Published online Oct 26, 2015. doi: 10.13105/wjma.v3.i5.206
Peer-review started: January 30, 2015
First decision: March 6, 2015
Revised: June 5, 2015
Accepted: September 16, 2015
Article in press: September 18, 2015
Published online: October 26, 2015
Processing time: 282 Days and 23.5 Hours
AIM: To evaluate the effectiveness and safety of acupuncture for the treatment of obesity by reviewing currently available randomised controlled trials.
METHODS: This review followed the Cochrane Handbook for Systematic Reviews of Interventions. Fifteen English and three Chinese databases were searched from their respective inceptions until July 2014. Key words used in the search consisted of acupuncture, needles, obesity, overweight, randomised trial and their synonyms. The risk of bias of included studies was assessed. The differences in effect size between acupuncture and control (including sham, no treatment, western medicine and dietary therapy/exercise) groups were compared using Cochrane Collaboration’s RevMan 5.3 software.
RESULTS: Two thousand six hundred and twenty-one records were identified; after full-text articles assessed for eligibility, 9 of them met inclusion criteria. Majority of included studies had unclear or high risk of bias across all domains. All included studies had high or unclear risk of bias in randomisation, blinding and outcome data. Meta-analysis showed that acupuncture was more effective for reducing body weight and body mass index than no treatment group. Manual acupuncture was also superior to dietary therapy alone for decreasing body weight. With dietary therapy as co-intervention, combined acupuncture group achieved lower body mass index than combined sham acupuncture group or dietary therapy alone group at the end of treatment period. No severe adverse events from acupuncture group were reported from all included studies.
CONCLUSION: Due to the poor quality of included studies the effectiveness of acupuncture cannot be concluded. Better-designed, large-scale, randomised, sham-controlled clinical trials with long-term follow-up are needed.
Core tip: This systematic review identified the benefit of traditional Chinese manual acupuncture in the management of obesity. However, the effectiveness cannot be confirmed due to poorly-design randomised clinical trials.
- Citation: Li KX, Yang AW, Xue CC, Lenon GB. Traditional Chinese manual acupuncture for management of obesity: A systematic review. World J Meta-Anal 2015; 3(5): 206-214
- URL: https://www.wjgnet.com/2308-3840/full/v3/i5/206.htm
- DOI: https://dx.doi.org/10.13105/wjma.v3.i5.206
Obesity is a medical condition involving more than one kind of biological basis or metabolic disease[1]. It is often accompanied with fatigue, lassitude, hydrosis, various neurosis, headache, palpitation, and abdominal distension[2]. The World Health Organisation (WHO) estimates more than one billion overweight adults worldwide out of which at least 500 million are obese[3]. The prevalence of obesity is a major public health concern since obesity is often associated with cerebrovascular and cardiovascular diseases, hypertension, arteriosclerosis, diabetes and speeding up the aging process[4]. Obesity places considerable economic burden on already strained healthcare systems as it reduces quality of life and leads to premature mortality[5].
However, the treatment for obesity without obvious causes is challenging. Currently, the main management of obesity includes dietary therapy, physical exercise, behaviour treatment, pharmacotherapy (such as Sibutramine and Orlistat) and surgery[6]. However, it is difficult to change behaviours to maintain the weight loss by the same dietary changes and physical exercises in a long term[7]. Pharmacotherapy often associates with undesired effects[8]. Surgery is usually considered only when there are serious medical conditions, for example, a high risk of obesity-related illness and death[9]. Recently, there is a global trend for obesity sufferers to seek treatment from complementary and alternative medicine including acupuncture.
Acupuncture for weight management has been practicing for many centuries. It involves inserting thin and solid needles to certain points on the body to achieve therapeutic effects. A number of reviews involving different types of needling and needle stimulation techniques (including traditional Chinese acupuncture, electro-acupuncture, dry needling, ear-acupuncture and transcutaneous electrical nerve stimulation) for weight loss have been published[10-12]. However, the effects of traditional Chinese manual acupuncture are unclear as its effects have not been reviewed separately. Traditionally, acupuncture applies manual stimulation based on Chinese medicine theory such as point selections and De Qi sensation without electrical stimulation. Therefore, this study aimed to evaluate the therapeutic benefits and safety of traditional manual stimulation acupuncture for the management of obesity by systematically reviewing the currently available randomised clinical trials (RCTs).
