Published online Feb 26, 2015. doi: 10.13105/wjma.v3.i1.54
Peer-review started: October 27, 2014
First decision: November 14, 2014
Revised: December 16, 2014
Accepted: December 29, 2014
Article in press: December 31, 2014
Published online: February 26, 2015
Processing time: 87 Days and 14.1 Hours
AIM: To estimate the pooled prevalence of hypertension in Zimbabwe and describe its trend since independence in 1980 using secondary source data.
METHODS: MEDLINE, EMBASE and Scopus databases from April 1980 to December 2013 were searched for population and community based studies on the prevalence of hypertension among adults (≥ 18 years) in Zimbabwe. The key words used were “prevalence”, “epidemiologic studies”, “hypertension” or “high blood pressure”, based on the cut-off (≥ 140 mmHg systolic blood pressure and/or ≥ 90 mmHg diastolic blood pressure). We conducted a meta-analysis on the published studies, using the random-effects model to estimate the pooled prevalence.
RESULTS: The search retrieved 87 publications, of which four studies met the selection criteria. The four studies had a total of 4829 study participants between 1997 and 2010 across 5 provinces in Zimbabwe. Two studies were in urban areas, while the other two had mixed study settings (urban and rural). The overall pooled prevalence of hypertension was 30% (95%CI: 19%, 42%, I2= 98%, χ2 = 164.15, P = 0.00).
CONCLUSION: Our results show a high prevalence of hypertension in Zimbabwe, with urban areas having higher prevalence than rural areas.
Core tip: A systematic review and meta-analysis of studies on the prevalence of hypertension in Zimbabwe, from April 1980 to December 2013 reveals a high prevalence of 30%. Hypertension prevalence was higher in studies in urban settings compared with studies in mixed settings (urban and rural), indicating the increase of cardiovascular risk factors associated with urbanization and economic progress. The development of national prevention policies and control strategies for hypertension are critical to reduce the increasing burden of hypertension in Zimbabwe.
- Citation: Mutowo MP, Mangwiro JC, Lorgelly P, Owen A, Renzaho AM. Hypertension in Zimbabwe: A meta-analysis to quantify its burden and policy implications. World J Meta-Anal 2015; 3(1): 54-60
- URL: https://www.wjgnet.com/2308-3840/full/v3/i1/54.htm
- DOI: https://dx.doi.org/10.13105/wjma.v3.i1.54
Hypertension-related conditions are the most common cause of death from non-communicable diseases (NCDs) in sub-Saharan Africa[1]. Hypertension is recognized as a global public health crisis due to it being asymptomatic and its high mortality rate[2]. The prevalence of hypertension is estimated at 22.9% in developing countries and 37.3% in developed countries[3]. Unfortunately, Zimbabwe faces the particular challenge of high morbidity and mortality from communicable diseases and increasing prevalence of NCDs[4]. NCDs accounted for an estimated 21% of total deaths in 2008 in Zimbabwe[5] and hypertension was ranked first amongst the NCD outpatient visits recorded in Zimbabwean public hospitals in 2006[4]. The limited data available suggests that there was a four-fold increase in the prevalence of hypertension from 1990 to 1997[6], and the age-standardized rate of hypertension in Zimbabwe (33.1%) was reported in one study to be higher than that seen in developed countries such as United States of America (20.3%), Canada (21.4%) and England (29.6%)[3].
Urbanization has resulted in the westernization of lifestyles in parts of Zimbabwe. In urban areas, diets high in refined, starchy carbohydrates are leading to high obesity rates and increased prevalence of hypertension, diabetes and cardiovascular diseases[7]. Hypertension awareness is low, resulting in inadequate treatment and management of hypertension in the Zimbabwean population, and hence there is an urgent need for a national policy for the prevention and control of hypertension in Zimbabwe[8]. This should include a major focus on prevention, as this may be more cost effective for a developing country with limited resources[9]. This will require development of evidence-based prevention strategies, which must be informed by a clear understanding of the hypertension burden across the country. However in Zimbabwe, as in many other resource-limited settings, the infrastructure available to enable detailed disease surveillance activities is lacking and no national studies on hypertension prevalence in Zimbabwe are available. The purpose of this study was to systematically review the epidemiological results of published studies and estimate the pooled prevalence of hypertension in Zimbabwe using meta-analysis.
The systematic review and meta-analysis was conducted according to the recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Group[10]. Published epidemiologic studies on the prevalence of hypertension we searched for between April 1980 and December 2013 in three electronic databases: MEDLINE, EMBASE and Scopus. The medical subject headings (MeSH) terms used in all databases were (“hypertension” OR “high blood pressure”) AND (“prevalence” OR “epidemiological studies”) AND (“Zimbabwe”). Prior to the national independence of Zimbabwe, on 18 April 1980, the nation had been known by several names including Rhodesia, Southern Rhodesia, and Zimbabwe-Rhodesia. We further searched the grey literature databases and individual Zimbabwean public health institute websites for relevant studies.
Inclusion criteria for studies included studies on the prevalence of hypertension or high blood pressure, conducted among Zimbabwean residents (≥ 18 years old); population or community studies that were cross-sectional or cohort studies and cut off points for hypertension were systolic blood pressure (SBP) (≥ 140 mmHg) and/or diastolic blood pressure (DBP) (≥ 90 mmHg).
Studies had to abide by the hypertension diagnostic criteria of the Seventh Report of the Joint National committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC7)[11], and/or the 1999 World Health Organization (WHO)/International Society of Hypertension (WHO/ISH) classification of blood pressure levels[12], and/or the 2003 WHO/ISH Statement on Management of Hypertension[13], whose cut-off points are based on 140/90 mmHg. Studies conducted before 1999 had blood pressure cut-off points defined as ≥ 160/95 mmHg. Subgroup prevalence based on the cut-off point based on 140/90 mmHg was included from these studies. Articles were excluded if the participants were limited to gender (male or female only), pregnant participants, studies conducted on animals, editorial letters, abstracts, and reviews of original studies.
Identified studies were screened by two independent reviewers (MM and AR) to confirm whether they satisfied the inclusion criteria. Lack of consensus about study selection was resolved through discussions with a third author (JC). Retrieved articles and their reference lists were searched for additional publications.
All data was independently extracted by the two reviewers (MM and AR), cross-checked and any disagreements were resolved by consensus. The following information was recorded from the included studies: author, year of publication, year of investigation, study period, study setting, sampling frame and method, sample size, age range of study population, reported prevalence, and diagnostic method and criteria used in the study.
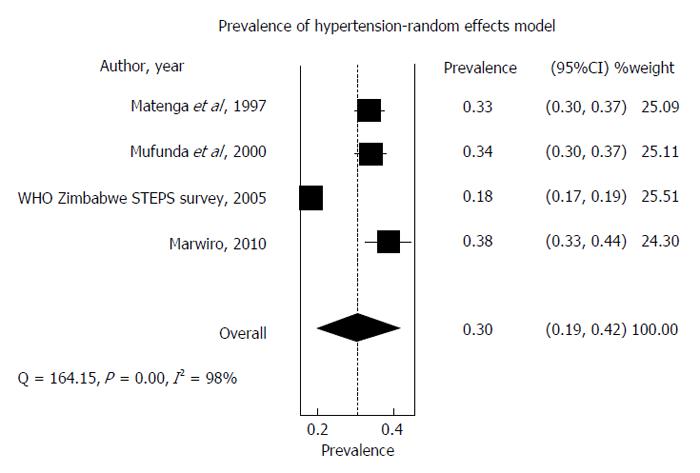
The Cochran Q test or χ2 and the I2 statistic were used to evaluate and quantify statistical heterogeneity[14,15]. The values for χ2 and I2 (low is < 25%, moderate 25%-50%, high > 50%) are mentioned in the forest plot used to visualize the magnitude of heterogeneity among studies. As the differences between studies were very large (I2 = 98%), we used a random-effects model to estimate the prevalence of hypertension and calculate the 95%CI[15]. All statistical analysis was done using MetaXL 1.4, Software[16]. The statistical methods of this study were reviewed by Dr. Baki Billah, Senior Biostatistician Consultant and Senior Lecturer in Biostatistics, from Monash University, Australia.
Dr. Baki Billah, Senior Biostatistician Consultant and Senior Lecturer in Biostatistics at Monash University reviewed and confirmed that the statistical approach reported in the manuscript was adequate and correct.
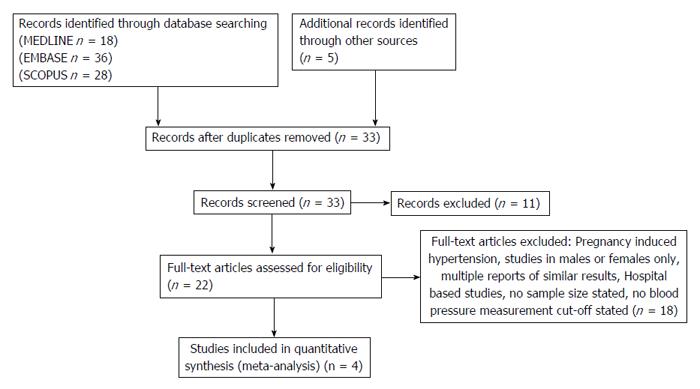
We initially identified 87 references from our search: 82 from electronic databases and 5 from other sources (Figure 1). After the application of inclusion and exclusion criteria, and removing duplications, as described in Methods, we selected four studies for the meta-analysis.
The four studies[8,17-19] were conducted across five provinces in Zimbabwe. The studies had a total of 4829 subjects and the enrollment years of the studies ranged from 1997 to 2010. Two studies[8,17] conducted in predominately urban areas, had a total sample size of 1077, while the other two studies[18,19], conducted in both urban and rural settings, had a total sample size of 3752. The four studies did not state age-specific data related to gender, and age was limited to above 25 years old in the four studies. Two studies[17,19] stated the use of JNC7 and WHO/ISH 2003 classifications, while the other two used cut-off points within the inclusion criteria.
Awareness of hypertension was found to be low and treatment and management of hypertension inadequate in one study sample[8]. One study reported a prevalence which was higher in females than in males and a family history of hypertension which was strongly associated with hypertension in participants in the study[19]. The commonly reported family members were mothers of participants and on stratified analysis, the association of hypertension and family history of hypertension was stronger in females than males. The study reported a high prevalence of abdominal obesity which is a powerful determinant of subsequent risk of hypertension[19]. Three studies reported the use of standardized measurement protocols, utilizing nurses or certified personnel for blood pressure measurement, with validity of readings done by a supervising physician[8,17,19]. Blood pressure was measured two times in a single visit in two studies[17,18], three times in a single visit in one study and the process for obtaining blood pressure readings was not reported in one study[8,19]. Two studies used standard mercury sphygmomanometer to measure blood pressure[8,17]; one study used digital blood pressure machines[19], while no specific instrument was reported for the remaining study[18].
Based on the reported hypertension prevalence in the included studies, Bulawayo (south Zimbabwe) had the highest prevalence of 38.4% (95%CI: 33%-44%)[19]. The lowest prevalence of 17.9% (95%CI: 17%-19%) was recorded across three provinces in mixed study setting (urban and rural)[17] (Table 1 summarizes the extracted data from included studies). Using the random-effects model for the meta-analysis, the overall hypertension prevalence is estimated to be 30% (95%CI: 19%-42%, I2 = 98%, χ2 = 164.15, P = 0.00) (Figure 2).
