Published online Nov 26, 2014. doi: 10.13105/wjma.v2.i4.221
Revised: October 23, 2014
Accepted: October 28, 2014
Published online: November 26, 2014
Processing time: 134 Days and 14.6 Hours
AIM: To study whether female-specific prostheses are superior to conventional prostheses after total knee arthroplasty (TKA) by conducting this meta-analysis to evaluate the effects of the 2 different designs.
METHODS: A systematic electronic search was conducted in the databases of PubMed, EMBASE and the Cochrane Library for prospective and retrospective trials. Meta-analysis was performed for the outcomes, including range of motion (ROM), Knee Society score, Hospital for Special Surgery scores (HSS) and complications including deep infection, manipulation under anesthesia (MUA), revisions, anterior knee pain, deep vein thrombosis and overhang rate. Meta-analysis was conducted where applicable. Weighted mean difference (WMD) and odds ratio were calculated according to study type.
RESULTS: Seven studies including 1174 knees were eligible for data extraction and pooled analysis. The overhang rate of female-specific prostheses was significantly lower than the conventional ones (WMD, 3.25; 95%CI: 0.00-0.27; P = 0.001). ROM in the female-specific prostheses group after TKA tended to be greater than the conventional prostheses group; however, with insignificant difference (WMD, 2.48; 95%CI: -0.83-5.78; P = 0.14). HSS (WMD, 0.48; 95%CI: -1.45-0.88; P = 0.63) and complications including deep infection (WMD, 0.39; 95%CI: 0.19-3.08; P =0 .70), MUA (WMD, 1.53; 95%CI: 0.02-1.61; P = 0.13) and revisions (WMD, 0.55; 95%CI: 0.07-4.34; P = 0.13) were all comparable between the two groups with at least 1 year follow-up. Other indexes were revealed to be similar between the two treatments with a descriptive analytical method.
CONCLUSION: Although the overhang rate is lower with female-specific prostheses, the current evidence does not support that female-specific prostheses outweigh conventional ones after TKA.
Core tip: In this meta-analysis, we systematically reviewed the literature and evaluated the clinical efficacy of female-specific vs conventional prostheses after total knee arthroplasty (TKA). We found that although the overhang rate is lower with female-specific prostheses and range of motion in the female-specific prostheses group tended to be greater than the conventional prostheses group, the current evidence does not support that female-specific prostheses are superior to conventional ones after TKA with all other parameters, including Knee Society score, Hospital for Special Surgery scores and complications including deep infection, manipulation under anesthesia, revisions, anterior knee pain and deep vein thrombosis comparable between the two treatments.
-
Citation: Rong GX, Huang L, Gui BJ, Xu AM, Zhang JL, Wang SS. Female-specific
vs conventional knee prostheses after total knee arthroplasty: A meta-analysis. World J Meta-Anal 2014; 2(4): 221-227 - URL: https://www.wjgnet.com/2308-3840/full/v2/i4/221.htm
- DOI: https://dx.doi.org/10.13105/wjma.v2.i4.221
Nowadays, total knee arthroplasty (TKA) has become an promising treatment for end-stage degenerative knee arthritis and nearly 60% of sufferers are women[1]. Viewed from the anatomical aspect, there are significant distinctions in arthrosis between men and women. Q angles of women are larger than men and the anterior heights of lateral and medial condyles are smaller in women compared with men. The ratio of anterior-posterior and medial-lateral of the anterior femoral condylar anatomy is larger than in men[2,3]. Conventional prostheses do not consider the gender difference so it may influence the clinical efficacy of TKA. Some research has shown that the clinical efficacy of females is inferior to men and the researchers think that this may because of the anatomical differences based on gender, which can result in patellofemoral joint tightness or overstuffing that eventually limits range of motion (ROM)[4-6]. In order to solve this problem, according to the knee joint anatomical structure of women, the following adjustments were performed based on the conventional prostheses: firstly, female-specific prostheses have 3 Q-angles increased to the distal femoral to solve the defective rate of postoperative patella trajectory; secondly, compared with conventional prostheses, the medial-lateral femoral condylar is shortened. Therefore, the aspect ratio of the medial-lateral to anterior–posterior femoral condylar become smaller and so the consequences of implant overhang is reduced; thirdly, female prostheses reduce the height of the anterior condyle to reduce the friction effectively[7]. Theoretically, female prostheses can obtain a better clinical effect compared with conventional prostheses. However, whether the female prostheses are better clinically is not clear.
Therefore, this meta-analysis was conducted to compare the clinical efficacy of female-specific prostheses versus conventional ones after primary TKA.
We searched EMBASE and MEDLINE databases and the Cochrane Library with the search terms: total knee arthroplasty/total knee replacement and gender-specific/sex-specific/female-specific/NexGen. We limited our search to trials from January 1966 to June 2014. References of the retrieved papers were also screened for any additional relevant studies.
Selection criteria included: (1) clinical trials which compared female-specific prostheses with conventional ones after primary TKA; (2) outcomes including the postsurgical clinical data with a minimum of one year follow-up; (3) presurgical diagnosis of end-stage arthritis; and (4) manuscripts published in English before June 2014.
Exclusion criteria were: (1) patients with a history of previous upper tibial osteotomy, septic arthritis, patellectomy or fixed varus/valgus deformity with an angle larger than 20°; (2) trials with insufficient data, e.g., without ROM, knee society score (KSS), Hospital for Special Surgery scores (HSS) or complications; and (3) comments, letters, guidelines, case reports, reviews, duplications or those that overlapped with other trials but with less information.
The methodological quality of trials was evaluated according to the Cochrane Handbook (version 5.1.2) for systematic reviews of interventions[8]. The assessment criteria have five aspects, including: (1) generation of adequate sequence; (2) concealment of allocation sequence; (3) blinding; (4) incomplete outcome data; and (5) selective outcome report.
Data were collected and extracted by two authors (Rong GX and Gui BJ) independently, including first author, publication date, study type, sample size, patient’s age, gender, body mass index, intervention, follow-up, pre and post-surgical ROMs, Knee score and complications. Any discrepancy was resolved through discussion and consensus. The 95%CI or standard error was converted into standard deviation (SD).
KSS includes Knee Society clinical and function scores. HSS has a high degree of accuracy in evaluating postoperative knee function. Overhang rate was defined as the incidence of the cases where the medial-lateral diameter of prosthesis is larger than the femoral condyle, which will lead to soft tissue irritation and balancing. When patients develop stiffness or less knee flexion, they will undergo manipulation under anesthesia (MUA) to gain knee flexion.
The effect measurements estimated were weighted mean difference (WMD) for continuous outcome and odds ratio for dichotomous outcome, both of which were reported with 95%CIs. Differences were considered to be statistically significant with a P value less than 0.05. Pooled estimate parameters were firstly evaluated with the fixed effect model, while when there was heterogeneity, the random effect model was applied. The heterogeneity among included trials was evaluated with the I2 statistic, representing the proportion of the total variation across trials (I2≤ 75%, extreme heterogeneity; 50% ≤I2≤ 75%, large heterogeneity; 25% < I2 < 50%, moderate heterogeneity; I2≤ 25%, no heterogeneity)[9]. With I2≤ 25%, a fixed effect model was selected and with 25% < I2 < 50%, a random effect model was applied. However, for a trial with I2≥ 50% indicating significant heterogeneity[10], we then tried to figure out the reasons and apply the method of sensitivity or subgroup analysis which was carried out via ruling out the studies possibly biasing the outcomes. The probable publication bias of the outcomes was evaluated using a funnel plot[11]. All statistical analyses were conducted with software RevMan 5.0.
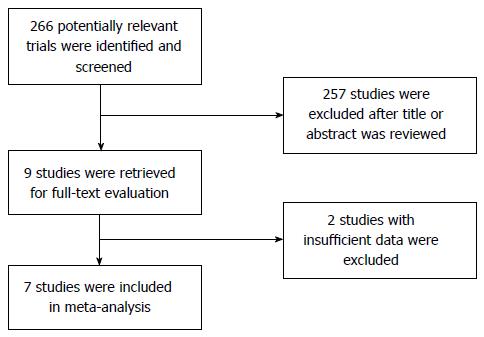
266 potential papers were initially identified according to the search strategy. After the abstracts were read, 257 articles were excluded because they were not related to our research. Seven studies were read as full text and 2 studies[12,13] were excluded subsequently without sufficient data. Ultimately, 7 trials[14-20] with 1174 knees were included: 595 in the female-specific prosthesis arm and 579 in the conventional prosthesis arm. The selection process is shown in Figure 1.