This review was conducted following the instructions specified in the Cochrane Handbook for Systematic Reviews of Interventions 5.2[13].
We searched 15 electronic English and three Chinese databases, including Cochrane Central Register of Controlled Trials, PubMed, EMBASE, CINAHL, Science Direct, LILACS (Latin American and Caribbean Health Sciences), ProQuest, Web of Science, Informit, Psycinfo, Blackwell Synergy, KoreaMed, INDMED, Ingenta, mRCT, VIP Information (http://www.cqvip.com), China National Knowledge Infrastructure (http://www.cnki.net), and Wanfang Data (http://www.wanfangdata.com), from their respective inceptions to July 2014. Key words used consisted of acupuncture, needles, obesity, overweight, weight loss, randomised trials and their synonyms. We also hand searched the reference lists of clinical trials and reviews as well as the conference proceedings of the World Congress of Chinese Medicine from 2003 onwards to identify the relevant studies.
RCTs, with or without blinding, were considered if they investigated the effects of manual acupuncture for adult patients of any gender, diagnosed as obesity or overweight according to WHO criteria [overweight: body mass index (BMI) ≥ 25; obesity: BMI ≥ 30]. A study was included when it compared traditional manual acupuncture with sham, no treatment, Western medicine, dietary therapy and/or exercise. Co-intervention was allowed as long as the same co-intervention was used in both arms.
Studies of non-traditional acupuncture such as electro-acupuncture, dry needling, ear-acupuncture or transcutaneous electrical nerve stimulation were excluded.
Two reviewers (Li KX and Yang AW) independently screened the titles and abstracts. When lack of adequate information for judgement identified, full texts were obtained for further assessment. Any discrepancies between two reviewers were resolved by discussion or consultation with the third party (Lenon GB).
A predefined data extraction form was used to extract the data of included studies, including characteristics of participants, interventions and outcomes. Two reviewers (Li KX and Yang AW) independently extracted the data and discussed the differences. Unresolved issues were consulted with the third party (Lenon GB).
We assessed the risk of bias of each study including random sequence generation, allocation concealment, blinding of participants and outcome assessors, incomplete outcomes, selective reporting and other bias (e.g., baseline imbalance). Each bias was classified as low, unclear or high risk.
The primary outcomes included effectiveness rate, body weight and BMI and the secondary outcome was adverse events. The meta-analysis on effectiveness rate, body weight and BMI were performed using Review Manager 5.3 developed by the Cochrane Collaboration[14]. The effectiveness rate was calculated as (scores before treatment - scores after treatment)/scores before treatment × 100%. The effects assessed immediately after the treatment period were considered as short-term effects whilst the effects followed up for more than three months after the last treatment were regarded as long-term. The effectiveness rate was analysed by risk ratio (RR). Body weight and BMI were calculated by difference in means (MD). All were with 95%CI.
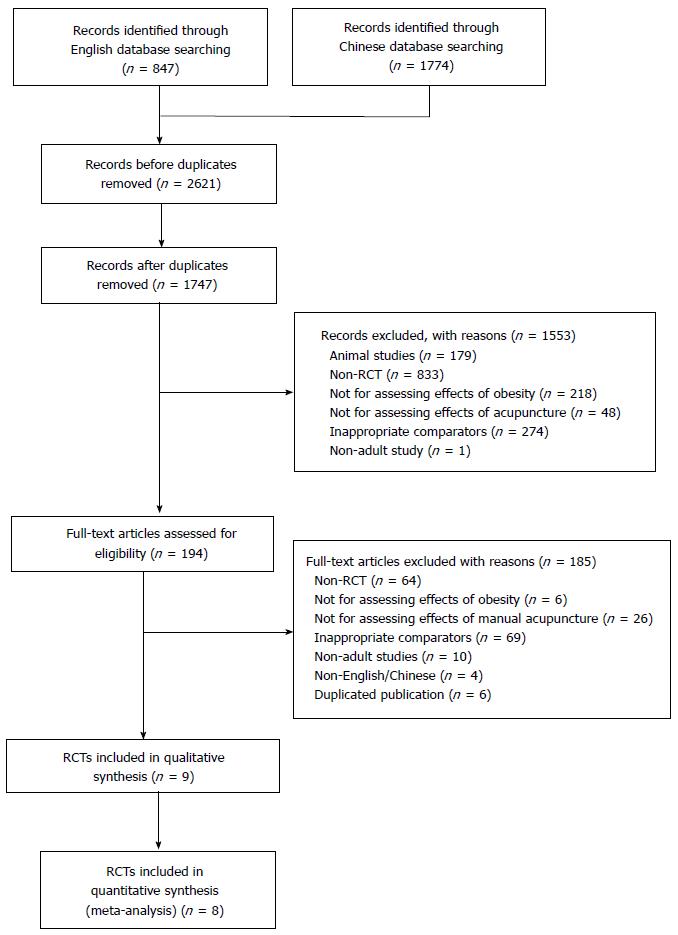
A total of 2621 potential studies were identified following search strategy and 2427 of them were excluded after screening titles and abstracts. Full texts were obtained for the remaining 194 studies and nine of them met inclusion criteria[15-23]. The main reasons for exclusion were non-obesity, non-acupuncture and non-RCT. Figure 1 illustrates the study selection process and provides the exclusion reasons.
Eight included studies were conducted in mainland China[15,16,18-23] and one in Turkey[17]. Except two studies published in English[17,23], the rest seven papers were published in Chinese. The total sample size is 556, ranging from 33 to 118 with an average of 61 per trial. A total of 110 males and 446 females were involved in the included studies. All the participants in the RCTs were clearly diagnosed as obesity and/or overweight. The duration of treatment lasted from 30 d to 65 d and the treatment sessions varied from 10 to 40.
Two studies used three-arm design[18,23] and the rest RCTs were two-arm trials. Although Xu et al[23]’s trial claimed it was a three-arm trial, the same treatment protocol was used in the two treatment groups by two different acupuncturists. In terms of interventions, all of them involved manual acupuncture in the treatment groups. Seven RCTs adopted standard acupoints to treat all participants in the acupuncture group. Only two studies[16,22] applied different groups of acupoints to treat participants with different syndromes (a complex of symptoms and signs according to Chinese medicine theory). Acupuncture treatment in seven trials obtained De Qi sensation[15-21]. Across the nine trials, different acupuncture point formulae were prescribed. The top five frequently used acupoints were Zusanli (ST36, 6 trials), Sanyinjiao (SP6, 6 trials), Zhongwan (CV12, 5 trials), Xuehai (SP10, 4 trials) and Tianshu (ST25, 4 trials).
In the control groups, comparators were various, including sham acupuncture, no treatment, Western medicine, dietary therapy and exercise. Five RCTs[16,17,19,22,23] and one arm of Luo et al[18]’s study did not involve any co-intervention. One compared manual acupuncture with sham acupuncture[17]. Two studies[22,23] and one arm of Luo et al[18]’s study compared manual acupuncture with no treatment and another two studies[16,19] compared acupuncture with dietary therapy. The remaining three RCTs involved co-interventions in both groups. Acupuncture was assessed as an adjunct treatment to dietary therapy and/or exercise[15,20,21] when compared to dietary therapy and/or exercise alone.
With regard to outcome measures, five RCTs used the effectiveness rate to present the effects of acupuncture on reduction of body weight of people with obesity[15,16,18,19,22]. Five RCTs evaluated BMI[17,18,20-22] and four studies assessed body weight[15,17,20,22] at the end of treatment period. Only one included study monitored adverse events[15].
The detailed characteristics of participants, interventions and outcome measures are summarised in Table 1.
| Ref. | Setting | Randomised sample size | Intervention | Outcome measure | Adverse events | |||
| T (n, age) | C (n, age) | T | C | |||||
| Acu vs sham acu | Güçe et al[17] | Clinic, outpatients | 20, NS M/F: 0/20 | 20, NS M/F: 0/20 | Acupoints: Hegu (LI4), Shenmen (HT7), Zusanli (ST36), Neiting (ST44), Sanyinjiao (SP6) Insertion depth: 5-10 mm; Duration: 5 wk; Sessions: 10; Frequency: 2/wk; Retention time: 20 min; Follow-up: NS | Sham acu: Same procedures as T group | BW BMI Blood test | NS |
| Acu vs no treatment | Luo et al[18] | NS | T1: 20, 21-48 yr; M/F: 8/12 T2: 20, 21-48 yr; M/F: 10/10 | 20, 21-48 yr M/F: 6/14 | T1: Electro acu; T2: Manual acu Acupoints (2 groups used alternatively): (1) Liangqiu (ST34), Xuehai (SP10), Zhigou (TE6), Waiguan (TE5), Sanyinjiao (SP6), Zusanli (ST36), Fujue (SP14), Daimai (GB26), Tianshu (ST25), Wailing (ST26), Guanyuan (CV4), Taixi (KI3), Shangjuxu (ST37) (2) Gongsun (SP4), Neiting (ST44), Fenglong (ST40), Neiguan (PC6), Yinlingquan (SP9), Zusanli (ST36), Shuifen (CV9), Zhongwan (CV12), Daju (ST27), Shuidao (ST28), Guanyuan (CV4), Taichong (LR3), Quchi (LI11), Xiajuxu (ST39) Insertion depth: 10-35 mm; Duration: 65 d Sessions: 27; Frequency: once every other day; Retention time: 30 min; Follow-up: NS | No treatment | ER BMI WHR Blood test | NS |
| Wang et al[22] | NS | 18, 20-55 yr M/F: NS | 18, 20-55 yr M/F: NS | Acupoints: (1) Stomach heat: 10 abdominal points + Quchi (LI11), Neiting (ST44), Shangjuxu (ST37), Pishu (BL20), Xuehai (SP10), Fenglong (ST40) (2) Qi deficiency: 10 abdominal points + Shangjuxu (ST37), Sanyinjiao (SP6), Yinlingquan (SP9), Pishu (BL20), Xinshu (BL15), Taixi (KI3), Guanyuan (CV4) Insertion depth: NS; Duration: 30 d; Sessions: 30; Frequency: 1/d; Retention time: 50 min; Follow-up: NS | No treatment | BW BMI F% Electrogastrography | NS | |
| Xu et al[23] | Hospital, outpatients | T1: 15, 29-63 yr; M/F: 0/15 T2: 15, 29-63 yr; M/F: 0/15 | 15, 29-63 yr M/F: 0/15 | T1 and T2 on same acupoints: Zhongwan (CV12), Shuifen (CV9), Qihaishu (BL24), Guanyuanshu (BL26), Shuidao (ST28), Tianshu (ST25), Zusanli (ST36), Sanyinjiao (SP6) Insertion depth: 1.5 inch; Duration: 40 d; Sessions: 20; Frequency: once every other day Retention time: 30 min; Follow-up: NS | No treatment | BMI Faecal microbial flora | NS | |
| Acu vs diet | Fan et al[16] | Hospital, outpatients | 50, NS M/F: 11/39 | 50, NS M/F: 10/40 | Primary acupoints: Xuehai (SP10), Sanyinjiao (SP6), Tianshu (ST25), Zusanli (ST36), Hegu (LI4) Insertion depth: NS; Duration: 50 d; Sessions: 30; Frequency: 1/d for the first 10 sessions; then once every other day for the last 20 sessions; Retention time: 30 min; Follow-up: NS | Dietary therapy for 50 d | ER Blood test | NS |
| Shen et al[19] | NS | 30, 18-52 yr; M/F: 1/29 | 30, 18-52 yr; M/F: 1/29 | Acupoints: Huatuojiaji T3 to L5 Insertion depth: 1-1.5 cun; Duration: 30 d; Sessions: 30; Frequency: 1/d; Retention time: 30 min; Follow-up: NS | Dietary therapy for 30 d | ER | NS | |
| Acu + diet vs sham acu + same diet | Tong et al[21] | Hospital, outpatients | 76, 18-60 yr M/F: 18/58 | 42, 18-60 yr M/F: 12/30 | Manual acu + dietary therapy Acupoints: Zhongwan (CV12), Zhongji (CV3), Daheng (SP12), Xiawan (CV10), Shimen (CV5), Tianshu (ST25), Liangqiu (ST34), Zusanli (ST36), Yinlingquan (SP9) Insertion depth: subject to De Qi; Duration: 5 wk; Sessions: 12; Frequency: once every other day; Retention time: 30 min; Follow-up: NS | Sham acu + same dietary therapy | BMI Adipose layer score | NS |
| Acu + diet vs Same diet | Tao[20] | NS, outpatients | 20, 20-27 yr M/F: NS | 20, 20-27 yr M/F: NS | Manual acu + dietary therapy Acupoints: Zhongwan (CV12), Qihai (CV6), Tianshu (ST25), Zhigou (TE6), Fenglong (ST40), Liangqiu (ST34), Yinlingquan (SP9), Zusanli (ST36), Sanyinjiao (SP6), Neiting (ST44) Insertion depth: NS; Duration: 37 d; Sessions: 20; Frequency: 1/d; Retention time: 30 min; Follow-up: NS | Dietary therapy: same as T group | BW BMI Blood test | NS |
| Acu + diet/ exercise vs WM + same diet/exercise | Dong[15] | Hospital, outpatients | 30, 18-65 yr M/F: NS | 30, 18-65 yr M/F: NS | Manual acu + dietary therapy and exercise Acupoints: Xuehai (SP10), Pishu (BL20), Weishu (BL21), Zhongwan (CV12), Guanmen (ST22) Insertion depth: NS; Duration: 40 d; Sessions: 40; Frequency: 1/d; Retention time: 30 min; Follow-up: 3 mo | WM + same dietary therapy and exercise WM: Sibutramine hydrochloride 10 mg/d for 40 d | ER BW F% | T: 16.67% C: 42.86%; dry mouth, constipation, dizziness, headache, insomnia, palpitation, poor appetite |
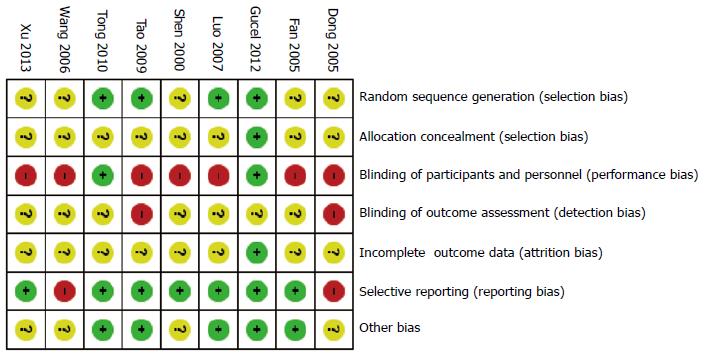
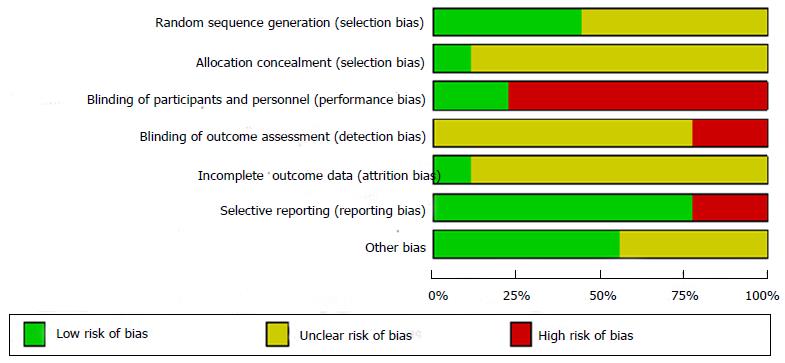
Randomisation was claimed in all included RCTs. The risk of bias assessment in illustrated in the Figures 2 and 3. However, only four trials clearly provided appropriate methods for random sequence generation, one using three colour cards[18], another using computer-generated randomisation numbers[17] and the other two applying random number table[20,21]. The rest of five RCTs did not provide the methods for randomisation. All but one did not state the methods for allocation concealment. Only Güçel et al[17]’s trial indicated that they used urn for allocating the randomisation numbers. The performance biases of seven RCTs were classified as high risk because they applied different forms of treatments to two groups which made blinding of participants impossible[15,16,18-20,22,23]. In addition, two of them only involved one author and this implied that it was unlikely to blind the outcome assessors in these trials[15,20]. One study clearly indicated that all participants completed the trial[17]. Another study[15] indicated two dropouts from the control group due to side effects. The rest of seven trials did not provide sufficient information for assessment. Dong[15]’s trial mentioned it followed up the participants for three months however, no results at the end of follow-up period were reported. In Wang et al[22]’s study, the results of body weight and BMI for the control group were not reported. The remained seven included studies reported all the outcome measures listed in the methods section of their published papers. Four trials did not report if the baseline data were comparable[15,19,22,23].
Effectiveness rate: Five RCTs assessed the short-term effects of acupuncture[15,16,18,19,22]. Long-term effects of acupuncture were not assessed due to lack of data in all the included studies. As one study used the different criteria for effectiveness rate, its data were not included in the meta-analysis[19]. The pooled data from two studies[18,22] showed that acupuncture was significantly more effective than no treatment at the end of treatment period (RR = 8.28; 95%CI: 1.04-65.97). When compared to dietary therapy, Fan et al[16]’s study indicated that acupuncture had better effects at the end of 20 treatments (RR = 1.93; 95%CI: 1.54-2.40). With dietary therapy and exercise as co-intervention[15], acupuncture group demonstrated similar effects to western medication (sibutramine hydrochloride) group at the end of 40-d treatment (RR = 1.09; 95%CI: 0.42-2.85).
Body weight: Only three studies reported body weight of two groups at the end of treatment period[15,17,20]. No significant difference was found in the three comparisons. There was no significant difference between real and sham acupuncture after 10 treatments[17] (MD: -4.40; 95%CI: -11.21-2.41). Similarly, combination of acupuncture and dietary therapy showed no difference in body weight from dietary alone group at the end of 20 sessions (MD: -0.93; 95%CI: -3.75-1.89)[20]. With dietary therapy and exercise as co-intervention, the findings from Dong[15]’s trial indicated that the body weight of patients treated by acupuncture combined group was not superior to that of patients treated by western medication combined group after 40-d treatment (MD: -2.44; 95%CI: -10.57-5.69).
BMI: BMI data from four trials were included in the meta-analysis[17,18,20,21]. There was no significant difference in BMI between real and sham acupuncture at the end of 10 treatments (MD: -2.56; 95%CI: -5.37-0.25)[17]. The pooled data from two studies[18,23] showed that acupuncture was more effective for BMI than no treatment (MD: -1.88; 95%CI: -2.67 to -1.08). With dietary therapy as co-intervention, real acupuncture group was superior to sham acupuncture group for BMI at the end of five-week treatment (MD: -1.97; 95%CI: -3.15 to -0.79)[21]. Combining acupuncture with dietary therapy was more effective on BMI after 20-session treatment than dietary therapy alone group (MD: -0.55; 95%CI: -1.03 to -0.07)[20].
Only one out of nine included studies reported adverse events. Dong[15]’s study mentioned that 16.67% of patients in treatment group and 42.86% in control group occurred adverse events, including constipation, dizziness, insomnia, palpitation and high blood pressure. Two patients dropped out from the control group due to side effects.
This project reviewed the effects of traditional Chinese manual acupuncture for the treatment of obesity. The focus on the manual acupuncture avoids other confounding variables involved in the intervention. Although the meta-analysis did not show any significant difference between two groups for body weight at the end of treatment, it demonstrated that manual acupuncture was more effective than no treatment for the reduction of body weight and BMI at the end of treatment period. Acupuncture could also significantly benefit for weight loss in a short term when compared to diet control (no co-intervention). With dietary therapy as co-intervention, combined acupuncture group was more effective for BMI than diet alone group or combined sham acupuncture group.
Future research may consider using the reduction of body weight instead of body weight itself as the primary outcome measure. Effects of acupuncture are probably resulted from improving the sense of wellbeing which may suppress the excessive desire of food[24], regulating metabolism and thereby enable the body to utilise food efficiently instead of storing it as fat[25,26]. It may also stimulate the nervous system to release chemicals which may in turn release other neurotransmitters or hormones producing the desired effects[27].
Although different acupoint prescriptions were used, the commonly used acupoints were identified, including Zusanli (ST36), Sanyinjiao (SP6), Zhongwan (CV12), Yinlingquan (SP9) and Tianshu (ST25). These acupoints have been widely used in Chinese medicine clinical practice due to their actions to remove dampness-heat and regulate digestive system. In Chinese medicine, obesity is considered resulted from excessively consuming high energy nutrition and causing accumulation of dampness and heat in the body[28]. Thus, the above-mentioned acupoints are appropriate for reducing weight.
Three of nine included RCTs[15,20,21] involved co-intervention (dietary therapy or dietary therapy with exercise) which reflects the fact that acupuncture is commonly used as an adjunct therapy to other modalities for weight loss in clinical practice. Our findings were consistent with others’ statement that patients with obesity tend to use combination of different therapies for weight loss[29] (Akilen, 2014 #44). This review could not identify an ideal treatment regimen for treating obesity because there were numerous confounders existed in the included studies, such as sample size (33 to 118 subjects), number of acupoints (5 to 14 points), number of needles (9 to 25 needles), and treatment duration (30 to 65 d).
In addition, the majority of the included studies had methodological issues, that is, high and/or unclear risk of bias in selection, performance, detection and attrition. The quality of evidence was classified as low or very low.
In conclusion, acupuncture showed certain beneficial effects for reducing body weight and BMI in patients with obesity. However, due to the high or unclear risk of bias, the results need to be interpreted with caution. More well-designed, large-scale, randomised, sham-controlled clinical trials with long-term follow-up are needed to assess the efficacy and safety of acupuncture for weight loss.
The authors would like to thank RMIT for Kang Xiao Li’s PhD scholarship.
Chinese acupuncture is becoming popular for weight management in the western countries. Many randomised controlled trials reported positive effects on electro-acupuncture and acupuncture microsystem. Traditional manual acupuncture trials are mainly conducted in China where obesity is growing rapidly; however, its effects have not been systematically evaluated.
To the best of our knowledge, no systematic review of traditional Chinese manual acupuncture has previously been reported. The aim of this study was to systematically review effectiveness of Chinese manual acupuncture in the management of overweight and obesity.
Prevalence of global obesity is on the rise which leads to many serious health complications. This creates an economic burden and quality of life. Traditional manual acupuncture is promising and safe for individuals with overweight and obesity.
Acupuncture can be applied to reduce weight in both conditions: Overweight and obesity. It is in everyday practice of traditional Chinese medicine clinics and it is becoming more popular in many countries.
Traditional Chinese manual acupuncture refers to body acupuncture without any electrical stimulation. This type of acupuncture has been practicing for thousands of years in China and Asian countries.
The paper is well written and highlights an extraordinary, but interesting theme.
P- Reviewer: Shin BC, Xiong XJ S- Editor: Gong XM L- Editor: A E- Editor: Wu HL
| 1. | Bray GA, Champagne CM. Obesity and the Metabolic Syndrome: implications for dietetics practitioners. J Am Diet Assoc. 2004;104:86-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 34] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 2. | Patterson RE, Frank LL, Kristal AR, White E. A comprehensive examination of health conditions associated with obesity in older adults. Am J Prev Med. 2004;27:385-390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 168] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 3. | Anderson AS, Caswell S. Obesity management--an opportunity for cancer prevention. Surgeon. 2009;7:282-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 30] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 4. | Sharma AM, Iacobellis G. Treatment of obesity: a challenging task. Contrib Nephrol. 2006;151:212-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Brown A, Siahpush M. Risk factors for overweight and obesity: Results from the 2001 National Health Survey. Public Health. 2007;121:603-613 Available from: http://www.sciencedirect.com/science/article/B73H6-4NYJS2V-1/2/c716d2a7e74abca3d87b2fa65c6048bd. |
| 6. | Eby JG, Colditz GA. Obesity/overweight: Prevention and weight management. International Encyclopedia of Public Health. Oxford: Academic Press 2008; . |
| 7. | Rippe JM, Crossley S, Ringer R. Obesity as a chronic disease: modern medical and lifestyle management. J Am Diet Assoc. 1998;98:S9-15. [PubMed] |
| 8. | Ballinger A, Peikin SR. Orlistat: its current status as an anti-obesity drug. Eur J Pharmacol. 2002;440:109-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 175] [Cited by in RCA: 165] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 9. | Shippey SH, Macedonia CR. Surgical treatment of extreme obesity. Primary Care Update for OB/GYNS. 2003;10:278-283. |
| 10. | Lin XM, Li B, Du YH, Xiong J, Sun P. [Systematic evaluation of therapeutic effect of acupuncture for treatment of simple obesity]. Zhongguo Zhen Jiu. 2009;29:856-860. [PubMed] |
| 11. | Cho SH, Lee JS, Thabane L, Lee J. Acupuncture for obesity: a systematic review and meta-analysis. Int J Obes (Lond). 2009;33:183-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 103] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 12. | Sui Y, Zhao HL, Wong VC, Brown N, Li XL, Kwan AK, Hui HL, Ziea ET, Chan JC. A systematic review on use of Chinese medicine and acupuncture for treatment of obesity. Obes Rev. 2012;13:409-430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 101] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 13. | Higgins JPT, Green S, editors . Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration. Oxford: Academic Press 2011; . |
| 14. | Review Manager (RevMan) [Computer program]. Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration 2014; . |
| 15. | Dong XY. Clinical study of acupuncture for the treatment of simple obesity. Liaoning Zhongyi Zazhi. 2005;32:1070-1071. |
| 16. | Fan YX, Bai YH, Gui H. Effects of acupuncture for the treatment of simple obesity complicated with hyperlipedia. Ningxia Yike Daxue Xuebao. 2005;27:144-145. |
| 17. | Güçel F, Bahar B, Demirtas C, Mit S, Cevik C. Influence of acupuncture on leptin, ghrelin, insulin and cholecystokinin in obese women: a randomised, sham-controlled preliminary trial. Acupunct Med. 2012;30:203-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 62] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 18. | Luo HL, Li RH. Dianzhen dui danchunxing feipang shoushu ji zhiliansu de yingxiang. Acupunct Res. 2007;32:264-267. |
| 19. | Shen J, Hou Q. Effects of needling huatuojiaji for the treatment of simple obesity. Shanghai Zhenjiu Zazhi. 2000;19:29. |
| 20. | Tao HX. Clinical observation on simple obesity in Stomach-heat and dampness-stagnation type mainly by acupuncture. Liaoning Zhongyiyao Daxue Xuebao. 2009;11:169-170. |
| 21. | Tong J, Chen JX, Zhang ZQ, Pan Y, Zheng J, Yao H. Therapeutic effect of acupuncture therapy for simple obesity. Guangzhou Zhongyiyao Daxue Xuebao. 2010;27:579-582. |
| 22. | Wang XY, Li JZ. Study on effects of electrogastrography of simple obesity with acupuncture. Zhongguo Meirong Yixue. 2006;15:570-572. |
| 23. | Xu Z, Li R, Zhu C, Li M. Effect of acupuncture treatment for weight loss on gut flora in patients with simple obesity. Acupunct Med. 2013;31:116-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 24. | Eich H, Hannig M, Zimmermann E, Klieser E. Acupuncture in the treatment of psychoactive-drug-induced obesity - An experimental study. Deutsche Zeitschrift fur Akupunktur. 2005;48:6-11. |
| 25. | Hsu CH, Hwang KC, Chao CL, Lin JG, Kao ST, Chou P. Effects of electroacupuncture in reducing weight and waist circumference in obese women: a randomized crossover trial. Int J Obes (Lond). 2005;29:1379-1384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 45] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 26. | Wei QL, Liu ZC. Treatment of simple obesity with auricular acupuncture, body acupuncture and combination of auricular and body acupuncture. Zhongguo Linchuang Kangfu. 2004;8:4357-4359. |
| 27. | Lacey JM, Tershakovec AM, Foster GD. Acupuncture for the treatment of obesity: a review of the evidence. Int J Obes Relat Metab Disord. 2003;27:419-427. [PubMed] |
| 28. | Deadman P. A manual of acupuncture. England: Journal of Chinese Medicine Publications 2009; . |
| 29. | Akilen R, Pimlott Z, Tsiami A, Robinson N. The use of complementary and alternative medicine by individuals with features of metabolic syndrome. J Integr Med. 2014;12:171-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |