Published online Jun 28, 2022. doi: 10.13105/wjma.v10.i3.143
Peer-review started: December 18, 2021
First decision: March 13, 2022
Revised: March 23, 2022
Accepted: June 21, 2022
Article in press: June 21, 2022
Published online: June 28, 2022
Processing time: 199 Days and 8.5 Hours
Platelet-rich plasma has been gaining popularity as an agent for biological augmentation either as the sole treatment modality or as an adjunct to surgical repair. There is substantial discrepancy in the results of the published meta-analyses; and the true efficacy and role of using autologous platelet-rich plasma (PRP) at the time of rotator cuff repair is still ambiguous.
To performed this systematic overview on the overlapping meta-analyses that analyzed autologous PRP as an adjuvant in the repair of rotator cuff tears and identify the studies which provide the current best evidence on this subject and generate recommendations for the same.
We conducted independent and duplicate electronic database searches in PubMed, Web of Science, Scopus, Embase, Cochrane Database of Systematic Reviews, Reference Citation Analysis and the Database of Abstracts of Reviews of Effects on September 8, 2021 to identify meta-analyses that analyzed the efficacy of PRP as an adjuvant in the repair of rotator cuff tears. Methodological quality assessment was made using Oxford Levels of Evidence, AMSTAR scoring and AMSTAR 2 grades. We then utilized the Jadad decision algorithm to identify the study with the highest quality to represent the current best evidence to generate the recommendation.
Twenty meta-analyses fulfilling the eligibility criteria were included. The AMSTAR scores of the included studies varied from 6-10 (mean: 7.9). All the included studies had critically low reliability in their summary of results due to their methodological flaws according to AMSTAR 2 grades. Significant heterogeneity was observed in the reporting of VAS, function outcome scores (long-term UCLA score, ASES score, SST score), operative time and long-term re-tear rates. Recent meta-analyses are more supportive of the role of intra-operative administration of PRPs at the bone-tendon interface in improving the overall healing and re-tear rates, functional outcome and pain. The initial size of the tear and type of repair performed do not seem to affect the benefit of PRPs. Among the different preparations used, leucocyte poor (LP)-PRP possibly offers the greatest benefit as a biological augment in these situations.
Based on this systematic overview, we give a level II recommendation that intra-operative use of PRPs at the bone-tendon interface can augment the healing rate, reduce re-tears, enhance functional outcome and mitigate pain in patients undergoing arthroscopic rotator cuff repair. LP-PRP possibly offers the greatest benefit in terms of healing rates, as compared with other platelet preparations.
Core Tip: Platelet-rich plasma has been gaining popularity as an agent for biological augmentation either as the sole treatment modality or as an adjunct to surgical repair. There is growing evidence on the positive effects of platelet-derived autologous growth factors on collagen production, cell proliferation, tissue revascularization and tendon regeneration thereby making them useful as an augment to arthroscopic rotator cuff repair. Based on our analysis, we found that the intra-operative use of PRPs at the bone-tendon interface can augment the healing rate, reduce re-tears, enhance functional outcome and mitigate pain in patients undergoing arthroscopic rotator cuff repair.
- Citation: Muthu S, Jeyaraman N, Patel K, Chellamuthu G, Viswanathan VK, Jeyaraman M, Khanna M. Evidence analysis on the utilization of platelet-rich plasma as an adjuvant in the repair of rotator cuff tears. World J Meta-Anal 2022; 10(3): 143-161
- URL: https://www.wjgnet.com/2308-3840/full/v10/i3/143.htm
- DOI: https://dx.doi.org/10.13105/wjma.v10.i3.143
Despite substantial improvements and huge strides made in the surgical procedures and the fixation constructs employed in the repair of rotator cuff tears, high failure rates persist to remain a major cause for concern[1]. The reported failure rates of rotator cuff repairs vary between 8 and 94%[1-4]; and multitudinous factors including age, systemic comorbidities, smoking status, size of tear, degree of fatty infiltration and surgical approaches or techniques have been purported to determine the outcome in these patients[5].
With the understanding that there is still room for significant improvement, the need for employing additional modalities for ameliorating healing in this setting has been growingly acknowledged[6]. It has been well-demonstrated that degenerated rotator cuff tissue has substantially compromised microcirculation, as compared with normal, healthy tissue[7]. Moreover, the fibro-vascular scar at the region of the bone-tendon interface following repair of the rotator cuff tear is of poorer quality in comparison with the innate tissue[8]. Since these aforementioned biological factors have been postulated to be the potential underlying cause for impaired tendon healing capacity after surgical repair, a significant degree of promise has been recently placed on biological augmentation strategies for enhancing tissue healing after rotator cuff repair surgeries[1,9].
Platelet-rich plasma (PRP) is a platelet concentrate which is prepared by centrifugation of autologous whole blood; and contains various growth factors including platelet-derived growth factor, insulin-like growth factor, transforming growth factor-β, epidermal growth factor and vascular endothelial growth factor. Based on the preparations and constitution (leukocyte content and fibrin architecture), PRP have been classified as pure PRP, leucocyte and PRP (L-PRP), leucocyte and platelet-rich fibrin (L-PRF) and pure platelet-rich fibrin (P-PRF)[1-6]. PRP and platelet-rich fibrin matrix have been gaining popularity as agents for biological augmentation in diverse sub-specialties of orthopedic surgery, either as the sole treatment modality or as an adjunct to surgical repair[8,9]. There is growing evidence from animal-based models on the positive effects of platelet-derived autologous growth factors on collagen produc
The overall purpose of the current study was to perform a detailed systematic review of the existing meta-analyses evaluating the role of PRP in patients undergoing rotator cuff repair; and to specifically provide answers to the following research questions, namely: (1) To evaluate the effect of this strategy on overall clinical outcome scores; (2) To evaluate the reduction in re-tear or failure rates; (3) To analyze the evolution and variations in the techniques of procurement and application of PRP across different studies; (4) To critically analyze and interpret the best currently available evidence and provide recommendations; and (5) To discern the major gaps in the existing literature and identify the scope for future research on this subject.
We present herewith a systematic overview of meta-analyses, performed by duly cohering the guidelines of the Back Review Group of Cochrane Collaboration[17]; and aim to report the same based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)[18].
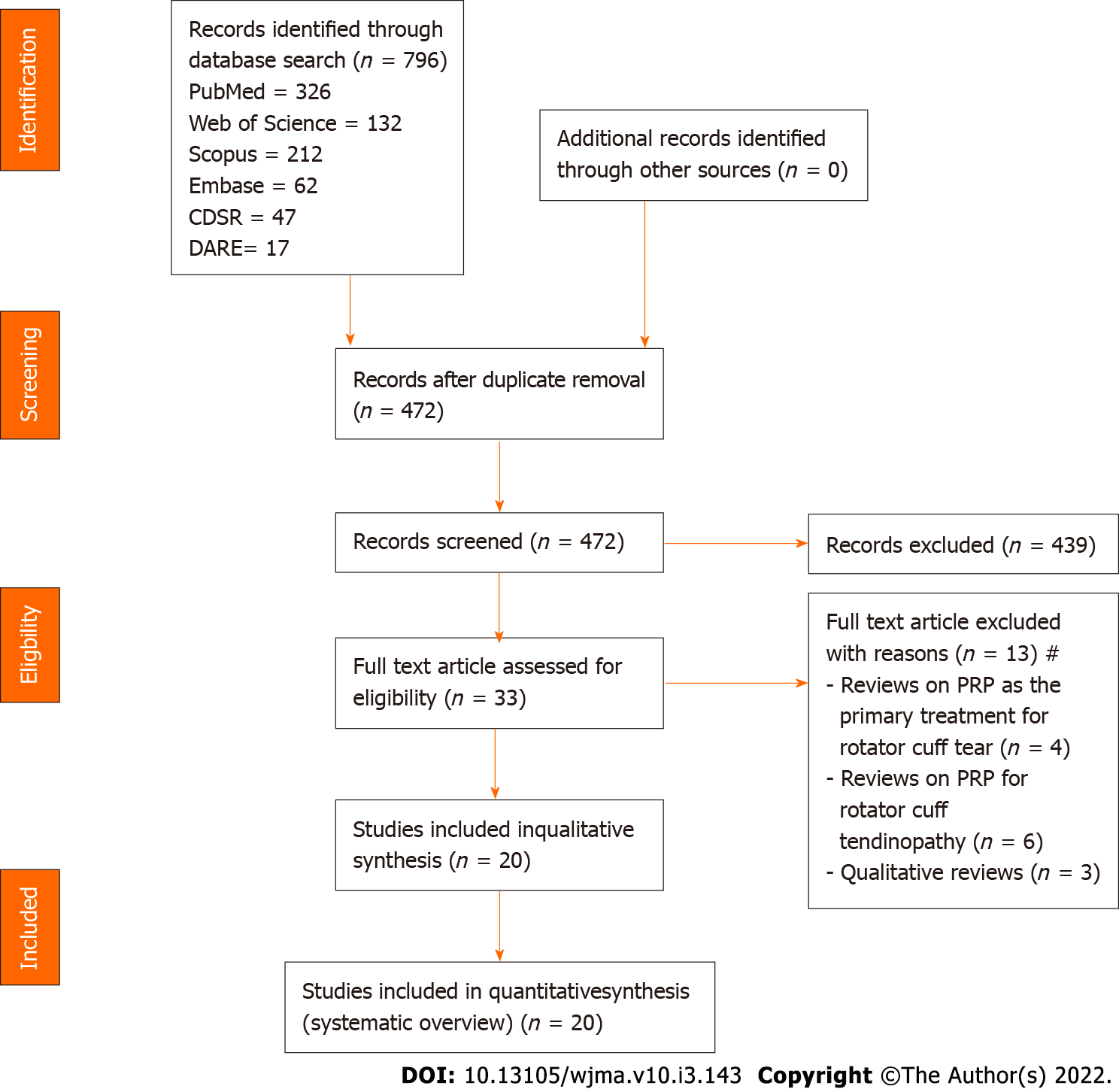
Two reviewers performed an independent literature search for systematic reviews with meta-analysis evaluating PRP therapy along with surgical repair for rotator cuff tear. The comprehensive search was performed on the electronic databases including PubMed, Web of Science, Scopus, Embase, Cochrane Database of Systematic Reviews, Reference Citation Analysis and the Database of Abstracts of Reviews of Effects on September 8, 2021. Our search was neither restricted to any specific language nor confined to any particular period. The electronic search strategy was designed in accordance with the Peer Review of Electronic Search Strategy (PRESS) guidelines[19]. The keywords used for the search included: “Platelet-rich Plasma”, “PRP”, “rotator cuff repair”, “rotator cuff tear”, “clinical outcome”, “re-tear rate”, “failure rate”, “Systematic Review”, “Meta-analysis” together with Boolean operators such as “AND”, “OR” and “NOT”. A manual search of the key journals was made; and reference list of the selected articles was searched to identify studies not identified in the primary search. Additionally, a search was also made in the International prospective register of systematic reviews for any ongoing review which is nearing completion. All the studies meeting the inclusion criteria were included and analyzed. Any discrepancy between the two reviewers was resolved through discussion until a consensus was achieved. The PRISMA flow chart for the study selection into systematic overview has been shown in Figure 1.