| Ref. | Study period | Setting | Sampling method | Sample size | Age range (yr) | Prevalence (cases) | Diagnostic criteria | Description of geographic area1 |
| Matenga et al[8] | October to early December 1996 | Community-household | Random | 749 | > 34 | 33.4% (250) | Hypertensive described as mean diastolic BP > 94 mmHg untreated or on antihypertensive medication, controlled BP described as mean DBP < 95 mmHg while on drug treatment | Marondera, Mashonaland East (mainly urban and unspecified rural area) |
| Hakim et al[17] | May to July 2005 | Subnational-household | Multi-stage | 3003 | ≥ 25 | 17.9% (538) | Systolic ≥ 140 and/or diastolic ≥ 90 mmHg | Urban and mainly rural communities in Midlands, Mashonaland Central, and Matebeleland South |
| Mufunda et al[18] | July-October 1995 | Community-household | Cluster sampling | 775 | > 25 | 33.5% (260) | Systolic ≥ 140 mmHg and diastolic ≥ 90 mmHg and/or antihypertensive medication | Marondera, Mashonaland East (urban) |
| Marwiro[19] | June-July, 2010 | Community-employee register | Systematic | 302 | > 25 to > 55 | 38.4% (116) | The 7th Report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure. Hypertension stage 1: systolic 140-159 mmHg, diastolic 90-99 mmHg, Hypertension stage 2: systolic ≥ 160 mmHg, diastolic ≥ 100 mmHg | Bulawayo (urban) |
There is a shortage of national data on hypertension prevalence in Zimbabwe. This study summarized the prevalence of hypertension in Zimbabwe over a 14 year period (1997 to 2010). The estimated pooled prevalence for hypertension for the 14 year period was 30%, however as this was not age-standardized and is likely to be an under-estimate. The hypertension prevalence for Zimbabwe, estimated by the WHO was higher at 39% for both genders aged at least 25 years, 38.2% (95%CI: 29.9-46.9) in men and 39.9% (95%CI: 30.4-49.4) in women[20]. However, concerns remain over the different cut-off points used for hypertension measurement in prevalence studies, data sources and modelling methodology and assumptions used, so this creates difficulties in comparing prevalence rates across Africa[21-23].
Despite this, the observed trend towards increasing hypertension prevalence in our meta-analysis is congruent with the literature. Studies have indicated that the prevalence of hypertension has increased in developing countries over recent decades, with hypertension increasingly prevalent in lower socio-economic groups with limited access to essential treatment[24,25].
Hypertension was found to be higher in the urban Zimbabwe population[8,19]. Rapid urbanization and lifestyle changes have been implicated in the development of hypertension in African urban populations, notably adoption of Western-type diet, physical inactivity and increased psychosocial stress[6]. Hypertension was found to be prevalent in the lowest income groups, more common in women, linked with overweight and obesity and in heavy alcohol consumers in low income countries[25]. The Zimbabwe National Health Strategy reports that the prevalence of hypertension in Zimbabwe is increasing mainly because of physical inactivity, tobacco smoking, high salt diet and excessive alcohol consumption[4]. Therefore preventive measures need to take into account urban planning, whereby effective policies can promote physical activity through re-designing the landscape.
Hypertension is generally asymptomatic until chronic vascular disease develops, with the risk of disease doubling with each blood pressure reading increase of 20/10 mmHg, beginning at lower readings of 115/75 mmHg[21]. The lack of symptoms contributes not only to the lack of awareness of the condition in those who have it, but also reduces the levels of compliance and persistence with blood pressure lowering interventions, as an improvement in blood pressure control may not result in perceptible benefit to the individual[25]. The largest cause of years of life lost in low income countries is cardiovascular disease[25], and with a growing prevalence of hypertension, the burden of cardiovascular diseases in Zimbabwe is likely to increase, which has significant implications for healthcare, individual wellbeing and social stability.
The limited number of population-based studies on hypertension prevalence and risk factors may have contributed to its low priority as a public health problem in Zimbabwe, when compared to higher profile communicable diseases like human immunodeficiency virus infection and acquired immune deficiency syndrome (HIV/AIDS), malaria and tuberculosis. Unlike HIV/AIDS, hypertension is not considered a health priority in Zimbabwe, and no national hypertension program has been established to date. However the HIV/AIDS epidemic in Zimbabwe adds a new dimension to the hypertension burden. The use of highly active antiretroviral therapy to treat HIV is also associated with increased risk of high blood pressure[26-28].
National programs to diagnose and treat hypertension can lower cerebrovascular disease burden by at least one third[9]. A focus on primary prevention, through awareness and screening programs, training the health work force to deal with hypertension and its associated risk factors, and access to low-cost anti-hypertensive agents is likely to be more cost-effective for a developing country with limited resources[29]. Emphasis should be placed on modifiable behavioral factors, such as lifestyle behaviors of family environment, dietary changes, weight reduction and cessation of smoking, all potentially modifiable, and likely to yield greater impact than concentrating on genetic factors for hypertension[21,30]. Primary prevention of hypertension prevents and reduces the expensive management of hypertension and its ensuing complications[31].
