Published online Apr 18, 2023. doi: 10.13105/wjma.v11.i4.112
Peer-review started: December 16, 2022
First decision: January 31, 2023
Revised: February 7, 2024
Accepted: April 6, 2023
Article in press: April 6, 2023
Published online: April 18, 2023
Processing time: 119 Days and 3.6 Hours
There is no consensus on the appropriate therapeutic strategy for Boerhaave syndrome due to its rarity and changing therapeutic approaches. We conducted a systematic review of case reports documenting Boerhaave syndrome.
To assess the therapeutic methods and clinical outcomes and discuss the current trends in the management of Boerhaave syndrome.
We searched PubMed, Google scholar, MEDLINE, and The Cochrane Library for studies concerning Boerhaave syndrome published between 2017 and 2022.
Of the included studies, 49 were case reports, including a total of 56 cases. The mean age was 55.8 ± 16 years old. Initial conservative treatment was performed in 25 cases, while operation was performed in 31 cases. The rate of conservative treatment was significantly higher than that of operation in cases of shock vital on admission (9.7% vs 44.0%; P = 0.005). Seventeen out of 25 conservative cases (68.0%) were initially treated endoscopic esophageal stenting; 2 of those 17 cases subsequently underwent operation due to poor infection control. Twelve cases developed postoperative leakage (38.7%), and 4 of those 12 cases underwent endoscopic esophageal stenting to stop the leakage. The length of the hospital stay was not significantly different between the conservative treatment and operation cases (operation vs conservation: 33.52 ± 22.69 vs 38.81 ± 35.28 days; P = 0.553).
In the treatment of Boerhaave syndrome, it is most important to diagnose the issue immediately. Primary repair with reinforcement is the gold-standard procedure. The indication of endoscopic esophageal stenting or endoluminal vacuum-assisted therapy should always be considered for patients in a poor general condition and who continue to have leakage after repair.
Core Tip: Totally 49 published case reports concerning the Boerhaave syndrome were systematically reviewed. In the treatment of Boerhaave syndrome, it is most important to diagnose the issue immediately. Primary repair with reinforcement is the gold-standard procedure. The indication of endoscopic esophageal stenting or endoluminal vacuum-assisted therapy should always be considered for patients in a poor general condition and who continue to have leakage after repair.
- Citation: Yamana I, Fujikawa T, Kawamura Y, Hasegawa S. Current approach for Boerhaaves syndrome: A systematic review of case reports. World J Meta-Anal 2023; 11(4): 112-124
- URL: https://www.wjgnet.com/2308-3840/full/v11/i4/112.htm
- DOI: https://dx.doi.org/10.13105/wjma.v11.i4.112
Since Herman Boerhaave first recognized the disease in 1724, spontaneous esophageal perforation has been described as a medical emergency in the relevant literature[1]. The annual incidence of spontaneous esophageal perforation, also called Boerhaave syndrome, is 3.1 per 1000000; although rare, this condition is associated with high rates of misdiagnosis and mortality[2].
Boerhaave syndrome can be caused by vomiting and is frequently associated with alcohol intoxication[3]. A long period of time between perforation and treatment often results in mediastinitis, followed by septic shock and multiorgan failure[4-10]. Surgery and conservative management are the major treatment options for Boerhaave syndrome. However, few reports have examined whether operation or conservation is the preferred treatment method. Indeed, in the past five years, only one systematic review of Australasian literature on Boerhaave syndrome has been reported[11]. At present, there is no consensus on the optimal therapeutic strategy due to the rarity of Boerhaave syndrome and changing therapeutic approaches.
We therefore reviewed and evaluated 56 cases published in 49 case report articles in PubMed, Google scholar, MEDLINE, and The Cochrane Library in the past 5 years to assess the therapeutic methods and clinical outcomes and discuss the current trends in the management of Boerhaave syndrome.
A case report literature review was conducted using Pubmed, Google scholar, Cochrane Library, and MEDLINE for articles published between October 2017 and October 2022. The search was limited to articles in English. “Boerhaave syndrome” or “spontaneous esophageal perforation” were key words in the search. All titles and abstracts of publications were screened to select articles describing Boerhaave syndrome or spontaneous esophageal perforation. The searches were further broadened by extensively checking all references in the articles retrieved that met the inclusion criteria.
The inclusion criterion was patients who underwent operation or conservative therapy for Boerhaave syndrome. The exclusion criteria were meta-analyses, reviews, articles without outcomes reported, articles without the operation method reported, articles involving cases of treatment refusal, articles involving recurrent cases of esophageal perforation, articles involving best supportive care, articles involving pediatric cases, articles focusing on other diseases, and articles in non-English languages.
The study design, and data on the patients’ demographics, interventions, and outcomes were extracted from the included studies. An independent researcher collected the study data using a standard Excel™ data collection sheet (Microsoft Corporation, Japan). This spreadsheet was used to calculate the descriptive statistics of all parameters that were evaluated in the present study. Continuous and categorical variables were shown as the mean and standard deviation (SD) and range.
The overall quality of the cases was classified as good to moderate. The majority of patients adequately described the chief complaint (100%), the patient’s medical history (82.1%), the sex (98.2%), the length from symptom onset (98.2%), the length of the hospital stay (76.8%), imaging findings (100%), treatments (100%), and outcomes (100%).
All values were presented as the mean ± SD. Intergroup differences were evaluated by an analysis of variance, while a nonparametric analysis was conducted for data with a skewed distribution. Statistical analyses were performed using EZR (Saitama Medical Center, Jichi Medical University)[12]. EZR for R (The R Foundation for Statistical Computing, version 2.13.0) is a modified version of the R commander (version 1.6–3) that includes statistical functions that are frequently used in biostatistics. P values of < 0.05 were considered statistically significant.
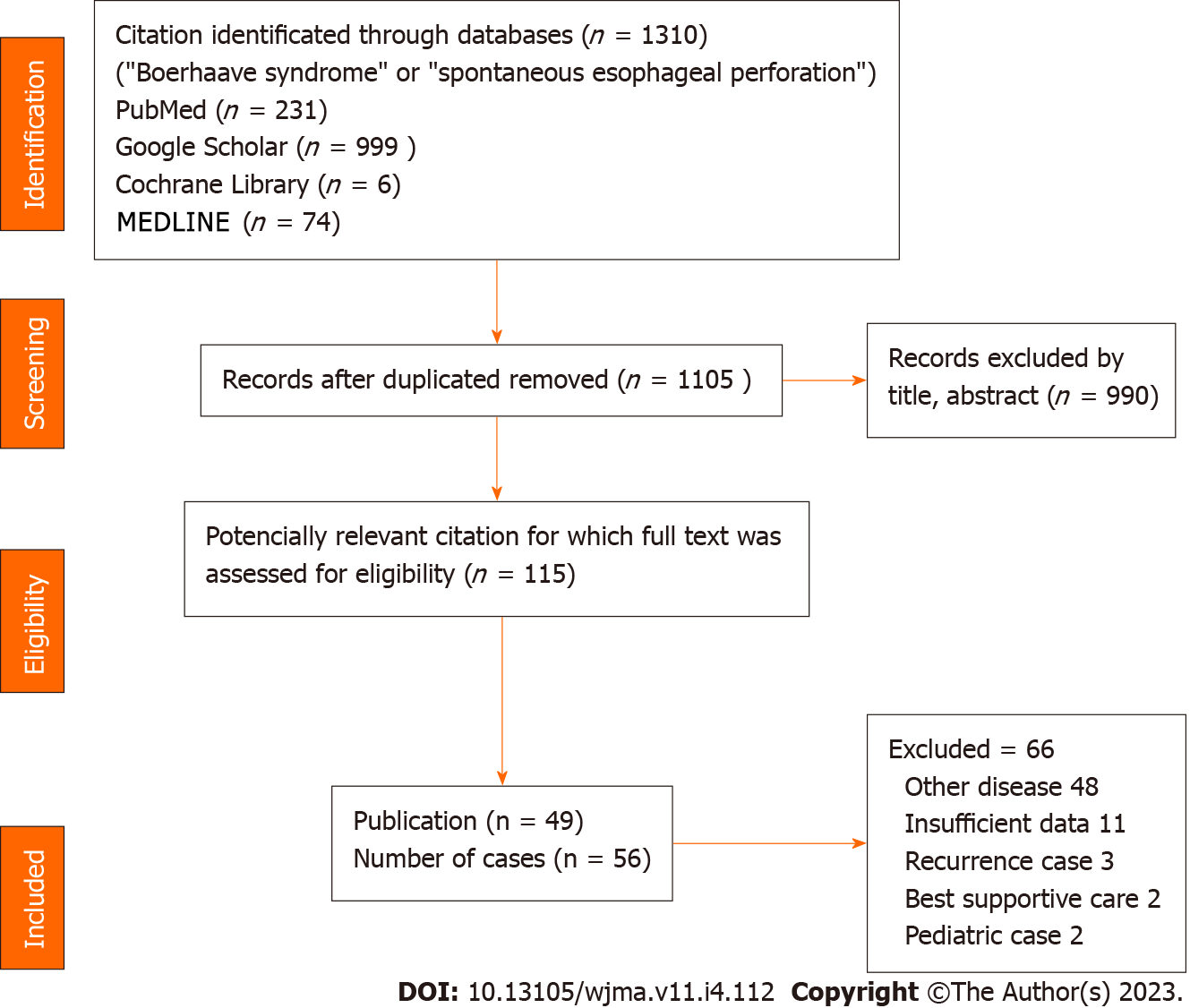
The results of the literature search are shown in Figure 1. Through our search, we identified 1310 studies. Of these, 990 studies were excluded by title and abstract. Of the remaining 115 potentially relevant articles, we excluded 48 concerning other diseases, 11 with insufficient data, 3 concerning recurrence cases, 2 involving best supportive care, and 2 pediatric cases. This resulted in the inclusion of 49 case report articles involving 56 cases for this study.
Table 1 shows the details of the included studies. Of the 55 patients whose sex was mentioned, 51 were male, and 4 were female (1 case with no information). The mean age was 55.8 ± 16 years old. Thirty-six of the 55 cases (65.5%) were referred to the hospital within 24 h after symptom onset (1 case with no information). The most common method of the diagnosis was computed tomography (n = 31), followed by esophagography (n = 15), endoscopy (n = 9), and exploratory laparotomy (n = 1). A total of 42 cases (75%) were accurately diagnosed on admission. Fourteen patients (25%) showed shock vitals when they arrived at the hospital. Twelve (21.4%) were intra-mediastinum type, and 44 (78.6%) were extra-mediastinum type. The mean (range) size of the laceration in the 30 cases for which such details were described was 3.8 (1-12) cm (Table 2).
| Ref. | Age | Sex | Accurate diagnosis | Rupture type | Shock vital | Laceration size (cm) | Treatment | Prognosis |
| Jahangir et al[4], 2021 | 64 | M | Yes | Intrapleural type | Yes | 1 | Stent, thoracic drainage | Death |
| Issa et al[23], 2019 | 32 | M | Yes | Intrapleural type | No | 2 | Stent, thoracic drainage | Alive |
| Tan et al[5], 2022 | 84 | M | No | Intrapleural type | No | Unknown | Thoracotomy, primary repair only | Death |
| Chang et al[13], 2021 | 67 | M | Yes | Intrapleural type | No | 3 | Thoracopy, primary repair only, feeding jejunostomy | Alive |
| Chang et al[13], 2021 | 62 | M | Yes | Intrapleural type | No | 2 | Thoracopy, primary repair only, feeding jejunostomy | Alive |
| Sheshala et al[24], 2021 | 39 | M | No | Intrapleural type | Yes | Unknown | Stent, thoracic drainage | Alive |
| Matsumoto et al[25], 2019 | 60 | M | No | Intrapleural type | Yes | Unknown | Stent, thoracic drainage | Alive |
| Ayazi et al[6], 2021 | 22 | M | Yes | Intrapleural type | Yes | Unknown | Thoracotomy, esophagectomy, gastrostomy | Death |
| Maki et al[44], 2022 | 76 | M | Yes | Intramediastinal type | No | 7 | Transhiatal approach, primary repair plus omentoplasty, feeding jejunostomy | Alive |
| Ioannidis et al[39], 2021 | 83 | F | Yes | Intrapleural type | No | Unknown | Thoracic drainage | Alive |
| Y K et al[26], 2018 | 86 | M | Yes | Intrapleural type | Yes | 5 | Stent, thoracic drainage, feeding jejunostomy | Alive |
| Czopnik et al[3], 2017 | 47 | M | Yes | Intrapleural type | No | 5 | Transhiatal approach, primary repair, gastrostomy | Alive |
| Awadelkarim et al[27], 2021 | 36 | M | Yes | Intrapleural type | Yes | 2 | Stent, thoracic drainage | Alive |
| Chalikonda et al[28], 2019 | 74 | M | No | Intrapleural type | Yes | Unknown | Stent, thoracic drainage | Alive |
| Śnieżyński et al[29], 2021 | 53 | M | Yes | Intrapleural type | No | 3 | Stent, thoracic drainage | Alive |
| Matsuura et al[21], 2022 | 69 | M | Yes | Intramediastinal type | No | Unknown | Endoscopic clipping | Alive |
| Chen et al[19], 2021 | 57 | M | No | Intramediastinal type | No | Unknown | Transhiatal approach, primary repair only, feeding jejunostomy | Alive |
| Truyens et al[30], 2020 | 66 | M | Yes | Intramediastinal type | Yes | Unknown | Antibiotic administration | Alive |
| Truyens et al[30], 2020 | 77 | M | Yes | Intramediastinal type | No | Unknown | Stent | Alive |
| Swol et al[7], 2019 | 70 | M | Yes | Intramediastinal type | No | 2 | Transhiatal approach, primary repair plus fundus pauch | Death |
| Park et al[45], 2021 | Unknown | Unknown | Yes | Intramediastinal type | No | 5 | Laparoscopic transhiatal approch, primary repair plus omentoplasty → endoscopic clipping, stent | Alive |
| Rahman et al[49], 2021 | 53 | M | Yes | Intrapleural type | No | Unknown | Thoracotomy, primary repair plus intercostal muscle pauch, gastro-jujuno tube → stent | Alive |
| Nachiappan et al[46], 2022 | 59 | M | No | Intrapleural type | No | 1,5 | Endscopic clipping, stent → laparoscopic transhiatal approach, primary repair plus omentoplasty | Alive |
| Pasternak et al[14], 2019 | 37 | M | Yes | Intrapleural type | No | Unknown | Thoracotomy, primary repair only, gastrostomy | Alive |
| Kita et al[55], 2022 | 46 | M | Yes | Intramediastinal type | No | 4 | Laparoscopic transhiatal approch, primary repair plus fundus pauch | Alive |
| Kita et al[55], 2022 | 48 | M | Yes | Intramediastinal type | No | 3 | Laparoscopic transhiatal approch, primary repair plus fundus pauch | Alive |
| Kita et al[55], 2022 | 65 | M | Yes | Intramediastinal type | No | 5 | Laparoscopic transhiatal approch, primary repair plus fundus pauch | Alive |
| Saffo et al[8], 2021 | 76 | M | No | Intrapleural type | Yes | Unknown | Stent, thoracic drainage | Death |
| Kochar et al[50], 2019 | 40 | M | Yes | Intrapleural type | Yes | Unknown | Thoracotomy, primary repair plus intercostal muscle pauch, intraoperative stent, thoracic drainage | Alive |
| Bury et al[51], 2022 | 50 | M | No | Intrapleural type | No | 4 | Thoracotomy, primary repair plus intercostal muscle pauch, thoracic drainage | Alive |
| Aref et al[47], 2019 | 32 | M | Yes | Intramediastinal type | No | 2 | Laparoscopic transhiatal approach, primary repair plus omentoplasty | Alive |
| Bani Fawwaz et al[15], 2022 | 63 | M | Yes | Intrapleural type | Yes | 3 | Stent, thoracic drainage | Alive |
| Bani Fawwaz et al[15], 2022 | 56 | F | Yes | Intrapleural type | No | Unknown | Thoracotomy, primary repair plus T tube, Belsey fundoplication, intraoperative stent, thoracic drainage, gastrostpomy | Alive |
| Xu et al[22], 2021 | 63 | M | Yes | Intrapleural type | No | Unknown | Endoscopic clipping | Alive |
| Tuñon et al[57], 2021 | 24 | M | Yes | Intrapleural type | No | 4 | Endoluminal vacuum therapy → endoscopic clipping | Alive |
| Lee et al[58], 2018 | 52 | M | Yes | Intrapleural type | No | Unknown | Thoracoscopic approach, primary repair only → endoluminal vacuum therapy, thoracic drainage | Alive |
| He et al[54], 2018 | 57 | M | Yes | Intramediastinal type | No | 6 | Endoscopic clipping | Death |
| Kim et al[59], 2019 | 56 | M | Yes | Intrapleural type | No | Unknown | Thoracotomy, primary repair only → endoluminal vacuum therapy, thoracic drainage | Alive |
| Shennib et al[52], 2021 | 47 | M | No | Intrapleural type | Yes | 5 | Thoracotomy, primary repair plus pericardial pauch, gastrostomy, feeding jejunostomy | Alive |
| Agrawal et al[40], 2019 | 26 | M | No | Intrapleural type | No | Unknown | thoracic drainage | Alive |
| Sato et al[31], 2018 | 52 | M | Yes | Intrapleural type | No | Unknown | Thoracotomy, primary repair only → stent, thoracic drainage | Alive |
| Sato et al[31], 2018 | 53 | M | No | Intrapleural type | Yes | Unknown | Stent, thoracic drainage | Alive |
| Ali et al[16], 2020 | 30 | F | No | Intrapleural type | No | 4 | Thoracotomy, primary repair only | Alive |
| Anand et al[48], 2022 | 64 | M | Yes | Intrapleural type | No | 2 | Thoracotomy, primary repair plus intercostal muscle pauch, thoracic drainage | Alive |
| Barakat et al[32], 2017 | 62 | M | Yes | Intrapleural type | No | 1 | Stent, endoscopic clipping | Alive |
| Alakkari et al[17], 2019 | 69 | F | Yes | Intrapleural type | No | Unknown | Thoracotomy, primary repair plus T tube | Alive |
| Zhu et al[18], 2021 | 33 | M | No | Intrapleural type | No | Unknown | Stent, PEG →thoracotomy, drainage | Alive |
| Sekiya et al[56], 2019 | 61 | M | Yes | Intrapleural type | No | 3 | Thoracoscopic and laparoscopic approach, primary repair plus pericardial pauch, gastrostomy | Alive |
| Sekiya et al[56], 2019 | 64 | M | Yes | Intrapleural type | No | 4 | Thoracoscopic and laparoscopic approach, primary repair plus pericardial pauch, feeding jejunostomy | Alive |
| Olivero et al[53], 2019 | 67 | M | No | Intrapleural type | No | 2 | Thoracotomy, primary repair plus pericardial pauch, thoracic drainage | Alive |
| Felipe et al[38], 2021 | 47 | M | Yes | Intrapleural type | No | 12 | Thoracotomy and laparotomy approach, esophagostomy, gastrostomy → stent | Alive |
| Ahmad et al[33], 2018 | 63 | M | Yes | Intrapleural type | No | 2.5 | Stent, thoracic drainage | Alive |
| Hashmi et al[10], 2021 | 83 | M | Yes | Intrapleural type | Yes | Unknown | Antibiotic administration | Death |
| Teblick et al[34], 2018 | 74 | M | Yes | Intrapleural type | No | Unknown | Stent, thoracic drainage | Alive |
| He et al[9], 2018 | 27 | M | Yes | Intrapleural type | No | 6 | Thoracotomy, primary repair plus pleural flap, feeding jejunostomy | Alive |
| Sex | aMale 51, female 4 | |
| Age | 55.8 ± 16 | |
| The length from symptom within 24 h | b36 (65.5) | |
| The method of diagnosis | CT | 31 |
| Esophagography | 15 | |
| Endoscopy | 9 | |
| Exploratory laparotomy | 1 | |
| Accurate diagnosis on admission | 42 (75) | |
| Shock vital on admission | 14 (25) | |
| Rupture type | Intramediastinal | 12 (21.4) |
| Extramediatinal | 44 (78.6) | |
| Lacelation size (cm) (range) | c3.8 (1-12) |
Conservative treatment was performed in 25 cases, while operation was performed in 31 cases. Conservative treatment included endoscopic esophageal stents in 17 cases, endoscopic clipping in 5, thoracic drainage in 21, and endoluminal vacuum-assisted (EVAC) therapy in 1. The operation approach was trans-thoracic and trans-abdominal approaches in 18 and 10 cases, respectively; a combined trans-abdominal and trans-thoracic approach was performed in 3 cases. In the trans-thoracic approach, minimally invasive surgery was performed in 5 cases (23.8%). In the trans-abdominal approach, minimally invasive surgery was performed in 8 cases (61.5%). The operation methods were primary repair only in eight cases, primary repair with omentoplasty in six cases, primary repair with fundus pouch in six cases, primary repair with intercostal muscle pouch in five cases, primary repair with pericardial fat pouch in five cases, T tube in two cases, esophagectomy in one case, and esophagostomy in one case. Twelve out of 31 cases (38.7%) developed postoperative leakage. Two of those cases underwent EVAC therapy, and four of the cases underwent endoscopic esophageal stenting. Seven out of the 56 total cases (12.5%) died following treatment for Boerhaave syndrome; notably, 4 of those 7 cases (57.1%) had already had shock vitals on arrival at the hospital (Table 3).
| The number do not add up because of duplication case | |||
| Conservation (n = 25)a | Esophageal stent | 17 | |
| Clipping | 5 | ||
| Thoracic drainage | 21 | ||
| EVACb | 1 | ||
| Operation (n = 31) | Approach | Trans-thoracic approach | 18 |
| Trans-abdominal approach | 10 | ||
| Trans-thoracic and abdominal approach | 3 | ||
| Method | Primary repair only | 8 | |
| Primary repair with omentoplasty | 6 | ||
| Primary repair with fundus pauch | 6 | ||
| Primary repair with intercostal muscle pauch | 5 | ||
| Primary repair with pericardial fat pauch | 5 | ||
| T tube | 2 | ||
| Esophagectomy | 1 | ||
| Esophagostomy and gastrostomy | 1 |
Seventeen cases underwent endoscopic esophageal stenting initially, and 14 of them (82.4%) had severe comorbidities. Ten of the 17 cases (58.8%) who underwent endoscopic esophageal stenting had had shock vitals on arrival at the hospital. One case (14.3%) was the intra-mediastinum type, while the other 16 (85.7%) were the extra-mediastinum type. Two of the 17 cases who underwent endoscopic esophageal stenting had initially undergone operation due to poor infection control.
Four of the cases who initially underwent operation consequently underwent endoscopic esophageal stenting to stop leakage.
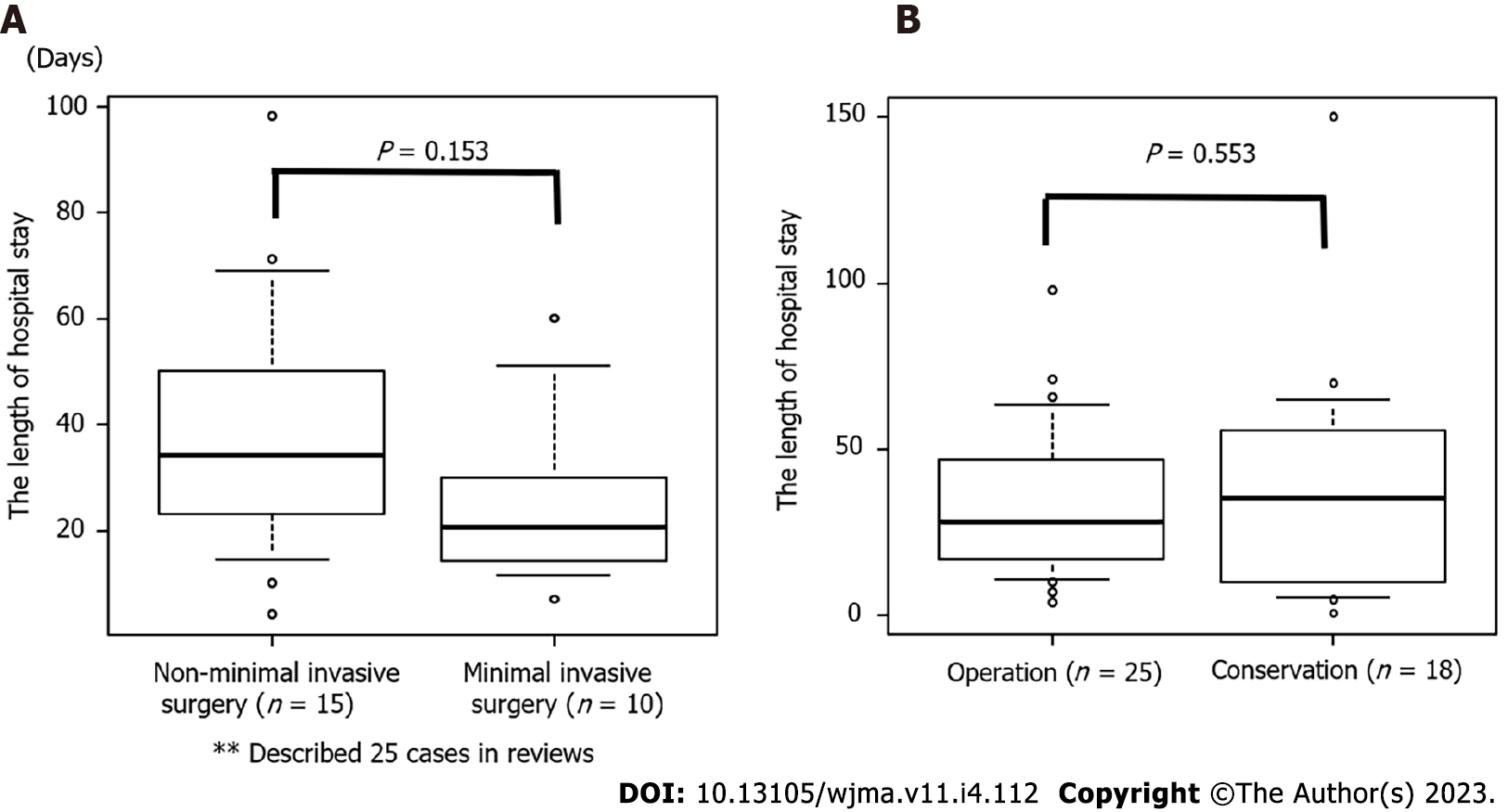
Eleven out of 31 cases (35.5%) underwent minimally invasive surgery. Seven of the 13 cases (53.8%) who underwent the trans-abdominal approach received the trans-hiatal approach specifically with laparoscopic surgery. Five of the 21 cases (23.8%) who underwent the trans-thoracic approach received thoracoscopic surgery. The length of the hospital stay after surgery tended to be shorter with minimally invasive surgery than with non-minimally invasive surgery [minimally invasive surgery (n = 10) vs non-minimally invasive surgery (n = 15): 25.5 ± 17.1 vs 38.86 ± 24.85 d; P = 0.153] (Figure 2A).