Review articles were included in our study if they satisfied the following criteria: Systematic review with meta-analysis comparing surgical repair with and without PRP for rotator cuff tears. Studies which analyzed at least one of the outcome measures like Visual analog scale (VAS) score, Disabilities of the Arm, Shoulder and Hand (DASH) score, Constant score, University of California Los Angeles (UCLA) score, American Shoulder and Elbow Surgeons (ASES) score, Simple Shoulder Test (SST) score, operating time, patient satisfaction, tendon healing and re-tear rates.
Narrative reviews, systematic reviews without data pooling/meta-analysis, systematic reviews with mixed intervention groups, correspondence articles, pre-clinical studies, studies on animal models and cadaveric studies were excluded.
Data was extracted from meta-analyses by two reviewers independently. Notably, data extracted from the studies included: First author details, date of last literature search performed, year and journal of publication, number, and nature of studies included, language restrictions, criteria for inclusion and exclusion for studies, databases used for literature search, software employed for analysis, subgroup/sensitivity analysis, analysis of publication bias, conflict of interest, Grading of Recommendations Assessment, Development, and Evaluation (GRADE) summary, and I2 statistic value of variables in each meta-analysis. Disagreements were settled by consensus.
The methodological quality of included reviews was evaluated using Oxford Levels of Evidence[20]. Additionally, the Assessment of Multiple Systematic Reviews (AMSTAR)[21] and its updated grading tool AMSTAR 2[22] were also used to assess their methodological robustness with good validity and reliability[23]. Two reviewers independently assessed quality of methodology of the included studies. Disagreements were settled by consensus.
I2 test was used for the assessment of heterogeneity[24]. When I2 > 50% and P < 0.1, heterogeneity is deemed to exist among included trials; and the reviewers evaluated whether the studies utilized sensitivity or subgroup analyses to assess the reasons for heterogeneity and strengthen the robustness of pooled data.
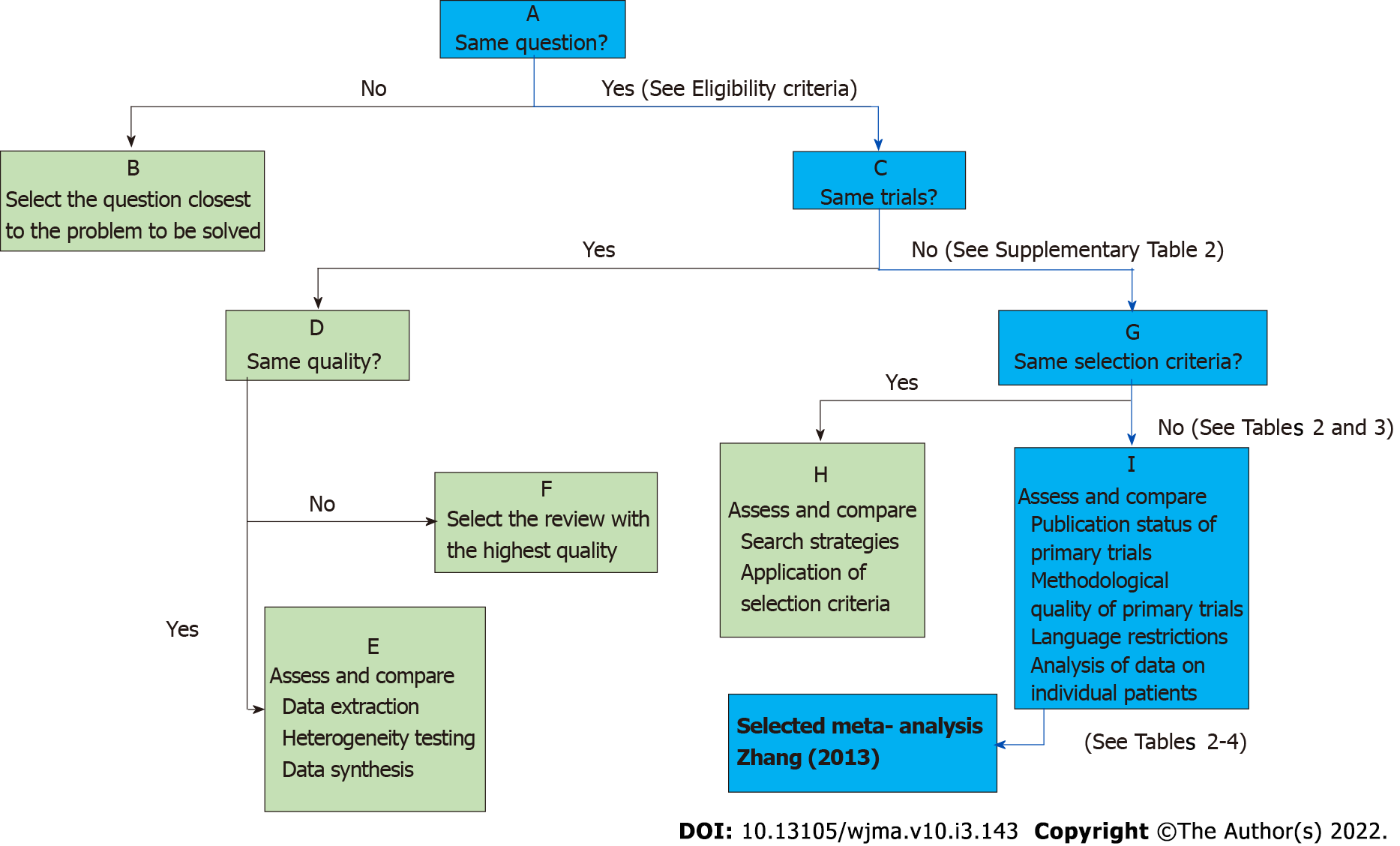
Variability in the findings among included meta-analyses was interpreted with the help of Jadad decision algorithm. As per Jadad et al[25], possible reasons for discordance in the results among studies include differences in study question, inclusion and exclusion criteria, quality assessment, data pooling/extraction and statistical analysis. Currently, this is the most commonly used algorithm for generating recommendations among meta-analyses with discordant results[26-29]. Two reviewers used this algorithm independently to arrive at a single meta-analysis representing the current best evidence in order to generate recommendations.
A comprehensive search of the electronic database generated 838 articles which were subjected to an initial screening for removing duplicate articles. This yielded 514 articles. Further screening of title and abstract resulted in the exclusion of 481 articles. Therefore, 33 articles qualified for reviewing the full-text. Upon full-text review by both reviewers, 13 were excluded. Finally, 20 meta-analyses were included in this systematic review[30-46,1,47,48]. These overlapping meta-analyses were published in different journals between 2012 and 2021; and the number of studies included in them ranged between 5 and 19 (Table 1). The publication years of the included studies in these meta-analyses ranged between 2008 and 2020 as shown in Supplementary Table 1.
