Published online Apr 26, 2015. doi: 10.13105/wjma.v3.i2.118
Peer-review started: November 5, 2014
First decision: January 20, 2015
Revised: February 13, 2015
Accepted: March 30, 2015
Article in press: April 2, 2015
Published online: April 26, 2015
Processing time: 174 Days and 4.1 Hours
AIM: To determine if the addition of hip-strengthening exercises decreases pain and improves function in patients with patellofemoral pain syndrome.
METHODS: The authors completed a systematic review searching eight databases (i.e., PubMed, Cochrane, CINHAL, MEDLINE, SportsDiscus, EMBASE, APTA Hooked on Evidence, and PEDro). Two independent reviewers screened and excluded studies if they did not meet the following inclusion criteria: subjects had a primary diagnosis of patellofemoral pain syndrome (PFPS), intervention group included hip-strengthening exercises, control group included a traditional physical therapy intervention, study included outcome measures of pain and/or function, study used a randomized controlled trial design, PEDro score was ≥ 7, and study was published in a peer-reviewed journal. Primary outcome measures were subjective scales of pain and function. These measures were converted to standardized mean difference [effect size (ES)], and a random-effects model was used to calculate the overall ES.
RESULTS: Two hundred eighty-three studies were screened for inclusion in our meta-analysis. Nine studies were deemed suitable for data extraction and analysis. A total of 426 subjects were used in the nine studies. Overall, there was a significant positive effect of hip-strengthening exercises on measures of pain and function in subjects with PFPS (ES = 0.94, P = 0.00004). None of the individual studies had a negative ES, with study ES ranging from 0.35 to 2.59. Because of the high degree of between-study variance (I2 = 76%; Q = 34.0, P < 0.001), subgroup meta-analyses and meta-regressions were performed. None of the potential moderator variables that were investigated (e.g., outcome type, hip region targeted, duration of treatment) could explain a significant amount of the between-study variance in ES (P≥ 0.23).
CONCLUSION: Overall, the addition of hip-strengthening exercises to traditional physical therapy produced greater improvements in measures of pain and function.
Core tip: The most effective treatment to improve pain and function in patellofemoral pain syndrome is uncertain. We performed a systematic review and meta-analysis to determine if the addition of hip-strengthening exercises to traditional physical therapy interventions could effectively reduce pain and increase function in patients with patellofemoral pain syndrome. Our analysis indicates that the addition of hip-strengthening exercises provides a significant and relatively large additional reduction in pain and increase in function.
- Citation: Morelli KM, Carrelli M, Nunez MA, Smith CA, Warren GL. Addition of hip exercises to treatment of patellofemoral pain syndrome: A meta-analysis. World J Meta-Anal 2015; 3(2): 118-124
- URL: https://www.wjgnet.com/2308-3840/full/v3/i2/118.htm
- DOI: https://dx.doi.org/10.13105/wjma.v3.i2.118
Patellofemoral pain syndrome (PFPS) is a prevalent lower-extremity disorder. PFPS can account for over 10% of physician office visits in an orthopedic setting, and account for 25%-40% of patients with knee pain and/or injury[1-4]. Women are twice as likely to be affected compared to men[3,5-7]. The etiology of PFPS has historically been attributed to abnormal tracking of the patella resulting from abnormal muscle forces, either weakness or tightness, and/or biomechanical factors (e.g., Q angle, shallow trochlear groove) that alter the normal compressive and shear forces at the patellofemoral joint[1-8]. Lateral tracking of the patella can occur with an excessive Q angle at the knee, which is a measure of the angle of pull of the knee extensors in relation to the patellar tendon[2,3,8]. However, there is no consensus on PFPS’s etiology.
Factors proximal to the patellofemoral joint are emerging as possible significant contributors to the cause of PFPS. There is a recent focus on the role of the hip abductor muscles in controlling the genu valgum angle at the knee during dynamic activity, finding that weakness of the hip abductors leads to an increased adduction/genu valgum moment with activity[8-10]. Weakness of the hip external rotators and extensors may also contribute to increased adduction and internal rotation of the lower leg with activity, thereby increasing biomechanical forces of shear and compression at the patellofemoral joint[10].