We followed the guidelines for reporting systematic reviews and meta-analysis[10], however certain drawbacks deserve attention.
Heterogeneity: The sample sizes in the studies used for the meta-analysis totalled a few hundred in three studies to a few thousands in one study. The number of included studies was very small, and various risk factors known to influence heterogeneity were not taken into account. The use of a few studies with large differences in sample size in a meta-analysis, results in pooled estimates with low precision and power, and higher χ2 and I2[32]. Due to insufficient data in the included studies, we were unable to perform sub-group analysis to assess the outcome of variations on the pooled prevalence.
Blood pressure measurement: The different methods of measuring blood pressure are documented in literature[22,23,33]. The World Health Organization recommends risk factor surveys measure blood pressure three times per single visit and use the average result[33], which was only done in two studies[8,18], as one measurement per single visit could result in overstated readings[34]. The number of blood pressure readings recorded has been found to determine whether a patient is classified as hypertensive[35].
Representativeness: A significant obstacle in developing effective national hypertension prevention programs is the lack of high quality health information systems to inform policy makers[36]. The burden of NCDs, such as hypertension, is not well documented in Zimbabwe, as its information system has communicable diseases as the main priority. Results from our meta-analysis indicate information on hypertension prevalence in Zimbabwe is limited with no studies providing age-standardized data, thus making direct comparison of results between studies difficult.
In conclusion, our study highlights that estimating the true prevalence of hypertension in Zimbabwe is a challenge due to methodological differences. Therefore, longitudinal national surveys using standardized methodologies are urgently needed in the future to further define the prevalence of hypertension and depict trends.
World Health Organization estimates the prevalence of hypertension in Sub-Saharan Africa to be 46%, making hypertension a major threat to public health. However the response of many governments and international aid agencies to hypertension has been described as similar to the “reaction to human immunodeficiency virus infection and acquired immune deficiency syndrome (HIV/AIDS) 20 years ago”. Zimbabwe (like most sub-Saharan African countries), faces the dual challenge of communicable and non-communicable diseases, however funds donated to fight HIV/AIDS consistently exceed all other national healthcare expenditure. Many countries at a similar stage of development receive more than 50 percent of their total healthcare budgets from donors. Hypertension and its ensuing complications accounted for less than 3% of the global health assistance between 2001 and 2008, despite 80% of deaths from cardiovascular disease occurring in low and middle-income countries. Therefore an estimate of the magnitude of the burden caused by hypertension in Zimbabwe is required to enable the government and international organizations to work together to reduce risk factors for non-communicable diseases such as hypertension.
There are very few studies on hypertension prevalence in Zimbabwe. This is the first meta-analysis, to the knowledge, to systematically review studies conducted in Zimbabwe, and provide a pooled estimate of hypertension prevalence in Zimbabwe, with the aim of promoting increased awareness of hypertension, and initiate a policy response in Zimbabwe.
By providing a pooled estimate for the prevalence of hypertension in Zimbabwe using studies conducted in Zimbabwe, can assist policy makers in preventive policies and strategies suited for the Zimbabwean urban and rural population.
The meta-analysis aimed to consolidate data on hypertension prevalence in Zimbabwean urban and rural areas to determine the burden of hypertension in the country.
Meta-analysis combines results from independent studies and explores the heterogeneity, as some studies are affected by small sample size and the quality of data. Heterogeneity is the differences in methodology or study populations used in the different studies under examination. Sources of inconsistency include study design, various forms of bias, and how the outcome is measured. The random-effects model is applied when studies have different effects and different characteristics. Forest plots enable the reader to view all the studies at once. One axis of the Forest plot displays the effect estimates (prevalence of hypertension expressed as a percentage for each study in the meta-analysis) and corresponding confidence intervals. The overall pooled prevalence estimate (with 95%CI) is represented as a diamond and placed towards the bottom of the plot.
This manuscript is a meta-analysis on the prevalence of hypertension in Zimbabwe. Its’ results have provide evidences on policies and interventions hypertension. The results are interesting.
P- Reviewer: Tan XR, Zhao D S- Editor: Ji FF L- Editor: A E- Editor: Liu SQ
| 1. | Peck RN, Green E, Mtabaji J, Majinge C, Smart LR, Downs JA, Fitzgerald DW. Hypertension-related diseases as a common cause of hospital mortality in Tanzania: a 3-year prospective study. J Hypertens. 2013;31:1806-1811. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 45] [Article Influence: 4.1] [Reference Citation Analysis (5)] |
| 2. | World Health Organization. A Global brief on Hypertension.Silent killer, global public health crisis. Geneva: World Health Organization 2013; . |
| 3. | Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365:217-223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2858] [Cited by in RCA: 3857] [Article Influence: 192.9] [Reference Citation Analysis (1)] |
| 4. | Ministry of Health and Child Welfare, Zimbabwe. National Health Strategy for Zimbabwe 2009-2013: Equity and Quality in Health: A People's Right. 2009;. |
| 5. | World Health Organization. NCD Country Profiles. 2011. [Accessed 2014 March 6]. Available from: http: //www.who.int/nmh/countries/zwe_en.pdf. |
| 6. | Mufunda J, Chatora R, Ndambakuwa Y, Nyarango P, Chifamba J, Kosia A, Sparks HV. Prevalence of noncommunicable diseases in Zimbabwe: results from analysis of data from the National Central Registry and Urban Survey. Ethn Dis. 2006;16:718-722. [PubMed] |
| 7. | Mathe S, Matovu HL, Mossop RT. Nutritional status of an urban community in Zimbabwe. Cent Afr J Med. 1985;31:59-62. [PubMed] |
| 8. | Matenga J, Allain TJ, Wilson AO, Adamchak DJ, Senzanje B, Mushangi E, and Gomo Z. Hypertension management in Zimbabwe- awareness, treatment and blood pressure control. S Afr J Med. 1997;87:1371-1373. |
| 9. | The costs and benefits of prevention. J Public Health Policy. 1980;1:285-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 10. | Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52948] [Cited by in RCA: 47144] [Article Influence: 2946.5] [Reference Citation Analysis (0)] |
| 11. | Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jones DW, Materson BJ, Oparil S, Wright JT. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560-2572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13416] [Cited by in RCA: 13291] [Article Influence: 604.1] [Reference Citation Analysis (0)] |
| 12. | Mabadeje AF. WHO-ISH Guidelines for the management of hypertension: implementation in Africa--the Nigerian experience. Clin Exp Hypertens. 1999;21:671-681. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Whitworth JA. 2003 World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertension. J Hypertens. 2003;21:1983-1992. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1679] [Cited by in RCA: 1732] [Article Influence: 82.5] [Reference Citation Analysis (0)] |
| 14. | Riley RD, Higgins JP, Deeks JJ. Interpretation of random effects meta-analyses. BMJ. 2011;342:d549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2076] [Cited by in RCA: 1930] [Article Influence: 137.9] [Reference Citation Analysis (0)] |
| 15. | Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39087] [Cited by in RCA: 46470] [Article Influence: 2112.3] [Reference Citation Analysis (3)] |
| 16. | Barendregt JJ, Doi SA. Epigear (2012) MetaXL. 2012; Available from: http: //www.epigear.com/index_files/MetaXL User Guide.pdf. |
| 17. | Hakim JG, Mujuru N, Rusakaniko S, Gomo ZAR. WHO STEPS Survey Zimbabwe. Available from: http: //www.who.int/chp/steps/STEPS_Zimbabwe_Data.pdf 2005. |
| 18. | Mufunda J, Scott LJ, Chifamba J, Matenga J, Sparks B, Cooper R, Sparks H. Correlates of blood pressure in an urban Zimbabwean population and comparison to other populations of African origin. J Hum Hypertens. 2000;14:65-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 19. | Marwiro A. Prevalence and Risk Factors for Hypertension among Bulawayo City Council Employees. 2012;. |
| 20. | World Health Organization. Global status report on noncommunicable diseases. Geneva: WHO 2011; . |
| 21. | World Health Organization. STEPwise approach to Surveillance of Chronic Diseases and Risk Factors Instrument. [Accessed 2014 March 5]. Available from: http: //www.who.int/chp/steps/Part1.pdf. |
| 22. | Croft PR. Standardising blood pressure measurement in everyday practice: what’s the gold standard? J Hum Hypertens. 1999;13:85-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 23. | McAlister FA, Straus SE. Evidence based treatment of hypertension. Measurement of blood pressure: an evidence based review. BMJ. 2001;322:908-911. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 95] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 24. | Kearney PM, Whelton M, Reynolds K, Whelton PK, He J. Worldwide prevalence of hypertension: a systematic review. J Hypertens. 2004;22:11-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 660] [Cited by in RCA: 668] [Article Influence: 31.8] [Reference Citation Analysis (0)] |
| 25. | Lloyd-Sherlock P, Beard J, Minicuci N, Ebrahim S, Chatterji S. Hypertension among older adults in low- and middle-income countries: prevalence, awareness and control. Int J Epidemiol. 2014;43:116-128. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 322] [Cited by in RCA: 331] [Article Influence: 30.1] [Reference Citation Analysis (0)] |
| 26. | Blair Research Institute, Zimbabwe. The early socio-demographic impact of the HIV-1 epidemic in rural Zimbabwe. 1996;. |
| 27. | Crane HM, Van Rompaey SE, Kitahata MM. Antiretroviral medications associated with elevated blood pressure among patients receiving highly active antiretroviral therapy. AIDS. 2006;20:1019-1026. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 123] [Article Influence: 6.5] [Reference Citation Analysis (1)] |
| 28. | Dillon DG, Gurdasani D, Riha J, Ekoru K, Asiki G, Mayanja BN, Levitt NS, Crowther NJ, Nyirenda M, Njelekela M. Association of HIV and ART with cardiometabolic traits in sub-Saharan Africa: a systematic review and meta-analysis. Int J Epidemiol. 2013;42:1754-1771. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 122] [Cited by in RCA: 153] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 29. | Miranda JJ, Kinra S, Casas JP, Davey Smith G, Ebrahim S. Non-communicable diseases in low- and middle-income countries: context, determinants and health policy. Trop Med Int Health. 2008;13:1225-1234. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 259] [Cited by in RCA: 248] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 30. | Addo J, Smeeth L, Leon DA. Hypertension in sub-saharan Africa: a systematic review. Hypertension. 2007;50:1012-1018. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 357] [Cited by in RCA: 408] [Article Influence: 22.7] [Reference Citation Analysis (0)] |
| 31. | National High Blood Pressure Education Program Working Group report on primary prevention of hypertension. Arch Intern Med. 1993;153:186-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 150] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 32. | Thorlund K, Imberger G, Johnston BC, Walsh M, Awad T, Thabane L, Gluud C, Devereaux PJ, Wetterslev J. Evolution of heterogeneity (I2) estimates and their 95% confidence intervals in large meta-analyses. PLoS One. 2012;7:e39471. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 132] [Cited by in RCA: 263] [Article Influence: 20.2] [Reference Citation Analysis (0)] |
| 33. | World Health Organization. WHO STEPS Surveillance Manual. Geneva: WHO 2008; . |
| 34. | Bovet P, Gervasoni JP, Ross AG, Mkamba M, Mtasiwa DM, Lengeler C, Burnier M, Paccaud F. Assessing the prevalence of hypertension in populations: are we doing it right? J Hypertens. 2003;21:509-517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 79] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 35. | Birkett NJ. The effect of alternative criteria for hypertension on estimates of prevalence and control. J Hypertens. 1997;15:237-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 28] [Article Influence: 1.0] [Reference Citation Analysis (1)] |
| 36. | Beaglehole R, Ebrahim S, Reddy S, Voûte J, Leeder S. Prevention of chronic diseases: a call to action. Lancet. 2007;370:2152-2157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 184] [Article Influence: 10.2] [Reference Citation Analysis (0)] |