| Sl. No | Ref. | Publication date | Publication journal | Literature search date | No. of studies included |
| 1 | Chahal et al[32], 2012 | June 14, 2012 | Arthroscopy: The Journal of Arthroscopic and Related Surgery | December 30, 2011 | 5 |
| 2 | Moraes et al[31], 2013 | December 23, 2013 | Cochrane Database of Systematic Reviews | March 25, 2013 | 19 |
| 3 | Zhang et al[30], 2013 | July 12, 2013 | PLoS One | April 20, 2013 | 7 |
| 4 | Li et al[33], 2014 | June 7, 2014 | Arthroscopy: The Journal of Arthroscopic and Related Surgery | May 1, 2013 | 7 |
| 5 | Zhao et al[29], 2014 | September 30, 2014 | Arthroscopy: The Journal of Arthroscopic and Related Surgery | September, 2013 | 8 |
| 6 | Warth et al[35], 2014 | November 13, 2014 | Arthroscopy: The Journal of Arthroscopic and Related Surgery | September, 2013 | 11 |
| 7 | Vavken et al[36], 2015 | March 12, 2015 | The American Journal of Sports Medicine | August 1, 2014 | 13 |
| 8 | Cai et al[38], 2015 | October 8, 2015 | Journal of Shoulder and Elbow Surgery | January, 2015 | 5 |
| 9 | Xiao et al[37], 2016 | October 30, 2016 | International Journal of Clininical and Experimental Medicine | February 1, 2016 | 15 |
| 10 | Hurley et al[40], 2018 | February 21, 2018 | The American Journal of Sports Medicine | March 24, 2017 | 18 |
| 11 | Han et al[39], 2019 | June 20, 2019 | Journal of Orthopaedic Surgery and Research | September, 2016 | 13 |
| 12 | Wang et al[41], 2019 | July 29, 2019 | PLoS One | September 15, 2018 | 8 |
| 13 | Chen et al[42], 2019 | November 19, 2019 | The American Journal of Sports Medicine | December, 2017 | 18 |
| 14 | Cavendish et al[43], 2020 | May 1, 2020 | Journal of Shoulder and Elbow Surgery | May 23, 2018 | 16 |
| 15 | Hurley et al[44], 2020 | July 30, 2020 | The American Journal of Sports Medicine | March, 2020 | 13 |
| 16 | Yang et al[45], 2020 | October 14, 2020 | Nature research | February 15, 2020 | 7 |
| 17 | Zhao et al[46], 2020 | November 18, 2020 | Journal of Shoulder and Elbow Surgery | March, 2020 | 10 |
| 18 | Ryan et al[1], 2021 | March 17, 2021 | Arthroscopy: The Journal of Arthroscopic and Related Surgery | June, 2020 | 17 |
| 19 | Xu et al[48], 2021 | July 13, 2021 | The Orthopaedic Journal of Sports Medicine | June 20, 2020 | 14 |
| 20 | Li et al[47], 2021 | May 27, 2021 | Arthroscopy: The Journal of Arthroscopic and Related Surgery | October 29, 2020 |
Although the included meta-analyses made a comprehensive literature search, the search databases employed were not similar. Sixteen, 1 and 7 studies searched PubMed, Embase and Medline databases, respectively. While 2 of them searched the Cochrane library, one searched Web of Science. 18 searched Scopus, 16 Google Scholar, 3 Cumulative Index to Nursing and Allied Health Literature (CINAHL) database, 2 China National Knowledge Infrastructure (CNKI) database, 1 Wan fang and 2 meta-analyses searched VIP database. Of the 20 studies, 4 included studies only in English[1,42,43,46] while 7 others mentioned no linguistic restriction in their search criteria[30,33,38,40,41,44,45]. Further details regarding the search methodology employed in the included meta-analyses has been presented in Table 2.
| Sl. No | Search parameters | Chahal (2012) | Moraes (2013) | Zhang (2013) | Li (2014) | Zhao (2015) | Warth (2015) | Vavken (2015) | Cai (2015) | Xiao (2016) | Hurley (2018) | Han (2019) | Wang (2019) | Chen (2019) | Cavendish (2020) | Hurley (2020) | Yang (2020) | Zhao (2021) | Ryan (2021) | Xu (2021) | Li (2021) |
| 1 | Publication language restriction | X | X | NA | X | X | X | X | NA | X | NA | X | NA | √ | √ | NA | NA | √ | √ | X | NA |
| 2 | Publication status restriction | X | NA | NA | NA | X | NA | NA | NA | X | X | NA | NA | X | NA | X | NA | NA | NA | X | NA |
| 3 | PubMed | √ | X | √ | √ | √ | √ | √ | √ | √ | X | √ | √ | √ | √ | X | √ | √ | √ | X | √ |
| 4 | Medline | √ | √ | X | X | X | X | X | X | X | √ | X | X | √ | X | √ | X | X | √ | √ | X |
| 5 | Embase | X | X | X | √ | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| 6 | Cochrane library | X | X | X | √ | X | X | X | X | X | X | X | X | X | X | X | X | X | X | √ | X |
| 7 | Web of Science | X | √ | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| 8 | Scopus | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ | X | √ | √ | √ | √ | X | √ | √ |
| 9 | Google Scholar | √ | √ | √ | X | √ | X | √ | X | √ | √ | √ | √ | √ | X | √ | √ | √ | √ | √ | √ |
| 10 | CINAHL | X | X | X | X | X | X | X | √ | √ | X | X | X | X | X | X | X | X | X | X | √ |
| 11 | AMED | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| 12 | CNKI | X | X | X | X | X | X | X | X | √ | X | X | X | X | X | X | √ | X | X | X | X |
| 13 | Wan Fang | X | X | X | X | X | X | √ | X | X | X | X | X | X | X | X | X | X | X | X | X |
| 14 | CBM literature | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X | X |
| 15 | VIP | X | X | X | X | X | X | X | X | X | √ | X | X | X | X | √ | X | X | X | X | X |
Using Oxford Levels of Evidence, the quality of included studies was determined based on the nature of primary studies considered in the analysis. Of the 20 studies analyzed, 6 were of level-II evidence, one level-III and the rest of them were of level III evidence (Table 3). Among the 20 studies, 12 used RevMan5.3, 4 used Stata software, 1 used open meta, 2 used R-foundation for data analyses; while in one study, the software employed was not mentioned (Table 3). Additionally, three studies utilized the GRADE system, 12 studies performed sensitivity analysis and 16 conducted sub-group analysis to explore the heterogeneity in their results. Eleven studies assessed for possible publication bias.
| Sl. No | Search parameters | Chahal (2012) | Moraes (2013) | Zhang (2013) | Li (2014) | Zhao (2015) | Warth (2015) | Vavken (2015) | Cai (2015) | Xiao (2016) | Hurley (2018) | Han (2019) | Wang (2019) | Chen (2019) | Cavendish (2020) | Hurley (2020) | Yang (2020) | Zhao (2021) | Ryan (2021) | Xu (2021) | Li (2021) |
| 1 | Primary study design | RCT, CCT,RCS | RCT | RCT | RCT | RCT | RCT CCT | RCT | RCT | RCTCCT | RCT | RCT | RCT | RCT | RCT | RCT | RCT | RCT | RCT | RCT | RCT |
| 2 | Level of Evidence | III | I | I | II | I | II | I | I | II | I | I | I | I | II | I | I | II | I | I | II |
| 3 | Software Used | RevMan 5.3 | RevMan 5.3 | RevMan 5.3 | NA | RevMan 5.3 | Open Meta | STATA 10 | RevMan 5.3 | RevMan 5.3 | RevMan 5.3 | RevMan 5.3 | RevMan 5.3 | STATA 15.1 | STATA 13 | R Foundation (netmeta package Version 0.9-6 in R) | RevMan 5.3 | RevMan 5.3 | R Foundation for Statistical Computing, Vienna, Austria | STATA 15 | RevMan 5.3 |
| 4 | GRADE Used | X | √ | X | X | √ | X | X | X | X | X | X | √ | X | X | X | X | X | X | X | X |
| 5 | Sensitivity Analysis | √ | √ | X | √ | √ | √ | √ | X | √ | X | √ | √ | √ | X | X | X | √ | X | X | √ |
| 6 | Subgroup Analysis | √ | √ | √ | X | √ | √ | √ | √ | X | √ | √ | √ | √ | √ | X | √ | √ | √ | √ | X |
| 7 | Publication Bias | X | √ | √ | X | √ | √ | √ | √ | √ | X | √ | √ | √ | √ | X | X | X | X | X | X |
As shown in Table 4, AMSTAR scores of included studies ranged between 6 and 10 (mean 7.8). Based on AMSTAR-2 grading, none of the studies were without any critical methodological flaw in the conduction of meta-analysis. Among all included studies, the meta-analysis by Zhang et al[30] was found to be of the highest quality with an AMSTAR score of 10/11 (Table 4). However, this study also suffered from critical methodological flaws of including status of publication (i.e. grey literature) as a criterion for inclusion and did not provide the list of (included and excluded) studies.
| Sl. No | AMSTAR domains | Chahal (2012) | Moraes (2013) | Zhang (2013) | Li (2014) | Zhao (2015) | Warth (2015) | Vavken (2015) | Cai (2015) | Xiao (2016) | Hurley (2018) | Han (2019) | Wang (2019) | Chen (2019) | Cavendish (2020) | Hurley (2020) | Yang (2020) | Zhao (2021) | Ryan (2021) | Xu (2021) | Li (2021) |
| 1 | Was a priori design provided? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 2 | Were there duplicate study selection and data extraction? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 |
| 3 | Was a comprehensive literature search performed? | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 1 |
| 4 | Was the status of publication (i.e. grey literature) used as an inclusion criterion? | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 5 | Was a list of studies (included and excluded) provided? | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 6 | Were the characteristics of the included studies provided? | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 7 | Was the scientific quality of the included studies assessed and documented? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 8 | Was the scientific quality of the included studies used appropriately in formulating conclusions? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 9 | Were the methods used to combine the findings of studies appropriate? | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| 10 | Was the likelihood of publication bias assessed? | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 |
| 11 | Was the conflict of interest stated? | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Total AMSTAR score | 8 | 8 | 10 | 8 | 8 | 7 | 8 | 6 | 8 | 8 | 8 | 8 | 7 | 9 | 8 | 8 | 6 | 7 | 8 | 8 | |
| Critical Methodological Flaw | 3 | 3 | 1 | 3 | 2 | 2 | 3 | 5 | 2 | 3 | 2 | 3 | 4 | 1 | 3 | 3 | 4 | 4 | 3 | 2 | |
| Non-Critical Flaw | 1 | 1 | 1 | 1 | 1 | 3 | 1 | 1 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | |
| AMSTAR 2 Grade | CL | CL | CL | CL | CL | CL | CL | CL | CL | CL | CL | CL | CL | CL | CL | CL | CL | CL | CL | CL |
All the studies included used I2 statistic for heterogeneity assessment. Mild heterogeneity was noted in short-term UCLA score, tendon healing rates and patient satisfaction. Heterogeneity in the reporting of DASH score, Constant score and short-term re-tear rate was moderate; while heterogeneity of VAS, long-term UCLA score, ASES score, SST score, operative time and long-term re-tear rates was significant (Table 5). It is of utmost importance to probe into source of discordance among included studies, as recommendations generated are put into clinical practice and for developing public health-care policies[49]. The heterogeneity of results among the meta-analyses was primarily due to variation in the nature of primary studies included (other than RCTs).
| Sl. No | Outcome variables | Chahal (2012) | Zhang (2013) | Moraes (2013) | Li (2014) | Zhao (2015) | Warth (2015) | Vavken (2015) | Cai (2015) | Xiao (2016) | Hurley (2018) | Han (2019) | Wang (2019) | Chen (2019) | Hurley (2020) | Yang (2020) | Cavendish (2020) | Zhao (2021) | Ryan (2021) | Xu (2021) | Li (2021) |
| 1 | VAS Score – Short term | 29.9%+ | 0%- | 38%- | 0%- | 60.5%+ | 0%+ | 0%+ | 0%+ | ||||||||||||
| 2 | VAS Score – Long term | 67%- | 0%- | 0%- | 0%- | 0%+ | 0%- | 87.5%- | 0%+ | 0%- | 0%+ | 4%+ | 63%+ | ||||||||
| 3 | DASH Score – Short term | 0%- | 32%- | 30%- | |||||||||||||||||
| 4 | DASH Score – Long term | 0%- | NR- | 0%- | 0%- | 32%- | |||||||||||||||
| 5 | Constant Score – Short term | 30%+ | 0%+ | 0%+ | 23%+ | ||||||||||||||||
| 6 | Constant Score – Long term | NR- | 17%- | 50%+ | 86%- | 0%- | 26%- | 0%- | 0%- | 0%- | 0%+ | 0%- | 30.7%+ | 0%+ | 0%- | 19%+ | 36%+ | 47%+ | 0%+ | ||
| 7 | UCLA Score – Short term | 0%+ | 8.9%+ | 0%+ | 0%+ | ||||||||||||||||
| 8 | UCLA Score – Long term | NR- | 0%- | 35.18%- | 75%- | 0%- | 0%- | 60%- | 47%- | 0%- | 47%+ | 12%+ | 0%+ | 0%- | 49%+ | 64.18%- | 63%+ | 46%+ | |||
| 9 | ASES Score | 0%- | 0%- | 46%- | 58%- | 0%- | 54%- | 0%- | 26%- | 0%- | 41%- | 52%- | 0%+ | ||||||||
| 10 | SST Score | NR- | 47%- | 0%+ | 90%- | 0%- | 0%- | 47%- | 0%+ | 0%+ | 0%- | ||||||||||
| 11 | Operative time | 85%- | |||||||||||||||||||
| 12 | Patient Satisfaction | 0%- | 0%- | ||||||||||||||||||
| 13 | Tendon healing rate | 0%+ | 0%- | 0%+ | 10%- | ||||||||||||||||
| 14 | Retear rate – Short term | 0%- | 25%+ | 15.2%- | 30%- | 0%+ | 0%+ | 0%- | |||||||||||||
| 15 | Retear rate – Long term | 0%+ | 11%- | 14%- | 22%- | 43%- | 0%- | 0%- | 71%- | 0%+ | 0%- | 0%+ | 0%+ | 0%+ | 0%+ | 0%+ | NA+ | 4.7%+ | 22%+ |
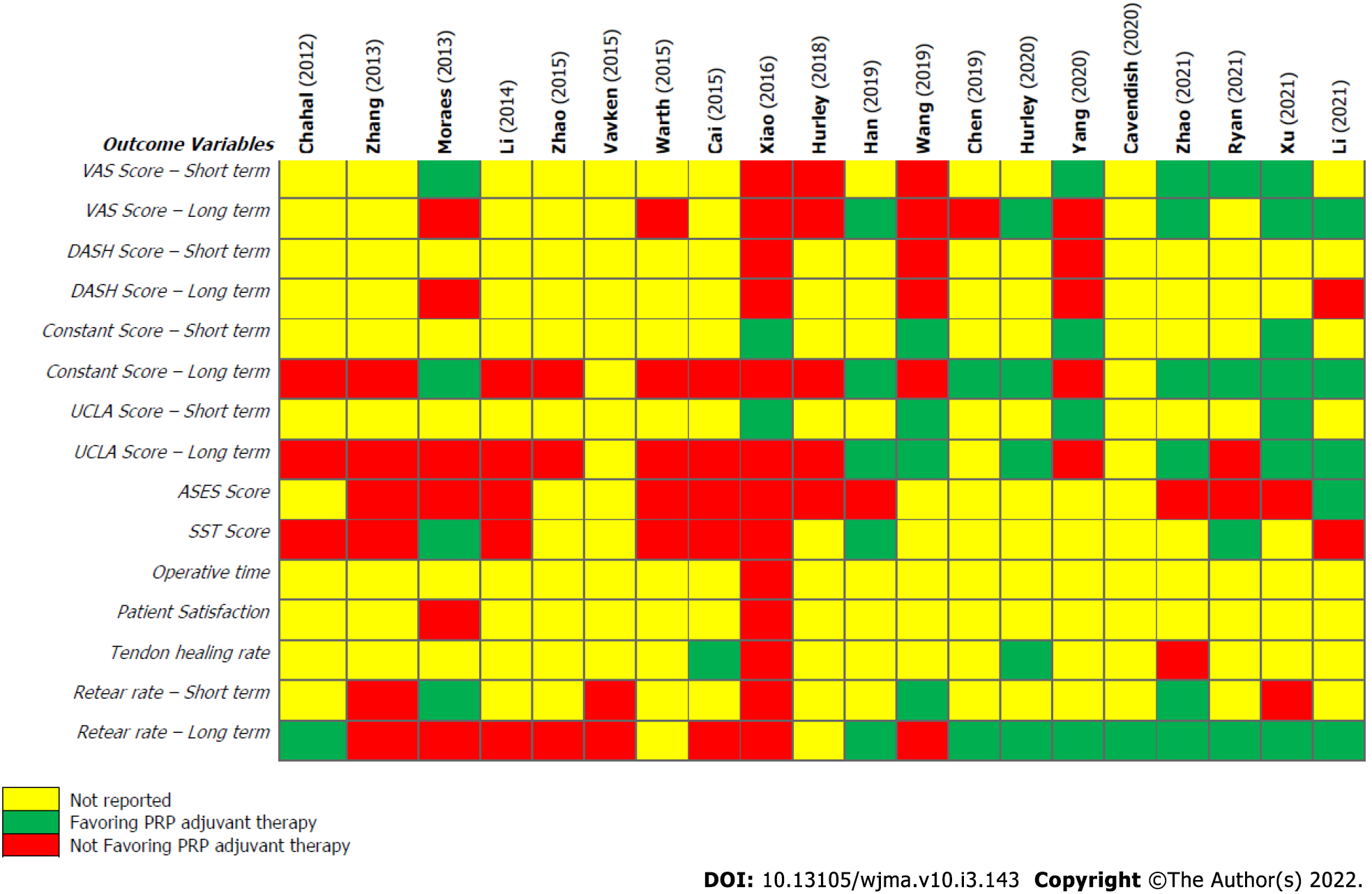
The pooled results from each included meta-analysis are presented in Figure 2. To identify the study which provides the best possible evidence to generate treatment recommendations, the Jadad decision algorithm was adopted. Two authors independently applied the decision algorithm to determine the meta-analysis with the highest quality to develop recommendation on the use of PRP in ARCR. Considering that all the 20 studies aimed to answer similar clinical questions despite analyzing a varied spectrum of primary studies, the study with the highest quality was selected on the basis of its methodological quality, restrictions involved (such as language or publication status), databases involved and analysis protocols adopted (Figure 3).
Based on this algorithm, the meta-analysis by Zhang et al[30] was determined to be the highest-quality study. This study observed no major benefits on overall clinical outcomes and re-tear rate following PRP administration in full-thickness rotator cuff tears; while a reduction in the rate of re-tears was demonstrated for small- and medium-sized tears. However, the selected study is also not free of critical methodological flaws based on AMSTAR 2 criteria. Hence, we analyzed the rationale for the development of the succedent systematic reviews as in Table 6 and tried to understand the evolution, variation in the techniques of procurement and application of PRP across different studies with due consideration to the high-quality evidence developed in the recent years and arrived at the following results.
| Sl. No. | Ref. | Date of publication | Date of last literature search | Level of evidence | Rationale for repeating meta-analysis | Conclusion |
| 1 | Chahal et al[32], 2012 | June 14, 2012 | December 30, 2011 | III | Earliest meta-analysis | No effect of PRP on overall retear rates or shoulder-specific outcomes after ARCR |
| 2 | Moraes et al[31], 2013 | December 23, 2013 | March 25, 2013 | I | Only included studies with intra-operative PRP application after ARCR | Some benefit of PRP in improving pain with comparable rates of retear (after 2 yr) between PRP and non-PRP groups |
| 3 | Zhang et al[30], 2013 | July 12, 2013 | April 20, 2013 | I | Included studies with high methodological quality and provided results without significant heterogeneity supported by larger number of patients | No benefit of PRP on overall clinical outcomes and retear rate in full-thickness rotator cuff tears and decrease in rate of retears with PRP for small- and medium-sized rotator cuff tear |
| 4 | Li et al[33], 2014 | June 7, 2014 | May 1, 2013 | II | All high-quality (7 studies) RCTs included (compared with previous studies) | No benefit with PRP regarding retear and clinical outcomes for ARCR |
| 5 | Zhao et al[29], 2014 | September 30, 2014 | September, 2013 | I | Newer RCTs as compared with previous meta-analysis | No benefit of PRP in ARCR of full-thickness tears in terms of similar retear rates and clinical outcomes |
| 6 | Warth et al[35], 2014 | September 13, 2014 | September, 2013 | II | Meta-regression analyses to evaluate the effects of 6 covariates such as inclusion of Level II studies, initial tear size, single- vs double-row repair constructs, varying PRP preparation, manual vs commercially available PRP preparation systems, method of PRP application on overall clinical and structural outcomes | No statistically significant differences in outcome scores or retear rate with the use of PRP. However, significant improvement in Constant scores when PRPs applied at tendon-bone interface and significant reduction in retear rate with PRP in tears > 3 cm repaired with double-row technique |
| 7 | Vavken et al[36], 2015 | March 12, 2015 | August 1, 2014 | I | To know if addition of PRP to ARCR results in statistically relevant as well as clinically meaningful reduction in retear rates along with analysis of its safety with difference in complication rates and its cost-effectiveness | PRP proved to be an effective and safe way of reducing retear rates in the arthroscopic repair of small- and medium-sized rotator cuff tears. However, no evidence to support its use in large and massive tear |
| 8 | Cai et al[38], 2015 | October 8, 2015 | January, 2015 | I | Meta-analysis of level I studies | PRP in full-thickness rotator cuff repairs showed no statistically significant difference in clinical outcome but demonstrated significant reduction in failure-to-heal rate for small-to-moderate tears |
| 9 | Xiao et al[37], 2016 | October 30, 2016 | February 1, 2016 | II | All level I and II evidence studies – included to enhance power of meta-analysis (15 studies) | No significant difference in the re-tear rates and clinical efficacy |
| 10 | Hurley et al[40], 2018 | February 21, 2018 | March 24, 2017 | I | First study to find that PRP was associated with significant improvement in tendon healing rates in tears > 3 cm with 9 new studies that have been published till Cai et al[38], 2015 | Use of PRP in rotator cuff repair improves the healing rates, pain levels, and functional outcomes. But PRF shows no benefit in improving tendon healing rates or functional outcomes |
| 11 | Han et al[39], 2019 | June 20, 2019 | September, 2016 | I | Inclusion of new RCTs, as compared with previous meta-analysis with improved pooled effect size | PRP treatment with ARCR showed decreases retear rate and improves clinical outcome |
| 12 | Wang et al[41], 2019 | July 29, 2019 | September 15, 2018 | I | To ensure homogeneity of data, only studies using PRP in full-thickness tears included along with addition of new high-level RCTs | PRP improved the short-term outcomes such as pain, retear rate, and shoulder function after ARCR in full-thickness rotator cuff tears. PRP when used in single-row fixation of ARCR demonstrated improved clinical outcomes. |
| 13 | Chen et al[42], 2019 | September 19, 2019 | December, 2017 | I | Exclusively reviewed only level 1 RCTs with multiple sub-groups, and comparative quantitative analysis with MCID on effects of LR-PRP vs LP-PRP, gel vs non-gel preparations, and tendon-specific outcomes analyzed | Long-term retear significantly decreased with PRP. Several PROs such as constant score, VAS, retear rate significantly improved in PRP-treated patients. However, all analyzed PROs failed to reach the 5% MCID threshold. Hence authors neither recommended nor discouraged the use of PRP for rotator cuff injuries |
| 14 | Cavendish et al[43], 2020 | May 1, 2020 | May 23, 2018 | II | Included 7 out of 16 studies published in the past 4 yr with larger sample size to reduce risk of type II error noted in previous studies | Intraoperative use of PRP reduces the failure risk following rotator cuff repair and has a consistent effect regardless of tear size and showed 25% reduction in the overall risk of failure in rotator cuff repairs |
| 15 | Hurley et al[44], 2020 | July 30, 2020 | March, 2020 | I | To ascertain whether there is evidence to support the use of LP- or LR-PRP as an adjunct to ARCR | LP-PRP reduces rate of retear and/or incomplete tendon healing after ARCR and improves patient-reported outcomes as compared with control whereas whether LP-PRP improves the tendon healing rate when compared with LR-PRP remained unclear |
| 16 | Yang et al[45], 2020 | October 14, 2020 | February 15, 2020 | I | Inclusion of studies that dealt with PRP application on bone–tendon interface only during arthroscopic repair and studies that administered only PRP and not any other platelet-rich matrix to lower bias caused by different materials. All included RCTs were conducted on patients with full thickness rotator cuff tear who received diagnoses based on preoperative MRI or sonography | Application of PRP shown to be beneficial in reducing the retear rate and improving the functional outcomes during the short-term follow-up of single-row repair |
| 17 | Zhao et al[46], 2020 | November 18, 2020 | March, 2020 | II | Meta-analysis of level I and II studies based on MCID values to comprehensively assess clinical efficacy of LP-PRP only for ARCR mainly to avoid heterogeneity due to different types of PRP | LP-PRP - significantly reduces the postoperative retear rate in medium and long term regardless of tear size and method used for repair. But no clinically meaningful effects in terms of postoperative pain and patient-reported outcomes were noted |
| 18 | Ryan et al[1], 2021 | March 17, 2021 | June, 2020 | I | Involved stratified pooled data on basis of leukocyte concentration, liquid and solid formulation, and all 4 types of PRP (P-PRP, P-PRF, LP-PRP, LP-PRF) | This analysis demonstrates significant reductions in retear when rotator cuff repair is augmented with PRP. LP-PRP appears to be most effective formulation, resulting in significantly improved retear rates and clinical outcome scores when compared with controls |
| 19 | Xu et al[48], 2021 | May 27, 2021 | October 29, 2020 | II | Analyzed PRP and PRF separately and PRP was sub grouped into leukocyte-poor and leukocyte-rich PRP. Compared with study by Hurley et al 5 more RCTs included. Cochrane Collaboration risk of bias tool- adopted and retear rate was analyzed based on duration of follow-up into 2 subgroups with a cut off of 2 yr | PRP in ARCR improved pain and functional outcome, reduces retear rates. PRF improved only the Constant score. Significant reduction of retear rate in leukocyte-poor PRP when followed-up > 2 yr |
| 20 | Li et al[47], 2021 | July 13, 2021 | June 20, 2020 | I | Strict eligibility criteria enforced in the inclusion of RCTs along with subgroup analysis, based on PRP preparation, time of administration, size of tear, type of repair, to assess the real utility of PRP | ARCR with PRP significantly improved long-term retear, shoulder pain and long-term shoulder function scores and intraoperative application of leukocyte-poor plasma for large to massive tears contributed to significant decrease in retear rates |
Significant heterogeneity was observed in the reporting of VAS, function outcome scores (long-term UCLA score, ASES score, SST score), operative time and long-term re-tear rates. Recent meta-analyses are more supportive of the role of intra-operative administration of PRPs at the bone-tendon interface in improving the overall healing and re-tear rates, functional outcome and pain. The initial size of the tear and type of repair performed do not seem to affect the benefit of PRPs. Among the different preparations used, leucocyte poor (LP)-PRP possibly offers the greatest benefit as a biological augment in these situations.
Different studies employed specific criteria to include studies with an aim to provide more useful and relevant information as compared to the previously-published literature. Chen et al[42] (2019), Hurley et al[44] (2020), Zhao et al[46] (2021), Ryan et al[1] (2021) and Li et al[47] (2021) compared the effects of PRP preparations on the basis of their relative leukocyte concentrations[1,42,44,46,47].
The initial studies by Chahal et al[32] (2012), Moraes[31] (2013), Zhang et al[30] (2013), Li et al[33] (2014), Zhao et al[34] (2014) and Xiao et al[37] (2016) did not reveal any benefit following PRP application[31-34,37]. Warth et al[35] (2014), Hurley et al[44] (2018) and Xu et al[48] (2021) observed that PRP was more helpful in enhancing the healing rates of large-sized tears[44,48]. Vavken et al[36] (2015) and Cai et al[38] (2015) reported better outcome following PRP application in small- to medium-sized tears[36,38]. The recent studies published by Han et al[39] (2019), Wang et al[41] (2019), Chen et al[42] (2019), Yang et al[45] (2020) and Cavendish et al[43] (2020) concluded that intraoperative PRP application significantly enhanced the short- and long-term clinical outcome and mitigated the re-tear rates after RC repair[39,41-43,45]. The recently-published literature [Hurley et al[44] (2020), Zhao et al[46] (2021), Ryan et al[1] (2021), Li et al[47] (2021) and Xu et al[48] (2021)] also seemed to demonstrate better outcome (functional scores and re-tear rates) with LP-PRP, as compared with LR-PRP[1,33,44,46,48]. The individual data of the included studies are presented in Table 6.
To date, numerous RCTs have analyzed the efficacy of adjuvant PRP therapy in patients undergoing surgical repair of RC tears[6,30,39]. Although theoretically, biological augmentation with PRP can potentially enhance healing and mitigate failure rates after arthroscopic rotator cuff repair, our understanding of the exact role of PRP therapy in this scenario is still ambiguous[9,33]. Limited sample sizes, heterogeneity in the treatment protocols, PRP preparations and techniques employed; and the paucity of long- term results have been the major limitations of the currently published studies on this subject[1,6].
To further strengthen the results, multiple meta-analyses have been conducted to consolidate the findings of more recent RCTs, so as to provide the higher level of evidence on the effectiveness of the intervention in operatively-treated RC tears[6]. However, the spectra of primary studies included in the recent analysis and the databases utilized for study inclusion are still discordant[1,37,48]. Hence, a systematic overview of these overlapping meta-analyses was planned in order to identify the highest quality study among the available studies; as well as to formulate and generate recommendations regarding the use of adjuvant PRP in such situations.
Platelets are a source of high concentrations of different growth factors (like platelet-derived growth factor, transforming growth factor-beta, fibroblast growth factor, vascular endothelial growth factor and epidermal growth factor) which can potentially stimulate cell proliferation. They form a temporary matrix which can fill the defects and thereby provide a scaffold for cell migration and tissue remodeling[34]. The earliest meta-analysis on this subject was published by Chahal et al[32] in 2013. Although they observed marginal benefits in small and moderate sized tears, there was no major improvement in the overall re-tear rates or shoulder-specific outcomes after ARCR in larger or at-risk tears. Following this, in a Cochrane review, Moraes et al[31] reviewed studies involving intra-operative application of PRP; and concluded marginal benefits of PRP administration, especially with respect to improvements in short-term VAS and short-term re-tears. There has been a recent surge in the number of meta-analyses published on this subject since 2020[1,34,47,48]. While a majority of the older meta-analyses failed to show any major benefit of PRP therapy in this cohort of patients, more recent studies seem to re-iterate the potential benefits of adjuvant PRP treatment as evident from Figure 2. Older age, number of tendons involved, large tear size, duration of pre-operative symptoms and degree of pre-operative fatty degeneration have been postulated as some of the major factors predictive of high post-operative re-tear rates[32]. Table 6 discusses in detail the observations of each of these meta-analyses and enlists the reasons put forth by authors on the need for performing an additional meta-analysis in the presence of multiple pre-existing studies in the literature.
Among all the initial meta-analyses, the study with an excellent quality of methodology and a larger sample size and minimal heterogeneity was published by Zhang et al[30] in 2013. This study also concluded that adjuvant PRPs could reduce the re-tear rates in small and medium-sized rotator cuff tears but not in massive or full-thickness tears. The meta-analyses by Li et al[33] (2014) and Zhao et al[34] (2014) incorporated a few more later-published RCTs. Both these studies did not reveal any major benefits of PRPs in terms of both clinical outcome scores and re-tear rates.
Warth et al[35] (2014) conducted a meta-regression analysis to evaluate the effect of 6 different co-variates (level of studies included, tear size, single- vs double-row repairs, types of PRP preparation, manual vs commercially available PRP preparations; and method of application of PRP) on overall clinical and structural outcome. They concluded that Constant scores were significantly improved when the PRPs were applied over the tendon-bone interface; and re-tears were significantly reduced in tears larger than 3 cm which were repaired using the double-row technique. In contrast, both the meta-analysis [Vavken et al[36]; Cai et al[38] (which included only RCTs)] published following this study revealed no benefit in large, full-thickness tears. In both these studies, PRPs enhanced healing rates only in small- to moderate-sized tears. Additionally, Vavken et al[36] concluded that despite its biological effectiveness; at the present costs, the use of PRPs is not a cost-effective strategy in arthroscopic repair of small- to moderate-sized RC tears. Another meta-analysis by Xiao et al[37] (2016) tried to enhance the power of the analysis by including both level I and II studies. Nevertheless, they too failed to reveal any major benefit in terms of both clinical outcome and re-tear rates. By being less selective in including studies for analysis, the quality of the meta-analysis also significantly deteriorated as compared to previous studies.
Between 2016 and 2018, many new RCTs were performed; and 4 new meta-analyses were published in 2018 and 2019 which included these recent studies as well. Hurley et al[40] (2018; involving 18 studies) compared PRP and platelet-rich fibrin (PRF) in ARCR. They concluded that PRPs improved pain score (short-term and long-term), Constant score and re-tear rates in RC tears of all sizes. Another similar study by Han et al[39] (involving 13 RCTs) also reported reduced re-tear rate and meliorated clinical outcome with PRP therapy in ARCR. Wang et al[41] (2019; included only 8 RCTs) observed good outcomes with PRPs when administered in ARCRs with a single-row technique. Chen et al[42] (2019) performed another higher quality meta-analysis (involving 18 level 1 studies) and concluded that long-term re-tear rates were significantly improved with PRP therapy. Additionally, the functional outcome scores (Constant score, UCLA score – at long- and short-terms) and VAS scores were better in the PRP-treated group. They also performed detailed sub-group analysis in 3 different categories and concluded that: a. Functional outcome measures were more significantly improved when multiple tendons were torn or ruptured, b. Leukocyte-rich PRP (LR-PRP) group had much better improvement in Constant scores as compared with LP-PRP, and c. Patients receiving gel-preparations of PRP had significantly greater Constant scores than their respective comparison groups. They also assessed the minimal clinically important differences (MCID) for these patient-related outcome (PRO) measures. It was concluded that although significant improvements were observed in multiple functional outcome measures in the PRP-treated patient group, none reached their respective MCID. They opined that despite a reasonable number of publications on this subject, limited data availability, substantial study heterogeneity and poor methodological quality hampered our ability to reach firm conclusions regarding PRPs.
Between 2020 and 2021, 7 new meta-analyses have been published on this topic. Owing to the availability of better quality, larger-scale RCTs over the recent years, these recent meta-analyses have been able to put forth stronger recommendations regarding the administration of PRPs. Cavendish et al[43] reported 16 RCTs and prospective trials (1045 participants), Hurley et al[44] included 13 RCTs (868 participants), Yang et al[45] analyzed 7 RCTs published between 2013 and 2018 (541 participants), Zhao et al[46] involved 10 RCTs (742 participants), Ryan et al[1] included 17 RCTs (1104 participants), Li et al[47] evaluated 23 RCTs (1440 patients) and Xu et al[48] studied 14 RCTs (923 patients). Hurley et al[44] analyzed RCTs comparing LP- or LR-PRP against controls, Zhao et al[46] evaluated studies involving LP-PRP, Ryan et al[1] evaluated 4 different types of PRPs (pure platelet-rich plasma [P-PRP], leukocyte and platelet-rich plasma, pure platelet-rich fibrin, and leukocyte and platelet-rich fibrin); and Li et al[47] analyzed RCTs comparing PRP or PRF to controls in ARCR. The remaining 3 studies included all RCTs evaluating the overall role of PRPs (with or without comparison to a control group)[43,45,48].
All the 7 recent meta-analyses support the role of PRPs in ARCR. Overall, based on their recommendations, PRPs are preferably delivered intra-operatively at the bone-tendon interface for the best possible outcome. Cavendish et al[43] reported that PRPs significantly reduce the failure rates after ARCR, irrespective of the size of tear. Xu et al[48] demonstrated substantially improved re-tear rates following intra-operative use of PRP in large- or massive-sized tears. Hurley et al[44] concluded that LP-PRP reduces re-tear, enhances healing potential and improves PRO, as compared with a control. Nevertheless, they could not make any strong recommendations regarding its superiority or inferiority as a biological augment, in comparison with LR-PRPs. Even in the meta-analysis by Zhao et al[46], LP-PRP was demonstrated to significantly reduce medium- and long-term post-operative re-tear rates in patients undergoing ARCR, irrespective of the size of tear and the technique of repair. Nevertheless, when defined in terms of MCID, the use of LP-PRP failed to reveal any clinically meaningful benefits in terms of post-operative VAS and PRO measures. Among the 4 different types of PRP employed, only P-PRP demonstrated statistically significant improvement in re-tear rate and Constant score. Theoretically, LP-PRP enhances the formation of normal collagen and mitigates the synthesis of inflammatory mediators. On the other hand, LR-PRP augments the cell catabolism and inflammatory response, both of which are not conducive for tendon healing. Therefore, in acute traumatic RC tears, use of LR-PRP may impair post-operative tissue healing. These recent meta-analyses also seem to indicate the superiority of LP-PRP (over LR-PRP) in ARCR[48]. Thus, despite multiple studies published on this topic, the literature is still unclear on whether the use of PRP is more beneficial in massive and full-thickness tears or smaller and partial thickness injuries[36,38,44,48]. A majority of the studies in the literature have also not clearly determined the correlation between the type of RC repair and the effect of PRP application[29-40,42-48]. However, two recent studies [Wang et al[41] (2019) and Yang et al[45] (2020)] have shown better outcome with PRP use following single-row RC repairs[6,41].
These recent studies have also cautioned regarding significant heterogeneity in the available preparations of PRPs, which leads to inconsistent outcome and difficulty in making strong recommendations in favor or against this treatment modality. Yang et al[45] demonstrated a significant decrease in re-tears as well as a substantial improvement in short-term pain severity (VAS) and short-term functional outcome (Constant and UCLA scores). In a sub-group analysis, they also demonstrated meliorated outcomes (in terms of VAS, functional scores and re-tear) in both single- and double-row repair groups. In a comparison study by Li et al[47] between PRP and PRF, PRP demonstrated significant improvement in pain, functional outcome and re-tears; while PRF only improved Constant score.
Although PRP has been considered as a minimally-invasive effective non-operative treatment methodology for partial RC tears[50], its utility as an adjuvant in the ARCR needs further refinement to preclude the heterogeneity in the results obtained and achieve consistent beneficial effects of the additive intervention performed. For example, role of repeat administration of PRP and utility of scaffolds as a medium of sustained delivery of the growth factors from the platelet concentrate may provide even more beneficial effects compared to the single direct use post-ARCR[51]. Although our systematic overview establishes the efficacy of PRP as an adjuvant to ARCR, there remains heterogeneity among the study results obtained due to the variability in the preparation and the utility of PRP. To clarify these aspects, blinded RCTs investigating the above-mentioned lacunae are required in the future.
This study has some limitations. The quality of the meta-analyses identified in our study were of Level I/II evidence due to the quality of the included primary studies in them. Hence, we were unable to provide a level I recommendation on the utility of PRP in ARCR with the existing literature. This systematic overview may be influenced by the limitations and biases involved in the meta-analyses and their primary studies. Moreover, selecting the meta-analysis of highest quality based on the Jadad algorithm generates recommendations based on the results of the selected meta-analysis at the cost of studies missed from their primary search as highlighted in Supplementary Table 1. Moreover, we identified many recent meta-analyses, apart from the meta-analysis selected through the Jadad algorithm, which had the power of the recent RCTs on the subject. Hence, we resorted to give collaborative documentation based on all the recent evidence though they lack the methodological robustness of the study identified by the Jadad algorithm thereby making the final level of recommendation that was achieved out of this study to be Level II. Heterogeneity was noted across the studies in terms of their methods of preparation, use of activators and method of application of PRP which could have accounted for the variability noted across the primary studies and the meta-analyses that included them into analysis.
Based on our systematic overview of the existing meta-analyses, we could observe that despite multiple publications on this subject over the past years, methodological quality of the included studies and heterogeneity in protocols employed across different individual trials continue to remain major impediments in clearly defining the role of PRPs in ARCR. Nevertheless, the recent meta-analysis published over the past 2 years to 3 years seems to indicate a clear benefit of intra-operative use of PRPs at the bone-tendon interface in terms of post-operative pain, functional outcome and re-tear rates (irrespective of the type of repair performed). Although the older studies supported its role in only small to moderate tears, recent studies indicate a definite benefit in tears of all sizes (including massive ones). Among the different preparations used, LP-PRP possibly offers the greatest benefit as a biological augment in these situations.
Platelet-rich plasma has been gaining popularity as an agent for biological augmentation either as the sole treatment modality or as an adjunct to surgical repair.
There is growing evidence on the positive effects of platelet-derived autologous growth factors on collagen production, cell proliferation, tissue revascularization and tendon regeneration thereby making them useful as an augment to arthroscopic rotator cuff repair.
The overall purpose of the current study was to perform a detailed systematic review of the existing meta-analyses evaluating the role of PRP in patients undergoing rotator cuff repair; and to specifically provide answers to the following research questions, namely: (1) To evaluate the effect of this strategy on overall clinical outcome scores; (2) To evaluate the reduction in re-tear or failure rates; (3) To analyze the evolution and variations in the techniques of procurement and application of PRP across different studies; (4) To critically analyze and interpret the best currently available evidence and provide recommendations; and (5) To discern the major gaps in the existing literature and identify the scope for future research on this subject.
We then utilized the Jadad decision algorithm to identify the study with the highest quality to represent the current best evidence to generate the recommendation.
Recent meta-analyses are more supportive of the role of intra-operative administration of PRPs at the bone-tendon interface in improving the overall healing and re-tear rates, functional outcome and pain. The initial size of the tear and type of repair performed do not seem to affect the benefit of PRPs. Among the different preparations used, leucocyte poor (LP)-PRP possibly offers the greatest benefit as a biological augment in these situations.
Based on this systematic overview, we give a Level II recommendation that intra-operative use of PRPs at the bone-tendon interface can augment the healing rate, reduce re-tears, enhance functional outcome and mitigate pain in patients undergoing arthroscopic rotator cuff repair.
LP-PRP possibly offers the greatest benefit in terms of healing rates as compared with other platelet preparations.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: India
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): D, D
Grade E (Poor): 0
P-Reviewer: Belluzzi E, Italy; Haque N, Bangladesh; Yang YZ, China; Zhang W, China; Zhu L, China S-Editor: Liu JH L-Editor: Filipodia P-Editor: Liu JH
| 1. | Ryan J, Imbergamo C, Sudah S, Kirchner G, Greenberg P, Monica J, Gatt C. Platelet-Rich Product Supplementation in Rotator Cuff Repair Reduces Retear Rates and Improves Clinical Outcomes: A Meta-analysis of Randomized Controlled Trials. Arthroscopy. 2021;37:2608-2624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 2. | Boileau P, Brassart N, Watkinson DJ, Carles M, Hatzidakis AM, Krishnan SG. Arthroscopic repair of full-thickness tears of the supraspinatus: does the tendon really heal? J Bone Joint Surg Am. 2005;87:1229-1240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 404] [Cited by in RCA: 526] [Article Influence: 26.3] [Reference Citation Analysis (0)] |
| 3. | Franceschi F, Ruzzini L, Longo UG, Martina FM, Zobel BB, Maffulli N, Denaro V. Equivalent clinical results of arthroscopic single-row and double-row suture anchor repair for rotator cuff tears: a randomized controlled trial. Am J Sports Med. 2007;35:1254-1260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 351] [Cited by in RCA: 308] [Article Influence: 17.1] [Reference Citation Analysis (0)] |
| 4. | Grasso A, Milano G, Salvatore M, Falcone G, Deriu L, Fabbriciani C. Single-row versus double-row arthroscopic rotator cuff repair: a prospective randomized clinical study. Arthroscopy. 2009;25:4-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 171] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 5. | Sugaya H, Maeda K, Matsuki K, Moriishi J. Repair integrity and functional outcome after arthroscopic double-row rotator cuff repair. A prospective outcome study. J Bone Joint Surg Am. 2007;89:953-960. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 355] [Cited by in RCA: 544] [Article Influence: 30.2] [Reference Citation Analysis (0)] |
| 6. | Saltzman BM, Jain A, Campbell KA, Mascarenhas R, Romeo AA, Verma NN, Cole BJ. Does the Use of Platelet-Rich Plasma at the Time of Surgery Improve Clinical Outcomes in Arthroscopic Rotator Cuff Repair When Compared With Control Cohorts? Arthroscopy. 2016;32:906-918. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 98] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 7. | P B, E W, A N, M K, T M, S D, W M. Microcirculation associated with degenerative rotator cuff lesions. In vivo assessment with orthogonal polarization spectral imaging during arthroscopy of the shoulder. J Bone Joint Surg Am. 2003;85 Accessed 26 November 2021. Available from: https://pubmed.ncbi.nlm.nih.gov/12637434/. |
| 8. | Thomopoulos S, Williams GR, Soslowsky LJ. Tendon to bone healing: differences in biomechanical, structural, and compositional properties due to a range of activity levels. J Biomech Eng. 2003;125:106-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 303] [Cited by in RCA: 277] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 9. | Fealy S, Adler RS, Drakos MC, Kelly AM, Allen AA, Cordasco FA, Warren RF, O'Brien SJ. Patterns of vascular and anatomical response after rotator cuff repair. Am J Sports Med. 2006;34:120-127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 96] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 10. | Randelli P, Arrigoni P, Ragone V, Aliprandi A, Cabitza P. Platelet rich plasma in arthroscopic rotator cuff repair: a prospective RCT study, 2-year follow-up. J Shoulder Elbow Surg. 2011;20:518-528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 332] [Cited by in RCA: 301] [Article Influence: 21.5] [Reference Citation Analysis (0)] |
| 11. | Castricini R, Longo UG, De Benedetto M, Panfoli N, Pirani P, Zini R, Maffulli N, Denaro V. Platelet-rich plasma augmentation for arthroscopic rotator cuff repair: a randomized controlled trial. Am J Sports Med. 2011;39:258-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 365] [Cited by in RCA: 333] [Article Influence: 23.8] [Reference Citation Analysis (0)] |
| 12. | Gulotta LV, Kovacevic D, Ehteshami JR, Dagher E, Packer JD, Rodeo SA. Application of bone marrow-derived mesenchymal stem cells in a rotator cuff repair model. Am J Sports Med. 2009;37:2126-2133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 237] [Cited by in RCA: 233] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 13. | Bielecki T, Dohan Ehrenfest DM. Platelet-rich plasma (PRP) and Platelet-Rich Fibrin (PRF): surgical adjuvants, preparations for in situ regenerative medicine and tools for tissue engineering. Curr Pharm Biotechnol. 2012;13:1121-1130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 77] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 14. | Malavolta EA, Gracitelli ME, Ferreira Neto AA, Assunção JH, Bordalo-Rodrigues M, de Camargo OP. Platelet-rich plasma in rotator cuff repair: a prospective randomized study. Am J Sports Med. 2014;42:2446-2454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 131] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 15. | Bava ED, Barber FA. Platelet-rich plasma products in sports medicine. Phys Sportsmed. 2011;39:94-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 31] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 16. | Beitzel K, Allen D, Apostolakos J, Russell RP, McCarthy MB, Gallo GJ, Cote MP, Mazzocca AD. US definitions, current use, and FDA stance on use of platelet-rich plasma in sports medicine. J Knee Surg. 2015;28:29-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 146] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 17. | Furlan AD, Malmivaara A, Chou R, Maher CG, Deyo RA, Schoene M, Bronfort G, van Tulder MW; Editorial Board of the Cochrane Back, Neck Group. 2015 Updated Method Guideline for Systematic Reviews in the Cochrane Back and Neck Group. Spine (Phila Pa 1976). 2015;40:1660-1673. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 424] [Cited by in RCA: 531] [Article Influence: 53.1] [Reference Citation Analysis (0)] |
| 18. | Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52948] [Cited by in RCA: 47187] [Article Influence: 2949.2] [Reference Citation Analysis (0)] |
| 19. | McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS Peer Review of Electronic Search Strategies: 2015 Guideline Statement. J Clin Epidemiol. 2016;75:40-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1398] [Cited by in RCA: 2989] [Article Influence: 332.1] [Reference Citation Analysis (0)] |
| 20. | Slobogean G, Bhandari M. Introducing levels of evidence to the Journal of Orthopaedic Trauma: implementation and future directions. J Orthop Trauma. 2012;26:127-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 38] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 21. | Shea BJ, Grimshaw JM, Wells GA, Boers M, Andersson N, Hamel C, Porter AC, Tugwell P, Moher D, Bouter LM. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol. 2007;7:10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2840] [Cited by in RCA: 2949] [Article Influence: 163.8] [Reference Citation Analysis (0)] |
| 22. | Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, Moher D, Tugwell P, Welch V, Kristjansson E, Henry DA. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3100] [Cited by in RCA: 5704] [Article Influence: 713.0] [Reference Citation Analysis (0)] |
| 23. | Sathish M, Eswar R. Systematic Reviews and Meta-Analysis in Spine Surgery-How Good Are They in Methodological Quality? Global Spine J. 2021;11:378-399. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 24. | Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39087] [Cited by in RCA: 46536] [Article Influence: 2115.3] [Reference Citation Analysis (3)] |
| 25. | Jadad AR, Cook DJ, Browman GP. A guide to interpreting discordant systematic reviews. CMAJ. 1997;156:1411-1416. [PubMed] |
| 26. | Ding F, Jia Z, Zhao Z, Xie L, Gao X, Ma D, Liu M. Total disc replacement versus fusion for lumbar degenerative disc disease: a systematic review of overlapping meta-analyses. Eur Spine J. 2017;26:806-815. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 39] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 27. | Fu BS, Jia HL, Zhou DS, Liu FX. Surgical and Non-Surgical Treatment for 3-Part and 4-Part Fractures of the Proximal Humerus: A Systematic Review of Overlapping Meta-Analyses. Orthop Surg. 2019;11:356-365. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 28. | Mascarenhas R, Chalmers PN, Sayegh ET, Bhandari M, Verma NN, Cole BJ, Romeo AA. Is double-row rotator cuff repair clinically superior to single-row rotator cuff repair: a systematic review of overlapping meta-analyses. Arthroscopy. 2014;30:1156-1165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 74] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 29. | Zhao Y, Yang S, Ding W. Unilateral versus bilateral pedicle screw fixation in lumbar fusion: A systematic review of overlapping meta-analyses. PLoS One. 2019;14:e0226848. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 30. | Zhang Q, Ge H, Zhou J, Cheng B. Are platelet-rich products necessary during the arthroscopic repair of full-thickness rotator cuff tears: a meta-analysis. PLoS One. 2013;8:e69731. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 41] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 31. | Moraes VY, Lenza M, Tamaoki MJ, Faloppa F, Belloti JC. Platelet-rich therapies for musculoskeletal soft tissue injuries. Cochrane Database Syst Rev. 2014;CD010071. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 83] [Cited by in RCA: 115] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 32. | Chahal J, Van Thiel GS, Mall N, Heard W, Bach BR, Cole BJ, Nicholson GP, Verma NN, Whelan DB, Romeo AA. The role of platelet-rich plasma in arthroscopic rotator cuff repair: a systematic review with quantitative synthesis. Arthroscopy. 2012;28:1718-1727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 127] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 33. | Li X, Xu CP, Hou YL, Song JQ, Cui Z, Yu B. Are platelet concentrates an ideal biomaterial for arthroscopic rotator cuff repair? Arthroscopy. 2014;30:1483-1490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 31] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 34. | Zhao JG, Zhao L, Jiang YX, Wang ZL, Wang J, Zhang P. Platelet-rich plasma in arthroscopic rotator cuff repair: a meta-analysis of randomized controlled trials. Arthroscopy. 2015;31:125-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 65] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 35. | Warth RJ, Dornan GJ, James EW, Horan MP, Millett PJ. Clinical and structural outcomes after arthroscopic repair of full-thickness rotator cuff tears with and without platelet-rich product supplementation: a meta-analysis and meta-regression. Arthroscopy. 2015;31:306-320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 109] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 36. | Vavken P, Sadoghi P, Palmer M, Rosso C, Mueller AM, Szoelloesy G, Valderrabano V. Platelet-Rich Plasma Reduces Retear Rates After Arthroscopic Repair of Small- and Medium-Sized Rotator Cuff Tears but Is Not Cost-Effective. Am J Sports Med. 2015;43:3071-3076. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 91] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 37. | Xiao W, Luo R, Sun J, Chen J, Ma Q, Cai X, Liu P. Efficacy and clinical outcomes of platelet-rich plasma for arthroscopic repair rotator cuff tears: a meta-analysis, 10. |
| 38. | Cai YZ, Zhang C, Lin XJ. Efficacy of platelet-rich plasma in arthroscopic repair of full-thickness rotator cuff tears: a meta-analysis. J Shoulder Elbow Surg. 2015;24:1852-1859. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 91] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 39. | Han C, Na Y, Zhu Y, Kong L, Eerdun T, Yang X, Ren Y. Is platelet-rich plasma an ideal biomaterial for arthroscopic rotator cuff repair? J Orthop Surg Res. 2019;14:183. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 36] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 40. | Hurley ET, Lim Fat D, Moran CJ, Mullett H. The Efficacy of Platelet-Rich Plasma and Platelet-Rich Fibrin in Arthroscopic Rotator Cuff Repair: A Meta-analysis of Randomized Controlled Trials. Am J Sports Med. 2019;47:753-761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 139] [Article Influence: 23.2] [Reference Citation Analysis (0)] |
| 41. | Wang C, Xu M, Guo W, Wang Y, Zhao S, Zhong L. Clinical efficacy and safety of platelet-rich plasma in arthroscopic full-thickness rotator cuff repair: A meta-analysis. PLoS One. 2019;14:e0220392. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 42. | Chen XT, Jones IA, Park C, Vangsness CT Jr. Use of Platelet-Rich Plasma for the Improvement of Pain and Function in Rotator Cuff Tears: Response. Am J Sports Med. 2020;48:NP39-NP41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 43. | Cavendish PA, Everhart JS, DiBartola AC, Eikenberry AD, Cvetanovich GL, Flanigan DC. The effect of perioperative platelet-rich plasma injections on postoperative failure rates following rotator cuff repair: a systematic review with meta-analysis. J Shoulder Elbow Surg. 2020;29:1059-1070. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 44. | Hurley ET, Colasanti CA, Anil U, Luthringer TA, Alaia MJ, Campbell KA, Jazrawi LM, Strauss EJ. The Effect of Platelet-Rich Plasma Leukocyte Concentration on Arthroscopic Rotator Cuff Repair: A Network Meta-analysis of Randomized Controlled Trials. Am J Sports Med. 2021;49:2528-2535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 45. | Yang FA, Liao CD, Wu CW, Shih YC, Wu LC, Chen HC. Effects of applying platelet-rich plasma during arthroscopic rotator cuff repair: a systematic review and meta-analysis of randomised controlled trials. Sci Rep. 2020;10:17171. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 46. | Zhao D, Han YH, Pan JK, Yang WY, Zeng LF, Liang GH, Liu J. The clinical efficacy of leukocyte-poor platelet-rich plasma in arthroscopic rotator cuff repair: a meta-analysis of randomized controlled trials. J Shoulder Elbow Surg. 2021;30:918-928. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 24] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 47. | Li Y, Li T, Li J, Tang X, Li R, Xiong Y. Platelet-Rich Plasma Has Better Results for Retear Rate, Pain, and Outcome Than Platelet-Rich Fibrin After Rotator Cuff Repair: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Arthroscopy. 2022;38:539-550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 26] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 48. | Xu W, Xue Q. Application of Platelet-Rich Plasma in Arthroscopic Rotator Cuff Repair: A Systematic Review and Meta-analysis. Orthop J Sports Med. 2021;9:23259671211016847. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 49. | Moja L, Fernandez del Rio MP, Banzi R, Cusi C, D'Amico R, Liberati A, Lodi G, Lucenteforte E, Minozzi S, Pecoraro V, Virgili G, Parmelli E. Multiple systematic reviews: methods for assessing discordances of results. Intern Emerg Med. 2012;7:563-568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 50. | El Gharbawy NH, Labib HS. Role of Platelet Rich Plasma (PRP) injection in treatment of rotator cuff tear. Egyptian Rheumatology and Rehabilitation. 2020;47:30. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 51. | Hitchen J, Wragg NM, Shariatzadeh M, Wilson SL. Platelet Rich Plasma as a Treatment Method for Rotator Cuff Tears. SN Compr Clin Med. 2020;2:2293-2299. [DOI] [Full Text] |