Published online Jun 28, 2022. doi: 10.13105/wjma.v10.i3.74
Peer-review started: January 12, 2022
First decision: February 21, 2022
Revised: April 19, 2022
Accepted: May 22, 2022
Article in press: May 22, 2022
Published online: June 28, 2022
Processing time: 174 Days and 8.3 Hours
The coronavirus pandemic was thrust upon all nations in the year 2020 and required swift public health responses. Resource-poor health care facilities, such as those in the Caribbean, were poorly prepared but had to respond to the threat. In this experience report we examined the response by the surgical specialty to evaluate the lessons learned and to identify positive changes that may continue post-pandemic.
Core Tip: Although resource-poor nations were not prepared to deal with the pandemic, they still had to respond to the global threat. This paper discusses the surgical specialty’s response in order to identify positive changes that may continue post-pandemic.
- Citation: Cawich SO, Narayansingh G, Ramdass MJ, Mencia M, Thomas DA, Barrow S, Naraynsingh V. Responses to disrupted operative care during the coronavirus pandemic at a Caribbean hospital. World J Meta-Anal 2022; 10(3): 74-80
- URL: https://www.wjgnet.com/2308-3840/full/v10/i3/74.htm
- DOI: https://dx.doi.org/10.13105/wjma.v10.i3.74
The coronavirus (COVID) pandemic was thrust upon all nations across the globe in the year 2020. Trinidad & Tobago, a small resource-poor Caribbean nation, recorded its first case in March, 2020. The health care system had to rapidly respond to the pandemic. In this experience report we examine the response by the surgical specialty to evaluate the lessons learned and to identify positive changes that may continue post-pandemic.
The Anglophone Caribbean is comprised of 17 independent countries, each with their own governments, budgets and health care delivery systems. Although the cumulative population is 7.5 million persons, the region is comprised mostly of small island states, with only four countries having populations over 200000 persons[1].
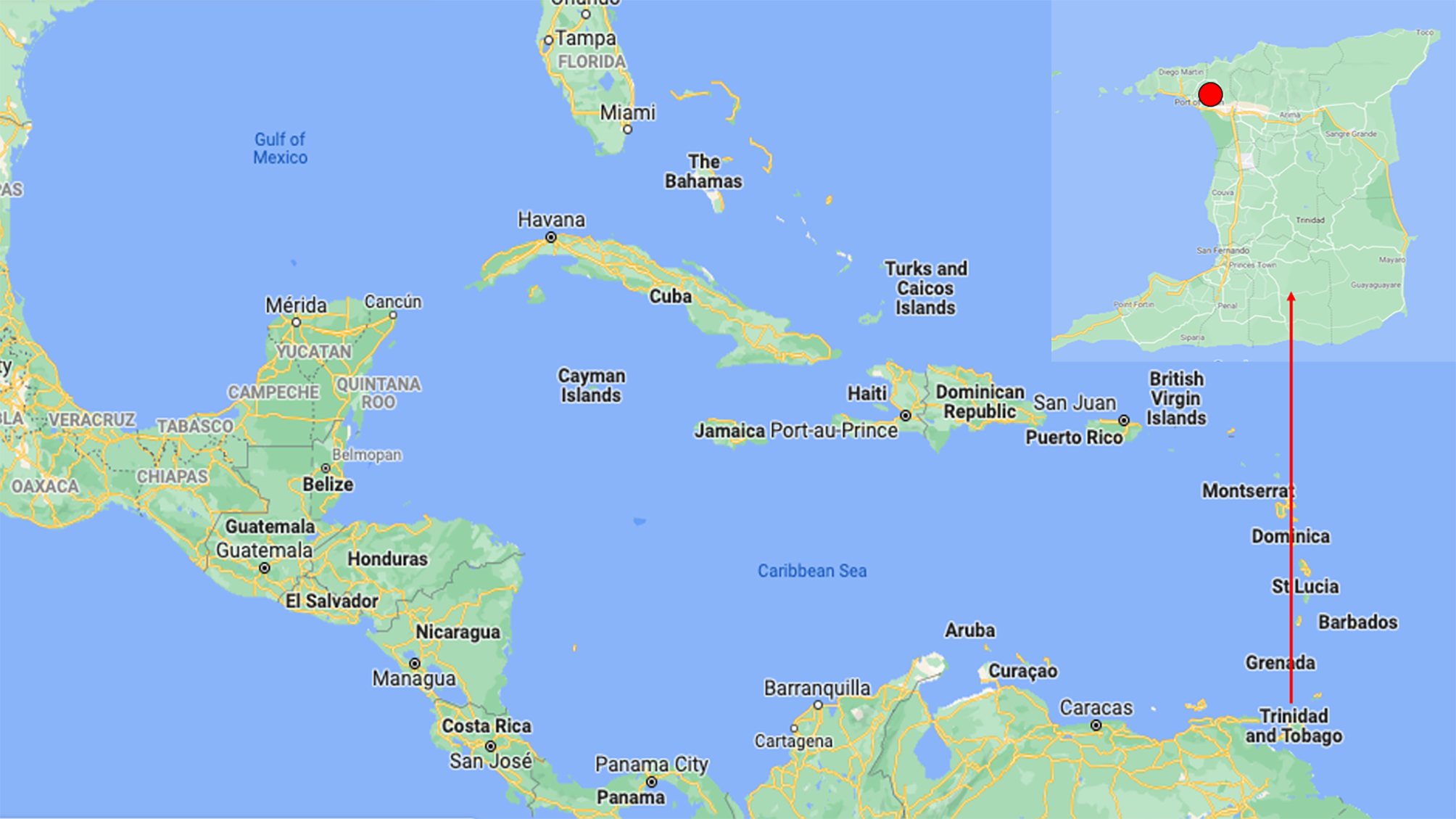
Trinidad & Tobago is a small island nation in the Eastern Caribbean, covering 1980 square miles (Figure 1). There was a population of 1.3 million persons at the last national census[2]. Citizens of this nation have access to government-sponsored health care through public hospitals managed by the health mininstry[2].