Table 4 shows the differences in details between patients who underwent an operation and those who received conservative treatment. The sex, age, rate of patients admitting within 24h after symptom onset, rupture type, and rate of survival did not significantly differ between patients who underwent an operation and those who received conservative treatment. The rate of patients with shock vitals on admission did differ significantly between patients who underwent an operation and those who received conservative treatment (9.7% vs 44.0%; P = 0.005). The length of hospital stay was not significantly different among the 43 cases (operation vs conservative treatment: 33.52 ± 22.09 vs 38.81 ± 35.28 d; P = 0.55) (Figure 2B).
| Factor | Group | Operation (n = 31) | Conservation (n = 25) | Pvalue |
| Sex (%) | M | 27 (90.0) | 24 (96.0) | 0.617 |
| F | 3 (10.0) | 1 ( 4.0) | ||
| mean ± SD | 53.17 (14.68) | 59.00 (18.14) | 0.193 | |
| The length from symptom within 24 h (%) | Yes | 10 (32.3) | 9 (36.0) | 1 |
| No | 20 (64.5) | 16 (64.0) | ||
| Shock vital on admission (%) | Yes | 3 ( 9.7) | 11 (44.0) | 0.005 |
| No | 28 (90.3) | 14 (56.0) | ||
| rupture type | Intramediastinal (%) | 8 (25.8) | 4 (16.0) | 0.516 |
| Extramediastinal (%) | 23 (74.2) | 21 (84.0) | ||
| Alive (%) | Yes | 28 (90.3) | 21 (84.0) | 0.688 |
| No | 3 ( 9.7) | 4 (16.0) |
Primary surgical repair has been the gold-standard treatment for esophageal perforation for a long time[13-19]. Primary repair of the esophagus conducted with mediastinal and thoracic drainage is reported to have a 90% success rate. Cases in which esophageal rupture is diagnosed at an early stage (within 24 h) without associated esophageal disease are reported to show a particularly high success rate[20]. There has been a recent trend toward more non-operative management[21,22], such as esophageal stent replacement via an endoscopic approach[23-32]. The indications for esophageal stenting include multiple comorbidities, advanced mediastinal sepsis, hemodynamic compromise, and clinical intolerance of extensive surgical repair[33]. In our review, the rate of conservation was significantly higher than that of operation in instances of shock vital on admission (44.0% vs 9.7%; P = 0.005).
Esophageal stenting was able to be attempted for patients who were in a bad general condition or intolerant to surgery[34]. Endoscopic esophageal stenting was also performed for cases of postoperative leakage. Kauer et al[35] in 2008 first described the usefulness of stent placement in the management of thoracic anastomotic leakage after esophagectomy. An interval approach utilizing covered metallic stent was then introduced for the management of anastomotic leakage after esophagectomy[36]. However, no prospective clinical study comparing the outcomes of esophageal stenting to that of conservative/surgical treatment has yet been performed. Bi et al[37] reported that the efficacy of the three-tube method, (tube drainage of the abscess, placement of a jejunal feeding tube, and placement of a gastrointestinal decompression tube, with implantation of a covered metallic stent) for the management of anastomotic leakage following esophagectomy. This means that it is important not only to place esophageal stents but also to provide adequate drainage, a concept that can also be applied for treating Boerhaave syndrome.
Surgical approaches differed among facilities in our review. The operation approach in our evaluated studies was the trans-thoracic approach in 18 cases, trans-abdominal approach in 10 cases, and combined trans-thoracic and trans-abdominal approach in 3 cases. The approach seemed to differ depending on laceration site, the patient’s general condition, and whether the operator was a thoracic surgeon or a gastrointestinal surgeon. The reported operative methods for Boerhaave syndrome include primary repair (with/without reinforcement), an exclusion diversion operation[38], esophageal resection, and simple thoracic drainage[39-40]. Previous reports mentioned that reinforcement with vascularized tissue was associated with reduced fistula formation and mortality rates in comparison to repair without reinforcement[41-43]. In the case of friability of the tissue, primary repair with reinforcement, such as omental flaps[44-47], intercostal muscle flaps[48-51], and pericardial flaps[52-54], should be performed. A comprehensive evaluation of the degree of laceration, extent of laceration, and general condition required for deciding the repair method should be conducted.
There have been a few recent reports concerning minimally invasive surgery for Boerhaave syndrome. Kita et al[55] suggested that a good clinical course can be obtained by laparoscopic trans-hiatal esophageal repair for Boerhaave's syndrome with localized mediastinal collections to avoid surgical invasion due to thoracotomy. Sekiya et al[56] reported the convenience and usefulness of minimally invasive surgery via an abdominal and left thoracic approach, which provides excellent visualization of the abdominal and thoracic cavities and facilitates quick switching between views. The authors further suggested that, in cases with an interval to the diagnosis < 24 h, no severe comorbidities, and a perforation site in the left lower esophagus, a trans-hiatal approach for minimally invasive surgery is feasible to repair the laceration and ameliorate the infection[56]. In our systematic review, the length of hospital stay after minimally invasive surgery tended to be shorter than after non-minimally invasive surgery (25.5 ± 17.1 vs 38.86 ± 24.85 d; P = 0.153). Minimally invasive surgery is useful for its cosmetic aspect, camera magnification effect, and ease of suturing, especially a laparoscopic trans-hiatal approach.
In our systematic review, 12 out of 31 cases (38.7%) developed postoperative leakage. Two of those 13 Leakage cases underwent EVAC therapy. Recently, the efficacy of EVAC therapy for esophago-pleural fistula after an operation for Boerhaave syndrome was reported[57-59]. EVAC therapy can be applied in postoperative management according to the principle applied for external wounds that provide wound drainage and tissue granulation. EVAC therapy can be applied to conservatively treat cases where primary surgical repair of esophageal perforation is unsuccessful. Moreover, with the use of an S-B tube, the patient can simultaneously receive intraluminal EVAC therapy with enteral nutrition in a non-invasive manner[58]. This may accelerate the healing of the injured esophagus and reduce the duration of hospitalization.
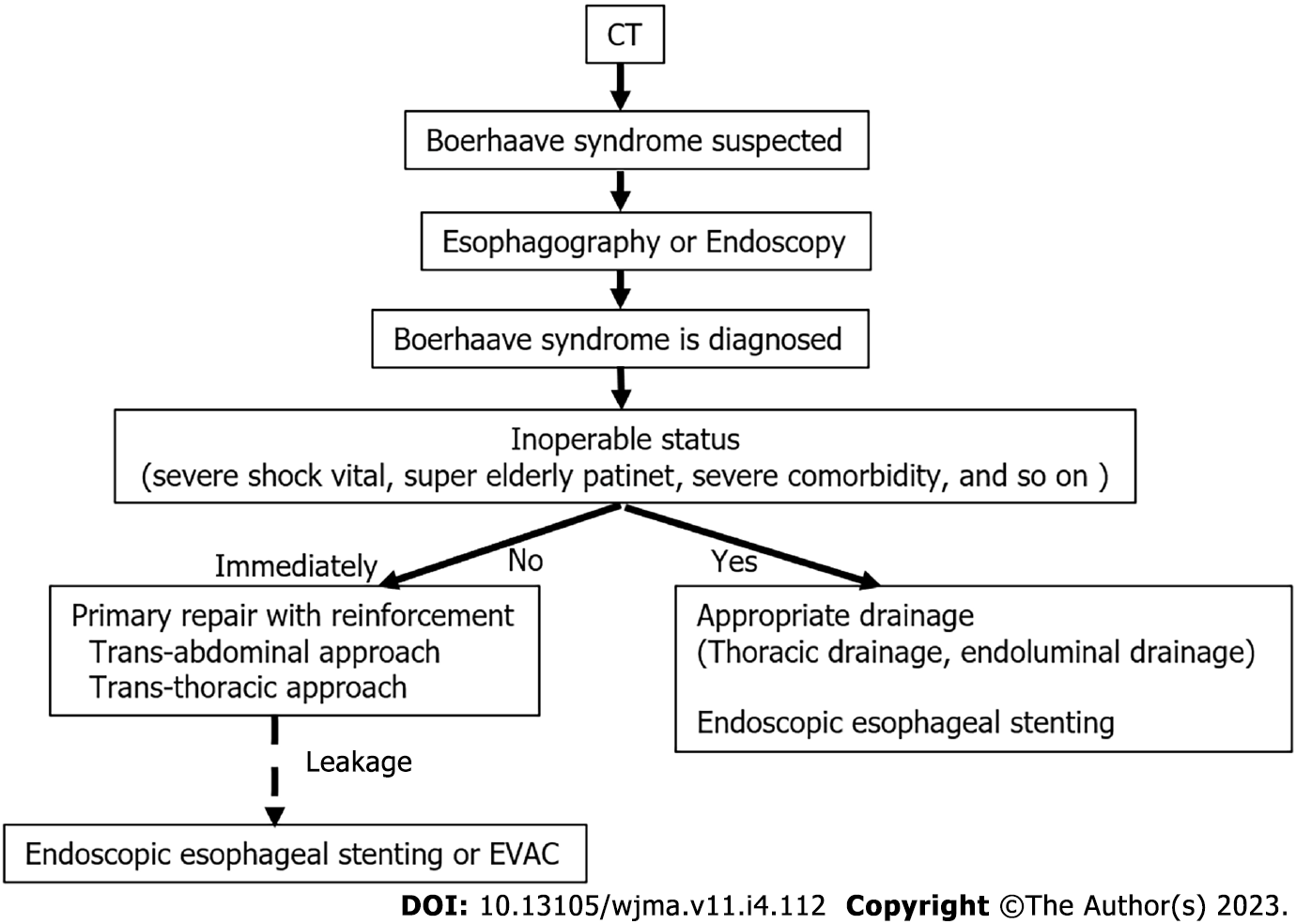
We suggest an algorithm that might be useful in the treatment of Boerhaave syndrome in Figure 3, with reference to our systematic review. If Boerhaave syndrome is suspected on computed tomography, esophagography or upper gastrointestinal endoscopy should be performed immediately. The treatment of Boerhaave syndrome is basically primary repair with reinforcement. If postoperative leakage occurs, endoscopic esophageal stenting or EVAC therapy should be considered. If the patient is inoperable (severe shock vitals, super-elderly patients, severe comorbidities, etc.), endoscopic esophageal stenting and thoracic drainage should be considered.
Several limitations associated with the present study warrant mention. Importantly, due to its rarity, there are few large case series on Boerhaave syndrome. Furthermore, the therapeutic strategies for Boerhaave syndrome have changed over time, with new approaches being developed recently. We reviewed and analyzed 49 articles; however, the review process may have included various publication biases.
In the treatment of Boerhaave syndrome, it is most important to diagnose the issue immediately. Primary repair with reinforcement is the gold-standard procedure. The optimal treatment should be determined according to the etiology, general physical condition of the patient, and site of perforation, as well as the extent of contamination, as determined by radiology. The indication of endoscopic esophageal stenting or endoluminal vacuum-assisted therapy should always be considered for patients in a poor general condition and who continue to have leakage after repair.
As far, it has long been reported that Boerhaave syndrome has a poor prognosis when diagnosed late. However, no consensus has been reached concerning the appropriate therapeutic strategy for Boerhaave syndrome because of the rarity of the disease and the changing therapeutic trends.
We assess the therapeutic methods [operation vs drainage vs stent vs endoluminal vacuum-assisted (EVAC), etc.] and clinical outcomes and discuss the current trends in the management of Boerhaave syndrome.
We believe that this systematic review will be useful in future treatment of Boerhaave syndrome when there is doubt as to whether conservative treatment or surgery should be done, as well as the method of surgery.
We searched PubMed, Google scholar, MEDLINE, and The Cochrane Library for studies concerning Boerhaave syndrome published between 2017 and 2022.
In results, the key to treatment of Boerhaave syndrome was early diagnosis. In addition, although surgery was the basic treatment, esophageal stents and drainage may be useful for patients with intolerance. Furthermore, for postoperative leakage, esophageal stents, drainage, and EVAC were useful.
In the treatment of Boerhaave syndrome, it is most important to diagnose the issue immediately. Primary repair with reinforcement is the gold-standard procedure. The indication of endoscopic esophageal stenting or endoluminal vacuum-assisted therapy should always be considered for patients in a poor general condition and who continue to have leakage after repair.
Because Boerhaave syndrome is a rare disease, observational studies should be conducted in collaboration with other centers. We hope that this will result in a high-quality strategy.
We gratefully acknowledge the work of past and present members.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Fakhradiyev I, Kazakhstan; Giordano A, Italy S-Editor: Liu JH L-Editor: A P-Editor: Yu HG
| 1. | Adams BD, Sebastian BM, Carter J. Honoring the Admiral: Boerhaave-van Wassenaer's syndrome. Dis Esophagus. 2006;19:146-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 2. | Vidarsdottir H, Blondal S, Alfredsson H, Geirsson A, Gudbjartsson T. Oesophageal perforations in Iceland: a whole population study on incidence, aetiology and surgical outcome. Thorac Cardiovasc Surg. 2010;58:476-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 101] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 3. | Czopnik P, Aporowicz M, Niepokój-Czopnik A, Szajerka T, Domosławski P. Barogenic rupture of esophagus (Boerhaave syndrome) as diagnostic and therapeutic challenge requiring rapid and effective interdisciplinary cooperation - case report. Pol Przegl Chir. 2017;89:37-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 4. | Jahangir A, Sahra S, Anwar S, Mobarakai N, Jahangir A. Catastrophic right-sided Candida empyema from spontaneous esophageal perforation. Respir Med Case Rep. 2021;33:101460. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Tan N, Luo YH, Li GC, Chen YL, Tan W, Xiang YH, Ge L, Yao D, Zhang MH. Presentation of Boerhaave's syndrome as an upper-esophageal perforation associated with a right-sided pleural effusion: A case report. World J Clin Cases. 2022;10:6192-6197. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 1] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Ayazi K, Samsami M, Qaderi S, Farsad SM, Tofigh AM, Nematihonar B, Tahmasbi H, Bagherour JZ. Spontaneous perforation as a fatal presentation of esophageal tuberculosis: A case report. Int J Surg Case Rep. 2021;78:197-200. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 7. | Swol J, Ficker JH, Mannke B. Cervical Emphysema in Boerhaave Syndrome. Dtsch Arztebl Int. 2019;116:211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Saffo S, Farrell J, Nagar A. Circumferential esophageal perforation resulting in tension hydropneumothorax in a patient with septic shock. Acute Crit Care. 2021;36:264-268. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 9. | He F, Dai M, Zhou J, He J, Ye B. Endoscopic repair of spontaneous esophageal rupture during gastroscopy: A CARE compliant case report. Medicine (Baltimore). 2018;97:e13422. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Hashmi MAR, El-Badawy M, Agha A. Suspecting a fatal condition on a plain chest radiograph; Boerhaave syndrome. Scott Med J. 2021;66:46-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Allaway MGR, Morris PD, B Sinclair JL, Richardson AJ, Johnston ES, Hollands MJ. Management of Boerhaave syndrome in Australasia: a retrospective case series and systematic review of the Australasian literature. ANZ J Surg. 2021;91:1376-1384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 12. | Kanda Y. Investigation of the freely available easy-to-use software 'EZR' for medical statistics. Bone Marrow Transplant. 2013;48:452-458. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9275] [Cited by in RCA: 13270] [Article Influence: 1105.8] [Reference Citation Analysis (0)] |
| 13. | Chang CW, Hung YJ, Chan CP, Huang CL. Spontaneous esophageal rupture following perforated peptic ulcer: a report of two cases. J Cardiothorac Surg. 2021;16:57. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 14. | Pasternak A, Ellero J, Maxwell S, Cheung V. Boerhaave's syndrome in an ultra-distance runner. BMJ Case Rep. 2019;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Bani Fawwaz BA, Gerges P, Singh G, Rahman SH, Al-Dwairy A, Mian A, Khan N, Farooq A. Boerhaave Syndrome: A Report of Two Cases and Literature Review. Cureus. 2022;14:e25241. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 16. | Ali N, Abate G. Candida Empyema as a Red Flag for Esophageal Rupture: A Case Report and Literature Review. Case Rep Infect Dis. 2020;2020:3935691. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 17. | Alakkari A, Sood R, Everett SM, Rembacken BJ, Hayden J, Sarela A, Mohammed N. First UK experience of endoscopic vacuum therapy for the management of oesophageal perforations and postoperative leaks. Frontline Gastroenterol. 2019;10:200-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 18. | Zhu C, Castrodad A, Santos AP. Alternative management of delayed spontaneous oesophageal perforation by endoscopic stenting. BMJ Case Rep. 2021;14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 19. | Chen JJ, Zhao W. Boerhaave's syndrome: A case of spontaneous oesophageal rupture. Indian J Med Res. 2021;154:156. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 20. | de Schipper JP, Pull ter Gunne AF, Oostvogel HJ, van Laarhoven CJ. Spontaneous rupture of the oesophagus: Boerhaave's syndrome in 2008. Literature review and treatment algorithm. Dig Surg. 2009;26:1-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 105] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 21. | Matsuura N, Saitou K. Boerhaave's Syndrome. Intern Med. 2022;61:265-266. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 22. | Xu H, Huang D, He C. Boerhaave's syndrome with rupture of the right wall of the esophagus after oral administration of sulfate solution. Rev Esp Enferm Dig. 2021;113:677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 23. | Issa D, Alwatari Y, Smallfield GB, Shah RD. Spontaneous transmural perforation in eosinophilic esophagitis: RARE case presentation and role of esophageal stenting. J Surg Case Rep. 2019;2019:rjz190. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 24. | Sheshala K, Kumar GN, Misra KC, Hemanth C, Appasani S. Bee Sting to Boerhaave's Syndrome. Indian J Crit Care Med. 2021;25:346-348. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 25. | Matsumoto R, Sasaki K, Omoto I, Noda M, Uchikado Y, Arigami T, Kita Y, Mori S, Maemura K, Natsugoe S. Successful conservative treatment of spontaneous intrathoracic esophageal perforation using a temporary covered esophageal stent with a check valve: a case report. Surg Case Rep. 2019;5:152. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 26. | Y K, F AB, A T, D H. Boerhaave syndrome in an elderly man successfully treated with 3-month indwelling esophageal stent. Radiol Case Rep. 2018;13:1084-1086. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 27. | Awadelkarim A, Shanah L, Ali M, Alhusain R, Adam O, Subahi A, Yassin AS, Lieberman R. Esophago-Pericardial Fistulae as a Sequela of Boerhaave Syndrome and Esophageal Stenting: A Case Report and Review of Literature. J Investig Med High Impact Case Rep. 2021;9:23247096211036540. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (1)] |
| 28. | Chalikonda D, Yoo J, Johnson D, Tofani C. Boerhaave Syndrome Causing Bilateral Empyemas. ACG Case Rep J. 2019;6:e00203. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 29. | Śnieżyński J, Wilczyński B, Skoczylas T, Wallner GT. Successful Late Endoscopic Stent-Grafting in a Patient with Boerhaave Syndrome. Am J Case Rep. 2021;22:e931629. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 30. | Truyens M, Hufkens E, Van Geluwe B, Vergauwe P, Van Moerkercke W. Boerhaave's syndrome: successful conservative treatment in two patients. Acta Gastroenterol Belg. 2020;83:654-656. [PubMed] |
| 31. | Sato H, Ishida K, Sasaki S, Kojika M, Endo S, Inoue Y, Sasaki A. Regulating migration of esophageal stents - management using a Sengstaken-Blakemore tube: A case report and review of literature. World J Gastroenterol. 2018;24:3192-3197. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 5] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 32. | Barakat MT, Girotra M, Banerjee S. (Re)building the Wall: Recurrent Boerhaave Syndrome Managed by Over-the-Scope Clip and Covered Metallic Stent Placement. Dig Dis Sci. 2018;63:1139-1142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 33. | Ahmad W, Kwong WT. Boerhaave's Syndrome: A Window to the Heart. Clin Gastroenterol Hepatol. 2018;16:e77-e78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 34. | Teblick A, Jansens H, Dams K, Somville FJ, Jorens PG. Boerhaave's syndrome complicated by a Saccharomyces cerevisiae pleural empyema. Case report and review of the literature. Acta Clin Belg. 2018;73:377-381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 35. | Kauer WK, Stein HJ, Dittler HJ, Siewert JR. Stent implantation as a treatment option in patients with thoracic anastomotic leaks after esophagectomy. Surg Endosc. 2008;22:50-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 100] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 36. | van Boeckel PG, Dua KS, Weusten BL, Schmits RJ, Surapaneni N, Timmer R, Vleggaar FP, Siersema PD. Fully covered self-expandable metal stents (SEMS), partially covered SEMS and self-expandable plastic stents for the treatment of benign esophageal ruptures and anastomotic leaks. BMC Gastroenterol. 2012;12:19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 107] [Cited by in RCA: 122] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 37. | Bi Y, Wu Z, Yi M, Han X, Ren J. Three-tube method and covered metallic stent for the treatment of anastomotic leakage after esophagectomy. BMC Gastroenterol. 2020;20:330. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 38. | Felipe N, King SA, Salerno A. 'Diagnosis of Boerhaave's Syndrome With Aid of Bedside Ultrasound. J Emerg Med. 2021;61:568-573. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 39. | Ioannidis O, Malliora A, Christidis P, Kotidis E, Pramateftakis MG, Mantzoros I, Ouzounidis N, Foutsitzis V, Angelopoulos S, Tsalis K. Conservative treatment of Boerhaave's syndrome in an octogenarian complicated with late distal esophageal stenosis and successfully treated by stent placement. Cir Cir. 2021;89:23-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 40. | Agrawal V, Aggarwal D. Undiagnosed spontaneous oesophageal rupture presenting as right hydropneumothorax. Indian J Thorac Cardiovasc Surg. 2019;35:111-114. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 41. | Jones WG 2nd, Ginsberg RJ. Esophageal perforation: a continuing challenge. Ann Thorac Surg. 1992;53:534-543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 254] [Cited by in RCA: 232] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 42. | Grillo HC, Wilkins EW Jr. Esophageal repair following late diagnosis of intrathoracic perforation. Ann Thorac Surg. 1975;20:387-399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 90] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 43. | Gouge TH, Depan HJ, Spencer FC. Experience with the Grillo pleural wrap procedure in 18 patients with perforation of the thoracic esophagus. Ann Surg. 1989;209:612-7; discussion 617. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 67] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 44. | Maki H, Inoue S, Goto M, Nishino T, Yoshida T, Takizawa H. Spontaneous esophageal perforation within a hiatal hernia: A case report. Int J Surg Case Rep. 2022;98:107484. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 45. | Park SB, Yum YJ, Cha JM. Cyanoacrylate injection treatment for postoperative leakage of Boerhaave's syndrome: A case report. Medicine (Baltimore). 2021;100:e28075. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 46. | Nachiappan M, Thota R, Gadiyaram S. Laparoscopic Repair of Spontaneous Esophageal Perforation After Multiple Endoscopic Failures. Cureus. 2022;14:e26784. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 47. | Aref H, Yunus T, Alhallaq O. Laparoscopic Management of Boerhaave's syndrome: a case report with an intraoperative video. BMC Surg. 2019;19:109. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 48. | Anand R, Puckett Y, Ronaghan CA. Above and Below the Diaphragm: A Previously Undescribed Case of Recurrent Boerhaave Syndrome Diagnosed With Computerized Tomography Esophagram. Cureus. 2022;14:e24015. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 49. | Rahman A, Alqaisi S, Downing C. Unusual Presentation of COVID Pneumonia as Esophageal Rupture Ended With Successful Management. Cureus. 2021;13:e17348. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 50. | Kochar T, Dhingra PS, Khaliq MF, Mcjunkin B. Eosinophilic esophagitis presenting with spontaneous esophageal rupture: a case report. J Med Case Rep 2019; 13: 275 . [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 51. | Bury J, Fratczak A, Nielson JA. Atypical Presentation of Boerhaave Syndrome With Hypoxia and Unresponsiveness. Cureus. 2022;14:e27848. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 52. | Shennib H, Baribault M, Heuser R. Bovine xenograft pericardial patch use for definitive single stage repair of a large esophageal defect: a case report. J Cardiothorac Surg. 2021;16:300. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 53. | Olivero R. Boerhaave syndrome: A rare postoperative complication. JAAPA. 2019;32:1-3. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 54. | He X, He Z, Li H. Boerhaave syndrome: Challenges in diagnosis and treatment of the early presentation and its complication. J Trauma Acute Care Surg. 2018;84:1030-1032. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 55. | Kita R, Kobayashi H, Nakao K, Iwaki K, Kondo M, Kaihara S. Three Cases of Boerhaave's Syndrome Treated via Laparoscopic Transhiatal Esophageal Repair. Case Rep Gastroenterol. 2022;16:406-412. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 56. | Sekiya S, Ebihara Y, Yamamura Y, Tanaka K, Nakanishi Y, Asano T, Noji T, Kurashima Y, Murakami S, Nakamura T, Tsuchikawa T, Okamura K, Shichinohe T, Hirano S. Two emergency cases of spontaneous esophageal perforation treated using a minimally invasive abdominal and left thoracic approach. Asian J Endosc Surg. 2020;13:406-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 57. | Tuñon C, De Lucas J, Cubilla J, Andrade R, Aguirre M, Zúñiga Cisneros J. Endoluminal vacuum therapy in the management of an esophago-pleural fistula as a complication of Boerhaave syndrome in a patient with eosinophilic esophagitis. BMC Gastroenterol. 2021;21:484. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 58. | Lee SY, Kim KW, Lee JI, Park DK, Park KY, Park CH, Son KH. Esophageal Endoscopic Vacuum Therapy with Enteral Feeding Using a Sengstaken-Blakemore Tube. Korean J Thorac Cardiovasc Surg. 2018;51:76-80. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 59. | Kim YE, Do YW, Cho JY, Kim ES, Lee DH. Successful Treatment Using Endoluminal Vacuum Therapy after Failure of Primary Closure in Boerhaave Syndrome. Korean J Gastroenterol. 2019;73:219-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |