Published online May 26, 2014. doi: 10.13105/wjma.v2.i2.24
Revised: January 25, 2014
Accepted: February 18, 2014
Published online: May 26, 2014
Processing time: 227 Days and 14.8 Hours
Several definitions of post percutaneous coronary intervention (PCI) thrombocytopenia (TC) were formulated. Recent studies demonstrated that a relative drop in platelet count ≥ 25% is the most appropriate criterion. By this definition a population is detected that is exposed not only to increased risk of hemorrhagic complications but also to increased risk of ischemic events, which may appear a paradox. In patients with acute coronary syndromes undergoing PCI, several conditions might be associated with TC: cardiopulmonary by-pass and the presence of extra corporeal membrane oxygenators, intra aortic balloon pump (IABP), cardiogenic shock, thrombolytic drugs and anticoagulant or antiplatelet drugs. Several studies demonstrated that TC and ischemic outcomes are related although it is unclear whether this is a direct relationship or TC is just a secondary effect of another cryptic protagonist. It is suggested that further investigations determine whether there is a real link between TC, a probably well defined covariate, and ischemic outcomes or whether IABP is the joining link between these two variables and whose presence needs in any case be considered in multivariable statistics. Post-PCI TC could be only a secondary effect of IABP use. On turn, the prolonged use of heparin necessarily accompanying the use of IABP, and producing a paradoxical pro-thrombotic TC, might also be implicated.
Core tip: This minireview suggested that further investigations are needed to determine whether there is a real link between thrombocytopenia (TC), a probably well defined covariate, and ischemic outcomes or whether intra-aortic balloon (IABP) is the joining link between these two variables and whose presence needs in any case be considered in multivariable statistics. Post-percutaneous coronary intervention TC could be only a secondary effect of IABP use. On turn, the prolonged use of heparin necessarily accompanying the use of IABP, and producing a paradoxical pro-thrombotic TC, might also be implicated.
- Citation: Schiariti M, Iannetta L, Torromeo C, Gregorio MD, Puddu PE. Prognostic significance of post percutaneous coronary intervention thrombocytopenia. World J Meta-Anal 2014; 2(2): 24-28
- URL: https://www.wjgnet.com/2308-3840/full/v2/i2/24.htm
- DOI: https://dx.doi.org/10.13105/wjma.v2.i2.24
Thrombocytopenia (TC) is a clinical condition related to decreased production, sequestration or increased destruction of platelets. Isolated TC is more likely due to peripheral destruction[1]. In the setting of acute coronary syndromes (ACS) the use of heparin[2,3], platelet glycoprotein IIb/IIIa receptor inhibitors[4] and intra-aortic balloon pump (IABP)[5] is associated to improved outcomes but, on the other hand, it exposes patients to higher risk of bleeding and decline in platelet count. When the magnitude of the platelet drop is large enough, one of the main definitions of “acquired” TC may be met. A summary of the main definitions is available in Table 1. Classically, acquired TC was defined as a decrease of platelet levels from normal baseline count (> 150 × 109/L) to thrombocytopenic levels (< 150 × 109/L)[6,7] or as a nadir platelet count < 100 × 109/L[8-10] during the in-hospital phase or as a ≥ 50% drop in platelet count from pre-intervention platelet values[6,8].
| Ref. | Number of thrombocytopenic patients n (%) | Definition of thrombocytopenia | Mortality rate1 | Hemorrhagic outcomes1 | Composite Ischemic outcomes1 |
| Berkowitz et al[10] | 81/2099 (3.9) | Nadir PLT count < 100 × 109/L | 12.1% vs 1.1% at 1 mo | 48.7% vs 9.5% at 1 mo | NSC |
| McClure et al[8] | 633/10948 (7.0) | Nadir PLT count < 100 × 109/L or delta PLT > 50% | 7.4% vs 3.3% at 1 mo | 75.8% vs 27.8% at 1 mo | 30% vs 14.1% at 1 mo |
| Eikelboom et al[3] | 87/10141 (1) | Nadir PLT count < 100 × 109/L | 11.50% at 6 mo | 8% vs 1.4% at 6 mo | 33.3% vs 30.8%2 at 6 mo3 |
| Merlini et al[4] | 99/4809 (2.9) | Nadir PLT count < 100 × 109/L or delta PLT ≥ 25% | 2.0% vs 0.4% at 1 mo | 5.1% vs 0.7% | 12.2% vs 6.6% at 1 mo |
| Nikolsky et al[9] | 50/2082 (2.5) | Nadir PLT count < 100 × 109/L | 10% vs 3.9% at 12 mo | 10% vs 2.7% | 26.1% vs 17.4% at 12 mo |
| Shenoy et al[32] | 41/1302 (3.1) | Nadir PLT count < 100 × 109/L or delta PLT > 50% | 10% vs 2% at 6 mo | 37% vs 3% | 39% vs 15% at 6 mo |
| Wang et al[6] | 4697/36182 (13) | Nadir PLT count < 150 × 109/L and/or delta PLT > 50% | 6.9% vs 2.6% in hospital stay | 26.7% vs 10% | NC |
| De Labriolle et al[11] | 1644/10146 (16.95) | Delta PLT ≥ 25% | 11% vs 4.2% at 12 mo | 21% vs 2.6% | 22.9% vs 16.01% at 12 mo |
| Caixeta et al[7] | 740/10836 (6.8) | Nadir PLT count < 150 × 109/L | 6.5% vs 3.4% at 12 mo | 14.0% vs 4.3% | 22.8% vs 15.1% at 12 mo |
| Kiviniemi et al[35] | 46/929 (9.7) | Nadir PLT count < 100 × 109/L or delta PLT > 50% | 12% vs 11%2 at 12 mo | 23% vs 22%2 at 12 mo | 24% vs 19%2 at 12 mo |
More recently, De Labriolle et al[11] proposed a novel threshold of ≥ 25% decrease in platelet count to define acquired TC. The latter definition is important to detect a population that is exposed not only to increased risk of hemorrhagic complications but also, as might be easily foreseen, to higher risk of ischemic events[11]. However, although the first correlation is intuitive, the second one seems a real paradox. The purpose of this review is to examine the subset of thrombocytopenic patients in the setting of ACS and to define the clinical relevance of TC for prognosis.
Several causes of TC are known but, in many instances, they cannot be identified[12]. In patients with ACS undergoing percutaneous coronary intervention (PCI), several conditions might be associated with TC.
These conditions may cause TC and platelet dysfunction related to the artificial membrane oxygenators used in these settings[1,13].
Platelet count decrease is correlated primarily to the device itself, independently from the use of intravenous heparin in one study[5]. It is a predictable platelet count decrease characterized by distinct features: it rapidly recovers if the device is removed or it stabilizes after 4 d if IABP remains in place[5,14].
Several studies demonstrated that TC is common in shocked patients[5,15]. This could be related to decreased bone marrow productive activity in severely ill patients, but these patients will also more likely receive an IABP[5,15,16]. Therefore some investigators in post-PCI TC de facto excluded shocked patients from the study population[4,9,11] and probably made a major selection bias.
In the setting of ACS, thrombolytic therapy is widely used since it improves mortality rate, although it is associated with TC and therefore to increased risk of hemorrhage and death[17]. Since this is a well-known cause of platelet count reduction, some studies in post-PCI TC excluded all patients undergone thrombolysis[8,9,11].
Since Silver, Rhodes and Dixon first identified central features of Heparin Induced TC (HIT) where TC and thrombosis have an immune pathogenesis, HIT has been deeply investigated[18]. HIT is due to a peculiar heparin-dependent and platelet-activating antibody (IgG)[18,19] and seems related to heparin preparations[2] with typical features: it is usually moderate and more frequently begins later than 5-14 d (typical onset) after the drug administration, although it can occur after 7-40 d (delayed onset) or, in patients who received it in the previous 100 d, within 24 h (rapid onset)[18,20].
Glycoprotein IIb/IIIa receptor inhibitors
Patients undergone triple antiplatelet therapy based on glycoprotein IIb/IIIa receptor inhibitors (GPI) have a better prognosis in the setting of ACS. However, based on a recent meta-analysis[21], GPI therapy seems to have no beneficial effect in elective PCI. The latter study does not clarify whether patients undergoing elective PCI were or not pretreated with a dual antiplatelet therapy before receiving a downstream GPI treatment[21]. GPI-related TC mostly occurs rapidly, within few hours from drug administration and, differing from HIT, it can be profound (platelet count < 20 × 109/L). It is related to the presence of drug-dependent antiplatelet antibodies[1,22,23]. This type of TC, independently from the specific GPI molecule administered, seems to follow a distinct clinical course when compared to other etiologies: it is more profound but has a quicker recovery[12,24,25]. Nevertheless, it seems also associated to increased rate of ischemic events[4].
Thrombocytopenic patients have some peculiar features: they are more likely men[6-11], with a lower body mass index[6,8-11], diabetics[6,9] and with arterial hypertension[6]. Medical history of thrombocytopenic patients is typically characterized by previous myocardial infarction[6], previous PCI[6-8], previous stroke[6] and heart failure[6,11]. Looking at their home therapy they more likely are on statins and oral hypoglycemic therapy[9,11] and less likely treated with aspirin[9]. Looking at laboratory parameters, these patients have a lower baseline platelet count[6,7,9,11] and baseline renal insufficiency[7,11]. All these parameters should be therefore taken into account when defining the independent role of TC.
Since its identification, post-PCI TC was classically related to hemorrhagic events[1,10,17,24]. Nevertheless, platelet count decline was also related to ischemic outcomes[3,4,7-9,11,32]. Several hypotheses were formulated to explain this relationship. Early discontinuation of antiplatelet agents for the onset of acute TC was considered causative of unfavorable clinical outcome[6,7], but other studies confuted this hypothesis[10]. It was also hypothesized that platelet consumption was associated with platelet activation, leading to downstream thrombotic events[6]. It was demonstrated that mean platelet volume was significantly increased despite concomitant decrease in platelet count in patients with ACS or stroke and animal models supported this, pointing to the fact that large platelets seem to have a higher thrombotic potential[33]. Moreover, TC was suspected to have a direct pathogenetic influence on adverse ischemic events[11] or it may be considered a simple marker of poor prognosis[6,32].
A clear-cut evolution in the definition of acquired TC and its relationship with ischemic outcomes may be seen between 1998 and 2013 (Table 1). Contrary to early studies defining TC only on the basis of absolute platelet count drop[7,9,10], more recent investigations clearly showed that post-PCI TC should be defined only based on relative drop in platelet count[11,34]. The different definitions of acquired TC are variously related to mortality and to ischemic or hemorrhagic outcomes (Table 1).
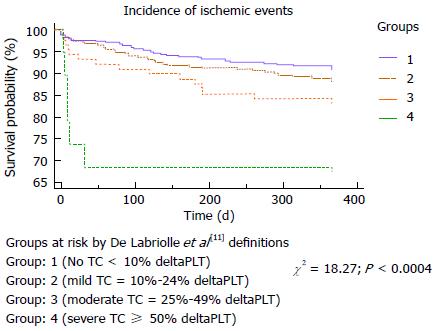
It is thus possible to identify individuals with substantial falls in platelet count, not reaching thrombocytopenic levels, that are at increased risk of ischemic events. We showed evidence[34] illustrated by Kaplan-Meyer curves (Figure 1) for a strong reverse relationship between platelet count[11] and the incidence of cumulative ischemic outcome. In 2013 Kiviniemi et al[35], assessing hemorrhagic and ischemic complications in patients on oral anticoagulation undergoing PCI, found a similar risk of adverse outcome in patients with acquired TC compared with the control group. On the other hand, we indicated[34] that in the setting of TC there might be a cryptic protagonist: IABP. Indeed, in ACS, previous studies did not consider the important association with IABP itself, apart that from the concomitant presence of shock, among the determinants of TC[3,6,7] or interpreted it as a simple predictor of acquired TC[8,11].
Since there is a well known relationship between ischemic events and IABP use[36], the question is whether post-PCI TC is causative of ischemic events or whether the other protagonist (IABP) may have a con-causal (mechanic) role. Under these perspectives, cardiogenic shock should be considered a further etiologic factor for TC[5,14,16,34]. On the other hand, as IABP is necessarily associated with concomitant heparin utilization, it is for further study to assess and quantify the impact of prolonged heparin on TC and long-term ischemic outcome.
An important question is whether TC, defined following the more recent investigations (Table 1) pointing to a ≥ 25% drop in platelet count from baseline to post-PCI, might be considered a covariate to be fed into multivariable statistics for prediction of ischemic or hemorrhagic outcomes. We tried to reply to this question by re-analyzing our data on 873 ACS patients treated by PCI[34] and of whom 867 had complete data (Figure 1): 107 (12%) of these were with TC according to the abovementioned definition[11]. We then run a logistic regression in forced mode and the area under the ROC curve was 75% (log likelihood -267, model r2 = 0.17) by fitting 13 covariates (age, gender, presence of shock, the occurrence of primary or rescue PCI, the number of vessels with significant coronary stenoses, the values of baseline platelet count, hemoglobin, red blood cells, creatine kinase, glomerular filtration rate by Modification of Diet in Renal Disease formula, absence of GPI inhibitors and presence of IABP). There were only 4 contributors to predict TC: age (P = 0.06008), the occurrence of primary (P = 0.00207) or rescue (P =0.00098) PCI and the presence of IABP (P = 0.00001) with a significant intercept (P = 0.02168). From these data it might be concluded that TC is indeed a potential covariate, although in order to fully disclose its predictive role in post-PCI investigations aimed at assessing long-term impact on ischemic outcome, it is essential to fit other confounders and among these latter: age, IABP and the type of PCI performed.
Post-PCI TC was classically related to increased mortality and incidence of bleeding and large evidence exists. On the other hand, TC was also related to higher risk of ischemic events. Although several hypotheses were formulated to define the latter relationship, no evidence proved that ischemic outcomes are related to TC per se or they might be just an ancillary phenomenon. It is suggested that further investigations determine whether there is a real link between TC, a probably well defined covariate, and ischemic outcomes or whether IABP is the joining link between these two variables. In any case presence of IABP should be considered in multivariable statistics. Post-PCI TC could be only a secondary effect of IABP use, possibly also related to the concomitant use of heparin, although precise quantification of this is lacking.
P- Reviewer: Lin GM S- Editor: Zhai HH L- Editor: A E- Editor: Wu HL
| 1. | Konkle BA. Acquired disorders of platelet function. Hematology Am Soc Hematol Educ Program. 2011;2011:391-396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 47] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 2. | Bell WR, Royall RM. Heparin-associated thrombocytopenia: a comparison of three heparin preparations. N Engl J Med. 1980;303:902-907. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 171] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 3. | Eikelboom JW, Anand SS, Mehta SR, Weitz JI, Yi C, Yusuf S. Prognostic significance of thrombocytopenia during hirudin and heparin therapy in acute coronary syndrome without ST elevation: Organization to Assess Strategies for Ischemic Syndromes (OASIS-2)study. Circulation. 2001;103:643-650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 37] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 4. | Merlini PA, Rossi M, Menozzi A, Buratti S, Brennan DM, Moliterno DJ, Topol EJ, Ardissino D. Thrombocytopenia caused by abciximab or tirofiban and its association with clinical outcome in patients undergoing coronary stenting. Circulation. 2004;109:2203-2206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 92] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 5. | Vonderheide RH, Thadhani R, Kuter DJ. Association of thrombocytopenia with the use of intra-aortic balloon pumps. Am J Med. 1998;105:27-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 67] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 6. | Wang TY, Ou FS, Roe MT, Harrington RA, Ohman EM, Gibler WB, Peterson ED. Incidence and prognostic significance of thrombocytopenia developed during acute coronary syndrome in contemporary clinical practice. Circulation. 2009;119:2454-2462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 88] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 7. | Caixeta A, Dangas GD, Mehran R, Feit F, Nikolsky E, Lansky AJ, Aoki J, Moses JW, Steinhubl SR, White HD. Incidence and clinical consequences of acquired thrombocytopenia after antithrombotic therapies in patients with acute coronary syndromes: results from the Acute Catheterization and Urgent Intervention Triage Strategy (ACUITY) trial. Am Heart J. 2011;161:298-306.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 30] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 8. | McClure MW, Berkowitz SD, Sparapani R, Tuttle R, Kleiman NS, Berdan LG, Lincoff AM, Deckers J, Diaz R, Karsch KR. Clinical significance of thrombocytopenia during a non-ST-elevation acute coronary syndrome. The platelet glycoprotein IIb/IIIa in unstable angina: receptor suppression using integrilin therapy (PURSUIT) trial experience. Circulation. 1999;99:2892-2900. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 110] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 9. | Nikolsky E, Sadeghi HM, Effron MB, Mehran R, Lansky AJ, Na Y, Cox DA, Garcia E, Tcheng JE, Griffin JJ. Impact of in-hospital acquired thrombocytopenia in patients undergoing primary angioplasty for acute myocardial infarction. Am J Cardiol. 2005;96:474-481. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 60] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 10. | Berkowitz SD, Sane DC, Sigmon KN, Shavender JH, Harrington RA, Tcheng JE, Topol EJ, Califf RM. Occurrence and clinical significance of thrombocytopenia in a population undergoing high-risk percutaneous coronary revascularization. Evaluation of c7E3 for the Prevention of Ischemic Complications (EPIC) Study Group. J Am Coll Cardiol. 1998;32:311-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 119] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 11. | De Labriolle A, Bonello L, Lemesle G, Roy P, Steinberg DH, Xue Z, Suddath WO, Satler LF, Kent KM, Pichard AD. Decline in platelet count in patients treated by percutaneous coronary intervention: definition, incidence, prognostic importance, and predictive factors. Eur Heart J. 2010;31:1079-1087. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 41] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 12. | Viswanathan G, Kidambi A, Nelson A, Mayurathan G, Hardy J, Kesteven P, Zaman A. Glycoprotein IIb/IIIa inhibitor associated severe thrombocytopenia in patients with coronary artery disease: Clinical course and outcomes. Platelets. 2012;23:224-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Kestin AS, Valeri CR, Khuri SF, Loscalzo J, Ellis PA, MacGregor H, Birjiniuk V, Ouimet H, Pasche B, Nelson MJ. The platelet function defect of cardiopulmonary bypass. Blood. 1993;82:107-117. [PubMed] |
| 14. | Bream-Rouwenhorst HR, Hobbs RA, Horwitz PA. Thrombocytopenia in patients treated with heparin, combination antiplatelet therapy, and intra-aortic balloon pump counterpulsation. J Interv Cardiol. 2008;21:350-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 15. | Naqvi TA, Ikhlaque N, Baumann MA. Thrombocytopenia due to hypotension unrelated to infection: shock marrow. Int J Clin Pract. 2005;59:782-784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 16. | Schiariti M, Puddu PE, Nesta C, Grillo P, Missiroli B, Cassese M. Prophylactic intra-aortic balloon pump is useful to facilitate percutaneous coronary interventions: images from rescue cases. Heart Surg Forum. 2007;10:E411-E414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 17. | Harrington RA, Sane DC, Califf RM, Sigmon KN, Abbottsmith CW, Candela RJ, Lee KL, Topol EJ. Clinical importance of thrombocytopenia occurring in the hospital phase after administration of thrombolytic therapy for acute myocardial infarction. The Thrombolysis and Angioplasty in Myocardial Infarction Study Group. J Am Coll Cardiol. 1994;23:891-898. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 54] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 18. | Kelton JG, Warkentin TE. Heparin-induced thrombocytopenia: a historical perspective. Blood. 2008;112:2607-2616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 129] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 19. | Stribling WK, Slaughter TF, Houle TT, Sane DC. Beyond the platelet count: heparin antibodies as independent risk predictors. Am Heart J. 2007;153:900-906. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 31] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 20. | Warkentin TE, Kelton JG. Temporal aspects of heparin-induced thrombocytopenia. N Engl J Med. 2001;344:1286-1292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 717] [Cited by in RCA: 646] [Article Influence: 26.9] [Reference Citation Analysis (0)] |
| 21. | Geeganage C, Wilcox R, Bath PM. Triple antiplatelet therapy for preventing vascular events: a systematic review and meta-analysis. BMC Med. 2010;8:36. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 39] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 22. | Shantsila E, Lip GY, Chong BH. Heparin-induced thrombocytopenia. A contemporary clinical approach to diagnosis and management. Chest. 2009;135:1651-1664. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 76] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 23. | Aster RH. Immune thrombocytopenia caused by glycoprotein IIb/IIIa inhibitors. Chest. 2005;127:53S-59S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 70] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 24. | Kereiakes DJ, Berkowitz SD, Lincoff AM, Tcheng JE, Wolski K, Achenbach R, Melsheimer R, Anderson K, Califf RM, Topol EJ. Clinical correlates and course of thrombocytopenia during percutaneous coronary intervention in the era of abciximab platelet glycoprotein IIb/IIIa blockade. Am Heart J. 2000;140:74-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 68] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 25. | Gurm HS, Tamhane U, Meier P, Grossman PM, Chetcuti S, Bates ER. A comparison of abciximab and small-molecule glycoprotein IIb/IIIa inhibitors in patients undergoing primary percutaneous coronary intervention: a meta-analysis of contemporary randomized controlled trials. Circ Cardiovasc Interv. 2009;2:230-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 52] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 26. | Steinhubl SR, Tan WA, Foody JM, Topol EJ. Incidence and clinical course of thrombotic thrombocytopenic purpura due to ticlopidine following coronary stenting. EPISTENT Investigators. Evaluation of Platelet IIb/IIIa Inhibitor for Stenting. JAMA. 1999;281:806-810. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 170] [Cited by in RCA: 180] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 27. | Zakarija A, Bandarenko N, Pandey DK, Auerbach A, Raisch DW, Kim B, Kwaan HC, McKoy JM, Schmitt BP, Davidson CJ. Clopidogrel-associated TTP: an update of pharmacovigilance efforts conducted by independent researchers, pharmaceutical suppliers, and the Food and Drug Administration. Stroke. 2004;35:533-537. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 85] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 28. | Bennett CL, Connors JM, Carwile JM, Moake JL, Bell WR, Tarantolo SR, McCarthy LJ, Sarode R, Hatfield AJ, Feldman MD. Thrombotic thrombocytopenic purpura associated with clopidogrel. N Engl J Med. 2000;342:1773-1777. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 465] [Cited by in RCA: 390] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 29. | Grosbois B, Milton D, Beneton C, Jacomy D. Thrombocytopenia induced by angiotensin converting enzyme inhibitors. BMJ. 1989;298:189-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 30. | Srinivasa Rao K, Prasad T, Mohanta GP, Manna PK. An overview of statins as hypolipidemic drugs. Int J Pharm Sci Rev Res. 2011;3:178-183. |
| 31. | Payne BA, Pierre RV. Pseudothrombocytopenia: a laboratory artifact with potentially serious consequences. Mayo Clin Proc. 1984;59:123-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 82] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 32. | Shenoy C, Orshaw P, Devarakonda S, Harjai KJ. Occurrence, predictors, and outcomes of post-percutaneous coronary intervention thrombocytopenia in an unselected population. J Interv Cardiol. 2009;22:156-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 33. | Yusuf SW, Iliescu C, Bathina JD, Daher IN, Durand JB. Antiplatelet therapy and percutaneous coronary intervention in patients with acute coronary syndrome and thrombocytopenia. Tex Heart Inst J. 2010;37:336-340. [PubMed] |
| 34. | Schiariti M, Saladini P, Cuturello D, Iannetta L, Torromeo C, Puddu PE. Decline in platelet count and long-term post-PCI ischemic events: implication of the intra-aortic balloon pump. Vascul Pharmacol. 2014;60:25-31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 35. | Kiviniemi T, Karjalainen P, Rubboli A, Schlitt A, Tuomainen P, Niemelä M, Laine M, Biancari F, Lip GY, Airaksinen KE. Thrombocytopenia in patients with atrial fibrillation on oral anticoagulation undergoing percutaneous coronary intervention. Am J Cardiol. 2013;112:493-498. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 36. | Schiariti M, Saladini A, Missiroli B, Papalia F, Cuturello D, Puddu PE, Gaudio C. Safety of downstream high-dose tirofiban bolus among 1578 patients undergoing percutaneous coronary intervention: the Sant’ANna TIrofiban Safety study. J Cardiovasc Med (Hagerstown). 2010;11:250-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |