Published online Nov 26, 2014. doi: 10.13105/wjma.v2.i4.186
Revised: September 16, 2014
Accepted: October 1, 2014
Published online: November 26, 2014
Processing time: 125 Days and 13.1 Hours
AIM: To investigate and test a causal model derived from previous meta-analytic data of health provider behaviors and patient satisfaction.
METHODS: A literature search was conducted for relevant manuscripts that met the following criteria: Reported an analysis of provider-patient interaction in the context of an oncology interview; the study had to measure at least two of the variables of interest to the model (provider activity, provider patient-centered communication, provider facilitative communication, patient activity, patient involvement, and patient satisfaction or reduced anxiety); and the information had to be reported in a manner that permitted the calculation of a zero-order correlation between at least two of the variables under consideration. Data were transformed into correlation coefficients and compiled to produce the correlation matrix used for data analysis. The test of the causal model is a comparison of the expected correlation matrix generated using an Ordinary Least Squares method of estimation. The expected matrix is compared to the actual matrix of zero order correlation coefficients. A model is considered a possible fit if the level of deviation is less than expected due to random sampling error as measured by a chi-square statistic. The significance of the path coefficients was tested using a z test. Lastly, the Sobel test provides a test of the level of mediation provided by a variable and provides an estimate of the level of mediation for each connection. Such a test is warranted in models with multiple paths.
RESULTS: A test of the original model indicated a lack of fit with the summary data. The largest discrepancy in the model was between the patient satisfaction and the provider patient-centered utterances. The observed correlation was far larger than expected given a mediated relationship. The test of a modified model was undertaken to determine possible fit. The corrected model provides a fit to within tolerance as evaluated by the test statistic, χ2 (8, average n = 342) = 10.22. Each of the path coefficients for the model reveals that each one can be considered significant, P < 0.05. The Sobel test examining the impact of the mediating variables demonstrated that patient involvement is a significant mediator in the model, Sobel statistic = 3.56, P < 0.05. Patient active was also demonstrated to be a significant mediator in the model, Sobel statistic = 4.21, P < 0.05. The statistics indicate that patient behavior mediates the relationship between provider behavior and patient satisfaction with the interaction.
CONCLUSION: The results demonstrate empirical support for the importance of patient-centered care and satisfy the need for empirical casual support of provider-patient behaviors on health outcomes.
Core tip: The meta-analysis provides advice about how to deliver the diagnosis of cancer to a patient that promotes more acceptance. The more constructive reaction a patient has to negative news increases adherence and speed of treatment. The focus on communication that is patient-centered creates the basis for improved clinical practice.
- Citation: Turkiewicz KL, Allen M, Venetis MK, Robinson JD. Observed communication between oncologists and patients: A causal model of communication competence. World J Meta-Anal 2014; 2(4): 186-193
- URL: https://www.wjgnet.com/2308-3840/full/v2/i4/186.htm
- DOI: https://dx.doi.org/10.13105/wjma.v2.i4.186
A substantial amount of research has been dedicated to illuminating the provider-patient communication dynamic during primary care medical interviews[1]. Effective/competent provider-patient communication has been empirically linked to both positive relational and health outcomes[2-4]. Demonstrable outcomes of competent provider-patient communication include: improved understanding and recall of medical information, improved health outcomes, higher levels of satisfaction, decreased anxiety and depression, improved coping, improved adherence/compliance, and improved perceptions of quality of life and well-being[5,6]. When the context is shifted from primary care medical interviews to consultations between oncologists and cancer patients, a variety of dimensions are affected including: standards of care, consultation length, patient’s health status, patient’s anxiety level, and the actual health facility[3]. Therefore, the typical provider-patient communication script of discussing medical problems, general patient education, treatment plans, and relationship building is fundamentally altered and confounded by the issues related to cancer treatment[7]. “Physicians are often challenged to communicate bad news, discuss prognosis, and often switch from curative treatment to supportive care and give appropriate and realistic information all along[7]”.
The increasing global cancer diagnosis rate[8] combined with the inherent issues related to effective/competent provider-patient communication creates both a research challenge and an opportunity. Similar to research efforts focused on the primary care medical interview, data is becoming increasingly available on communication during a cancer consultation. While not as substantial as primary care medical interactions, there has been enough published data to conduct a meta-analysis of observed (i.e., taped and coded) communication between oncologists and patients[4]. In brief, the results provide preliminary evidence to support meta-analytically derived data for patient-centered oncology care. The authors conclude by calling for more advanced analysis to demonstrate actual effects-pathways between provider behaviors, patient behaviors, and patient satisfaction levels[4]. This requires the formulation of a causal model to determine specific associations and sequential relationships among provider-patient behavioral variables, provider-patient communication variables, and patient satisfaction levels. A causal model with detailed statistical support for which specific provider behaviors promote the best patient outcomes would serve to strengthen the evidence base for the efficacy of patient-centered oncology care and provide physicians with direct guidance on maximizing particular communication behaviors that enhance positive patient outcomes.
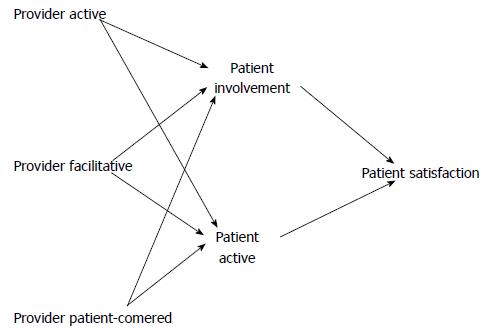
The following review of the literature will examine provider-patient oncology communication and the issues and challenges associated with this specific context. A brief review of communication competence theory[9] and its relationship to provider-patient communication will also be provided. Next, each of the components (input, throughput, and output) of the proposed causal model will be examined: (1) input - provider active, provider facilitative, and provider patient-centered behaviors; (2) throughput - patient involvement and patient active behaviors; and (3) output - patient satisfaction. Finally, a related research question will be advanced regarding provider communication competence within an oncology context.
Provider-patient oncology communication: The general features of provider-patient communication in oncology contexts share many of the same features as primary care provider-patient interactions[10]. Some of the key areas of departure are due to the emotionally charged and uncertain nature of cancer diagnoses[10,11]. The relevant literature on cancer communication highlights the problematic features of the oncology context. The amount of information conveyed during cancer consultations is more substantial and complex than primary care visits[10,11]. Additionally, the emotional component of the situation is salient and covers a range of largely negative reactions including anxiety, fear, frustration, and stigma[10-13]. These general informational and emotional barriers provide the foundation for the more specific issues that contribute to the “unique ecology” of cancer communication contexts[4].
In their summary of the literature, Venetis et al[4]. identify three specific ways that oncology consultations impact the provider-patient communication dynamic: (1) evidence suggests that oncologists are perceived as less competent communicators than their primary care counterparts and demonstrate more resistance to improving their communication skills; (2) the agenda for oncology visits is quite narrow and focused (i.e., the development of a treatment plan), and does not follow the traditional script of history taking, exam, and diagnosis; and (3) the psychosocial (affective, emotional) vs biomedical component of cancer consultations is heightened, corresponding with the emotional issues the patient is facing. Each of these components presents substantial challenges, but they are not insurmountable. Effective and targeted skills training, based on basic principles of communication competence, can improve the interaction for both provider and patient.
Communication competence theory: Communication competence is the ability to choose a communication behavior that is appropriate and effective for a given situation, allowing a person to achieve their communication goals. The model most often used to describe competence is the component model, which includes knowledge, skill, and motivation[9]. Knowledge means knowing what behavior is best suited for a given situation, skill is having the ability to apply that behavior, and motivation is having the desire to communicate in a competent manner. This theory and its components are salient to provider-patient interactions within the oncology context and provide a relevant framework through which to examine communication skills and shortcomings.
The issue of substandard communication competence has been established as a barrier to effective provider-patient communication in the primary care setting[1]. As discussed previously, characteristics of the oncology context exacerbate this issue. According to Cegala et al[1], communication competence in a medical setting can be operationalized as, “Communicative moves that effectively advance a participant’s goals and, at the same time, reflect understanding and appropriate accommodation of the other’s goals” (p.3). Although there may be several goals working in tandem during a medical exchange, the primary goal for both provider and patient is information exchange[1]. Competent information exchange facilitates discussion regarding medical history, the medical problem/issue, diagnosis, treatment plan, and procedures[1].
In a recent study of a communication skills training curriculum based on communication competence theory and specifically designed for oncologists, Bylund et al[14] provided a detailed framework divided into six different skill set modules: (1) establishing the consultation framework skills; (2) checking skills; (3) questioning skills; (4) empathic communication skills; (5) information organization skills; and (6) shared decision-making skills. Based upon these categories, oncologists were assessed for their use of these skill sets both prior to and after attending a communication-training program. The results indicated marked increases in the first two skill sets, establishing the consultation framework and checking. Questioning, empathic communication, and information organization skills demonstrated limited changes. The final skill set, shared decision-making, did not demonstrate any change at all. These findings are informative, promising for ongoing communication skills training efforts, and provide clear indications of where improvements need to be made. Oncologists in this sample clearly demonstrated the ability to absorb and put into practice critical communication competence skills. However, the more affective and socioemotional communicative skills demonstrated the least amount of change.
Communication competence theory[9] is a vital component to informed provider communication skills training. Regardless of the framework or specific training approach, the goal of communication competence is the unifying foundation for all physician skills training programs. As recently demonstrated by Bylund et al[14], the oncology context is no exception. The communication competence theoretical framework provided a tangible set of skill modules for training to be designed around, a clear indication of what skills were successfully adopted by oncologists, and a reasonable understanding of the skills that require additional training.
Proposed causal model components: The explicit and implicit communication challenges associated with the oncology context combined with study results demonstrating both promise and challenges for oncologists in adopting competent communication behaviors, indicate the importance of an enhanced understanding of specific ways oncologists can adopt behaviors with a high likelihood of positively affecting patient outcomes. Recent meta-analysis results confirm the importance of patient-centered oncology care and call for more advanced statistical support of effects pathways among provider behaviors, patient behaviors, and patient outcomes[4]. In an effort to respond to this need, the following investigation advances a proposed causal model with three general components: (1) input; (2) throughput; (3) output. Each of these components includes provider behaviors (i.e., input), patient behaviors (i.e., throughput); and (4) patient outcomes (i.e., output). The following expands on each of the three components and provides detailed explanation of the classification system employed for the casual model.
Provider communication: Three distinct types of provider communication behaviors comprise the input component of the casual model: (1) provider active; (2) provider facilitative; and (3) provider patient-centered behaviors. The proposed casual model positions these three behaviors, when employed effectively, as catalysts for positive patient responses and satisfaction outcomes. Provider active is the most straightforward element and represents measureable behaviors that include frequencies and time allotments (i.e., the amount of information provided and duration of time spent with the patient). Provider facilitative is focused on the emotional tone of the provider. Provider patient-centered is less straightforward, as it also centers on emotional elements. However, the key differences between facilitative and patient-centered are the direction of the emotion (i.e., provider to patient) and the element of inclusion the provider extends to the patient. According to Dimoska et al[15], “A patient-centered approach is one in which the doctor listens to patients attentively and sympathetically, talks about psychosocial and non-medical issues, appears warm and caring towards the patient rather than hurried, and allows the patient to have input into the consultation” (p. 1508). It is this definition, which attends to the affective, psychosocial, and empowerment needs of the patient that will be employed for the proposed model[4].
Based on the 14 eligible studies[2,3,5,7,10,11,13,15-21] used to contribute to the proposed model, the following measured communication behaviors were categorized accordingly. Provider active behaviors include: (1) amount of provider communication; (2) amount of information given by the provider; (3) duration of the provider’s talk; and (4) time spent with the patient. Provider facilitative communication and behaviors are conceptualized to encompass provider: (1) affect/emotionality; (2) friendliness/warmth; (3) depersonalization; (4) emotional responsiveness; (5) empathy; and (6) hostile vs friendly behaviors. The third element, provider patient-centered behaviors, encompasses the largest range of communication and behaviors: (1) partnership building; (2) supportive communication; (3) communicative responsiveness; (4) interest/engagement; (5) use of open-ended questions; (6) framing; (7) health-related quality of life concerns; (8) authoritative vs affiliative behaviors; (9) psychological exchange; and (10) psychosocial partnership issues.
Patient communication: The intermediaries of the proposed causal model are patient-focused and include two elements, patient involvement and patient active communication and behaviors. The relevant literature generally combines these two categories and discusses them more broadly as “patient participation” and more narrowly as “patient question-asking”[16,17,22]. “Patient participation has been operationalized as patients’ relative contribution to the conversation, their discussing of experiences with the illness, the number of questions they ask, their expressions of concerns and worries, and their agenda setting talk[22]”. Street et al[17] provide a more general definition of patient participation, “as the extent to which patients produce verbal responses that have the potential to significantly influence the content and structure of the interaction as well as the health care provider’s beliefs and behaviors” (p. 62).
For the purpose of this model, it is critical to be more specific and to parse out patient participation behaviors into the two categories. Similar to the approach taken with the input component of the model, patient involvement is conceptualized from the 14 eligible studies and includes: (1) length of visit/consultation; (2) preference for information; (3) decision style; (4) question-asking; and (5) treatment decisions. Patient active includes: (1) preference for participation; (2) increases in question asking; and (3) patient information-giving.
Patient satisfaction: As the least complex and most straightforward component of the proposed model, the output represents positive patient outcomes, namely satisfaction with the interaction. As discussed previously, patient outcomes in oncology contexts are substantial and could include physical and emotional dimensions (i.e., improved health, better treatment adherence, improved perceived quality of life, etc.). According to Eide et al[7], patient satisfaction is an outcome measure that usually represents a combination of a patients’ assessment of their relationship with the provider and the medical support they receive. As a driving and central element to almost all provider-patient communication research, patient satisfaction represents an important outcome, particularly in oncology interviews.
Cancer represents a frightening and uncertainty-producing diagnosis. The belief is that more satisfied patients are more likely to complete treatment as well as experience more successful outcomes from treatment. Based on the studies that contributed to the proposed model, patient satisfaction was conceptualized by patient self-reported anxiety levels post-consultation or expressions of satisfaction with the consultation.
It is no longer necessary to argue the importance of effective/competent provider-patient communication, as that has been clearly established in the literature. Similarly, the communication challenges unique to oncology interactions are largely above dispute. The results of a recent meta-analysis establish the importance of patient-centered oncology communication and demonstrate the measurable potential it could have on positive patient outcomes[4]. The remaining piece to this line of research is to provide measurable relationships among these behaviors. These statistics will promote a refined understanding of patient-centered oncology care, identify and isolate the behaviors with the most impact, and inform more directed communication competence skills training programs for oncologists. The driving question is how do all of these components fit together to form an ideal model of physician communication competence?
A search was made of electronic databases and existing reviews of the literature for relevant manuscripts that met the following criteria: (1) reported an analysis of provider-patient interaction in the context of an oncology interview; (2) the study had to measure at least two of the variables of interest to the model (provider activity-measured by total amount of communication/information, provider patient-centered communication-supportive/interest/engagement/framing/asking for open-ended responses, provider facilitative communication-emotional/personalized, patient activity-amount of participation, patient involvement-question asking/length of visit/amount of discussion, and patient satisfaction or reduced anxiety); and (3) the information had to be reported in a manner that permitted the calculation of a zero-order correlation between at least two of the variables under consideration.
Manuscripts that failed to report adequate information for a statistical estimate were not included. A complete list is available from the first author. In some cases the data report only included enough information to provide estimates for only some of the relevant relationships and was included. The lack of complete statistical information reduced the contribution of that data set to this analysis. A simple editorial and publication solution requires the reporting of a complete zero order matrix among all variables and the data could have been included in this report.
Data from 14 studies[2,3,5,7,10,11,13,15-21] were transformed into correlation coefficients and corrected (see Table 1 for details of included studies), where applicable, for various measurement artifacts (for procedures see Hunter et al[23]). Each effect also has the accompanying sample size that was used to estimate the observed relationship. The effects for each separate correlation were averaged and compiled to produce the correlation matrix used for data analysis reported in Table 2. The correlation matrix provides the average estimate for each separate effect and the corresponding sample size estimate for the combined average effect. The averaging process for the estimation is weighted by sample size to reflect the varying contribution and accuracy of the individual effect.
| Butow et al[11] (1995). Sydney, Australia. 142 patients. Interactions coded using the CN-LOGIT Interaction Analysis System. Patients completed the psychological adjustment to cancer scale, the functional living index: cancer, profile of mood states, and satisfaction with the consultation scale |
| Detmar et al[18] (2001). Amsterdam, Netherlands. 71 patients. Interactions coded using the RIAS. Patients completed health-related quality of life survey |
| Dimoska et al[15] (2008). Sydney, Australia. 155 patients. Interactions coded using CANCODE interaction analysis. Patients completed Spielberger State Anxiety Scale, patient satisfaction, and mental adjustment to cancer scale |
| Eggly et al[16] (2006). United States. 28 patients. Interactions coded for content by the Neuendorf system. Communication was evaluated using the Karmanos Accrual Assessment System |
| Eide et al[7] (2003). Norway. 36 patients. Interactions coded using the Roter Interaction Analysis System. Patients completed a satisfaction instrument |
| Ishikawa et al[2] in Patient Education & Counseling (2002). Tokyo, Japan. 128 patients from National Cancer Center Hospital. Interactions coded using the RIAS (Roter Interaction Analysis System). Patients evaluated quality of provider communication |
| Ishikawa et al[5] in Social Science & Medicine (2002). Uses same data as above study |
| Koedoot et al[19] (2004). Amsterdam, Netherlands. 140 patients. Interactions coded on the basis of information provided by the provider. Patients completed surveys involving anxiety, depression, preference for participation in decision-making style, and communicative responsiveness of the provider |
| Leighl et al[20] (2001). Australia. 101 patients. Interactions coded using coded content analysis system developed by the authors. Patients completed adapted form of the Cassileth Information Styles Questionnaire, patient satisfaction, and Spielberger State Anxiety Scale |
| Ong et al[13] (2000). Amsterdam, Netherlands. 96 patients. Interactions coded using the Roter Interaction Analysis System. Patients completed the Rotterdam Symptoms Checklist, and patient satisfaction questionnaire |
| Siminoff et al[10] (2000). Cleveland, OH and San Antonio, TX, United States. 50 patients. Interactions coded using the RIAS. Patients completed knowledge comprehension and satisfaction items (VAS - Visual Analog Scales), decisional conflict scale, and a satisfaction with decision scale |
| Street et al[3] (2006). United States. 62 patients. Interactions coded using system developed by first author |
| Street et al[17] (2001). United States. 9 patients. Interactions coded using system developed by first author |
| Street et al[21] (1995). College Station, TX, United States. 60 patients. Interactions coded using a system developed by the first author. Patients completed the perceived involvement in healthcare scale, the perceived decision control instrument, a knowledge test about cancer treatment, and an optimism scale |
| Provider active | |||||
| Provider facilitative | 0.15 (128) | ||||
| Provider patient-center | 0.10 (328) | 0.18 (71) | |||
| Patient involvement | 0.31 (531) | 0.37 (458) | 0.16 (426) | ||
| Patient active | 0.39 (128) | 0.37 (220) | 0.20 (208) | 0.34 (323) | |
| Patient satisfaction | 0.14 (450) | 0.18 (670) | 0.23 (732) | 0.23 (158) | 0.16 (251) |
The test of the causal model is a comparison of the expected correlation matrix generated using an Ordinary Least Squares (OLS) method of estimation. A good model considered an adequate explanation or fit to the available data will meet a variety of tests: (1) overall fit of the model between actual and expected correlations; (2) each path coefficient is significant; (3) each predicted and actual zero order correlation is within sampling error; and (4) each intervening or mediating variable provides a significant level of mediation. A good or sufficient model will meet each of these four tests described in detail below.
The expected matrix is compared to the actual matrix of zero order correlation coefficients. A model is considered a possible fit if the level of deviation is less than expected due to random sampling error as measured by a χ2 statistic. A nonsignificant chi-square indicates that the level of deviation between the expected and actual matrix is within sampling error, indicating that the model is not inconsistent with the observed data.
The significance of the path coefficients was tested using a Z test. The first test only describes whether the proposed model is consistent with the observed data. This test indicates that the sizes of the relationships are considered significant. The importance of this test is that the first test would still work if the observed path coefficients were all zero. The fit of the overall data, while important, does not indicate the value of the proposed causal connections.
The comparison of the actual and expected correlations in the zero order matrix employs a Z test. The overall test indicates that the combined errors are less than expected due to sampling error but does not indicate whether all connections are within sampling error. An adequate model would demonstrate fit, within sampling error for all observed correlations compared to the expected correlations given the model.
The Sobel test provides a test of the level of mediation provided by a variable and provides an estimate of the level of mediation for each connection. For example, suppose variable A causes variable B causes variable C. The Sobel test considers the connection between A and C and the impact or strength of the mediating effect of variable B on that relationship. The test provides an estimate of that impact and should demonstrate significant reduction. Such a test is warranted in models with multiple paths.
A test of the original model, appearing in Figure 1, indicated a lack of fit with the summary data as reported in Table 2. The first test of the model generated a comparison of the expected and actual matrix that was significant, χ2 (7, average n = 342) = 32.17. The results indicate that the model is not consistent with the data. Examination of the expected and observed zero order matrix was examined to determine if any identifiable changes could be made to the model to arrive at a more consistent model.
The largest discrepancy in the model was between the patient satisfaction and the provider patient-centered utterances. The observed correlation was far larger than expected given a mediated relationship. The decision was made to test the model without the mediated relationship (i.e., removing patient involvement and patient active) to determine if provider patient-centered utterances would have a direct (rather than mediated) impact on patient satisfaction.
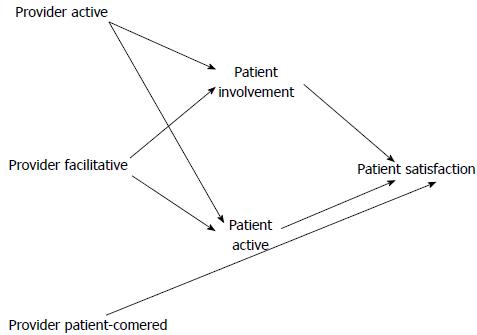
The test of a modified model was undertaken to determine possible fit. The corrected model provides a fit to within tolerance as evaluated by the test statistic, χ2 (8, average n = 342) = 10.22.
Each of the path coefficients for the model displayed in Figure 2 reveals that each one can be considered significant, P < 0.05. The path for provider active to patient involvement (0.39) and provider active to patient active (0.31) are significant. The path coefficients from provider facilitative to patient involvement (0.37) and to patient active (0.37) are significant. All three paths from patient involvement (0.16), patient active (0.23), and provider patient-centered utterances (0.23) to patient satisfaction are significant.
A test of the individual discrepancies between expected and observed correlations demonstrates no value-achieved significance, P < 0.05. What this indicates is that each of the values between the expected and observed correlation matrix are within sampling error.
The Sobel test examines the impact of the mediating variables (patient involvement and patient active) on the relationship between provider active and provider facilitative communication and patient satisfaction. Patient involvement was demonstrated to be a significant mediator in the model, Sobel statistic = 3.56, P < 0.05. Patient active was also demonstrated to be a significant mediator in the model, Sobel statistic = 4.21, P < 0.05. The statistics indicate that patient behavior mediates the relationship between provider behavior and patient satisfaction with the interaction.
The proposed model hypothesized the following casual relationship: a patient’s perception of provider active, facilitative, and patient-centered behavior (i.e., input) generates an intermediate outcome of patient involvement and activity (i.e., throughput), which in turn increases overall patient satisfaction (i.e., output). The modified model that emerged after statistical analysis is: a patient’s perception of provider active and facilitative behavior (i.e., input) generates an intermediate outcome of patient involvement and activity (i.e., throughput), which in turn increases overall patient satisfaction (i.e., output). Similarly, the model also demonstrates a direct (rather than mediated) relationship between a patient’s perception of a provider’s patient-centered behavior and a patient’s overall satisfaction.
The initial proposed model required slight modification after advanced statistical analysis, indicating that provider patient-centered behaviors were not mediated by any type of patient behavior or involvement. Instead, they simply directly impacted patient satisfaction outcomes. This finding is salient to provider communication competence training efforts, as it demonstrates that providers can learn to adopt specific behaviors that will have direct demonstrable outcomes on their success with patients. Similarly, the model also provides substantial insight and support for specific provider behaviors that promote and support patient involvement.
The data remains limited to a relatively small set of studies. While the quality of the data is high - because it is based on actual recorded observations of interaction as opposed to self-reported recollections - the number of providers and patients in the sample is less than 1000. The types of cancers were limited as well and did not include many different cancers with a variety of lifestyle changes. Similarly, the advice is restricted only to oncology and does not consider a number of other important medical contexts where the delivery of information to a patient is important in influencing subsequent participation in treatment or other aspects of the healthcare system.
The most pressing need for future research is to address the questions of generalizability of the findings beyond the limited application to oncology. The theoretical expectations seem to suggest very strongly that the focus of providers on the patient to facilitate understanding and address concerns seems almost tautological in nature. What the findings clearly do indicate is that providers lacking in communication competence will enable a situation of nonparticipation by the patient. Providers should continue to keep in mind that what is offered is medical advice and advice is only valuable from an expert if it is followed.
The results of this investigation demonstrate additional empirical support for the importance of patient-centered care within the oncology context and begin to satisfy the need for empirical casual support of provider-patient behaviors on overall health outcomes. Furthermore, the results provide guidance and proof of tangible competent behavioral patterns that providers can train for and adopt to improve the emotional and physical outcomes for their patients. A statistical causal assessment of provider-patient communication behaviors within the oncology context through the lens of communication competence theory is a logical continuation of previous related research[4]. The findings of this investigation support and enlarge the existing evidence base for the importance of patient-centered care.
The article proposes a model based on actual observations of doctor/patient interactions involving the delivery of the presence of cancer. The challenge is to find a means of delivering this bad news in a constructive manner that creates a focus on patient participation in available treatments as soon as possible.
The challenge for oncologists is to generate a means of patient-centered communication when delivering the results of medical tests. The goal of the provider is to create a full understanding of the medical condition and provide a motivation for the patient to respond in a constructive emotional manner as well as to develop a sense of urgency about participation in treatment options.
The use of meta-analysis to derive and test the model means that the successful model works consistently across the entire body of research and not simply the individual data set. Establishing a model that can explain an entire set of divergent data creates the basis for generalized scientific knowledge.
The study provides advice about how to deliver the diagnosis of cancer to a patient that promotes more acceptance. The more constructive reaction a patient has to negative news increases adherence and speed of treatment. The focus on communication that is patient-centered creates the basis for improved clinical practice.
Meta-analysis refers to a variety of statistical methods used to compare the results from different studies. A causal model is a quantitative representation of real-world dynamics and attempts to describe the causal and other relationships, among a set of multiple variables.
This is an interesting study, indicating that oncologists can directly influence patient satisfaction, by training and adopting specific behavioral patterns.
P- Reviewer: Al-Badawi I, Robotin MC, Sajid MS S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Cegala DJ, Socha McGee D, McNeilis KS. Components of patients’ and doctors’ perceptions of communication competence during a primary care medical interview. Health Commun. 1996;8:1-27. [DOI] [Full Text] |
| 2. | Ishikawa H, Takayama T, Yamazaki Y, Seki Y, Katsumata N. Physician-patient communication and patient satisfaction in Japanese cancer consultations. Soc Sci Med. 2002;55:301-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 71] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 3. | Street RL, Gordon HS. The clinical context and patient participation in post-diagnostic consultations. Patient Educ Couns. 2006;64:217-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 21] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Venetis MK, Robinson JD, Turkiewicz KL, Allen M. An evidence base for patient-centered cancer care: a meta-analysis of studies of observed communication between cancer specialists and their patients. Patient Educ Couns. 2009;77:379-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 139] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 5. | Ishikawa H, Takayama T, Yamazaki Y, Seki Y, Katsumata N, Aoki Y. The interaction between physician and patient communication behaviors in Japanese cancer consultations and the influence of personal and consultation characteristics. Patient Educ Couns. 2002;46:277-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 41] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Siminoff LA, Graham GC, Gordon NH. Cancer communication patterns and the influence of patient characteristics: disparities in information-giving and affective behaviors. Patient Educ Couns. 2006;62:355-360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 244] [Cited by in RCA: 270] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 7. | Eide H, Graugaard P, Holgersen K, Finset A. Physician communication in different phases of a consultation at an oncology outpatient clinic related to patient satisfaction. Patient Educ Couns. 2003;51:259-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 43] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 8. | American Cancer Society. Cancer facts and figures (2014). Available from: http://www.cancer.org. |
| 9. | Spitzberg BH, Cupach WR. Interpersonal communication competence. 1st ed. Beverly Hills, CA: Sage 1984; 26-29. |
| 10. | Siminoff LA, Ravdin P, Colabianchi N, Sturm CM. Doctor-patient communication patterns in breast cancer adjuvant therapy discussions. Health Expect. 2000;3:26-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 93] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 11. | Butow PN, Dunn SM, Tattersall MH, Jones QJ. Computer-based interaction analysis of the cancer consultation. Br J Cancer. 1995;71:1115-1121. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 134] [Cited by in RCA: 138] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 12. | Brown RF, Butow PN, Dunn SM, Tattersall MH. Promoting patient participation and shortening cancer consultations: a randomised trial. Br J Cancer. 2001;85:1273-1279. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 244] [Cited by in RCA: 251] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 13. | Ong LM, Visser MR, Lammes FB, de Haes JC. Doctor-patient communication and cancer patients’ quality of life and satisfaction. Patient Educ Couns. 2000;41:145-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 299] [Cited by in RCA: 303] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 14. | Bylund CL, Brown R, Gueguen JA, Diamond C, Bianculli J, Kissane DW. The implementation and assessment of a comprehensive communication skills training curriculum for oncologists. Psychooncology. 2010;19:583-593. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 83] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 15. | Dimoska A, Butow PN, Dent E, Arnold B, Brown RF, Tattersall MH. An examination of the initial cancer consultation of medical and radiation oncologists using the Cancode interaction analysis system. Br J Cancer. 2008;98:1508-1514. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 16. | Eggly S, Penner LA, Greene M, Harper FW, Ruckdeschel JC, Albrecht TL. Information seeking during “bad news” oncology interactions: Question asking by patients and their companions. Soc Sci Med. 2006;63:2974-2985. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 96] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 17. | Street RL, Millay B. Analyzing patient participation in medical encounters. Health Commun. 2001;13:61-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 184] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 18. | Detmar SB, Muller MJ, Wever LD, Schornagel JH, Aaronson NK. The patient-physician relationship. Patient-physician communication during outpatient palliative treatment visits: an observational study. JAMA. 2001;285:1351-1357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 126] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 19. | Koedoot CG, Oort FJ, de Haan RJ, Bakker PJ, de Graeff A, de Haes JC. The content and amount of information given by medical oncologists when telling patients with advanced cancer what their treatment options are. palliative chemotherapy and watchful-waiting. Eur J Cancer. 2004;40:225-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 95] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 20. | Leighl N, Gattellari M, Butow P, Brown R, Tattersall MH. Discussing adjuvant cancer therapy. J Clin Oncol. 2001;19:1768-1778. [PubMed] |
| 21. | Street RL, Voigt B, Geyer C, Manning T, Swanson GP. Increasing patient involvement in choosing treatment for early breast cancer. Cancer. 1995;76:2275-2285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 22. | Timmermans LM, van der Maazen RW, Verhaak CM, van Roosmalen MS, van Daal WA, Kraaimaat FW. Patient participation in discussing palliative radiotherapy. Patient Educ Couns. 2005;57:53-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 23. | Hunter J, Schmidt F. Methods of meta-analysis: Correcting for artifact and bias in research. 2nd ed. Beverly Hills, CA: Sage 2004; 185-197. [DOI] [Full Text] |