The General Hospital in Port of Spain is a 400-bed tertiary referral public hospital that serves a densely populated area, with a catchment population approximately 650000 persons[3]. The hospital offers virtually all areas of subspecialty care to the population in the North-Western part of the island (Figure 1). From a surgical point of view, due to the dense population and the high prevalence of interpersonal violence, the hospital is well known as a trauma center throughout the Caribbean[3]. The hospital is also affiliated with the local University[3], provides tertiary level oncology care to the catchment population[4] and serves as a quaternary referral center for vascular, hepatobiliary and laparoscopic surgery for the nation.
Similar to other facilities across the globe, the Port of Spain General Hospital was significantly affected by the COVID pandemic[5,6]. After the first reported case in Trinidad & Tobago, there was a swift initial response to close international sea and air borders to all incoming and outgoing passengers on March 22, 2021[7]. The borders remained closed to all forms of transit until July 17, 2021. During this time, all persons had to apply to the Government for exemptions to allow emergency travel.
The Government of Trinidad & Tobago also declared a State of Emergency in an attempt to limit travel and social activity within the nation[7]. A State of Emergency is triggered when there is a existing or potential threat to the nation and/or its population[3]. While in effect, only persons deemed “essential to national function” were allowed to travel in public spaces[3].
Before this incident, a State of Emergency was declared on six prior occasions[8]. All six prior States of Emergencies were declared in response to inter-personal violence[3]. The 2021 declaration was the only one due to a natural event. As a part of this response, the government organized intensified law enforcement operations with three specific aims: curtail inter-island transit, ensure that persons who required emergency travel maintained social distancing and mask wearing and to limit social gatherings. To facilitate this, a nationwide curfew was imposed and non-compliant citizens were subject to arrest for up to 24-h.
During this State of Emergency, health workers were permitted to travel in order to ensure continued healthcare via the Government-funded public hospitals. The Government attempted to create a parallel health care system that attended to the needs of COVID positive patients only, preserving the regular health care system for unaffected patients. However, the underfunded and resource-poor healthcare systems were unprepared[9].
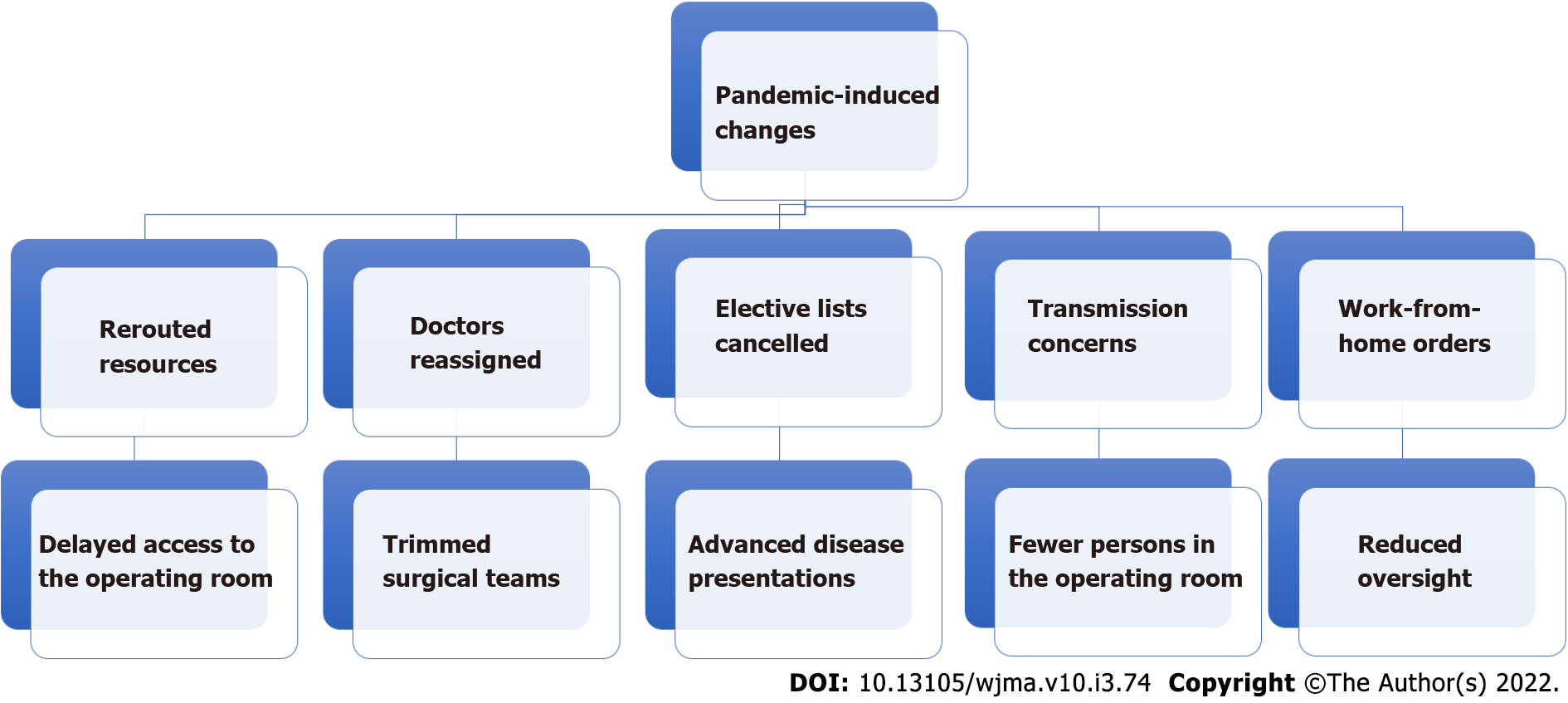
In the grand scheme of the healthcare response, surgery became an irrelevant specialty[10]. The overwhelming majority of COVID related complications affected the cardiovascular and respiratory systems. There were few, if any, surgical complications recognized. Therefore, it was understandable that surgical services in Trinidad & Tobago were curtailed. This saw surgical house officers re-allocated to COVID teams, procurement practices changed, clinics postponed, operating room lists cancelled and face-to-face multidisciplinary team meetings discontinued. These changes, while totally understandable, crippled the delivery of surgical care (Figure 2).
In the meantime, patients with surgical diseases continued to present to the hospitals for care. Surgical care was delayed in many cases, due to both patient reluctance to present to hospital[11] and prolonged transit through the healthcare delivery systems. Therefore, patients who presented for surgical care were now in advanced disease states. Surgical leaders recognized that a potential crisis was developing and responded in several ways.
The Port of Spain General Hospital is a post-graduate training facility associated with a regional medical university. Surgical firms were comprised of a consultant surgeon, at least one registrar (PGY4/5) and junior residents commencing post-graduate training (PGY1/2).
Elective outpatient care required that patients attended the surgical clinic for follow-up visits. However, this could not continue as it would mean clustering of patients without effective methods to maintain social distancing. To overcome this, the surgical teams accessed a list of patients requiring elective outpatient care and contacted them by telephone for triage. Patients whose conditions allowed had their appointments postponed. For patients who required urgent consultations, the surgical teams used FaceTime (Apple Inc., Cupertino, California, United States) video conferencing applications on mobile phones to view wounds and/or carry out face-to-face consultations.
This facility practiced a multiple disciplinary approach to health care since the year 2013[12]. Traditionally, this was achieved by healthcare workers meeting face-to-face in a dedicated meeting room to discuss cases. In this setting, there was initially poor buy-in to the MDT concept. As a result, there was little dedicated funding for MDT processes. This was overcome by members utilizing free software, such as coordination via WhatsApp® (WhatsApp Inc., California, United States) and Google mail® (Google Inc., Mountain View, CA 94043, United States) groups. Radiology images were accessed using free OsiriX® DICOM software (Pixmeo, Geneva, Switzerland) and shared via Dropbox® (Dropbox Inc, San Francisco, California). Initially, this was laborious, but when the pandemic changes were thrust upon us, we were already in a position to switch effectively to electronic meetings via Zoom (Zoom Video Communications, San Jose, California) – also freely available on the internet.
Interestingly, upon review of our records, we found that the attendance increased once there was no longer a need for face-to-face meetings. Also, the images were viewed directly on individual devices, allowing better visualization and participation. In the first 90 days, virtual meetings lasted for 20 min (mean) and discussed an average of 2.45 cases. After one year of virtual meetings, the process became streamlined and the workload increased, culminating in a mean meeting duration of 75 minutes and mean of 6.5 case discussions per meeting. We also recorded the attending surgeons’ clinical plan pre- and post-meetings and noted that 52% of therapeutic plans had changed post-discussion.
Patients continued to present to hospitals with surgical emergencies. Priority was given to triaging patients, channeling COVID positive patients to a parallel COVID health care facility. This ensured other patients and staff were not exposed to the virus. Since our facility had no access to any form of rapid COVID status testing, patients with suspected infections were isolated in tents until they could be formally tested, often at the expense of disease progression and poor outcomes.
Government-mandated instructions to work-from-home where possible also affected rostering of surgical teams. This affected the number of surgical nurses, doctors and support staff[9]. Redistribution of personnel to COVID units[9] further reduced the cadre of staff available for emergency surgical care. In addition, the surgical teams were ordered to further subdivide to mitigate risk of entire teams being exposed at once and to reduce utilization of scarce personal protective equipment stocks[10].
As it relates to the operating room, the usual oversight was not feasible as attending surgeons could not be present for all cases fearing the service collapsing if all members of the team became exposed/ infected[13]. We turned to technology using the distance mentoring technique, described in detail in previous publications[10,14].
In summary, a PGY4/5 resident performing an operation used two smartphones to video conference with the consultant surgeon. One was fixated to the theater lights viewing the surgical field and the second was on the anesthetic machine to view the PGY4/5 residents while operating[10,14]. Occasionally, operating room staff manipulated the smart phones for closer inspection. The consultant surgeon used separate devices to virtually guide residents through surgery. We reported this experience with trauma patients[10] and since then have amassed more experience with laparoscopy[14,15], hepatobiliary surgery[14,16] and emergency operations at this facility. We were able to use this method with 96% success[10] with good outcomes. This technique may be considered in the post-pandemic operating room to maintain safety while minimizing virus transmission, once a reliable high-bandwidth network connection is present. The main concerns with this method were the inability for the attending surgeon to take over in case of a complication and the concern that it may suppress the PGY4/5 learning experience. But for the most part, our residents were encouraged by the attendings virtual presence. It is important to note that the consultant and resident surgeons had previously worked together and were well aware of the others’ skill sets, capabilities and judgment.
During the pandemic, teams were truncated to one consultant and a resident with limited first-surgeon experience in major cases. While the distance mentoring technique allowed continuation of care where the PGY4/5 residents were able to safely complete 96% of emergency laparotomies[10], this would have little impact on attending surgeons. The reduction of surgical staff in the operating room remained a problem.
Robotic surgery would have been a good solution, since it had enjoyed good success across the globe[17], but it had not been used in the Caribbean before. One reason for this is that most Caribbean nations are in middle-income or low-income brackets[1,4] and could not afford to acquire commercially available surgical robots[13]. In addition, distributors were generally reluctant to supply robotic equipment to the Caribbean because most were low-income countries, including some of the poorest in the Western Hemisphere[1,4]. From an economic standpoint, distributors may have been reluctant because they thought that these poor nations would not be able afford the hardware and necessary consumables.
Surgical leaders recognized the need to accelerate the search for affordable technology in the face of the 2020 pandemic. We were able to identify a suitable and relatively inexpensive robotic arm and then engage a distributor to supply the equipment in the Caribbean. The FreeHand® robotic arm (Freehand 2010 Ltd., Guildford, Surrey, United Kingdom) is a single robotic arm designed to control the laparoscope via infrared signals from the surgeon. This alleviates the need for an assistant surgeon and allows the operating room to function with skeleton staff. Via a private-public partnership, a FreeHand® robotic arm (Freehand 2010 Ltd., Guildford, Surrey, United Kingdom) was first used at this facility during the pandemic[18]. To date, the robot has been used to perform a variety of FreeHand® robot-assisted operations including liver resections, pancreatic resections, ventral hernia repairs, inguinal hernia repairs, fundoplications, colectomies, gastrectomies, prostatectomies and hysterectomies.
In our experience, this provided a good balance with a lower procurement cost than other commercially available surgical robots, but provides some advantages over traditional laparoscopy. First, the surgeon is in full control over the robot that handles the laparoscope, thereby eliminating human error by a camera person. The head movements to control the robot easy to learn as they are similar to the surgeons’ actions to move their heads to view the operative field. While training is obviously necessary before embarking on the use of FreeHand, the training is fairly simple for attending surgeons who are already adept at laparoscopy.
As this paper was being written, Trinidad & Tobago was at the peak of its third wave of the COVID pandemic and the existing responses remained in place. It is clear that humankind will have to learn to live with the pandemic induced changes. Therefore, we acknowledge that the situation is fluid and that these changes will need to be versatile. In order to overcome this, we must consolidate and have.
Surgical leaders must recognize that the pandemic has forced us to make significant changes. Of course, some surgeons will resist the deviation from “cultural norms” in the Caribbean. We have to address this early by seeking stakeholder buy-in and by providing training for technology, which at first may seem daunting to many persons. We also believe that surgical leaders must continue to step up and advocate for policy to ensure that surgical services to function appropriately in the face of the pandemic[19,20].
It is clear that the healthcare environment in the Caribbean differ significantly from those in developed countries. We work in low-resource systems with many limitations, including high dependency bed shortages, understocked blood banks, consumable shortages and limited operating time. We have found ways to overcome these challenges that may not be suitable to large, developing countries. We advocate, therefore, that surgeons must critically appraise their local hospitals and understand the pitfalls in their environment in order to introduce policy that would maintain quality service delivery that suits the local healthcare environment.
Admittedly, these changes were largely driven by the need to continue patient care during the pandemic. We also acknowledge that technical capability has outpaced the medico-legal aspect of patient care during the pandemic. This should serve as a stimulus for policy makers to have guidelines in place for telemedicine.
The COVID pandemic has proved to be resilient and expected to continue for years to come. In the face of this, surgical leaders should continue to adapt and lead the charge for policy that will allow their hospital to continue functioning. In our environment, virtual multidisciplinary meetings, FaceTime® consultations, remote mentoring and robot-assist laparoscopy have been invaluable adjuncts that allow our service to continue functioning effectively. COVID may have acted as a catalyst increasing our use of basic digital technology. This is unlikely to return to pre-pandemic behavior, further improving our practice.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: Trinidad and Tobago
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Fakhradiyev I, Kazakhstan; Lopes-Junior LC, Brazil; Tung TH, China S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Hunte SA, Pierre K, St Rose R, Simeon DT. Health Systems' Resilience: COVID-19 Response in Trinidad and Tobago. Am J Trop Med Hyg. 2020;103:590-592. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 2. | Tang B, Bodkyn C, Gupta S, Denburg A. Access to WHO Essential Medicines for Childhood Cancer Care in Trinidad and Tobago: A Health System Analysis of Barriers and Enablers. JCO Glob Oncol. 2020;6:67-79. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 3. | Ramdass MJ, Cawich SO, Pooran S, Milne D, Ali E, Naraynsingh V. Declaration of a state of emergency in Trinidad and Tobago: effect on the trauma admissions at the National Referral Trauma Centre. Prehosp Disaster Med. 2015;30:229-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Bahall M. Health services in Trinidad: throughput, throughput challenges, and the impact of a throughput intervention on overcrowding in a public health institution. BMC Health Serv Res. 2018;18:129. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 5. | Maharaj SB, Ramsewak SS, Dookeram D, Franco D. Did vaccine inequity lead to the second wave of COVID-19 infections in Trinidad and Tobago? BMJ Glob Health. 2021;6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Ramsingh RAE, Duval JL, Rahaman NC, Rampersad RD, Angelini GD, Teodori G. Adult cardiac surgery in Trinidad and Tobago during the COVID-19 pandemic: Lessons from a developing country. J Card Surg. 2020;35:3387-3390. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 7. | Selby L, Tripathi V, Hariharan S. Knowledge, Attitudes and Practices (KAP) regarding the Novel Coronavirus Disease (COVID-19) Post-lockdown in Trinidad and Tobago. Soc Work Public Health. 2021;36:558-576. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Besson GA Ed. The Caribbean History Archives. 1st ed. Palo Alto. CA, USA. Paria Publishing Company Ltd. 2013: 31-33. [DOI] [Full Text] |
| 9. | Nayak BS, Sahu PK, Ramsaroop K, Maharaj S, Mootoo W, Khan S, Extravour RM. Prevalence and factors associated with depression, anxiety and stress among healthcare workers of Trinidad and Tobago during COVID-19 pandemic: a cross-sectional study. BMJ Open. 2021;11:e044397. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 27] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 10. | Cawich SO, Mencia M, Thomas D, Spence R, Milne D, Naraynsingh V, Barrow S. Trauma surgery via distance mentoring: A model inspired by the 2020 pandemic. Trop Doct. 2022;52:101-103. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Gopaul CD, Ventour D, Thomas D. ChAdOx1 nCoV-19 Vaccine Side Effects among Healthcare Workers in Trinidad and Tobago. Vaccines (Basel). 2022;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Cawich SO, Johnson PB, Shah S, Roberts P, Arthurs M, Murphy T, Bonadie KO, Crandon IW, Harding HE, Abu Hilal M, Pearce NW. Overcoming obstacles to establish a multidisciplinary team approach to hepatobiliary diseases: a working model in a Caribbean setting. J Multidiscip Healthc. 2014;7:227-230. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 13. | Hariharan S, Chen D. Costs and Utilization of Operating Rooms in a Public Hospital in Trinidad, West Indies. Perm J. 2015;19:e128-e132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 14. | Griffith SP, Cawich SO, Mencia M, Naraynsingh V, Pearce NW. Laparoscopic Liver Resection by Distance Mentoring - Trinidad to Barbados: A Report. Cureus. 2019;11:e5796. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Cawich SO, Griffith SP, Wilson C, FaSiOen PR, Burgess P, Thomas DA, Mencia M, Pearce NW, Kluger MD, Naraynsingh V. Distance mentoring in advanced minimally invasive surgery in the Caribbean: A model for low‐resource environments. Curr Med Res Prac. 2021;11:125-127. [DOI] [Full Text] |
| 16. | Cawich SO, Simpson L, Josephs A. Laparoscopic Hepatectomy via Remote Mentoring From Jamaica to Trinidad. Cureus. 2021;13:e20177. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Lane T. A short history of robotic surgery. Ann R Coll Surg Engl. 2018;100:5-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 99] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 18. | Cawich SO, Arulampalam T, Senasi R, Naraynsingh V. Robot-Assisted Minimally Invasive Surgery: First Report from the Caribbean. Cureus. 2021;13:e18739. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | Stephens EH, Dearani JA, Guleserian KJ. Courage, Fortitude, and Effective Leadership of Surgical Teams During COVID-19. World J Pediatr Congenit Heart Surg. 2020;11:675-679. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 20. | Klingensmith ME. Leadership and followership in surgical education. Am J Surg. 2017;213:207-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |