Published online Jan 12, 2023. doi: 10.13105/wjma.v11.i1.18
Peer-review started: October 26, 2022
First decision: November 16, 2022
Revised: November 17, 2022
Accepted: December 27, 2022
Article in press: December 27, 2022
Published online: January 12, 2023
Processing time: 76 Days and 15.4 Hours
Kyoto global consensus reports that the current ICD-10 classification for gastritis is obsolete. The Kyoto classification of gastritis states that severe mucosal atrophy has a high risk of gastric cancer, while mild to moderate atrophy has a low risk. The updated Kimura-Takemoto classification of atrophic gastritis considers five histological types of multifocal corpus atrophic gastritis according to stages C2 to O3. This method of morphological diagnosis of atrophic gastritis increases sensitivity by 2.4 times for severe atrophy compared to the updated Sydney system. This advantage should be considered when stratifying the high risk of gastric cancer. The updated Kimura-Takemoto classification of atrophic gastritis should be used as a reference standard (gold standard) in studies of morpho-functional relationships to identify serological markers of atrophic gastritis with evidence-based effectiveness. The use of artificial intelligence in the serological screening of atrophic gastritis makes it possible to screen a large number of the population. During serological screening of atrophic gastritis and risk stratification of gastric cancer, it is advisable to use the Kyoto classification of gastritis with updated Kimura-Takemoto classification of atrophic gastritis.
Core Tip: Prevention of gastric cancer is an actual challenge of modern oncology. Its implementation is possible by means of serological screening of atrophic gastritis with accurate morphological diagnostics within the framework of the Kyoto classification of gastritis. If the Kyoto classification of gastritis is supplemented with the updated classification of Kimura-Takemoto atrophic gastritis, then it will be easier to estimate the risk of developing stomach cancer. The new system of gastric cancer risk stratification has the prospect of practical application in any population. For gastric cancer prevention at the level of large populations, we suggest using computer programs. The authors' computer program is given in this manuscript.
- Citation: Kotelevets SM, Chekh SA, Chukov SZ. Cancer risk stratification system and classification of gastritis: Perspectives. World J Meta-Anal 2023; 11(1): 18-28
- URL: https://www.wjgnet.com/2308-3840/full/v11/i1/18.htm
- DOI: https://dx.doi.org/10.13105/wjma.v11.i1.18
The statement that Helicobacter pylori (H. pylori) is the main cause of gastritis, atrophic gastritis, and gastric and duodenal ulcers belongs to the Kyoto global consensus. “Question of the hour” of gastroenterology is whether the current ICD-10 classification for gastritis is appropriate for use. Kyoto global consensus reports that the current ICD-10 classification for gastritis is obsolete[1]. At the present time, the complete classification of atrophic gastritis is absent. Lahner et al[2] mention autoimmune atrophic gastritis other than H. pylori-induced atrophic gastritis. There are very few modern publications on the topic of reflux-induced atrophic gastritis. Gad Elhak et al[3] revealed that after cholecystectomy, the incidence of reflux-induced atrophic gastritis increases, and the incidence of H. pylori-associated gastritis decreases. Nishidoi et al[4] found a relationship between resection of the stomach of male Wistar rats and the incidence of remnant stomach carcinoma. Moreover, the larger part of the stomach was removed, the more often carcinoma of the stomach remnant developed. The pathway of carcinogenesis in this case is considered duodeno-gastric reflux, especially bile acid reflux. Histologic examination of the gastric mucosa revealed atrophic gastritis. Bile acid reflux contributes to the development of atrophic gastritis and increases the incidence of intestinal metaplasia of the gastric mucosa[5].
Japanese authors Toyoshima et al[6] proposed an integral system for stratification of the risk of gastric cancer development, including the Kyoto classification of gastritis and neutrophil activity which was scored according to the updated Sydney System using biopsy samples obtained from the greater curvature of the corpus and the antrum. The Kyoto classification is based on the following scoring criteria: Atrophy, intestinal metaplasia, enlarged folds, nodularity, and diffuse redness ranging from 0 to 8. This is a visual endoscopic rating. The morphological assessment is restricted only by neutrophil activity scoring in a small number of biopsy specimens taken by means of the Sydney system. Histological evaluation of the mucosal atrophy and intestinal metaplasia is absent.
The integrated assessment of the risk of developing stomach cancer using the updated Kimura-Takemoto classification of atrophic gastritis has many possibilities because biopsy specimens are available in optimal numbers. There are five biopsy specimens for the gastric corpus and one for the antrum. Each biopsy specimen represents the stage of gastric mucosal atrophy from C1 to O2[7]. The Kyoto global consensus states that severe mucosal atrophy has a high risk of gastric cancer, while mild to moderate atrophy has a low risk[1]. The updated Sydney system takes into account two types of multifocal atrophic gastritis: Antral atrophic gastritis and corpus atrophic gastritis[8-13]. The updated Kimura-Takemoto classification of atrophic gastritis considers five histological types of multifocal corpus atrophic gastritis according to stages C2 to O3. This method of morphological diagnosis of atrophic gastritis increases sensitivity by 2.4 times for severe atrophy compared to the updated Sydney system. This advantage should be considered when stratifying the high risk of gastric cancer[7].
Endoscopic and morphological diagnosis of atrophic gastritis cannot be used for a large number of the population. Non-invasive serological screening for atrophic gastritis is essential at the first step in the prevention of gastric cancer. The search for effective serological markers of gastric mucosal atrophy is a very long process. Modern methods for the detection of atrophic gastritis and risk of gastric cancer using gastrin-17 (G-17), pepsinogen-I (PG-I), and the ratio of PG-I/PG-II are not perfect. Development of markers for atrophic gastritis and risk of gastric cancer continues[9,14-20]. Uniform criteria for assessing the concentration levels of the markers G17, PG1, PG2, and PG1/PG2 ratio are not defined when using by various authors. The location of gastric mucosal atrophy (antral atrophic gastritis, corpus atrophic gastritis, and multifocal atrophic gastritis) is not taken into account when using serological levels and other criteria to assess the severity of atrophy. The updated Sydney system was used in all morpho-functional studies as a reference method. At the same time, it does not have sufficient sensitivity to detect multifocal atrophic gastritis[7,21-28].
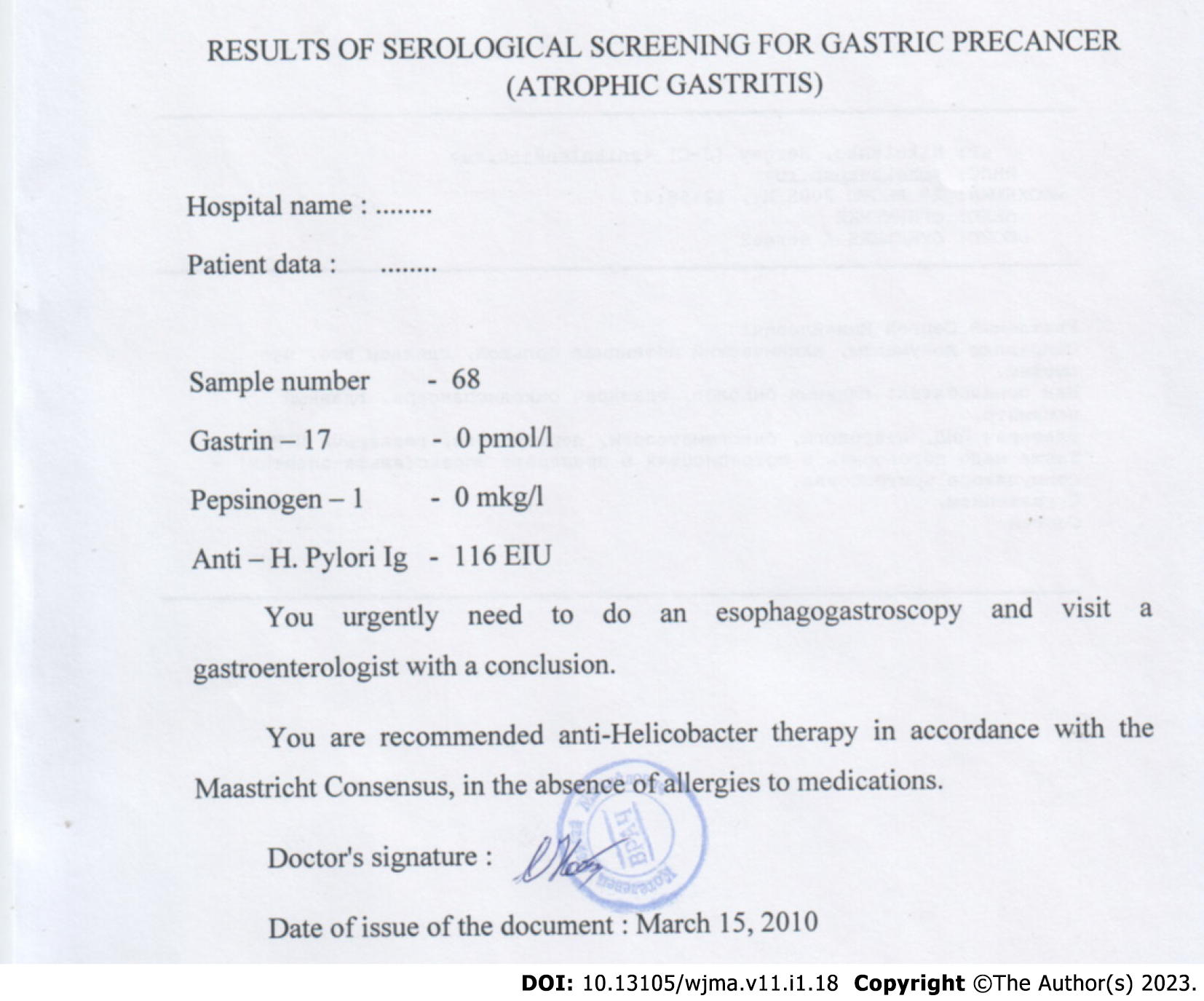
The use of machine processing can improve the efficiency of finding markers. Kotelevets CM and Chekh SA selected three markers of gastric mucosal atrophy from 47 factors associated with atrophy using computer data processing in 360 patients. In addition, serological criteria for mild, moderate, and severe atrophy were determined for the gastric antrum and corpus. These criteria were used for screening of about 5000 patients. Patient data, including personal data, were recorded in the registry after obtaining informed consent. Then, depersonalized referrals for serological testing were issued to the patient. Blood samples are stored at low temperature (-20 degrees Celsius). The analysis is performed on an enzyme immunoassay analyzer, which has 96 cells. Five of them are used for calibration samples, and the rest are used for patient samples. The optical density values are entered into the program, where the concentration values are calculated taking into account the calibration samples. Concentration values can be entered directly if the instrument used provides calibration (Figure 1). The time for obtaining optical densities on an enzyme immunoassay analyzer is 3.5 h. The researcher enters the year of birth and gender for each patient, and receives recommendations from the program (adjust them if necessary). The results are given to the patient in printed form, indicating the patient's full name, and affixing a signature and seal (Figures 2 and 3). This screening technique was presented in detail at the Third Congress of Therapists of the North Caucasian Federal District (Stavropol, May 19, 2016). This approach allowed to save the lives of patients with precancerous gastric disease[29,30]. Machine processing allows to reduce the fuzziness and randomness in data handling and thus can serve as the primary choice for obtaining results and big data analysis to make informed decisions. Artificial intelligence and Bidirectional Deep Neural Networks (BiDEN) are increasingly used for stratification of risk of gastric cancer development. Modern information technologies make it possible to obtain numerous multiomics data during screening of atrophic gastritis[29-33]. They are also used to evaluate data obtained from endoscopic and histological findings from initial endoscopy, barium double-contrast radiography of the upper gastrointestinal tract, and endoscopic three-dimensional (3D) reconstruction of the mucosal surface[34-36].
Due to the limitations of the endoscopic method of examining the stomach, a full-fledged endoscopic screening for atrophic gastritis and precancerous changes in the gastric mucosa in the population is not possible[37]. The Kyoto global consensus states that serological tests are useful for risk stratification of gastric cancer[1]. Therefore, it seems useful to include a section on serological screening for atrophic gastritis in the Kyoto classification of gastritis. For many years, the best markers of atrophic gastritis, precancerous changes, and the risk of gastric cancer have been PG-1, PG-2, G-17, the ratio of PG-1/PG-2, and antibodies to Helicobacter pylori (H. pylori). This has been confirmed by numerous multicenter studies and meta-analyses[37-46]. The current analysis is carried out, first of all, regarding the economics of serological screening for atrophic gastritis and precancerous changes in the gastric mucosa and determining the risk of gastric cancer. The main requirement for any screening is the availability of implementation in a large population. The cost should be low and the method should be non-invasive. These conditions are met by serological screening using markers PG-1, PG-2, G-17, the ratio of PG-1/PG-2, and anti-H. pylori IgG[47-49]. The effectiveness of serological screening of atrophic gastritis is significantly increased if serological markers are used that allow to differentiate between mild, moderate, and severe mucosal atrophy. The use of such markers by means of computer data processing made it possible to save more than four lives within seven years in a group of 2220 people[28,29].
Accurate diagnosis of chronic atrophic gastritis is of critical importance in monitoring stomach cancer, which remains the leading cause of death of cancer patients worldwide. According to the International Agency for Research on Cancer (IARC) GLOBOCAN project, worldwide, there were 1033701 new cases of gastric cancer (representing 5.7% of all cancer cases diagnosed)[50]. Gastric carcinogenesis is a complex multifactorial process. Currently, obvious evidence has been obtained about the main role of H. pylori in the development of gastric cancer[51]. H. pylori was declared a class 1 carcinogen by the World Health Organization committee of experts, even though the final mechanism of H. pylori-associated carcinogenesis has to be studied[52]. The main events in the pathogenesis of gastric cancer include the interaction of H. pylori virulent factors, environmental factors, and genetically determined sensitivity of the patient's organism. At least 70% of cases of non-cardiac gastric cancer are associated with the consequences of H. pylori infection[53]. It is also known that the risk of developing gastric cancer in H. pylori-infected subjects is significantly (from 6 to 25 times or more) higher than that in uninfected[54]. Gastric cancer is divided into two main types according to the Lauren classification – intestinal and diffuse. Intestinal gastric cancer, in accordance with the Correa paradigm[55], occurs through the sequential development of a cascade of pathological changes, starting with gastritis, followed by the appearance of atrophy, intestinal metaplasia, dysplasia, and finally, adenocarcinoma. Diffuse gastric cancer occurs de novo, without obvious previous histological changes in the gastric mucosa[56]. Both types of gastric cancer are characterized by the clear association with H. pylori infection[57]. H. pylori infection usually occurs in early childhood, and there is global interest to determine the age period from which it makes sense to carry out H. pylori eradication as a preventive measure for the development of gastric cancer – the so-called “point of no return” of precancerous changes in the gastric mucosa. An increased risk of developing gastric cancer in chronic H. pylori infection is associated with increased proliferation of gastric epithelial stem cells, and this increase occurs in two ways: As a response to damage to the gastric mucosa requiring intensive regeneration, and as a direct consequence of activation of intraepithelial signaling pathways associated with accelerated cell division. Studies of the surgical material of resected stomachs carried out in the first half of the last century showed that in cases of gastric cancer, there was always detected chronic gastritis of greater severity than in cases of peptic ulcer disease[58]. The researchers also noted that the foci of adenocarcinoma were more often found in areas of chronic inflammation, especially in atrophic gastritis. The advantage and necessity of histological examination are that it reveals causative relationships in the pathogenesis of H. pylori-associated gastric mucosal injury, establishing the presence of bacteria and the consequences of an inflammatory response to the infection as a cascade of changes, starting with acute inflammation, followed by transformation into a chronic course, with further disruption of regeneration processes in the form of atrophy, metaplasia, dysplasia, and finally, tumor growth. This defines the histological examination of gastric specimens as diagnostic “gold standard”[59-61]. At the same time, the problems of histological examination remain, such as sampling (the number and site of biopsies), the staining methods, and the pathologist's experience[61-64]. Although atrophy and intestinal metaplasia (IM) are independent stages of the Correa cascade, they are often detected simultaneously. Atrophy is defined by most pathologists as the loss of specialized glandular tissue (for example, the loss of the main gastric glands in the stomach corpus mucosa)[65]. Atrophy is usually detected in the form of a multifocal or diffuse process, and in the cases of atrophy of the oxyntic mucosa, one can reveal the appearance of mucous glands characteristic of the antral mucosa - the so-called pseudopiloric metaplasia (PM)[58]. IM is the replacement of the original gastric glands with intestinal crypts lined with absorbent and goblet cells, in combination with inflammatory infiltration of the mucosal lamina propria[65]. According to studies, PM correlates more closely with the presence of gastric cancer than IM, and may be a precursor of neoplastic changes[66]. One of the possible explanations for the relationship between the loss of parietal cells in atrophic gastritis and the development of metaplastic changes is the fact that the loss of parietal cells is associated with a decrease in the levels of signaling molecules modulating the growth and differentiation of stem cells of the gastric mucosa, which leads to increased proliferation and accumulation of undifferentiated progenitor cells[67]. Among such signaling molecules, there is a family of Sonic hedgehog (SHH) proteins, which are considered one of the key regulators of growth and differentiation of a wide range of tissues during embryogenesis. Immunohistochemical studies have shown that SHH is expressed by parietal cells[68], and SHH levels are reduced in patients with atrophic gastritis[69]. Experimental studies have shown that SHH-deficient mice developed IM in the gastric mucosa[70]. In acute pharmacological ablation of parietal cells, rapid and reversible development of PM was observed[71]. There are three categories of IM based on the structure of the crypts formed and the type of mucin. Type I (or complete type of) IM resembles a small intestinal mucosa in structure, while enterocytes, Paneth cells and goblet cells containing sialomucins are detected in direct crypts. Type III IM resembles a large intestinal mucosa: Columnar epithelial cells containing sulfomucins are found in the convoluted crypts. Type II is an incomplete small intestinal metaplasia without Paneth cells, or there can be the mixture of the first and third types. Type III IM is considered to be more precancerous. Thus, in a prospective study of 1281 patients, Filipe et al[72] found that with the development of type III IM, the risk of developing gastric cancer is increased by 3.8 times compared to type I IM. Despite the fact that atrophy and IM often accompany each other in patients with chronic gastritis, these conditions represent two different processes. The mechanisms of development of these two conditions continue to be studied. It is important that the pathologists separately evaluate the severity of gastric atrophy and IM, with the interpretation of the degree of their progression. The mechanism of IM development is caused in general by an impairment of differentiation of gastric mucosal proliferating stem cells. In particular, the differentiation of these cells is regulated by the homeobox genes, Hox and ParaHox clusters containing the Pdx1, Cdx1, and Cdx2 genes. The latter seem to be the most important in the expression of the small-intestinal phenotype, unlike Cdh1 genes, whose expression is realized in the direction of the large-intestinal phenotype[73]. The Cdx2 protein is not found in the normal gastric mucosa, but is expressed in the IM sites, as well as in the cases of Barrett's esophagus. The mechanism of induction of Cdx2 gene expression in chronic gastritis has to be elucidated. After the development of IM, according to the Correa cascade, dysplasia develops in the gastric mucosa, and the mechanism of this transition also remains unclear. The concept proposed by Correa in 1975[74] is generally accepted, according to which the metaplastic epithelium itself is a precursor of neoplasia. An alternative hypothesis suggests that IM is nothing more than an adaptive process in response to chronic damage. IM foci may be surrounded by areas of enhanced apoptosis, while apoptosis in the IM foci is reduced[75]. This is due to the expression of trefoil peptides that reduce apoptosis and stimulate differentiation in the direction of IM. The progression of gastric carcinogenesis is stimulated by the accumulation of genetic changes, which, in particular, manifest themselves at the chromosomal level. The molecular changes underlying these precursor processes require further study. The increased risk of developing gastric cancer may also be due to other factors that occur during the development of atrophic gastritis. These factors may include constantly enhanced cellular renewal in the atrophic mucosa, enhanced mutagenesis due to high levels of nitrites, and reduced levels of ascorbic acid in the gastric juice of these patients. Another proposed mechanism is based on the hypothesis that hydrochloric acid production may have a protective effect against gastric carcinogenesis. In the atrophic mucosa, a decrease in hydrochloric acid production leads to a decrease in purification from anaplastic cells in areas of micro-injury and the development of carcinoma in situ[76]. The unification of the assessment of inflammatory damage, atrophy, and IM in H. pylori-associated gastritis by means of a visual-analog scale was carried out in the Sydney system and its Houston modification[77]; however, it did not allow assessing the prognosis of damage and seemed to some researchers too weighty for use in routine diagnostics. In April 2005, in Parma, an international group of researchers, including gastroenterologists and pathologists [Operative Link for Gastritis Assessment (OLGA)], made a critical revision of the modified Sydney system[78]. OLGA experts concluded that since the risk of developing gastric cancer is directly related to the prevalence of gastritis and atrophy of the gastric mucosa, it is necessary to develop a system for assessing the stage of atrophic gastritis, which would ensure the determination of the prognosis and possibly, the tactics of the gastroenterologist. The proposed staging system combines indicators of atrophy in the stomach corpus and antrum, by using a visually analog scale of the modified Sydney system. Such a scheme will allow the clinician to get an idea of the prevalence of damage to the gastric mucosa and the degree of risk of developing gastric cancer in the specific patient. Also, very reliable associations can be obtained in the diagnosis of atrophic gastritis by endoscopy using the Kimura-Takemoto system, the results of which also correlate quite satisfactorily with histological data. The accuracy of endoscopic diagnosis of atrophic gastritis by means of the Kimura-Takemoto system was proven by many research groups, and we also established high levels of its sensitivity and specificity in our studies[7]. Finally, in 2013, the Japan Gastroenterological Endoscopy Society advocated the Kyoto classification, a new grading system for endoscopic gastritis. The classification is described above in this article. Ongoing studies indicate the usefulness of the Kyoto classification. For example, Toyoshima et al[79] accessed the association between the Kyoto classification and updated Sydney system score by comparison of endoscopic and pathologic (histologic) data. All endoscopic findings in the Kyoto classification for gastritis were associated with high scores of pathological inflammation (i.e., neutrophil activity and chronic inflammation) in both the corpus and antrum. Endoscopic atrophy and intestinal metaplasia were associated with high scores of pathological atrophy and intestinal metaplasia in both the corpus and antrum. Nodularity was associated with a low score of pathological intestinal metaplasia in the antrum. Thus, endoscopy by means of the Kyoto classification is very close to the real state of affairs, and yet, it is strongly recommended to be accompanied with histology of the gastric mucosa in patients with chronic atrophic gastritis, especially when the precancerous changes are revealed by endoscopy. It should be noted that the histological assessment of the gastric mucosa both by the modified Sydney system and by OLGA (Operational Link for Gastritis Assessment), or by Kimura-Takemoto classification is significantly limited by the number of biopsies and by the site of the biopsy. All three classifications use the same standard for taking a biopsy. Three biopsies (including incisura angularis) allow to characterize and evaluate the antral mucosa (the lesser functional part of the stomach), which reflects the morphological state of only the initial stage of the atrophic process according to Kimura-Takemoto – C1. Only two biopsies from the Sydney system remain to assess the stage of the atrophic process in the largest functional part of the stomach - the body, analogous to the respective grades of Kimura-Takemoto visual endoscopic classification (C2, C3, O1, O2, and O3). The updated Kimura-Takemoto classification of atrophic gastritis has much greater diagnostic capabilities and possibilities for stratifying the risk of gastric cancer. According to this technique, it is necessary to take six biopsies in accordance with C1 to O3 grades. Each biopsy allows stratifying the risk of gastric cancer from low to high at each stage: C1 – O3, according to the degree of histological atrophy from mild to severe[7].
The practical significance of the classification of stomach diseases is the prevention of stomach cancer, since this malignancy is the third most common cause of cancer death (782685 cases in 2018) among all oncological diseases[80]. The main advantage of the Kyoto classification is that it contains a detailed section on the etiology of gastritis. In the section of chronic atrophic gastritis, only mild to moderate atrophy of the stomach and severe atrophy of the stomach are distinguished[1]. This is not enough to effectively stratify the risk of stomach cancer. For effective practical use of the Kyoto classification of gastritis, it is advisably to supplement it with at least three more sections.
At the initial stage of gastric cancer risk stratification, serological screening for atrophic gastritis should be used. When using serological markers of atrophic gastritis, it is necessary to take into account the serological criteria for mild, moderate, and severe atrophy of the antrum mucosa and the stomach body[28].
At the second stage, it is necessary to carry out endoscopic screening among patients with atrophic gastritis who were identified at the stage of serological screening. Since the Kyoto classification of gastritis based on endoscopy and the pathological topographic distribution of neutrophil infiltration correlate with the risk of stomach cancer, endoscopic screening should be carried out taking into account the Kyoto endoscopic classification scale[6].
At the final diagnostic stage, it is necessary to carry out histological diagnosis of multifocal atrophic gastritis in accordance with the updated Kimura-Takemoto classification of atrophic gastritis[7].
Only the integral approach to creating an effective classification of gastric pathology based on morphology will allow to achieve the overall goal of preventing stomach cancer by means of more accurate identification and morphological monitoring of severe atrophic gastritis (stomach precancerous condition).
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Russia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): E
P-Reviewer: Muguruma N, Japan; Quach DT, Viet Nam S-Editor: Liu JH L-Editor: Wang TQ P-Editor: Liu JH
| 1. | Sugano K, Tack J, Kuipers EJ, Graham DY, El-Omar EM, Miura S, Haruma K, Asaka M, Uemura N, Malfertheiner P; faculty members of Kyoto Global Consensus Conference. Kyoto global consensus report on Helicobacter pylori gastritis. Gut. 2015;64:1353-1367. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1322] [Cited by in RCA: 1181] [Article Influence: 118.1] [Reference Citation Analysis (0)] |
| 2. | Lahner E, Conti L, Annibale B, Corleto VD. Current Perspectives in Atrophic Gastritis. Curr Gastroenterol Rep. 2020;22:38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 41] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 3. | Gad Elhak N, Abd Elwahab M, Nasif WA, Abo-Elenein A, Abdalla T, el-Shobary M, Haleem M, Yaseen A, el-Ghawalby N, Ezzat F. Prevalence of Helicobacter pylori, gastric myoelectrical activity, gastric mucosal changes and dyspeptic symptoms before and after laparoscopic cholecystectomy. Hepatogastroenterology. 2004;51:485-490. [PubMed] |
| 4. | Nishidoi H, Koga S, Kaibara N. Possible role of duodenogastric reflux on the development of remnant gastric carcinoma induced by N-methyl-N'-nitro-N-nitrosoguanidine in rats. J Natl Cancer Inst. 1984;72:1431-1435. [PubMed] |
| 5. | Li T, Guo H, Li H, Jiang Y, Zhuang K, Lei C, Wu J, Zhou H, Zhu R, Zhao X, Lu Y, Shi C, Nie Y, Wu K, Yuan Z, Fan DM, Shi Y. MicroRNA-92a-1-5p increases CDX2 by targeting FOXD1 in bile acids-induced gastric intestinal metaplasia. Gut. 2019;68:1751-1763. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 75] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 6. | Toyoshima O, Nishizawa T, Yoshida S, Sakaguchi Y, Nakai Y, Watanabe H, Suzuki H, Tanikawa C, Matsuda K, Koike K. Endoscopy-based Kyoto classification score of gastritis related to pathological topography of neutrophil activity. World J Gastroenterol. 2020;26:5146-5155. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 17] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (4)] |
| 7. | Kotelevets SM, Chekh SA, Chukov SZ. Updated Kimura-Takemoto classification of atrophic gastritis. World J Clin Cases. 2021;9:3014-3023. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 6] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (1)] |
| 8. | Correa P, Piazuelo MB. The gastric precancerous cascade. J Dig Dis. 2012;13:2-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 355] [Cited by in RCA: 520] [Article Influence: 40.0] [Reference Citation Analysis (0)] |
| 9. | Grad C, Pop A, Gaborean E, Grad S, Dumitrascu D. Value of GastroPanel in the diagnosis of atrophic gastritis. Exp Ther Med. 2021;22:1347. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 10. | Piazuelo MB, Bravo LE, Mera RM, Camargo MC, Bravo JC, Delgado AG, Washington MK, Rosero A, Garcia LS, Realpe JL, Cifuentes SP, Morgan DR, Peek RM Jr, Correa P, Wilson KT. The Colombian Chemoprevention Trial: 20-Year Follow-Up of a Cohort of Patients With Gastric Precancerous Lesions. Gastroenterology. 2021;160:1106-1117.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 87] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 11. | Esposito G, Dilaghi E, Cazzato M, Pilozzi E, Conti L, Carabotti M, Di Giulio E, Annibale B, Lahner E. Endoscopic surveillance at 3 years after diagnosis, according to European guidelines, seems safe in patients with atrophic gastritis in a low-risk region. Dig Liver Dis. 2021;53:467-473. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 12. | Garai J, Li L, Zabaleta J. Biomarkers of Gastric Premalignant Lesions. 2019 Dec 13. In: Advancing the Science of Cancer in Latinos [Internet]. Cham (CH): Springer; 2020–. [PubMed] |
| 13. | Bravo LE, Bravo JC, Realpe JL, Zarama G, Piazuelo MB, Correa P. [Source of variation in the diagnosis of Helicobacter pylori-associated multifocal atrophic gastritis]. Colomb Med (Cali). 2008;39:58-65. [PubMed] |
| 14. | Cai Q, Zhu C, Yuan Y, Feng Q, Feng Y, Hao Y, Li J, Zhang K, Ye G, Ye L, Lv N, Zhang S, Liu C, Li M, Liu Q, Li R, Pan J, Yang X, Zhu X, Li Y, Lao B, Ling A, Chen H, Li X, Xu P, Zhou J, Liu B, Du Z, Du Y, Li Z; Gastrointestinal Early Cancer Prevention & Treatment Alliance of China (GECA). Development and validation of a prediction rule for estimating gastric cancer risk in the Chinese high-risk population: a nationwide multicentre study. Gut. 2019;68:1576-1587. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 83] [Cited by in RCA: 149] [Article Influence: 24.8] [Reference Citation Analysis (0)] |
| 15. | Shen H, Xiong K, Wu X, Cheng S, Lou Q, Jin H, Zhang X. The Diagnostic Value of Serum Gastrin-17 and Pepsinogen for Gastric Cancer Screening in Eastern China. Gastroenterol Res Pract. 2021;2021:6894248. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 16. | Sadighbayan D, Tohidkia MR, Mehdipour T, Hasanzadeh M, Yari Khosroushahi A. Bio-assay of the non-amidated progastrin-derived peptide (G17-Gly) using the tailor-made recombinant antibody fragment and phage display method: a biomedical analysis. Anal Methods. 2020;12:2735-2746. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 17. | Zheng S, Hu R, Yu X, Chen L, BinrongWang, Qin Y, Zhou X, Wang Y, Huang B, Fang H, Liu P. Development of a time-resolved fluorescence immunoassay based on immunomagnetic beads for gastrin-17. J Immunol Methods. 2021;499:113179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 18. | Zhao WX, Liu ZF, Li XL, Li Z. Correlations of serum homocysteine, VEGF and gastrin 17 with gastric cancer and precancerous lesions. Eur Rev Med Pharmacol Sci. 2019;23:4192-4198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 19. | Wang Y, Zhu Z, Liu Z, Zhao Z, Xue X, Li X, Li P, Rong G, Ma Y. Diagnostic value of serum pepsinogen I, pepsinogen II, and gastrin-17 levels for population-based screening for early-stage gastric cancer. J Int Med Res. 2020;48:300060520914826. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 24] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 20. | Lin Z, Bian H, Chen C, Chen W, Li Q. Application of serum pepsinogen and carbohydrate antigen 72-4 (CA72-4) combined with gastrin-17 (G-17) detection in the screening, diagnosis, and evaluation of early gastric cancer. J Gastrointest Oncol. 2021;12:1042-1048. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 25] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 21. | Wang R, Chen XZ. Prevalence of atrophic gastritis in southwest China and predictive strength of serum gastrin-17: A cross-sectional study (SIGES). Sci Rep. 2020;10:4523. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 22. | Yu G, Wang GX, Wang HG, Mo FF, Tang BB. The value of detecting pepsinogen and gastrin-17 levels in serum for pre-cancerous lesion screening in gastric cancer. Neoplasma. 2019;66:637-640. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 23. | Huang RJ, Park S, Shen J, Longacre T, Ji H, Hwang JH. Pepsinogens and Gastrin Demonstrate Low Discrimination for Gastric Precancerous Lesions in a Multi-Ethnic United States Cohort. Clin Gastroenterol Hepatol. 2022;20:950-952.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 20] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 24. | Koivurova OP, Koskela R, Blomster T, Ala-Rämi A, Lumme H, Kettunen O, Hukkanen J, Karttunen TJ, Mäkinen M, Ronkainen J, Syrjänen K. Serological Biomarker Panel in Diagnosis of Atrophic Gastritis and Helicobacter pylori Infection in Gastroscopy Referral Patients: Clinical Validation of the New-Generation GastroPanel® Test. Anticancer Res. 2021;41:5527-5537. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 25. | Wang XT, Ji ZZ, Han F, Lyu B. [A comparative study of new gastric cancer screening scoring system and new ABC method for screening gastric cancer and precancerous lesions]. Zhonghua Nei Ke Za Zhi. 2021;60:227-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 26. | Bakulina N, Tikhonov S, Malkov V, Vorobyev S, Belyakov I, Peshkova N, Belko E, Syrjänen K. Non-invasive Screening of Autoimmune Atrophic Gastritis in Asymptomatic Subjects by Serological Biomarker Test (GastroPanel®). Anticancer Res. 2022;42:1517-1526. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 27. | Leja M, Kupcinskas L, Funka K, Sudraba A, Jonaitis L, Ivanauskas A, Janciauskas D, Kiudelis G, Chiu HM, Lin JT. The validity of a biomarker method for indirect detection of gastric mucosal atrophy versus standard histopathology. Dig Dis Sci. 2009;54:2377-2384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 47] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 28. | Kotelevets SM, Chekh SA. Serological Criteria for Mild, Moderate and Severe Atrophy in Atrophic Gastritis. Biol Med J. 2015;7:235. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 29. | Kotelevets SM, Chekh SA. Screening, Monitoring, and Treatment of Precancerous Atrophic Gastritis in the Prospective Study for Seven Years. Asian Pac J Cancer Prev. 2020;21:331-336. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 30. | Patel SK, George B, Rai V. Artificial Intelligence to Decode Cancer Mechanism: Beyond Patient Stratification for Precision Oncology. Front Pharmacol. 2020;11:1177. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 36] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 31. | Xu J, Yao Y, Xu B, Li Y, Su Z. Unsupervised learning of cross-modal mappings in multi-omics data for survival stratification of gastric cancer. Future Oncol. 2022;18:215-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 32. | Nakahira H, Ishihara R, Aoyama K, Kono M, Fukuda H, Shimamoto Y, Nakagawa K, Ohmori M, Iwatsubo T, Iwagami H, Matsuno K, Inoue S, Matsuura N, Shichijo S, Maekawa A, Kanesaka T, Yamamoto S, Takeuchi Y, Higashino K, Uedo N, Matsunaga T, Tada T. Stratification of gastric cancer risk using a deep neural network. JGH Open. 2020;4:466-471. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 33. | Lu J, Xue Z, Xu BB, Wu D, Zheng HL, Xie JW, Wang JB, Lin JX, Chen QY, Li P, Huang CM, Zheng CH. Application of an artificial neural network for predicting the potential chemotherapy benefit of patients with gastric cancer after radical surgery. Surgery. 2022;171:955-965. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 34. | Ali S, Bailey A, Ash S, Haghighat M; TGU Investigators, Leedham SJ, Lu X, East JE, Rittscher J, Braden B. A Pilot Study on Automatic Three-Dimensional Quantification of Barrett's Esophagus for Risk Stratification and Therapy Monitoring. Gastroenterology. 2021;161:865-878.e8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 21] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 35. | Arai J, Aoki T, Sato M, Niikura R, Suzuki N, Ishibashi R, Tsuji Y, Yamada A, Hirata Y, Ushiku T, Hayakawa Y, Fujishiro M. Machine learning-based personalized prediction of gastric cancer incidence using the endoscopic and histologic findings at the initial endoscopy. Gastrointest Endosc. 2022;95:864-872. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 34] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 36. | Togo R, Yamamichi N, Mabe K, Takahashi Y, Takeuchi C, Kato M, Sakamoto N, Ishihara K, Ogawa T, Haseyama M. Detection of gastritis by a deep convolutional neural network from double-contrast upper gastrointestinal barium X-ray radiography. J Gastroenterol. 2019;54:321-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 37. | Zagari RM, Rabitti S, Greenwood DC, Eusebi LH, Vestito A, Bazzoli F. Systematic review with meta-analysis: diagnostic performance of the combination of pepsinogen, gastrin-17 and anti-Helicobacter pylori antibodies serum assays for the diagnosis of atrophic gastritis. Aliment Pharmacol Ther. 2017;46:657-667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 133] [Article Influence: 16.6] [Reference Citation Analysis (0)] |
| 38. | Botezatu A, Bodrug N. Chronic atrophic gastritis: an update on diagnosis. Med Pharm Rep. 2021;94:7-14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 39. | Syrjänen K, Eskelinen M, Peetsalu A, Sillakivi T, Sipponen P, Härkönen M, Paloheimo L, Mäki M, Tiusanen T, Suovaniemi O, DiMARIO F, Fan ZP. GastroPanel® Biomarker Assay: The Most Comprehensive Test for Helicobacter pylori Infection and Its Clinical Sequelae. A Critical Review. Anticancer Res. 2019;39:1091-1104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 40. | Syrjänen K. Accuracy of Serum Biomarker Panel (GastroPanel®) in the Diagnosis of Atrophic Gastritis of the Corpus. Systematic Review and Meta-analysis. Anticancer Res. 2022;42:1679-1696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 41. | Kornoukhova LA, Emanuel VL, Denisov NL, Nikonov EL. Helicobacter pylori infection: place of serological and cultural diagnostics in clinical guidelines. Klin Lab Diagn. 2021;66:496-501. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 42. | Kishino T, Oyama T, Tomori A, Takahashi A, Shinohara T. Usefulness and Limitations of a Serum Screening System to Predict the Risk of Gastric Cancer. Intern Med. 2020;59:1473-1480. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 43. | Kim BC, Song MA, Kwon SH. Endoscopic Characteristics of Rugal Hyperplasia and Related Acid Condition in Helicobacter pylori-Infected Stomach. Clin Endosc. 2021;54:73-84. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 44. | Inoue M, Sawada N, Goto A, Shimazu T, Yamaji T, Iwasaki M, Tsugane S; JPHC Study Group. High-Negative Anti-Helicobacter pylori IgG Antibody Titers and Long-Term Risk of Gastric Cancer: Results from a Large-Scale Population-Based Cohort Study in Japan. Cancer Epidemiol Biomarkers Prev. 2020;29:420-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 45. | Okuno H, Suzuki S, Watanabe H, Kusano C, Ikehara H, Moriyama M, Gotoda T. Histological Features of Gastric Mucosa Serologically Diagnosed as Gastric Atrophy without Helicobacter pylori Infection. Digestion. 2020;101:217-226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 46. | den Hollander WJ, Holster IL, den Hoed CM, Capelle LG, Tang TJ, Anten MP, Prytz-Berset I, Witteman EM, Ter Borg F, Hartog GD, Bruno MJ, Peppelenbosch MP, Lesterhuis W, Doukas M, Kuipers EJ, Spaander MCW. Surveillance of premalignant gastric lesions: a multicentre prospective cohort study from low incidence regions. Gut. 2019;68:585-593. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 106] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 47. | Areia M, Carvalho R, Cadime AT, Rocha Gonçalves F, Dinis-Ribeiro M. Screening for gastric cancer and surveillance of premalignant lesions: a systematic review of cost-effectiveness studies. Helicobacter. 2013;18:325-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 96] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 48. | Belkovets AV, Kurilovich SA, Reshetnikov O, Ragino YI, Scherbakova LV. [Noninvasive diagnostics of the phenotype of gastritis: Analisis of the first thousand of cases]. Eksp Klin Gastroenterol. 2015;26-30. [PubMed] |
| 49. | Tucci A, Bisceglia M, Rugge M, Tucci P, Marchegiani A, Papadopoli G, Spada A, Villani A, Pennelli G, Fusaroli P, Caravelli G, Catalano T, Cennamo V, Cianci M, De Fanis C, Fabbri C, Feliciangeli G, Gizzi G, Spadaccini A, Caletti G. Clinical usefulness of gastric-juice analysis in 2007: the stone that the builders rejected has become the cornerstone. Gastrointest Endosc. 2007;66:881-890. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 50. | Thrift AP, El-Serag HB. Burden of Gastric Cancer. Clin Gastroenterol Hepatol. 2020;18:534-542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 432] [Cited by in RCA: 980] [Article Influence: 196.0] [Reference Citation Analysis (1)] |
| 51. | Wang C, Yuan Y, Hunt RH. The association between Helicobacter pylori infection and early gastric cancer: a meta-analysis. Am J Gastroenterol. 2007;102:1789-1798. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 101] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 52. | IARC Working Group on the Evaluation of Carcinogenic Risks to Humans: Schistosomes, liver flukes and Helicobacter pylori, Lyon, June 7–14, 1994. IARC Monogr Eval Carcinog Risks Hum 1994; 61: 1–241: 1–241 . [RCA] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 72] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 53. | Ekström AM, Held M, Hansson LE, Engstrand L, Nyrén O. Helicobacter pylori in gastric cancer established by CagA immunoblot as a marker of past infection. Gastroenterology. 2001;121:784-791. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 278] [Cited by in RCA: 287] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 54. | Leodolter A, Naumann M, Malfertheiner P. Prevention of gastric cancer by Helicobacter pylori eradication. Dig Dis. 2004;22:313-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 55. | Correa P. Human gastric carcinogenesis: a multistep and multifactorial process--First American Cancer Society Award Lecture on Cancer Epidemiology and Prevention. Cancer Res. 1992;52:6735-6740. [PubMed] |
| 56. | Sipponen P, Marshall BJ. Gastritis and gastric cancer. Western countries. Gastroenterol Clin North Am. 2000;29:579-592, v. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 71] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 57. | Huang JQ, Sridhar S, Chen Y, Hunt RH. Meta-analysis of the relationship between Helicobacter pylori seropositivity and gastric cancer. Gastroenterology. 1998;114:1169-1179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 625] [Cited by in RCA: 618] [Article Influence: 22.9] [Reference Citation Analysis (0)] |
| 58. | Fox JG, Wang TC. Inflammation, atrophy, and gastric cancer. J Clin Invest. 2007;117:60-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 587] [Cited by in RCA: 612] [Article Influence: 34.0] [Reference Citation Analysis (0)] |
| 59. | Kapetanakis N, Kountouras J, Zavos C, Polyzos SA, Kouklakis G, Venizelos I, Nikolaidou C, Vardaka E, Paikos D, Katsinelos P, Romiopoulos I. Helicobacter pylori infection and colorectal carcinoma: pathologic aspects. J Gastrointest Oncol. 2012;3:377-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 60. | Tonkic A, Vukovic J, Vrebalov Cindro P, Pesutic Pisac V, Tonkic M. Diagnosis of Helicobacter pylori infection : A short review. Wien Klin Wochenschr. 2018;130:530-534. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 61. | Best LM, Takwoingi Y, Siddique S, Selladurai A, Gandhi A, Low B, Yaghoobi M, Gurusamy KS. Non-invasive diagnostic tests for Helicobacter pylori infection. Cochrane Database Syst Rev. 2018;3:CD012080. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 98] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 62. | Rupp S, Papaefthymiou A, Chatzimichael E, Polyzos SA, Spreitzer S, Doulberis M, Kuntzen T, Kountouras J. Diagnostic approach to Helicobacter pylori-related gastric oncogenesis. Ann Gastroenterol. 2022;35:333-344. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 63. | Lopes AI, Vale FF, Oleastro M. Helicobacter pylori infection - recent developments in diagnosis. World J Gastroenterol. 2014;20:9299-9313. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 58] [Reference Citation Analysis (0)] |
| 64. | Lee JY, Kim N. Diagnosis of Helicobacter pylori by invasive test: histology. Ann Transl Med. 2015;3:10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 57] [Reference Citation Analysis (0)] |
| 65. | Correa P. Chronic atrophic gastritis as a precursor of cancer. In Precancerous lesions of the gastrointestinal tract. P. Sherlock, B. Morson, L. Barbara, and U. Veronesi, editors. Raven Press. New York, New York, USA. 1983; 145–153. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 66. | Halldórsdóttir AM, Sigurdardóttrir M, Jónasson JG, Oddsdóttir M, Magnússon J, Lee JR, Goldenring JR. Spasmolytic polypeptide-expressing metaplasia (SPEM) associated with gastric cancer in Iceland. Dig Dis Sci. 2003;48:431-441. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 88] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 67. | Li Q, Karam SM, Gordon JI. Diphtheria toxin-mediated ablation of parietal cells in the stomach of transgenic mice. J Biol Chem. 1996;271:3671-3676. [PubMed] |
| 68. | van den Brink GR, Hardwick JC, Tytgat GN, Brink MA, Ten Kate FJ, Van Deventer SJ, Peppelenbosch MP. Sonic hedgehog regulates gastric gland morphogenesis in man and mouse. Gastroenterology. 2001;121:317-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 187] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 69. | Shiotani A, Iishi H, Uedo N, Ishiguro S, Tatsuta M, Nakae Y, Kumamoto M, Merchant JL. Evidence that loss of sonic hedgehog is an indicator of Helicobater pylori-induced atrophic gastritis progressing to gastric cancer. Am J Gastroenterol. 2005;100:581-587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 78] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 70. | Ramalho-Santos M, Melton DA, McMahon AP. Hedgehog signals regulate multiple aspects of gastrointestinal development. Development. 2000;127:2763-2772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 603] [Cited by in RCA: 552] [Article Influence: 22.1] [Reference Citation Analysis (0)] |
| 71. | Nomura S, Yamaguchi H, Ogawa M, Wang TC, Lee JR, Goldenring JR. Alterations in gastric mucosal lineages induced by acute oxyntic atrophy in wild-type and gastrin-deficient mice. Am J Physiol Gastrointest Liver Physiol. 2005;288:G362-G375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 115] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 72. | Filipe MI, Muñoz N, Matko I, Kato I, Pompe-Kirn V, Jutersek A, Teuchmann S, Benz M, Prijon T. Intestinal metaplasia types and the risk of gastric cancer: a cohort study in Slovenia. Int J Cancer. 1994;57:324-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 298] [Cited by in RCA: 294] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 73. | Silberg DG, Swain GP, Suh ER, Traber PG. Cdx1 and cdx2 expression during intestinal development. Gastroenterology. 2000;119:961-971. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 436] [Cited by in RCA: 463] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 74. | Correa P, Haenszel W, Cuello C, Tannenbaum S, Archer M. A model for gastric cancer epidemiology. Lancet. 1975;2:58-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 725] [Cited by in RCA: 733] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 75. | van Grieken NC, Meijer GA, zur Hausen A, Meuwissen SG, Baak JP, Kuipers EJ. Increased apoptosis in gastric mucosa adjacent to intestinal metaplasia. J Clin Pathol. 2003;56:358-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 76. | Kuipers EJ, Siersema PD. The aetiology and clinical relevance of gastric intestinal metaplasia. Dig Liver Dis. 2004;36:501-504. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 77. | Price AB, Misiewicz JJ. Sydney classification for gastritis. Lancet. 1991;337:174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 78. | Rugge M, Genta RM. Staging and grading of chronic gastritis. Hum Pathol. 2005;36:228-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 188] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 79. | Toyoshima O, Nishizawa T, Yoshida S, Matsuno T, Odawara N, Toyoshima A, Sakitani K, Watanabe H, Fujishiro M, Suzuki H. Consistency between the endoscopic Kyoto classification and pathological updated Sydney system for gastritis: A cross-sectional study. J Gastroenterol Hepatol. 2022;37:291-300. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 16] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 80. | Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53206] [Cited by in RCA: 55806] [Article Influence: 7972.3] [Reference Citation Analysis (132)] |