Three trials compared posterior cruciate retaining prostheses and 4 studies compared legacy posterior stabilized prostheses. The follow-up period was 12 to 39 mo. The clinical and demographic features are summarized in Table 1.
| Study ID | Implant used | Sample size (knees) | Study design | Mean age (yr) | Follow-up (mo) | BMI (kg/m2) | ||||
| GSP | CP | GSP | CP | GSP | CP | GSP | CP | |||
| Kim et al[14] | Gender-specific CR- Flex | Standard CR- Flex | 138 | 138 | RCT | 71.2 | 71.2 | 39 | 27.3 | 27.3 |
| Kim et al[15] | Gender-specific LPS-Flex | Standard LPS-Flex | 85 | 85 | RCT | 69.7 | 69.7 | 25.6 | 27.1 | 27.1 |
| Tanavalee et al[16] | Gender-specific LPS-Flex | Standard LPS-Flex | 165 | 149 | CCT | 70 | 70.5 | 24 | 23.4 | 23.5 |
| Singh et al[17] | Gender-specific LPS High-Flex | Standard LPS-Flex | 100 | 100 | RCT | 64 | 68 | 24 | 30.7 | 31.1 |
| Song et al[18] | Gender Solutions | Standard CR- Flex | 46 | 46 | RCT | 68.8 | 68.8 | 31.5 | 26.8 | 26.8 |
| Lionberger et al[19] | Gender-specific CR or LPS-Flex | Standard CR- Flex | 39 | 39 | CCT | 67.9 | 68.3 | 12 | 29.9 | 30 |
| Thomsen et al[20] | Gender Solutions high-Flex | Standard LPS-Flex | 22 | 22 | RCT | 66 | 66 | 13 | 29.3 | 29.3 |
Methodological quality of the eligible studies is shown in Table 2. In the 7 studies, 5 were randomized controlled studies and 2 were retrospective studies.
| Study | Sequence generation | Allocation concealment | Assessor blinding | Incomplete outcome | Selective reporting |
| Kim et al[14] | Yes | Yes | Unclear | Yes | Yes |
| Kim et al[15] | Yes | Yes | Yes | Yes | Yes |
| Tanavalee et al[16] | No | No | No | Yes | Yes |
| Singh et al[17] | Yes | Unclear | Unclear | Yes | Yes |
| Song et al[18] | Yes | Unclear | Yes | Yes | Yes |
| Lionberger et al[19] | No | No | No | Yes | Yes |
| Thomsen et al[20] | Yes | Unclear | Yes | Yes | Yes |
Only 3 studies provided postoperative HSS and 1 does not offer SD (Table 3). Compared with preoperative HSS, both of the implants significantly enhanced postoperative HSS. However, no difference was found (WMD, 0.48; 95%CI: -1.45-0.88; P = 0.63). Four studies provided postoperative KSS but only one study provided SD; therefore, we also just applied a descriptive analysis (Table 4). The 4 trials all reported that the postoperative KSS clinical score was more than 90 points and that the postoperative KSS function score was more than 80 points in the female-specific and conventional groups. The KSS score was significantly improved but there was no difference between the two groups.
| Study | Preoperative ROM | P | Postoperative ROM | P | Preoperative HSS | P | Postoperative HSS | P | ||||
| GSP | CP | GSP | CP | GSP | CP | GSP | CP | |||||
| Kim et al[14] | 127 (100-150) | 123 (80-150) | NR | 124 (85-140) | 126 (85-140) | NR | NR | NR | NR | NR | NR | NR |
| Kim et al[15] | 123 (85-150) | 120 (58-150) | 0.139 | 126 (85-140) | 125 (80-140) | 0.739 | 59.7 (37-58) | 59.1 (37-68) | 0.120 | 91.2 (77-100) | 90.7 (84-100) | 0.252 |
| Tanavalee et al[16] | 126 | 125.6 | > 0.05 | 134.1 | 133.5 | > 0.05 | NR | NR | NR | NR | NR | NR |
| Singh et al[17] | 111.7 ± 13.5 | 110.5 ± 13.7 | 0.282 | 122.8 ± 8.0 | 119.9 ± 8.7 | 0.007 | 55.7 ± 9.1 | 56.7 ± 9.0 | 0.212 | 91.5 ± 4.8 | 91.9 ± 4.1 | 0.313 |
| Song et al[18] | 120.4 ± 16.6 | 121.8 ± 13.5 | 0.64 | 131.1 ± 9.2 | 133.7 ± 19.2 | 0.16 | 57.5 ± 11.5 | 57.1 ± 12.1 | 0.880 | 92.7 ± 8.0 | 92.1 ± 8.7 | 0.75 |
| Lionberger et al[19] | 102.7 ± 9.5 | 107.5 ± 11.5 | 0.048 | 123.4 ± 9.8 | 118.3 ± 9.7 | 0.023 | NR | NR | NR | NR | NR | NR |
| Thomsen et al[20] | NR | NR | NR | 125 (105-142) | 125 (105-139) | 0.82 | NR | NR | NR | NR | NR | NR |
| Study | Preoperative KSS clinical score | P | Postoperative KSS clinical score | P | Preoperative KSS function score | P | Postoperative KSS function score | P | ||||
| GSP | CP | GSP | CP | GSP | CP | GSP | CP | |||||
| Kim et al[14] | 39.8 (10-70) | 35.3 (0-50) | 0.149 | 93 (70-100) | 94 (70-100) | 0.69 | 44.2 (20-70) | 44.2 (20-70) | 1.000 | 84 (60-100) | 83 (60-100) | 0.322 |
| Kim et al[15] | 34.4 (7-62) | 31.2 (0-55) | 0.145 | 96.5 (83-100) | 95.5 (81-100) | 0.424 | 48.3 (20-80) | 47.9 (20-80) | 0.320 | 84.8 (60-100) | 84.8 (60-100) | NR |
| Tanavalee et al[16] | 34.3 | 34.7 | > 0.05 | 92.1 | 92.9 | > 0.05 | 32.2 | 31.8 | > 0.05 | 89.7 | 89.5 | > 0.05 |
| Singh et al[17] | 34.2 ± 11.5 | 36.3 ± 13.4 | 0.118 | 94.9 ± 4.7 | 95.8 ± 3.6 | 0.061 | 37.6 ± 14.0 | 38.7 ± 10.2 | 0.254 | 80.2 ± 10.6 | 79.9 ± 13.0 | 0.429 |
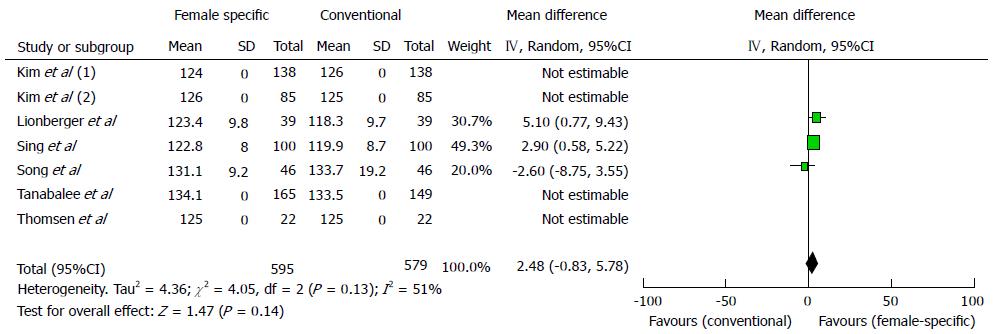
Statistical test with homogeneity based on all trials suggested significant heterogeneity (I2 = 50.6%, P = 0.13), so a random effects model was applied. We found that ROM in the female-specific prostheses group after TKA tended to be greater than the conventional prostheses group; however, with insignificant difference between the 2 groups (WMD, 2.48; 95%CI: -0.83-5.78; P = 0.14; Figure 2).
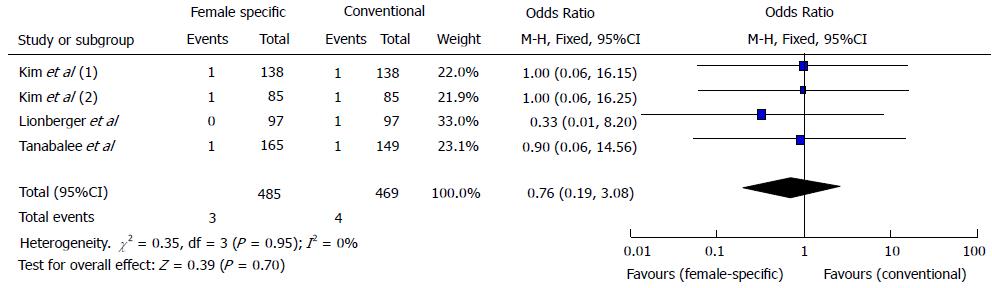
Seven trials recorded surgical complications. Information on deep infection was found in 4 trials[14-16,19] and the pooled WMD was 0.76 (95%CI: 0.19-3.08; P = 0.76), showing that there was no significant difference between the two groups. The P value of heterogeneity test was 0.95 and I2 was 0, indicating no heterogeneity (Figure 3).
Information on overhang was available in 3 trials[14,15,20]. Statistical heterogeneity was not found between the female-specific prosthesis group with conventional ones (P = 0.88), so we use a fixed effects model. The pooled WMD was 3.25 (95%CI: 0.00-0.27; P = 0.001), showing that the overhang rate of the female-specific prosthesis group was significantly lower than the conventional prosthesis group.
There was one patient with a superficial wound infection after gender-specific TKA, as reported by Thomsen et al[20]. MUA for patients was found in 2 trials[16,17]. Revisions performed were also reported in 2 trials[14,16]. Anterior knee pain was reported by Singh et al[17]. There was no supracondylar fracture or deep vein thrombosis reported. These are all shown in Table 5 and significant statistical differences were not found between the 2 groups (MUA: WMD, 1.53; 95%CI: 0.02-1.61; P = 0.13. Revisions: WMD, 0.55; 95%CI: 0.07-4.34; P = 0.13).
DISCUSSION
The meta-analysis showed that there was no significant statistical difference in knee ROM, which is one of the most significant measurements of knee arthroplasty but not the only measure of knee arthroplasty. Meneghini et al[21] reported that there was no difference between the patients who obtained flexion greater than 115° and those who obtained high flexion greater than 125° in Knee Society scores and function scores, which have been widely used in TKA since 1989. HSS was put forward by the American Special Surgery Hospital and has a high degree of accuracy in indicating postoperative knee function. We found no difference between the two groups on KSS and HSS.
Postoperative complications include deep infection which is one of the most serious postoperative complications that could lead to operational failure, MUA, revisions, anterior knee pain and deep vein thrombosis, which in our meta-analysis were not found to have significant statistical differences between the two groups. But, because the follow-up time is not long enough, the long-term complications are not shown. Female-specific prostheses were designed to reduce the ratio of mediolateral overhang in women. Clarke et al[12] found that the incidence of overhang was reduced in female patients when using a female-specific prosthesis. Our meta-analysis suggested that the overhang rate of female-specific prostheses was lower than conventional prostheses. So, the female specific prosthesis provides an easy way to manage the improper mediolateral matching between the femoral component and condyle, a phenomenon that frequently occurs in mid-sized to large-sized female patients[16].
However, some scholars question the design of female-specific prostheses. They report that when conventional prostheses are used, women achieve equal or even better results than men in aspects of prosthesis survival, pain, outcomes scores, risk of revision, ROM, stiffness, wear-related failures and satisfaction[22]. This finding does not support the theory that conventional prostheses place women at a disadvantage compared to men. Besides, Merchant et al[23] summarized 19 studies for full review and concluded that the Q angle and anterior heights of the medial and lateral condyles in women are not significantly different from men and that the smaller female medial-lateral/anterior-posterior aspect ratio has no measurable clinical effect. This finding refutes the theory that female-specific prostheses are needed to address anatomic differences between men and women. In addition, the clinical efficacy after TKA is not only concerned with prostheses but also with many other factors, such as body mass index, age, preoperative ROM, surgical technique, the removal of the posterior cruciate ligament and osteophyte, the management of postoperative pain and compliance of the patient[24].
Meta-analysis itself belongs to an observational study rather than controlled trial study so the result is likely to be affected by bias and confounding factors. Our meta-analysis has some limitations. Firstly, 2 retrospective studies were included and the inherent bias of nonrandomized studies may affect the reliability of conclusion. Secondly, not all the studies provided each clinical result in detail and some studies did not offer SD, which could not be included in the analysis using RevMan. Thirdly, the follow-up periods of the included studies were short so we could not learn about the long-term clinical efficacy. Fourthly, because small number of articles were incorporated in our study, we failed to assess the publication biases by a funnel plot analysis. So, the level of confidence in the estimates is relatively low. However, the inclusion and exclusion criteria in the present meta-analysis are very strict and we evaluated the publication bias qualitatively so the conclusion is believable.
In conclusion, despite the limitations, the meta-analysis indicated that there were no differences between female-specific and conventional prostheses groups in knee ROM, KSS, HSS and complications, including deep infection, MUA, revisions, anterior knee pain and deep vein thrombosis with at least 1 year follow-up but the overhang rate of female-specific prosthesis group was lower than conventional prosthesis group. The absence of evidence does not necessarily mean evidence of absence and more studies of high quality are needed to demonstrate the results and long-term follow-up is needed to prove whether there are any differences in long-term clinical efficacy.
Nowadays, total knee arthroplasty (TKA) has become an effective therapy for end-stage degenerative arthritis of the knee and nearly 60% of sufferers are women. Female-specific prostheses consider the difference of knee joint anatomical structure between men and women. Theoretically, female-specific prostheses can obtain a better clinical effect compared to conventional prostheses. However, whether the female prostheses are superior to the conventional prostheses clinically is not clear.
In recent years, many studies have been performed to compare the clinical efficacy of female-specific vs conventional prostheses after TKA. Moreover, a systematic review was performed. However, these reviews were methodologically insufficient and thus could not achieve a comprehensive conclusion.
Meta-analysis was performed for the outcomes, including range of motion, Knee Society Score (KSS), Hospital for Special Surgery scores (HSS) and complications, including manipulation under anesthesia (MUA), revisions, anterior knee pain, deep vein thrombosis and overhang rate. Meta-analysis was conducted where applicable. These findings were not presented clearly in previous systematic reviews.
Although the overhang rate is lower with female-specific prostheses, the current evidence does not support that female-specific prostheses are superior to conventional ones after TKA. This can be used as a clinical reference when choosing prostheses for TKA.
KSS includes Knee Society clinical and function scores. HSS has a high degree of accuracy in evaluating postoperative knee function. Overhang rate was defined as the incidence of the cases where the medial-lateral diameter of prosthesis is larger than the femoral condyle, which will lead to soft tissue irritation and balancing. When patients develop stiffness or less knee flexion, they will be undergo MUA to gain knee flexion.
This is a well-performed meta-analysis of currently available studies on whether female-specific prostheses are better than conventional prostheses after TKA. The manuscript deals with a relevant topic; the style and structure are good.
P- Reviewer: Laudner K, Tunio MA, Trkulja V S- Editor: Gong XM L- Editor: Roemmele A E- Editor: Wu HL
| 1. | Ritter MA, Wing JT, Berend ME, Davis KE, Meding JB. The clinical effect of gender on outcome of total knee arthroplasty. J Arthroplasty. 2008;23:331-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 126] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 2. | Conley S, Rosenberg A, Crowninshield R. The female knee: anatomic variations. J Am Acad Orthop Surg. 2007;15 Suppl 1:S31-S36. [PubMed] |
| 3. | Cheng FB, Ji XF, Lai Y, Feng JC, Zheng WX, Sun YF, Fu YW, Li YQ. Three dimensional morphometry of the knee to design the total knee arthroplasty for Chinese population. Knee. 2009;16:341-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 116] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 4. | Mihalko W, Fishkin Z, Krackow K. Patellofemoral overstuff and its relationship to flexion after total knee arthroplasty. Clin Orthop Relat Res. 2006;449:283-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 94] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 5. | SooHoo NF, Lieberman JR, Ko CY, Zingmond DS. Factors predicting complication rates following total knee replacement. J Bone Joint Surg Am. 2006;88:480-485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 159] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 6. | Vincent KR, Vincent HK, Lee LW, Alfano AP. Outcomes in total knee arthroplasty patients after inpatient rehabilitation: influence of age and gender. Am J Phys Med Rehabil. 2006;85:482-489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 45] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 7. | Guy SP, Farndon MA, Sidhom S, Al-Lami M, Bennett C, London NJ. Gender differences in distal femoral morphology and the role of gender specific implants in total knee replacement: a prospective clinical study. Knee. 2012;19:28-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 53] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 8. | Xu AM, Huang L, Liu W, Gao S, Han WX, Wei ZJ. Neoadjuvant chemotherapy followed by surgery versus surgery alone for gastric carcinoma: systematic review and meta-analysis of randomized controlled trials. PLoS One. 2014;9:e86941. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 61] [Cited by in RCA: 61] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 9. | Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39087] [Cited by in RCA: 46438] [Article Influence: 2110.8] [Reference Citation Analysis (3)] |
| 10. | Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539-1558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21630] [Cited by in RCA: 25764] [Article Influence: 1120.2] [Reference Citation Analysis (0)] |
| 11. | Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias. Dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA. 1995;273:408-412. [PubMed] |
| 12. | Clarke HD, Hentz JG. Restoration of femoral anatomy in TKA with unisex and gender-specific components. Clin Orthop Relat Res. 2008;466:2711-2716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 63] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 13. | Song EK, Park SJ, Yoon TR, Park KS, Seo HY, Seon JK. Hi-flexion and gender-specific designs fail to provide significant increases in range of motion during cruciate-retaining total knee arthroplasty. J Arthroplasty. 2012;27:1081-1084. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 14. | Kim YH, Choi Y, Kim JS. Comparison of standard and gender-specific posterior-cruciate-retaining high-flexion total knee replacements: a prospective, randomised study. J Bone Joint Surg Br. 2010;92:639-645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 46] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 15. | Kim YH, Choi Y, Kim JS. Comparison of a standard and a gender-specific posterior cruciate-substituting high-flexion knee prosthesis: a prospective, randomized, short-term outcome study. J Bone Joint Surg Am. 2010;92:1911-1920. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 43] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 16. | Tanavalee A, Rojpornpradit T, Khumrak S, Ngarmukos S. The early results of gender-specific total knee arthroplasty in Thai patients. Knee. 2011;18:483-487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 17. | Singh H, Mittal V, Nadkarni B, Agarwal S, Gulati D. Gender-specific high-flexion knee prosthesis in Indian women: a prospective randomised study. J Orthop Surg (Hong Kong). 2012;20:153-156. [PubMed] |
| 18. | Song EK, Jung WB, Yoon TR, Park KS, Seo HY, Seon JK. Comparison of outcomes after bilateral simultaneous total knee arthroplasty using gender-specific and unisex knees. J Arthroplasty. 2012;27:226-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 19. | Lionberger DR, Eggers MD, Brewer KE, Fang L. Improved knee flexion following high-flexion total knee arthroplasty. J Orthop Surg Res. 2012;7:22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 20. | Thomsen MG, Husted H, Bencke J, Curtis D, Holm G, Troelsen A. Do we need a gender-specific total knee replacement? A randomised controlled trial comparing a high-flex and a gender-specific posterior design. J Bone Joint Surg Br. 2012;94:787-792. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 21. | Meneghini RM, Pierson JL, Bagsby D, Ziemba-Davis M, Berend ME, Ritter MA. Is there a functional benefit to obtaining high flexion after total knee arthroplasty? J Arthroplasty. 2007;22:43-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 49] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 22. | Baker PN, Khaw FM, Kirk LM, Esler CN, Gregg PJ. A randomised controlled trial of cemented versus cementless press-fit condylar total knee replacement: 15-year survival analysis. J Bone Joint Surg Br. 2007;89:1608-1614. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 103] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 23. | Merchant AC, Arendt EA, Dye SF, Fredericson M, Grelsamer RP, Leadbetter WB, Post WR, Teitge RA. The female knee: anatomic variations and the female-specific total knee design. Clin Orthop Relat Res. 2008;466:3059-3065. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 79] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 24. | Rajgopal V, Bourne RB, Chesworth BM, MacDonald SJ, McCalden RW, Rorabeck CH. The impact of morbid obesity on patient outcomes after total knee arthroplasty. J Arthroplasty. 2008;23:795-800. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 115] [Article Influence: 6.8] [Reference Citation Analysis (0)] |