Traditional physical therapy interventions have focused on knee extensor strengthening, as well as bracing, taping, and modalities in treating patients with PFPS[2]. Often times, interventions focused strictly at the knee joint and knee extensors are not successful at decreasing a patient’s pain complaint[2]. With the recent interest in the role of the proximal hip joint musculature contributing to PFPS, the objective of this study was to determine, utilizing a systematic review and meta-analysis, if the addition of hip-strengthening exercises to a traditional physical therapy intervention reduces pain and improves function in patients with PFPS more so than the traditional physical therapy intervention alone.
We reviewed the research literature to identify studies that examined the effects of hip-strengthening exercises on pain and functional limitations in patients with PFPS. Our literature search began September 2013 and continued through October 2014. Databases including PubMed, Cochrane, CINHAL, MEDLINE, SportsDiscus, EMBASE, APTA Hooked on Evidence, and PEDro were searched electronically. The search terms included: “patellofemoral AND hip strength*” and MeSH terms (patellofemoral pain syndrome/rehabilitation AND hip) OR (patellofemoral pain syndrome/therapy AND hip).
Study inclusion and exclusion criteria: Two independent reviewers screened and excluded studies if they did not meet the following inclusion criteria: (1) study utilized subjects with a principal medical diagnosis of patellofemoral pain syndrome; (2) study included a treatment group performing hip-strengthening exercises in combination with or without a traditional physical therapy intervention; (3) study included a control group performing a traditional physical therapy intervention; (4) study named the muscles or muscle region targeted with exercises performed; (5) study measured pain or function as outcomes; (6) studies were randomized controlled trials and had a PEDro score greater than or equal to 7[11]; and (7) study was published in a peer-reviewed journal.
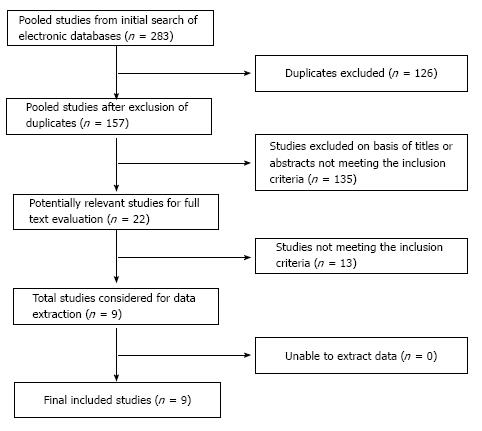
Selection of studies: Two hundred eighty-three studies were identified through the database searches and review of article reference lists. Of those, 126 studies were eliminated as duplicates among the different databases. Then, 135 studies were excluded on the basis of the title and/or review of the abstract. Twenty-two studies were fully evaluated via a careful review of the full text. On the basis of the inclusion and exclusion criteria, 13 studies were excluded leaving a total of nine studies to be included in the meta-analysis[12-20] (Figure 1).
Data extraction: For the meta-analysis, pain and function as reported by the numeric pain rating scale (NPRS), pain visual analog scale (VAS), Kujala anterior knee pain scale (AKPS), lower extremity functional scale (LEFS), and Womac pain rating scale data were extracted in the form of means, standard deviations, and sample sizes for the intervention (i.e., group employing hip-strengthening exercises) and control groups. The number of sessions, region of hip targeted, total duration of treatment sessions, time for follow-up assessments, and subject descriptive measures were also extracted from the studies. The region of the hip targeted with exercise was extracted from the studies, and categorized as posterolateral if the exercises were isolated to the posterolateral hip muscles or general if the exercises involved the major thigh and muscles that cross the hip joint. The time for follow-up was extracted from the studies and categorized as immediate follow-up if outcome assessments were done when the intervention ceased or as long-term for any assessment performed 3 or more months after the intervention ceased. Exercise intensity was extracted for all studies but was not found to be usable because of the variability among studies in how intensity was expressed or because it varied within and between sessions in some studies but not in others.
The extracted pain and functional measures data were converted to a standard format, i.e., standardized mean difference, which will be referred to as an effect size (ES) from this point on. Meta-analyses were run using the random-effects model that accounts for true between-study variation in effects as well as random error within each study. A random-effects model was employed for this analysis because the nine studies used dissimilar experimental designs and/or procedures[21]. Between-study variance was assessed using the Q value and I2. Because substantial between-study variance was detected, we sought to determine the role that different experimental factors might have in explaining this variance. These factors can be treated as potential moderator variables. Meta-regressions (using a methods of moment model) or subgroup meta-analyses were used to probe the following potential moderator variables: region of hip targeted during the hip exercises, number of exercise sessions, duration in weeks of exercise intervention, control group type, outcome type, and time of follow-up. Subgroup meta-analyses and meta-regressions were used for analysis of categorical and continuous variables, respectively. In studies with more than one experimental factor level being evaluated (e.g., a study using both pain and function outcomes in the subgroup meta-analysis evaluating the effect of outcome type), an ES was calculated for each level and was treated as if it originated from an independent study.
Meta-analyses were conducted using comprehensive meta-analysis software (version 2.2; Biostat Inc., Englewood, NJ). An α level of 0.05 was used in all analyses. Effect sizes of 0.2, 0.5, and 0.8 were considered to be small, moderate and large respectively[22]. The possible effect of publication bias on the meta-analysis was assessed by visual assessment of a funnel plot and using Duval and Tweedie’s trim and fill correction.
In total, nine studies were included in the meta-analysis examining the effect of hip-strengthening exercises on pain and function in persons with PFPS. The characteristics of these studies are summarized in Table 1. All nine studies were published in peer-reviewed journals and used a randomized controlled trial design. Subjects were randomly assigned to the two groups, i.e., one receiving a traditional intervention and one receiving traditional intervention plus hip exercises. Therapy providers were not blinded to which group they were assigned to. Assessors administering the outcome assessments (i.e., Pain VAS, NPRS, LEFS, and Kujala AKPS) were blinded to the groups that the subjects were assigned to; however, subjects completed these questionnaires and were aware of the group they were assigned to. All but one study included measures of both pain and function; the one study included only a measure of pain[18]. Seven of the studies measured outcomes immediately after completing the intervention[12,14-19], while two studies did not make assessments of pain and function until at least 3 mo post intervention[13,20]. Dolak et al[12] made a follow-up assessment at 1 and 2 mo post intervention; however, this data was not included in the analysis because the exercise regimen changed after post-treatment and did not meet our inclusion criteria. Witvrouw et al[20] made a follow-up assessment at 5 years post intervention; however, these data were not included in the analysis because baseline measures were not available for the subjects who reported for the 5-year follow-up and subjects were inconsistent in adhering to their exercise regimen during this period. Six studies specified hip exercises as targeting the posterolateral musculature of the hip, such as hip abduction, hip lateral rotation and hip extension[12-14,16-18], while three studies’ hip exercises were considered general to the hip musculature[15,19,20]. A total of 426 subjects were used in the nine studies. Subject gender in the studies was generally a mixture of men and women but one study used men only[15] and three studies used women only[12-14]. The duration of intervention varied among studies from 4 to 12 wk, with total number of treatment sessions ranging from 12 to 84.
| Ref. | Subject information | Subject mean age (min-max) | Hip region targeted | Outcome measured | Time to follow-up (mo) | Number of exercise sessions | Exercise duration (wk) | PEDro quality score (0-11) |
| Dolak et al[12] | 33 women | 25.5 | Posterolateral | Pain VAS and LEFS | 0, 11, 21 | 12 | 4 | 7 |
| (16-35) | ||||||||
| Fukuda et al[14] | 41 women | 25 | Posterolateral | NPRS, Kujala AKPS, LEFS | 0 | 12 | 4 | 9 |
| (20-40) | ||||||||
| Fukuda et al[13] | 49 women | 22.5 | Posterolateral | NPRS, Kujala AKPS, LEFS | 3, 6, 12 | 12 | 4 | 9 |
| (20-40) | ||||||||
| Herrington et al[15] | 30 men | 26.9 | General | Pain VAS, Kujala AKPS | 0 | 18 | 6 | 9 |
| (18-35) | ||||||||
| Ismail et al[16] | 32 (9 men, 23 women) | 21 | Posterolateral | Pain VAS, Kujala AKPS | 0 | 18 | 6 | 8 |
| (18-30) | ||||||||
| Khayambashi et al[17] | 36 (18 men, 18 women) | 27.8 | Posterolateral | Pain VAS, Womac | 0, 6 | 24 | 8 | 7 |
| (12-44) | ||||||||
| Nakagawa et al[18] | 14 (4 men, 10 women) | 23.6 | Posterolateral | Pain VAS | 0 | 30 | 6 | 10 |
| (17-40) | ||||||||
| van Linschoten et al[19] | 131 (47 men, 84 women) | 24 | General | Pain VAS, Kujala AKPS | 0, 9 | 84 | 12 | 7 |
| (14-40) | ||||||||
| Witvrouw et al[20] | 60 (20 men, 40 women) | 20.3 | General | Pain VAS, Kujala AKPS | 3, 601 | 15 | 5 | 8 |
| (14-33) |
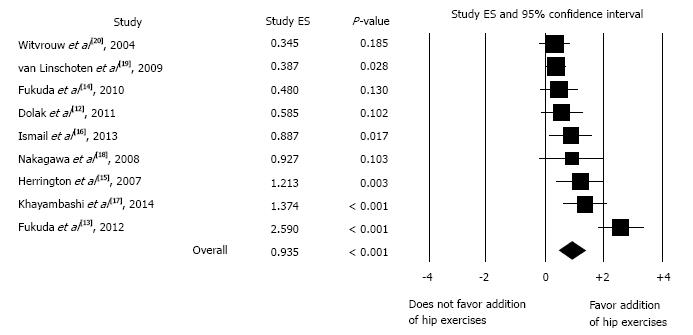
When combining all outcome types and times for follow-up, meta-analysis of all nine studies yielded a statistically significant and large effect size (ES = 0.94, P = 0.00004), indicating that patients with PFPS performing hip exercises in addition to traditional physical therapy interventions reported less pain and increased function than control subjects receiving traditional interventions (Figure 2). None of the individual studies had a negative ES, with the standardized mean difference ranging from 0.35 to 2.59. No one study was found to dominate the calculation of the overall ES. Fukuda et al[13] 2012 had the single largest effect on the overall ES but even if it was removed from the analysis, the overall ES was still moderate-to-large and statistically significant (ES = 0.67, P = 0.000001). Publication bias also did not appear to affect the overall ES. We did not observe any overt asymmetry in the funnel plot of standard error versus study ES. Furthermore, when the Duval and Tweedie’s trim and fill adjustment was applied to correct for potential publication bias, no studies were trimmed and thus the procedure made no adjustment to the overall ES.
The two assessments of variation in ES among the studies indicate that the variation is both large (I2 = 76%) and statistically significant (Q = 34.0, df = 8, P < 0.001). Because of this variability, subgroup meta-analyses and meta-regressions were used to probe possible roles for six experimental factors that might help to explain ES variation among the nine studies. Table 2 summarizes the findings of those analyses. None of the experimental factors were able to significantly account for any ES variation. Subgroup analysis of outcome type, time of follow-up, control group type, and hip region targeted with exercise indicated that these variables could not explain a significant amount of the between-study ES variation (P≥ 0.23). Using meta-regression, it was determined that exercise duration in number of weeks and the total number of treatment sessions also could not explain a significant amount of the between-study ES variation (P≥ 0.38).
| Moderator variable | Comparison (or slope for continuous variables) | P value |
| Outcome type | Function (n = 8, ES = 0.92) vs Pain (n = 9, ES = 0.95) | 0.95 |
| Time of follow-up | Immediate (n = 7, ES = 0.79) vs Long term (n = 4, ES = 1.111) | 0.44 |
| Control group type | Knee extensor strengthening only (n = 6, ES = 1.15) vs Knee extensor strengthening plus other (n = 3, ES = 0.56) | 0.24 |
| Hip region targeted with exercise | General hip (n = 3, ES = 0.60) vs Posterolateral hip (n = 6, ES = 1.13) | 0.23 |
| Number of exercise sessions | -0.009/session | 0.38 |
| Number of weeks of exercise | -0.066/wk | 0.48 |
The main finding of this study is that in persons diagnosed with patellofemoral pain syndrome the addition of hip-strengthening exercises to traditional physical therapy produced greater improvements in measures of pain and function than traditional therapy alone. Given this finding, developing a targeted program to strengthen both the hip and knee musculature as opposed to alternatives such as strengthening only the knee extensors may lead to fewer number of physical therapy and doctor visits and overall quicker recovery times. Interestingly, the number of exercise sessions and/or number of weeks of exercise intervention did not appear to affect the variation between studies in the effectiveness of the hip-strengthening exercises.
There are several potential limitations of our systematic review and meta-analysis, as well as some methodological concerns with the underlying studies themselves. One possible limitation of our systematic review was publication bias. Publication bias occurs when published research is systematically unrepresentative of the total population of studies[21]. Studies with non-significant and/or negative findings are less likely to be published, and this may influence the overall ES in a meta-analysis that is based largely on published studies. Publication bias was assessed in our review by examination of the funnel plot. Additionally, the Duval and Tweedie’s trim and fill adjustment was applied but there was no correction to the overall ES. But because of the relatively few studies, the sensitivity of these analyses could be lacking. Furthermore, we did not rigorously examine the grey literature for unpublished studies.
A second potential limitation of our analysis was the inability to explain the substantial between-study variance in ES. Subgroup analyses and meta-regressions did not identify any experimental factors that could help explain this variance. Many of these analyses probably did not have adequate statistical power because of the limited number of studies in the review and because some subgroups had as few as three studies in them. We tried to assess the ability of gender to explain the between-study variance in ES but could not run a subgroup analysis on gender because there was only one study that used only male subjects. Another concern of the systematic review and meta-analysis is that the exercises performed in each study were categorized by the region of the thigh the exercises targeted (i.e., knee extensors, general hip, posterolateral hip) vs listing each specific exercise performed. Thus, we were not able to assess how the performance of specific exercises might explain the between-study variance in ES and enable us to hypothesize a particular exercise to be more effective in reducing pain and improving function in patellofemoral pain syndrome. We also were not able to assess if the exercise intensity for the interventions might explain the between-study variance in ES.
A third potential limitation of our analysis is the inability to completely blind the subjects and therapy providers within the individual studies. All studies are randomized control trials with random assignment of subjects to groups. Subjects that have basic knowledge of anatomy and exercise would likely be aware of which group they were assigned to. While assessors administering the outcome assessment tools (i.e., Pain VAS, NPRS, LEFS, and Kujala AKPS) were blinded to subject group assignment, the subjects themselves completed the outcome tools which consists of questionnaires. Whether an assessor is blinded or not should not affect how a subject completes these forms.
This study’s findings provide justification for future research. All study ES including the overall ES were positive, suggesting that despite the large variation in experimental design among studies, the addition of hip strengthening to traditional physical therapy interventions is beneficial in reducing pain and function in patellofemoral pain syndrome when compared to traditional knee-focused interventions alone. Future research examining whether hip-strengthening exercises are equally effective in men and women is important to know, especially when considering that women are more frequently diagnosed with patellofemoral pain syndrome. It would also be helpful, with a larger number of studies, to be able to identify individual hip exercises that are more beneficial than others in decreasing pain and improving function.
Patellofemoral pain syndrome (PFPS), is a common disorder of the knee. There is no consensus on the etiology of PFPS, however there is an emerging focus on the contribution of proximal structures, i.e., the hip, on PFPS. Traditional therapeutic exercises performed to address PFPS focus on strengthening the knee extensor muscles.
Interventions targeting the more proximal segment, the hip, in treating PFPS are becoming more of a focus in rehabilitation than targeting the knee extensor muscles alone.
Previous systematic reviews that looked at PFPS only performed review of the literature. The present study included more high quality studies and performed a meta-analysis to quantitatively assess the effect of hip exercises on PFPS compared to traditional interventions.
The present study suggests that the addition of hip strengthening exercises to traditional therapy improves pain and function in patients with PFPS.
Patellofemoral pain syndrome is a diagnosis characterized by anterior knee pain surrounding the patella.
The authors present a well written manuscript with a sound conclusion.
P- Reviewer: Lee SP, Mashreky SR, van der Veen HC S- Editor: Qi Y L- Editor: A E- Editor: Lu YJ
| 1. | Bizzini M, Childs JD, Piva SR, Delitto A. Systematic review of the quality of randomized controlled trials for patellofemoral pain syndrome. J Orthop Sports Phys Ther. 2003;33:4-20. [PubMed] [DOI] [Full Text] |
| 2. | Bolgla LA, Boling MC. An update for the conservative management of patellofemoral pain syndrome: a systematic review of the literature from 2000 to 2010. Int J Sports Phys Ther. 2011;6:112-125. [PubMed] |
| 3. | Petersen W, Ellermann A, Gösele-Koppenburg A, Best R, Rembitzki IV, Brüggemann GP, Liebau C. Patellofemoral pain syndrome. Knee Surg Sports Traumatol Arthrosc. 2014;22:2264-2274. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 139] [Cited by in RCA: 150] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 4. | Rixe JA, Glick JE, Brady J, Olympia RP. A review of the management of patellofemoral pain syndrome. Phys Sportsmed. 2013;41:19-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 5. | Baldon Rde M, Serrão FV, Scattone Silva R, Piva SR. Effects of functional stabilization training on pain, function, and lower extremity biomechanics in women with patellofemoral pain: a randomized clinical trial. J Orthop Sports Phys Ther. 2014;44:240-A8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 104] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 6. | Boling M, Padua D, Marshall S, Guskiewicz K, Pyne S, Beutler A. Gender differences in the incidence and prevalence of patellofemoral pain syndrome. Scand J Med Sci Sports. 2010;20:725-730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 343] [Cited by in RCA: 410] [Article Influence: 29.3] [Reference Citation Analysis (0)] |
| 7. | Nakagawa TH, Baldon Rde M, Muniz TB, Serrão FV. Relationship among eccentric hip and knee torques, symptom severity and functional capacity in females with patellofemoral pain syndrome. Phys Ther Sport. 2011;12:133-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 8. | Powers CM. The influence of altered lower-extremity kinematics on patellofemoral joint dysfunction: a theoretical perspective. J Orthop Sports Phys Ther. 2003;33:639-646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 589] [Cited by in RCA: 561] [Article Influence: 25.5] [Reference Citation Analysis (0)] |
| 9. | Ferber R, Kendall KD, Farr L. Changes in knee biomechanics after a hip-abductor strengthening protocol for runners with patellofemoral pain syndrome. J Athl Train. 2011;46:142-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 143] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 10. | Peters JS, Tyson NL. Proximal exercises are effective in treating patellofemoral pain syndrome: a systematic review. Int J Sports Phys Ther. 2013;8:689-700. [PubMed] |
| 11. | Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83:713-721. [PubMed] |
| 12. | Dolak KL, Silkman C, Medina McKeon J, Hosey RG, Lattermann C, Uhl TL. Hip strengthening prior to functional exercises reduces pain sooner than quadriceps strengthening in females with patellofemoral pain syndrome: a randomized clinical trial. J Orthop Sports Phys Ther. 2011;41:560-570. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 131] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 13. | Fukuda TY, Melo WP, Zaffalon BM, Rossetto FM, Magalhães E, Bryk FF, Martin RL. Hip posterolateral musculature strengthening in sedentary women with patellofemoral pain syndrome: a randomized controlled clinical trial with 1-year follow-up. J Orthop Sports Phys Ther. 2012;42:823-830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 103] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 14. | Fukuda TY, Rossetto FM, Magalhães E, Bryk FF, Lucareli PR, de Almeida Aparecida Carvalho N. Short-term effects of hip abductors and lateral rotators strengthening in females with patellofemoral pain syndrome: a randomized controlled clinical trial. J Orthop Sports Phys Ther. 2010;40:736-742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 133] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 15. | Herrington L, Al-Sherhi A. A controlled trial of weight-bearing versus non-weight-bearing exercises for patellofemoral pain. J Orthop Sports Phys Ther. 2007;37:155-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 63] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 16. | Ismail MM, Gamaleldein MH, Hassa KA. Closed kinetic chain exercises with or without additional hip strengthening exercises in management of patellofemoral pain syndrome: a randomized controlled trial. Eur J Phys Rehabil Med. 2013;49:687-698. [PubMed] |
| 17. | Khayambashi K, Fallah A, Movahedi A, Bagwell J, Powers C. Posterolateral hip muscle strengthening versus quadriceps strengthening for patellofemoral pain: a comparative control trial. Arch Phys Med Rehabil. 2014;95:900-907. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 48] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 18. | Nakagawa TH, Muniz TB, Baldon Rde M, Dias Maciel C, de Menezes Reiff RB, Serrão FV. The effect of additional strengthening of hip abductor and lateral rotator muscles in patellofemoral pain syndrome: a randomized controlled pilot study. Clin Rehabil. 2008;22:1051-1060. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 135] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 19. | van Linschoten R, van Middelkoop M, Berger MY, Heintjes EM, Verhaar JA, Willemsen SP, Koes BW, Bierma-Zeinstra SM. Supervised exercise therapy versus usual care for patellofemoral pain syndrome: an open label randomised controlled trial. BMJ. 2009;339:b4074. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 118] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 20. | Witvrouw E, Danneels L, Van Tiggelen D, Willems TM, Cambier D. Open versus closed kinetic chain exercises in patellofemoral pain: a 5-year prospective randomized study. Am J Sports Med. 2004;32:1122-1130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 88] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 21. | Borenstein MHL, Higgins J, Rothstein HR. Introduction to meta-analysis. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale (NJ): Lawrence Erlbaum Associates 1988; . |
| 22. | Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale (NJ): Lawrence Erlbaum Associates 1988; . |