Published online Aug 26, 2014. doi: 10.13105/wjma.v2.i3.91
Revised: May 23, 2014
Accepted: June 18, 2014
Published online: August 26, 2014
Processing time: 197 Days and 18.6 Hours
AIM: To determine the role of statin on mortality outcome in patient with pneumonia.
METHODS: For the present meta-analysis, we search the published literatures online through PubMed, Embase, Scopus and the Cochrane Library databases and the search words used were “statins’”, “bacteraemia”, “pneumonia”, and “ICU infections”. During the online search our focus was on full text articles, peer-reviewed, observational cohort or case control studies and randomized controlled trials. Those studies were selected whose outcome was hospital mortality among patients with pneumonia whether or not on statins. In this meta-analysis, 30 d mortality was used as the primary outcome as it has been demonstrated in the previous research that 30 d mortality is primarily because of community acquired pneumonia. As all studies were observational, where statin users were compared with historical rather than randomized controls, odds ratio for in-hospital or all-cause 30 d mortality was used as the primary effect measure used in the meta-analysis.
RESULTS: We came across the total 25 studies comprising 35355 patients (2734 statin users and 32621 statin non-users) during the electronic search. Four studies out of 25 were included in the final analysis. In this meta-analysis, when data regarding the use of statin in pneumonia patients on mortality was pooled, its results showed the non-significant effect of the statin on mortality outcome.
CONCLUSION: Although statins seems to be useful in the treatment of pneumonia patients but for statistical conclusion, further randomized controlled trials needs to be done or their results still waited to be published of ongoing trials, with the conclusion that presently statins showing no clinical benefit in the pneumonia patients.
Core tip: The relation between statin treatment and improvement in outcomes in patients with pneumonia have been reported in published literatures. This is believed to be due to anti-inflammatory and immunoregulatory effects rather than an effect on cholesterol metabolism. Recently, however, the potential benefit of statins has been called into question and the study has suggested that there may be confounding factor responsible for the observed benefit. All the studies were observational. In this present meta-analysis of randomized controlled trials, results showed the non-significant effect of the statin on mortality outcome.
- Citation: Saha L, Kumar N, Khosla P, Kaur S. Role of statin on mortality outcome in pneumonia patients: A meta-analysis. World J Meta-Anal 2014; 2(3): 91-97
- URL: https://www.wjgnet.com/2308-3840/full/v2/i3/91.htm
- DOI: https://dx.doi.org/10.13105/wjma.v2.i3.91
Statins, an inhibitor of 3-hydroxy-3 methylglutaryl coenzyme A reductase (HMG CoA reductase), was used to reduce total cholesterol, low-density lipoprotein cholesterol, apolipoprotein B and triglyceride levels[1-5]. Statins are effective in reducing the cardiovascular mortality and morbidity in patients with or without coronary artery disease. Apart from its lipid lowering effect, statins also possess multiple pleiotropic effects like anti-inflammatory/immunomodulatory effects. These immunomodulatory effects appear to be mediated through the blockade of mevalonate synthesis[6]. The positive impact observed in the cardiovascular disorders is due to their antioxidant effect, plaque stability, favorable coagulation profile, normalization of sympathetic outflow and immunomodulatory effect[7]. By virtue of their pleiotropic effect they have got a role to play in various other disorders like sepsis, dementia, osteoporosis, bacteremia, venous thromboembolism[6-9].
There is an increased rate of morbidity and mortality in hospitalized Patients with pneumonia[10]. Antimicrobial therapy is the mainstay of treatment for pneumonia. Irrespective of the efforts towards more timely treatment of pneumonia and advances in antimicrobial therapy, mortality rates for patients hospitalized with bacterial pneumonia remains relatively unchanged[11]. Studies published in the literatures have demonstrated a link between statin treatment and improvements in patients with bacterial pneumonia. Several large retrospective observational studies have shown a reduced incidence of pneumonia and improvement in outcomes in pneumonia patients taking statins[12-14]. This is believed to be due to anti-inflammatory and immunoregulatory effects rather than an effect on cholesterol metabolism. Statin drugs are known to reduce cytokine levels in stable patients with coronary artery disease and hypercholesterolemia[15-17]. Excess pro-inflammatory cytokines are found to be associated with severity of pneumonia and the development of complications such as acute respiratory distress syndrome[18-22]. Agents with anti-inflammatory properties such as statins might therefore have the potential to improve pneumonia outcomes. Recently, however, the potential benefit of statins has been called into question and the study has suggested that the confounding factors might be the reason for the observed benefit[23]. A series of studies with contradictory results have been published in the literature that has made clinicians hopeful but confused. With this background, we planned to do a meta-analysis of studies using statins in patients with pneumonia to study the role of statin use in the management of pneumonia.
To get the studies published in the literature, we search the various databases online like PubMed, Embase, Scopus and the Cochrane Library. The search words used were “statins”, “bacteraemia”, “pneumonia’”, and “ICU infections”. The type of studies looked for were peer-reviewed, full text, observational cohort or case controls studies and randomized controlled trials. Those studies whose outcome were hospital mortality in patients with pneumonia, whether or not received statins. Those studies which included patients with pneumonia due to bacterial infection were included in the present meta-analysis. Those studies were excluded from the meta-analysis where the effects of statins on viral (i.e., influenza and human immunodeficiency virus infection), fungal and protozoan infections were studied. Experimental and laboratory studies were also excluded from the meta-analysis. In our search, there were no time or language limits. For additional relevant information, all references from the identified articles were scanned and search. The following data were extracted and tabulated from the selected articles: study design, patient settings, type of infection, the number of patients included, primary and secondary outcomes. For randomized controlled trials (RCTs), we search online registry of RCTs through http://www.controlled-trial.com for relevant studies. The last date of our review process was July 31, 2013.
Those studies which were related to use of statin in pneumonia were first identified. Observational cohort studies whether prospective or retrospective or case control studies which compared 30 d mortality in pneumonia patients among statin users and statin non-users were included in this meta-analysis. We could not identify any randomized control trials.
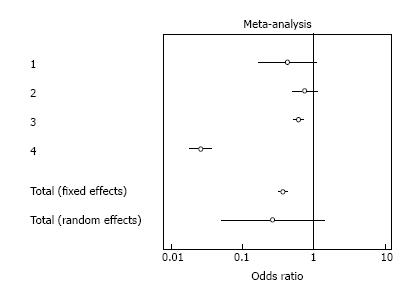
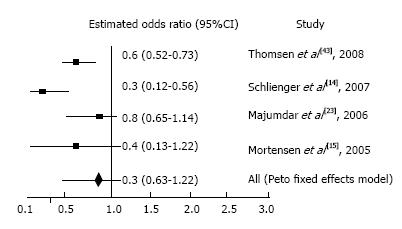
Patients who are taking statin at time of hospital admission were defined as current statin users. The primary outcome in the meta-analysis was 30 d mortality in patients with bacterial pneumonia because studies in the literatures have shown that 30 d mortality is primarily due to community acquired pneumonia rather than other coexisting co morbid conditions. Odds ratio (OR) for in-hospital or all-cause 30 d mortality was measured effect in this meta-analysis as all studies used for meta-analysis were observational, where statin users were compared with historical rather than randomized controls. The heterogeneity between reports was assessed by using χ2 test of heterogeneity. As significant heterogeneity was found between the reports (P < 0.05), we used a random effects model to calculate weighted summary (total) odds ratio and their 95% confidence intervals (CIs) to take the decision. The Mantel-Haenszel method was used to compute the total ORs and CIs. ORs with 95% confidence intervals of all the four studies and the overall odds ratio with 95%CI are depicted in the forest plot (Figure 1) and Peto plot (Figure 2).
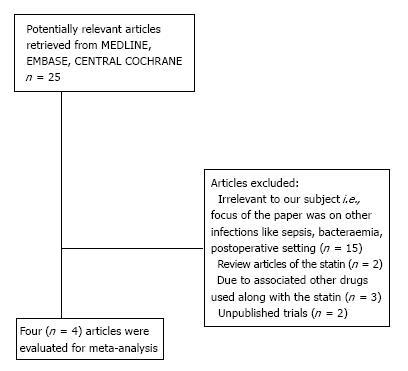
The total number of studies searched for literature was twenty five. Among all these, two were review articles[7,24], another fifteen commented upon the infections like sepsis, bacteremia and other post operative settings[10,25-38], one trial is complete, but the results are still unpublished[39] and in an another trial, recruitment is still going on[40]. There were two studies which have evaluated the impact of statin use along with other drugs[41,42]. Four studies were actually evaluated to document the effect of statin in pneumonia[14,15,23,43] (Figure 3).
Four studies out of the total 25 studies comprising 35355 patients (2734 statin users and 32621 statin non-users) were included in this meta-analysis and in the final analysis. The details of these 4 studies have been mentioned in Table 1. It included both the prospective and retrospective observational studies. All studies were published from 2005 to 2008 (Table 2). In this meta-analysis, when data regarding the use of statin in pneumonia patients on mortality was pooled, its results showed the non-significant effect of the statin on mortality outcome (Figure 1).
| Ref. | Study design | Patient’s setting and study groups | Outcomes and odds ration (95%CI) | Conclusion |
| Thomsen et al[43], 2008 Preadmission Use of Statins and outcomes After Hospitalization With Pneumonia: Population-Based Cohort Study of 29900 Patients | Retrospective population based cohort study | 29900 adults hospitalized with pneumonia for the first time between January 1, 1997, and December 31, 2004 in northern Denmark. Data on statin and other medication use, comorbidities, socioeconomic markers, laboratory findings,bacteremia, pulmonary complications and death were obtained from medical databases. SU: 1371 NSU: 28529 | Of patients with pneumonia, 1371 (4.6%) were current statin users. Mortality among statin users was lower than among nonusers: 10.3% vs 15.7% after 30 d and 16.8% vs 22.4% after 90 d, corresponding to adjusted 30- and 90-d mortality rate ratios of 0.69 (95%CI: 0.58-0.82) and 0.75 (0.65-0.86). | The use of statins is associated with de creased mortality after hospitalization with pneumonia |
| Schlienger et al[14], 2007 Statins and the Risk of Pneumonia: A population-Based, Nested Case-Control Study | Population-based, retrospective, nested case-control analysis | The study population (134262 patients aged > 30 yr) consisted of 55118 patients who took statins and/or fibrates, 29144 patients with hyperlipidemia not taking lipid-lowering agents, and 50000 randomly selected patients without hyperlipidemia and without lipid-lowering treatment. Authors identified 1253 patients with pneumonia and matched them with 4838 control subjects based on age, sex, general practice, and index date.After adjusting for comorbidity and frequency of visits to general practitioners, we calculated the risks (OR with 95% confidence intervals) of uncomplicated pneumonia, hospitalization for pneumonia with survival, and fatal pneumonia in participants who used statins compared with those who did not. SU: 927 NSU: 326 | 30 d Mortality ratio 0.262 (0.182-0.377) | Significant lower mortality among statin users as compared to non users |
| Majumdar et al[23], 2006 Statins and outcomes in patients admitted to hospital with community acquired pneumonia: population based prospective cohort study | Prospective population based cohort study | 3415 adult patients admitted with CAP and categorised according to use of statins for at least one week before admission and during hospital stay. SU: 325 NSU: 3090 | Of 3415 patients with pneumonia admitted to hospital, 624 (18%) died or were admitted to an intensive care unit. Statin users were less likely to die or be admitted to an intensive care unit than non-users [50/325 (15%) vs 574/3090 (19%), OR = 0.80, P = 0.15]. After more complete adjustment for confounding, however, the OR changed from potential benefit (0.78, adjusted for age and sex) to potential harm (1.10, fully adjusted including propensity scores, 95%CI: 0.76-1.60) | Statins are not associated with reduced mortality or need for admission to an intensive care unit in patients with pneumonia; reports of benefit in the setting of sepsis may be a result of confounding. |
| Mortensen et al[15], 2005 The effect of prior statin use on 30-d mortality for patients hospitalized with community-acquired pneumonia | Retrospective cohort study | A retrospective cohort study conducted at two tertiary teaching hospitals. Eligible subjects were admitted with a diagnosis of, had a chest x-ray consistent with, and had a discharge ICD-9 diagnosis of pneumonia. Subjects were excluded if they were “comfort measures only” or transferred from another acute care hospital. Subjects were considered to be on a medication if they were taking it at the time of presentation. Data was abstracted on 787 subjects at the two hospitals. SU: 110 NSU: 677 | In the multivariable regression analysis, after adjusting for the propensity score and processes of care, the use of statins at presentation (OR = 0.36, 95%CI: 0.14-0.92) was significantly associated with decreased 30-d mortality | Prior outpatient statin use was associated with decreased mortality in patients hospitalized with community-acquired pneumonia despite their use being associated with comorbid illnesses likely to contribute to increased mortality |
| Ref. | Mortality in SU | Mortality in NSU | OR | 95%CI |
| Thomsen et al[43] | 141/1372 | 4489/28528 | 0.61 | 0.514-0.732 |
| Schlienger et al[14] | 54/927 | 229/326 | 0.262 | 0.182-0.377 |
| Majumdar et al[23] | 25/325 | 309/3090 | 0.75 | 0.491-1.147 |
| Mortensen et al[15] | 5/110 | 67/677 | 0.434 | 0.171-1.101 |
| Total (fixed effects) | 225/2734 | 5094/32621 | 0.373 | 0.322 - 0.431 |
| Total (Random effects) | 225/2734 | 5094/32621 | 0.267 | 0.0499 - 1.428 |
| Test for heterogeneity Computed value | 246.1742 | |||
| Degrees of freedom | 3 | |||
| Significance level | P < 0.05 |
Studies regarding the statins use have favourably focused on their cardiovascular outcome. Regarding their pleiotropic effects, studies have been conducted which have shown varying/mixed results. Different observational studies regarding statin use in pneumonia have too shown invariably mixed results. The calculated weighted summary (total) OR obtained in this meta-analysis suggests that there was no significant effect of the statin use on mortality outcome in patients with pneumonia.
The important known facts regarding the value of any meta-analysis is that it depends upon the quality of reporting of information in individual trials. If we individually comment on the results of these studies regarding their effect on mortality in the pneumonia patients, it was found that three studies reported lower mortality on pneumonia outcome[13,42,43] and one study reported the nonsignificant effect with its use[23]. The studies which we omitted are the ones in which other cardiovascular drugs have been used like aspirin, beta blockers and angiotensin converting enzyme (ACE) inhibitors, which can bias the results of the meta-analysis[42], in another study by Mortensen 2008[41], again along with stations, ACE inhibitors were added and results of starting a group and station along with ACE inhibitors were compared. The third conducted by Van de Garde[13] was excluded due to the reasons that it evaluated the risk outcome associated with the statin use on pneumonia patients rather than the mortality in them.
Chopra and Flanders[44] in their evidence based study demonstrated results favoring and against the use of statins in mortality outcome, with the ultimate conclusions that further randomized, controlled studies are needed to reach a valid conclusion[44]. Kopterides et al[45] also looked at the outcomes in a different infections, including the sepsis, bacteraemia and pneumonia, but without reaching the firm conclusions of clinical benefit of the statin therapy. A study conducted by Falagas et al[46] has also reported similar results, but no definitive conclusions could be drawn from the pooled data.
The major limitation of this meta-analysis is the inclusion of only observational studies and marked heterogeneity seen in these clinical studies. The heterogeneity was related to the design of the studies along with the sample size, current statin use, associated Co morbidities, and identification of the clinical infection seen in these patients. Another important issue regarding statin use is a healthy user effect, which refers to those patients receiving statins also belongs to higher socioeconomic classes than patients who do not. These patients have the advantage of higher education, better awareness regarding their health which increases the complaint regarding their visits to doctors and treatment schedule, with the results for a better outcome in case of infection.
Based on currently available clinical evidence it can be concluded that statins use shows no clinical benefit in terms of mortality outcome in the pneumonia patients. This conclusion is despite the fact the three studies reported the positive outcome regarding the statin use in the pneumonia patients as compared to the only single one reporting the negative results. As the studies included were heterogeneous, therefore the results of ongoing trials and further randomized controlled trials could only provide a definitive evidence regarding the effect of statins on mortality in pneumonia.
Statins, an 3-hydroxy-3 methylglutaryl coenzyme A reductase (HMG CoA) reductase inhibitor, used to reduce total cholesterol, low-density lipoprotein cholesterol, apolipoprotein B and triglyceride levels. Statins are also effective in reducing the cardiovascular mortality and morbidity in patients with or without coronary artery disease. Apart from its lipid lowering effect, statins also possess multiple pleiotropic effects like anti-inflammatory/immunomodulatory effects. The association between statin use and improvement in outcomes in patients with pneumonia has been reported in published literatures. This is believed to be due to anti-inflammatory and immunoregulatory effects rather than an effect on cholesterol metabolism.
Several large retrospective observational studies have shown a reduced incidence of pneumonia and improvement in outcomes in pneumonia patients taking statins. Recently, however, the potential benefit of statins has been called into question and study has suggested that the confounding factors might be the reason for the observed benefit of those studies. A series of studies with contradictory results have been published in the literature that has made clinicians hopeful but confused. With this background, the authors planned to do a meta-analysis of studies using statins in patients with pneumonia to study the role of statin use in the management of pneumonia.
Four studies out of the total 25 studies comprising 35355 patients (2734 statin users and 32621 statin non-users) were included in this meta-analysis and in the final analysis. It included both the prospective and retrospective observational studies. All studies were published from 2005 to 2008. Odds ratio (OR) for in-hospital or all-cause 30 d mortality was measured effect in this meta-analysis as all studies used for meta-analysis were observational, where statin users were compared with historical rather than randomized controls. The heterogeneity between reports was assessed by using χ2 test of heterogeneity. As significant heterogeneity was found between the reports (P < 0.05), the authors used a random effects model to calculate weighted summary (total) odds ratio and their 95%CIs to take the decision. The Mantel-Haenszel method was used to compute the total OR and CIs. OR with 95%CIs of all the four studies and the overall OR with 95%CI are depicted in the forest plot and Peto plot.
In this meta-analysis, when data regarding the use of statin in pneumonia patients on mortality was pooled, its results showed the non-significant effect of the statin on mortality outcome. As the studies included were heterogeneous, therefore the results of ongoing trials and further randomized controlled trials could only provide a definitive evidence regarding the effect of statins on mortality in pneumonia.
HMG CoA reductase is 3-hydroxy-3 methylglutaryl coenzyme A reductase is the rate-controlling enzyme of the mevalonate pathway, the metabolic pathway that produces cholesterol and other isoprenoids. Pleiotropic effects of statin are those properties of statins other than cholesterol lowering effects like the effect on osteoporosis, dementia and so on.
Authors done a meta-analysis to identify the effectiveness of statin use on mortality due to pneumonia. Authors conducted study well.
P- Reviewer: Surani S, Undela K S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Simvastatin Survival Study Group. Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet. 1994;344:1383-1389. [PubMed] |
| 2. | Sacks FM, Pfeffer MA, Moye LA, Rouleau JL, Rutherford JD, Cole TG, Brown L, Warnica JW, Arnold JM, Wun CC. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. Cholesterol and Recurrent Events Trial investigators. N Engl J Med. 1996;335:1001-1009. [PubMed] |
| 3. | The Long-term Intervention with Pravastatin in Ischaemic Disease (LIPID) Study Group. Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. The Long-Term Intervention with Pravastatin in Ischaemic Disease (LIPID) Study Group. N Engl J Med. 1998;339:1349-1357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3947] [Cited by in RCA: 3721] [Article Influence: 137.8] [Reference Citation Analysis (0)] |
| 4. | West of Scotland Coronary Prevention Group. West of Scotland Coronary Prevention Study: identification of High- risk Groups and Comparison with Other Cardiovascular Intervention Trials. Lancet. 1996;348:1339-1342. [DOI] [Full Text] |
| 5. | Downs JR, Clearfield M, Weis S, Whitney E, Shapiro DR, Beere PA, Langendorfer A, Stein EA, Kruyer W, Gotto AM. Primary prevention of acute coronary events with lovastatin in men and women with average cholesterol levels: results of AFCAPS/TexCAPS. Air Force/Texas Coronary Atherosclerosis Prevention Study. JAMA. 1998;279:1615-1622. [PubMed] |
| 6. | Terblanche M, Almog Y, Rosenson RS, Smith TS, Hackam DG. Statins and sepsis: multiple modifications at multiple levels. Lancet Infect Dis. 2007;7:358-368. [PubMed] |
| 7. | Tandon V, Bano G, Khajuria V, Parihar A, Gupta S. Pleiotropic effects of statins. Indian J Pharmacol. 2005;37:77-85. [RCA] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 26] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Waldman A, Kritharides L. The pleiotropic effects of HMG-CoA reductase inhibitors: their role in osteoporosis and dementia. Drugs. 2003;63:139-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 39] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | Chopra V, Choksi PU, Cavusoglu E. Beyond lipid lowering: the anti-hypertensive role of statins. Cardiovasc Drugs Ther. 2007;21:161-169. [PubMed] |
| 10. | Kruger P, Fitzsimmons K, Cook D, Jones M, Nimmo G. Statin therapy is associated with fewer deaths in patients with bacteraemia. Intensive Care Med. 2006;32:75-79. [PubMed] |
| 11. | Thomsen RW, Riis A, Nørgaard M, Jacobsen J, Christensen S, McDonald CJ, Sørensen HT. Rising incidence and persistently high mortality of hospitalized pneumonia: a 10-year population-based study in Denmark. J Intern Med. 2006;259:410-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 114] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 12. | Fry AM, Shay DK, Holman RC, Curns AT, Anderson LJ. Trends in hospitalizations for pneumonia among persons aged 65 years or older in the United States, 1988-2002. JAMA. 2005;294:2712-2719. [PubMed] [DOI] [Full Text] |
| 13. | van de Garde EM, Hak E, Souverein PC, Hoes AW, van den Bosch JM, Leufkens HG. Statin treatment and reduced risk of pneumonia in patients with diabetes. Thorax. 2006;61:957-961. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 97] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 14. | Schlienger RG, Fedson DS, Jick SS, Jick H, Meier CR. Statins and the risk of pneumonia: a population-based, nested case-control study. Pharmacotherapy. 2007;27:325-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 109] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 15. | Mortensen EM, Restrepo MI, Anzueto A, Pugh J. The effect of prior statin use on 30-day mortality for patients hospitalized with community-acquired pneumonia. Respir Res. 2005;6:82. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 125] [Cited by in RCA: 132] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 16. | Jialal I, Stein D, Balis D, Grundy SM, Adams-Huet B, Devaraj S. Effect of hydroxymethyl glutaryl coenzyme a reductase inhibitor therapy on high sensitive C-reactive protein levels. Circulation. 2001;103:1933-1935. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 481] [Cited by in RCA: 469] [Article Influence: 19.5] [Reference Citation Analysis (0)] |
| 17. | Musial J, Undas A, Gajewski P, Jankowski M, Sydor W, Szczeklik A. Anti-inflammatory effects of simvastatin in subjects with hypercholesterolemia. Int J Cardiol. 2001;77:247-253. [PubMed] |
| 18. | Strandberg TE, Vanhanen H, Tikkanen MJ. Effect of statins on C-reactive protein in patients with coronary artery disease. Lancet. 1999;353:118-119. [PubMed] |
| 19. | Almirall J, Bolíbar I, Toran P, Pera G, Boquet X, Balanzó X, Sauca G. Contribution of C-reactive protein to the diagnosis and assessment of severity of community-acquired pneumonia. Chest. 2004;125:1335-1342. [PubMed] |
| 20. | Fernandez-Serrano S, Dorca J, Coromines M, Carratala J, Gudiol F, Manresa F. Molecular inflammatory responses measured in blood of patients with severe community acquired pneumonia. Clin Diagn Lab Immunol. 2003;10:813-820. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 21. | Glynn P, Coakley R, Kilgallen I, Murphy N, O’Neill S. Circulating interleukin 6 and interleukin 10 in community acquired pneumonia. Thorax. 1999;54:51-55. [PubMed] |
| 22. | Puren AJ, Feldman C, Savage N, Becker PJ, Smith C. Patterns of cytokine expression in community-acquired pneumonia. Chest. 1995;107:1342-1349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 105] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 23. | Majumdar SR, McAlister FA, Eurich DT, Padwal RS, Marrie TJ. Statins and outcomes in patients admitted to hospital with community acquired pneumonia: population based prospective cohort study. BMJ. 2006;333:999. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 195] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 24. | Daniel Pella, Rafael Rybar and Viola Mechirova. Pleoitropic effect of statins. Acta Cardiol Sin. 2005;21:190-198. |
| 25. | Mortensen EM, Restrepo MI, Copeland LA, Pugh JA, Anzueto A, Cornell JE, Pugh MJ. Impact of previous statin and angiotensin II receptor blocker use on mortality in patients hospitalized with sepsis. Pharmacotherapy. 2007;27:1619-1626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 58] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 26. | Yang KC, Chien JY, Tseng WK, Hsueh PR, Yu CJ, Wu CC. Statins do not improve short-term survival in an oriental population with sepsis. Am J Emerg Med. 2007;25:494-501. [PubMed] |
| 27. | Tseng MY, Hutchinson PJ, Czosnyka M, Richards Hugh, Pickard JD, Kirkpatrick PJ. Effects of acute pravastatin treatment on intensity of rescue therapy, length of inpatient stay, and 6-month outcome in patients after aneurysmal subarachnoid hemorrhage. Stroke. 2007;38:1545–1550. [RCA] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 94] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 28. | Martin CP, Talbert RL, Burgess DS, Peters JI. Effectiveness of statins in reducing the rate of severe sepsis: a retrospective evaluation. Pharmacotherapy. 2007;27:20-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 46] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 29. | Gupta R, Plantinga LC, Fink NE, Melamed ML, Coresh J, Fox CS, Levin NW, Powe NR. Statin use and sepsis events [corrected] in patients with chronic kidney disease. JAMA. 2007;297:1455-1464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 84] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 30. | Almog Y, Novack V, Eisinger M, Porath A, Novack L, Gilutz H. The effect of statin therapy on infection-related mortality in patients with atherosclerotic diseases. Crit Care Med. 2007;35:372-378. [PubMed] |
| 31. | Fernandez R, De Pedro VJ, Artigas A. Statin therapy prior to ICU admission: protection against infection or a severity marker? Intensive Care Med. 2006;32:160-164. [PubMed] |
| 32. | Hackam DG, Mamdani M, Li P, Redelmeier DA. Statins and sepsis in patients with cardiovascular disease: a population-based cohort analysis. Lancet. 2006;367:413-418. [PubMed] |
| 33. | Almog Y, Shefer A, Novack V, Maimon N, Barski L, Eizinger M, Friger M, Zeller L, Danon A. Prior statin therapy is associated with a decreased rate of severe sepsis. Circulation. 2004;110:880-885. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 282] [Cited by in RCA: 278] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 34. | Thomsen RW, Hundborg HH, Johnsen SP, Pedersen L, Sørensen HT, Schønheyder HC, Lervang HH. Statin use and mortality within 180 days after bacteremia: a population-based cohort study. Crit Care Med. 2006;34:1080-1086. [PubMed] |
| 35. | Liappis AP, Kan VL, Rochester CG, Simon GL. The effect of statins on mortality in patients with bacteremia. Clin Infect Dis. 2001;33:1352-1357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 251] [Cited by in RCA: 249] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 36. | Subramaniam K, Koch CG, Bashour A, O’Connor M, Xu M, Gillinov AM, Starr NJ. Preoperative statin intake and morbid events after isolated coronary artery bypass grafting. J Clin Anesth. 2008;20:4-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 40] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 37. | Coleman CI, Lucek DM, Hammond J, White CM. Preoperative statins and infectious complications following cardiac surgery. Curr Med Res Opin. 2007;23:1783-1790. [PubMed] |
| 38. | Hauer-Jensen M, Fort C, Mehta JL, Fink LM. Influence of statins on postoperative wound complications after inguinal or ventral herniorrhaphy. Hernia. 2006;10:48-52. [PubMed] |
| 39. | Pravastatin and ventilatory associated pneumonia. Available from: http://clinicaltrials.gov. |
| 40. | Statin-Vap statin-Vap - Statins and Ventilator-Associated Pneumonia. Available from: http: //clinicaltrials.gov. |
| 41. | Mortensen EM, Pugh MJ, Copeland LA, Restrepo MI, Cornell JE, Anzueto A, Pugh JA. Impact of statins and angiotensin-converting enzyme inhibitors on mortality of subjects hospitalised with pneumonia. Eur Respir J. 2008;31:611-617. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 100] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 42. | Chalmers JD, Singanayagam A, Murray MP, Hill AT. Prior statin use is associated with improved outcomes in community-acquired pneumonia. Am J Med. 2008;121:1002-1007.e1. [PubMed] |
| 43. | Thomsen RW, Riis A, Kornum JB, Christensen S, Johnsen SP, Sørensen HT. Preadmission use of statins and outcomes after hospitalization with pneumonia: population-based cohort study of 29,900 patients. Arch Intern Med. 2008;168:2081-2087. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 132] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 44. | Chopra V, Flanders SA. Does statin use improve pneumonia outcomes? Chest. 2009;136:1381-1388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 45. | Kopterides P, Falagas ME. Statins for sepsis: a critical and updated review. Clin Microbiol Infect. 2009;15:325-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 87] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 46. | Falagas ME, Makris GC, Matthaiou DK, Rafailidis PI. Statins for infection and sepsis: a systematic review of the clinical evidence. J Antimicrob Chemother. 2008;61:774-785. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 127] [Article Influence: 7.5] [Reference Citation Analysis (0)] |