operative MI as compared to ICR (RR: 0.759, 95%CI: 0.615 to 0.937, P = 0.091, I2 = 45.1%) (Figure 4). In a subgroup analysis: mid-term follow-up of < 5 years group, occurrence of MI is less with CR as compared to ICR (RR: 0.608, 95%CI: 0.484 to 0.763, P = 0.388, I2 = 0.0%). Long-term follow-up of > 5 years shows that CR is associated with reduced rates of MI (RR: 0.894, 95%CI: 0.731 to 1.095, P = 0.419, I2 = 0.0%). In the age group of > 60 years, CR is associated with reduced MI (RR: 0.758, 95%CI: 0.589 to 0.974, P = 0.053, I2 = 54.1%).
Of the ten studies, six reported repeat revascularization and were consequently used in this analysis. CR is associated with reduced rates of revascularization (PCI and/or CABG) relative to ICR (RR: 0.691, 95%CI: 0.541 to 0.883, P = 0.0, I2 = 88.3%). In a subgroup analysis: Mid-term follow-up of < 5 years shows that CR is associated with less repeat revascularizations (RR: 0.827, 95%CI: 0.651 to 1.052, P = 0.323, I2 = 11.6%). Long-term follow up of > 5 years shows that CR is associated with less repeat revascularizations (RR: 0.827, 95%CI: 0.651 to 1.052, P = 0.009, I2 = 78.9%). In the age group > 60 years, CR is associated with reduced rates of repeat revascularization (RR: 0.646, 95%CI: 0.484 to 0.863, P = 0.0, I2 = 89.2%).
Of the ten studies, five reported MACCE and were used in this analysis. CR is associated with reduced MACCE relative to ICR (RR: 0.731, 95%CI: 0.668 to 0.8, P = 0.453, I2 = 0.0%). In a subgroup analysis of MACCE: Mid-term follow-up of < 5 years shows that CR is associated with lower MACCE rates as compared to ICR (RR: 0.717, 95%CI: 0649 to 0.792, P = 0.427, I2 = 0.0%). Long-term follow-up of > 5 years shows that CR is associated with reduced rates of MACCE (RR: 0.799, CI: 0.644 to 0.990, P = 0.427, I2 = 0.0%). In the age group of > 60 years, CR is associated with less MACCE (RR: 0.731, 95%CI: 0.668 to 0.8, P = 0.453; I2 = 0.0%).
The results of our study comparing the outcomes of CR vs ICR show that CR is associated with a 25% reduction in overall mortality, 24% reduction in MI, 27% reduction in MACCE, and 31% reduction in repeat revascularization procedures. Our findings are quite similar to the paper published by Santiago et al[5] where they reported a 30% reduction in long term mortality, a 22% reduction in MI, and a 26% reduction in repeat coronary revascularization procedures. Moreover, the results of our subgroup analysis show that independent of the modality of revascularization, CR is associated with better mid-term (< 5 years), long-term (> 5 years) outcomes and is also associated with lesser adverse outcomes in the > 60 years old patient population.
Conventionally, there are two distinct approaches to coronary artery revascularization, one of them being CABG and the other being PCI. Both of these revascularization strategies have their set of advantages and disadvantages. The advantages of PCI include use of local anesthesia, minimal post-procedural morbidity, and shorter hospital stay. New advancement in the form of DES has also allowed effective treatment of long diffuse stenosed segments. Despite these numerous advantages, PCI remains restricted with respect to its inability to overcome chronic total occlusions, whereby success rates vary and symptomatic failures eventually require CABG. CABG surgery, on the other hand, despite having the ability to overcome chronic occlusions, and necessitating fewer repeat revascularization procedures, is nevertheless associated with substantial postoperative morbidity, longer periods of hospitalization, and a slower return to normal activities. Multiple diseased vessel segments are challenging, requiring multiple grafts and longer operative times which translate into longer periods of CPB, and are associated with higher morbidity[10]. Among the main adverse outcomes, PCI is associated with higher rates of MI and repeat revascularization while CABG is associated with higher morbidity and risk of stroke[11]. Many variables have to be considered when selecting a patient for any procedure, which might be a cause for dissimilarities between the outcomes from different studies. Although SYNTAX reported a higher incidence of MACCE at 5 years, data concerning the incidence of death, MI and stroke at 5 years was inconsistent between these studies, even in the diabetic subgroup. In SYNTAX there was no significant difference reported at 5 years in any of the individual outcomes of death, MI, or stroke between PCI and CABG in either the diabetic or non-diabetic subgroups[12]. On the other hand, in the FREEDOM trial PCI was associated with higher incidence of death and MI with a lower incidence of stroke when compared to CABG[10]. Past studies have compared post-procedural outcomes of these two revascularization approaches[13-15]. The primary focus of our study is the clinical outcome(s) of complete revascularization as compared to ICR, achieved by any particular method of revascularization, or both methods simultaneously (hybrid procedures), rather than a comparison of CABG vs PCI.
The association between CR and lower risk for subsequent cardiovascular events has been documented in some studies in which the benefits of complete revascularization are reduction and often elimination of myocardial ischemia (which has been linked to worse prognosis especially when large), improvement in left ventricular function with preserved ejection fraction in heart failure patients, reduction of arrythmias, improved exercise capacity, and better tolerance to future acute myocardial ischemic events[12,16]. More importantly, the mortality benefit of CR is independent of revascularization modality and definition of CR used[17]. In a study by An Den Brand et al[14], the authors reported that the frequency with which CR was achieved was greater in CABG treated patients (84.1%) as compared to stented patients, despite the potential for equivalent revascularization. Although no difference in mortality or the combined endpoint of death/stroke/MI were seen, overall MACCE rates were significantly higher in the incompletely revascularized stented group, driven by an increased need for CABG within the first year of follow up.
Over the past decades, CABG has evolved to better peri-operative management, more frequent use of arterial grafting and off pump surgery, and development of minimally invasive direct coronary artery bypass grafting (MIDCAB) and robot-assisted totally endoscopic coronary artery bypass (TECAB) grafting as genuine options. PCIs, especially percutaneous transluminal coronary angioplasty (PTCA), initially developed as a strategy in the treatment of single-vessel disease. Currently, particularly with the advent of DES and new devices to treat chronic total occlusions, it is considered an alternative to CABG in the treatment of multiple vessel disease in certain cases[18,19]. These improvements in technique have increased the feasibility and practicability of complete revascularization. Although CABG and PCI have their own sets of inclusion and exclusion criteria, overlapping in selection criteria exist, where the decision to proceed with a particular technique is generally made by a heart team, consisting of both cardiac surgeons and cardiologists among others. All other factors excluded, we propose that CR/IR should influence a decision to proceed with any specific surgical approach of coronary artery revascularization.
The short-term, mid-term, and long-term outcomes of a strategy of revascularization are as important to the patient as it is to the doctor, and we consider it a pivotal factor in the decision making process. In our study, we sub-divided the follow-up time at the 5-year mark, and obtained the two sub-groups, namely the mid-term follow-up group (< 5 years) and long-term follow-up group (> 5 years). Statistical analysis was separately performed on each of the subgroups. CR was found to be associated with less mortality, post-op MI, reduced MACCE, and repeat revascularization procedures.
There has been a gradual increase in the average age of patients now referred for CABG. Contemporary cohorts consist of a greater proportion of octogenarians[15,20]. The BARI trial reported no survival disadvantage associated with IR, where non-LAD territories were left ungrafted. Siamak Mohammadi et al[32] in their study of octogenarians undergoing CABG reported that short-term and long-term mortality were not negatively affected by a strategy of ICR during CABG. Due to the greater number of grafted vessels, CR is associated with longer procedural times. This translates into increased duration of general anesthesia, longer cardiopulmonary bypass times, which increase the incidence of negative post-procedural complication and delay discharge from the hospital. Hence, some surgeons have advocated the concept of incomplete “reasonable” revascularization[21-23]. The results of our subgroup analysis show that there is a reduction across all negative outcomes associated with CR in patients who are > 60 years old. Despite the general trend in the elderly population, we propose CR as a precautionary measure against leaving potential myocardial regions and graftable target coronary arteries un-revascularized.
There are several limitations to our meta-analysis. The results are affected by variation in study design, end-point definitions and reporting and possible publication bias. Moreover, our results and analysis are limited to the papers found on the Pubmed database and those added by hand-search.
Our study is concordant with similar studies from the past, whereby CR is associated with lower mortality, reduced post-op MI and MACCE, and lower rates of repeat procedures for revascularization. Furthermore, our study shows that CR is also associated with better mid-term and long-term outcomes, and less adverse outcomes in the > 60 years of age patient population. In our experience, CR acts as a buffer between CABG and PCI, and reduces the adverse outcomes associated with any one particular technique. With this in mind, and as dictated by the patient’s condition, the technique with which CR is most likely to be accomplished should be used, and hybrid techniques can be emphasized for complicated cases, thus maximizing the gains from both techniques while minimizing the drawbacks. Given the obvious benefits, CR should be considered as the standard to determine the strategy of revascularization in patients with multi-vessel CAD.
Two strategies are used in the treatment of multivessel coronary artery disease (CAD), namely percutaneous coronary intervention with stenting and coronary artery bypass grafting. Previous studies have proved the importance of complete revascularization. However, the extent to which completeness of revascularization influences the outcomes is still unclear.
Nowadays with new improvements in technology and technique, the feasibility of complete revascularization is less of an issue. Hence, a thorough understanding of how complete revascularization affects post-procedural outcomes is mandatory.
To investigate the influence and outcomes of complete vs incomplete myocardial revascularization in patients with multivessel CAD.
Database (pubmed) search coupled with hand search was performed for the identification and collection of relevant studies. Filters, inclusion and exclusion criteria were used to ensure quality and homogenecity of studies. Standard tables were used for data extraction. The data was analyzed and subjected to the appropriate tests by a statistician. A systematic review was then performed.
Ten studies were identified, including 13327 patients of whom, 8053 received complete revascularization and 5274 received ICR. Relative to ICR, CR was associated with lower mortality (RR: 0.755, 95%CI: 0.66 to 0.864, P = 0.765, I2 = 0.0%), lower rates of MI (RR: 0.759, 95%CI: 0.615 to 0.937, P = 0.091, I2 = 45.1%), lower rates of MACCE (RR: 0.731, 95%CI: 0.668 to 0.8, P = 0.453, I2 = 0.0%) and reduced rates of repeat coronary revascularization (RR: 0.691, CI: 0.541 to 0.883, P = 0.0, I2 = 88.3%).
Completeness of revascularization is not mandatory for the treatment of multivessel CAD. The results of our study show that CR is associated with lower rates of adverse outcomes. The results propose that the extent to which a technique can achieve complete revascularization should be a major deciding factor in the choice of any one particular technique.
Complete revascularization is an alternative standard to decide the choice of a particular technique of revascularization. With emerging techniques of coronary revascularization, new retrospective cohort studies can be performed. Further research is needed to better understand the benefits of complete revascularization with a particular technique.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Liang Y, Pani SP, Petrucciani N S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | DeFrances CJ, Lucas CA, Buie VC, Golosinskiy A. 2006 National Hospital Discharge Survey. Natl Health Stat Report. 2008;1-20. [PubMed] |
| 2. | Yusuf S, Zucker D, Peduzzi P, Fisher LD, Takaro T, Kennedy JW, Davis K, Killip T, Passamani E, Norris R. Effect of coronary artery bypass graft surgery on survival: overview of 10-year results from randomised trials by the Coronary Artery Bypass Graft Surgery Trialists Collaboration. Lancet. 1994;344:563-570. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1405] [Cited by in RCA: 1373] [Article Influence: 44.3] [Reference Citation Analysis (0)] |
| 3. | Hachamovitch R, Hayes SW, Friedman JD, Cohen I, Berman DS. Comparison of the short-term survival benefit associated with revascularization compared with medical therapy in patients with no prior coronary artery disease undergoing stress myocardial perfusion single photon emission computed tomography. Circulation. 2003;107:2900-2907. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1163] [Cited by in RCA: 1113] [Article Influence: 50.6] [Reference Citation Analysis (0)] |
| 4. | Bell MR, Gersh BJ, Schaff HV, Holmes DR Jr, Fisher LD, Alderman EL, Myers WO, Parsons LS, Reeder GS. Effect of completeness of revascularization on long-term outcome of patients with three-vessel disease undergoing coronary artery bypass surgery. A report from the Coronary Artery Surgery Study (CASS) Registry. Circulation. 1992;86:446-457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 237] [Cited by in RCA: 224] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 5. | Garcia S, Sandoval Y, Roukoz H, Adabag S, Canoniero M, Yannopoulos D, Brilakis ES. Outcomes after complete versus incomplete revascularization of patients with multivessel coronary artery disease: a meta-analysis of 89,883 patients enrolled in randomized clinical trials and observational studies. J Am Coll Cardiol. 2013;62:1421-1431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 268] [Cited by in RCA: 288] [Article Influence: 24.0] [Reference Citation Analysis (0)] |
| 6. | Adabag AS, Ishani A, Bloomfield HE, Ngo AK, Wilt TJ. Efficacy of N-acetylcysteine in preventing renal injury after heart surgery: a systematic review of randomized trials. Eur Heart J. 2009;30:1910-1917. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 66] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 7. | Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39087] [Cited by in RCA: 46470] [Article Influence: 2112.3] [Reference Citation Analysis (3)] |
| 8. | DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26739] [Cited by in RCA: 30401] [Article Influence: 779.5] [Reference Citation Analysis (0)] |
| 9. | Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629-634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34245] [Cited by in RCA: 40493] [Article Influence: 1446.2] [Reference Citation Analysis (2)] |
| 10. | Ong AT, Serruys PW. Complete revascularization: coronary artery bypass graft surgery versus percutaneous coronary intervention. Circulation. 2006;114:249-255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 94] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 11. | French JK, Burgess S, Chew DP. Re-infarction after primary percutaneous coronary intervention. Curr Opin Cardiol. 2015;30:354-358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Weintraub WS, Grau-Sepulveda MV, Weiss JM, O’Brien SM, Peterson ED, Kolm P, Zhang Z, Klein LW, Shaw RE, McKay C. Comparative effectiveness of revascularization strategies. N Engl J Med. 2012;366:1467-1476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 430] [Cited by in RCA: 433] [Article Influence: 33.3] [Reference Citation Analysis (0)] |
| 13. | Fanari Z, Weiss SA, Zhang W, Sonnad SS, Weintraub WS. Comparison of percutaneous coronary intervention with drug eluting stents versus coronary artery bypass grafting in patients with multivessel coronary artery disease: Meta-analysis of six randomized controlled trials. Cardiovasc Revasc Med. 2015;16:70-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 14. | van den Brand MJ, Rensing BJ, Morel MA, Foley DP, de Valk V, Breeman A, Suryapranata H, Haalebos MM, Wijns W, Wellens F. The effect of completeness of revascularization on event-free survival at one year in the ARTS trial. J Am Coll Cardiol. 2002;39:559-564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 147] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 15. | Serruys PW, Unger F, Sousa JE, Jatene A, Bonnier HJ, Schönberger JP, Buller N, Bonser R, van den Brand MJ, van Herwerden LA. Comparison of coronary-artery bypass surgery and stenting for the treatment of multivessel disease. N Engl J Med. 2001;344:1117-1124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 808] [Cited by in RCA: 768] [Article Influence: 32.0] [Reference Citation Analysis (0)] |
| 16. | Shaw LJ, Berman DS, Maron DJ, Mancini GB, Hayes SW, Hartigan PM, Weintraub WS, O’Rourke RA, Dada M, Spertus JA. Optimal medical therapy with or without percutaneous coronary intervention to reduce ischemic burden: results from the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial nuclear substudy. Circulation. 2008;117:1283-1291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1215] [Cited by in RCA: 1163] [Article Influence: 68.4] [Reference Citation Analysis (0)] |
| 17. | Yang ZK, Zhang RY, Hu J, Zhang Q, Ding FH, Shen WF. Impact of successful staged revascularization of a chronic total occlusion in the non-infarct-related artery on long-term outcome in patients with acute ST-segment elevation myocardial infarction. Int J Cardiol. 2013;165:76-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 52] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 18. | Kappetein AP, Head SJ, Morice MC, Banning AP, Serruys PW, Mohr FW, Dawkins KD, Mack MJ; SYNTAX Investigators. Treatment of complex coronary artery disease in patients with diabetes: 5-year results comparing outcomes of bypass surgery and percutaneous coronary intervention in the SYNTAX trial. Eur J Cardiothorac Surg. 2013;43:1006-1013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 256] [Cited by in RCA: 256] [Article Influence: 21.3] [Reference Citation Analysis (0)] |
| 19. | Serruys PW, Ong AT, van Herwerden LA, Sousa JE, Jatene A, Bonnier JJ, Schönberger JP, Buller N, Bonser R, Disco C. Five-year outcomes after coronary stenting versus bypass surgery for the treatment of multivessel disease: the final analysis of the Arterial Revascularization Therapies Study (ARTS) randomized trial. J Am Coll Cardiol. 2005;46:575-581. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 467] [Cited by in RCA: 440] [Article Influence: 22.0] [Reference Citation Analysis (0)] |
| 20. | Tarakji KG, Sabik JF 3rd, Bhudia SK, Batizy LH, Blackstone EH. Temporal onset, risk factors, and outcomes associated with stroke after coronary artery bypass grafting. JAMA. 2011;305:381-390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 231] [Cited by in RCA: 231] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 21. | Ferguson TB Jr, Hammill BG, Peterson ED, DeLong ER, Grover FL; STS National Database Committee. A decade of change--risk profiles and outcomes for isolated coronary artery bypass grafting procedures, 1990-1999: a report from the STS National Database Committee and the Duke Clinical Research Institute. Society of Thoracic Surgeons. Ann Thorac Surg. 2002;73:480-489; discussion 489-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 465] [Cited by in RCA: 438] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 22. | Capodanno D, Stone GW, Morice MC, Bass TA, Tamburino C. Percutaneous coronary intervention versus coronary artery bypass graft surgery in left main coronary artery disease: a meta-analysis of randomized clinical data. J Am Coll Cardiol. 2011;58:1426-1432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 149] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 23. | Bainey KR, Mehta SR, Lai T, Welsh RC. Complete vs culprit-only revascularization for patients with multivessel disease undergoing primary percutaneous coronary intervention for ST-segment elevation myocardial infarction: a systematic review and meta-analysis. Am Heart J. 2014;167:1-14.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 120] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 24. | Bell MR, Bailey KR, Reeder GS, Lapeyre AC 3rd, Holmes DR Jr. Percutaneous transluminal angioplasty in patients with multivessel coronary disease: how important is complete revascularization for cardiac event-free survival? J Am Coll Cardiol. 1990;16:553-562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 91] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 25. | McLellan CS, Ghali WA, Labinaz M, Davis RB, Galbraith PD, Southern DA, Shrive FM, Knudtson ML; Alberta Provincial Project for Outcomes Assessment in Coronary Heart Disease (APPROACH) Investigators. Association between completeness of percutaneous coronary revascularization and postprocedure outcomes. Am Heart J. 2005;150:800-806. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 59] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 26. | Sarno G, Garg S, Onuma Y, Gutiérrez-Chico JL, van den Brand MJ, Rensing BJ, Morel MA, Serruys PW; ARTS-II Investigators. Impact of completeness of revascularization on the five-year outcome in percutaneous coronary intervention and coronary artery bypass graft patients (from the ARTS-II study). Am J Cardiol. 2010;106:1369-1375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 66] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 27. | Farooq V, Serruys PW, Garcia-Garcia HM, Zhang Y, Bourantas CV, Holmes DR, Mack M, Feldman T, Morice MC, Ståhle E. The negative impact of incomplete angiographic revascularization on clinical outcomes and its association with total occlusions: the SYNTAX (Synergy Between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery) trial. J Am Coll Cardiol. 2013;61:282-294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 251] [Cited by in RCA: 228] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 28. | Bourassa MG, Kip KE, Jacobs AK, Jones RH, Sopko G, Rosen AD, Sharaf BL, Schwartz L, Chaitman BR, Alderman EL. Is a strategy of intended incomplete percutaneous transluminal coronary angioplasty revascularization acceptable in nondiabetic patients who are candidates for coronary artery bypass graft surgery? The Bypass Angioplasty Revascularization Investigation (BARI). J Am Coll Cardiol. 1999;33:1627-1636. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 40] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 29. | Bourassa MG, Yeh W, Holubkov R, Sopko G, Detre KM. Long-term outcome of patients with incomplete vs complete revascularization after multivessel PTCA. A report from the NHLBI PTCA Registry. Eur Heart J. 1998;19:103-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 55] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 30. | Head SJ, Mack MJ, Holmes DR Jr, Mohr FW, Morice MC, Serruys PW, Kappetein AP. Incidence, predictors and outcomes of incomplete revascularization after percutaneous coronary intervention and coronary artery bypass grafting: a subgroup analysis of 3-year SYNTAX data. Eur J Cardiothorac Surg. 2012;41:535-541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 153] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 31. | Schwartz L, Bertolet M, Feit F, Fuentes F, Sako EY, Toosi MS, Davidson CJ, Ikeno F, King SB 3rd. Impact of completeness of revascularization on long-term cardiovascular outcomes in patients with type 2 diabetes mellitus: results from the Bypass Angioplasty Revascularization Investigation 2 Diabetes (BARI 2D). Circ Cardiovasc Interv. 2012;5:166-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 52] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 32. | Mohammadi S, Kalavrouziotis D, Dagenais F, Voisine P, Charbonneau E. Completeness of revascularization and survival among octogenarians with triple-vessel disease. Ann Thorac Surg. 2012;93:1432-1437. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 2.5] [Reference Citation Analysis (0)] |