Published online Jun 28, 2022. doi: 10.13105/wjma.v10.i3.122
Peer-review started: March 15, 2022
First decision: April 13, 2022
Revised: May 11, 2022
Accepted: June 24, 2022
Article in press: June 24, 2022
Published online: June 28, 2022
Processing time: 112 Days and 0.2 Hours
Regarded as a minimally invasive procedure, endoscopic retrograde cholangiopancreatography (ERCP) is commonly used to manage various pancreaticobiliary disorders. The rate of complications is low and starts from 4% for diagnostic interventions. The group of most frequent negative outcomes is commonly known and includes pancreatitis, cholecystitis, and hemorrhage. Rare adverse effects occur occasionally but carry a significant risk of unexpected and potentially dangerous results. In some cases, including splenic injury, the knowledge of pre-existing conditions might be helpful in avoiding the unwanted outcome, while in others, the risk factors are not clearly defined. Such situations demand increased caution in the post-ERCP period. The appearance of abdominal pain, peritoneal symptoms, or instability of the patient’s hemodynamic condition should alert the physician and lead to further investigation of the possible causes. The diagnostic process usually involves imaging tests. The implementation of the appropriate treatment should be immediate, as many of the rare complications carry the risk of dangerous, even potentially lethal, results.
Core Tip: Endoscopic retrograde cholangiopancreatography is a common procedure used to manage pancreaticobiliary disorders. The group of most frequent complications is well described and includes pancreatitis, cholecystitis, and hemorrhage. Rare adverse effects occur occasionally but carry a significant risk of unexpected and potentially dangerous results. In some cases, the knowledge of pre-existing conditions might be helpful in avoiding the unwanted outcome, while in others, the risk factors are not clearly defined. Such situations demand increased caution in the post-procedure period. Physicians should be alerted by symptoms of abdominal pain or instability of patient’s condition, investigate further for possible causes, and be ready to implement the appropriate treatment immediately.
- Citation: Przybysz MA, Stankiewicz R. Rare post-endoscopic retrograde cholangiopancreatography complications: Can we avoid them? World J Meta-Anal 2022; 10(3): 122-129
- URL: https://www.wjgnet.com/2308-3840/full/v10/i3/122.htm
- DOI: https://dx.doi.org/10.13105/wjma.v10.i3.122
Endoscopic retrograde cholangiopancreatography (ERCP) is nowadays a common procedure used to manage various pancreaticobiliary disorders, including bile duct stones, malignant obstructions, and strictures. Regarded as a minimally invasive procedure, diagnostic ERCP is a technique with a low complication rate starting from 4%, though significantly rising up in cases of a therapeutic procedure[1,2]. The most common complications include pancreatitis (1.7%-4.9%), hemorrhage (1.2%-4.5%), and cholangitis (0.6%-2.3%)[3,4]. A history of previous pancreatitis and cholecystitis has been a well-documented risk factor for post-ERCP pancreatitis (PEP) and post-ERCP cholecystitis (PEC)[5,6], while pre-cut sphincterotomy increases the risk of post-ERCP hemorrhage[7].
The group of less common post-ERCP adverse effects is diverse and heterogeneous, which makes it much more difficult to predict and, therefore, manage. Unexpected complications might be a result of the introduction of the endoscope itself or of its accessories (i.e., a variety of splenic and hepatic injuries, impaction of the stone retrieval basket or stent migration, and colonic or small bowel perforation), might be due to the air leakage (localized or systemic embolism and pneumothorax), might be caused by an allergic reaction to the contrast, or might as well be the consequence of existing comorbid diseases (i.e. cardiopulmonary events and sedation-related adverse effects). The uncommon post-ERCP complications occur significantly less often than PEP or PEC. The Italian systematic review presents a rate of 1.3%, with a mortality rate of 0.07% (12973 patients with a total of 173 rare adverse effects and 9 deaths)[8]. While the occurrence of miscellaneous complications seems low and insignificant, it tends to extend the length of the patient’s hospitalization, might result in surgical interventions and, possibly – in rare cases – causes death. Therefore, the awareness of its existence is crucial in order to recognize the problem, manage it properly, and avoid the possible negative outcomes.
Commonly known adverse effects, such as PEP, had been already analyzed thoroughly from multiple points of view. This review focuses on the rare post-ERCP complications, mostly those directly connected to the technical aspects of the procedure, especially the ones requiring a surgical intervention. We take a closer look at some of the possibly severe final outcomes and discuss potential strategies of prevention and management. In order to present the subject in a clear manner, the various post-ERCP complications have been divided into minor groups.
While splenic injuries as a result of colonoscopy are well documented, cases of post-ERCP splenic injuries remain rare. The severity of possible negative outcomes varies, but even though they are not common, they can potentially be lethal[9]. Possible risk factors for this uncommon complication include chronic pancreatitis, as the calcified ligaments stiffen and decrease the mobility of the organs[10]. Another presumed mechanism of the complication might be the bowing of the endoscope with torsion of the greater curvature while cannulating the papilla[11]. Postoperative adhesions due to prior surgical abdominal interventions might also lead to splenic injury, as they decrease the mobility between the spleen and other organs[12].
According to the American Association for the Surgery of Trauma, splenic injury can be graded depending on the severity of the damage. Table 1 shows the American Association for the Surgery of Trauma: Splenic injury grading scale[13].
| GRADE I | Laceration < 1 cm; Subcapsular hematoma < 10% of the surface area |
| GRADE II | Laceration 1-3 cm; Subcapsular hematoma 10%-50% of the surface area |
| GRADE III | Laceration > 3 cm; Subcapsular hematoma > 50% of the surface area; Ruptured subcapsular or parenchymal hematoma |
| GRADE IV | Segmental or hilar vascular injury; Devascularization > 25% of the spleen |
| GRADE V | Hilar injury; Shattered spleen |
Post-ERCP splenic injury was first reported in 1989 by Trondsen et al[14]. The case considered a 46-year-old female patient who underwent ERCP with sphincterotomy which resulted, 15 h later, in splenectomy due to the decapsulated spleen. Although most of the post-ERCP splenic injuries require a surgical procedure, in less severe cases, such as subcapsular hematomas[15], peri-splenic hematomas[11], or splenic abscess[16], the management might be conservative.
One of the latest reports on the subject presents a non-surgical approach to the post-ERCP spleen injury. Bajwa et al[17] reported the case of an 83-year-old woman who underwent ERCP procedure with sphincterotomy which resulted in forming a grade 3 splenic laceration with intraparenchymal and subcapsular hematoma and moderate peritoneal free fluid. As the patient was hemodynamically stable with no signs of peritoneal symptoms, the management remained conservative. Splenectomy becomes a procedure of choice in more severe cases including a rupture of the spleen[18] or an avulsion of the short gastric vessels[12]. The decision should consider the dynamics of the patient’s condition as they do not always present with acute abdomen and the onset of the symptoms might often be delayed. As the pain in the upper left abdomen is not always accompanied by signs of peritoneal irritation or significant decrease of hemoglobin levels, it should itself be considered a strong premise to diagnose the possible causes. All the reports on the subject acknowledge that a fast response in those cases is crucial for properly managing the issue.
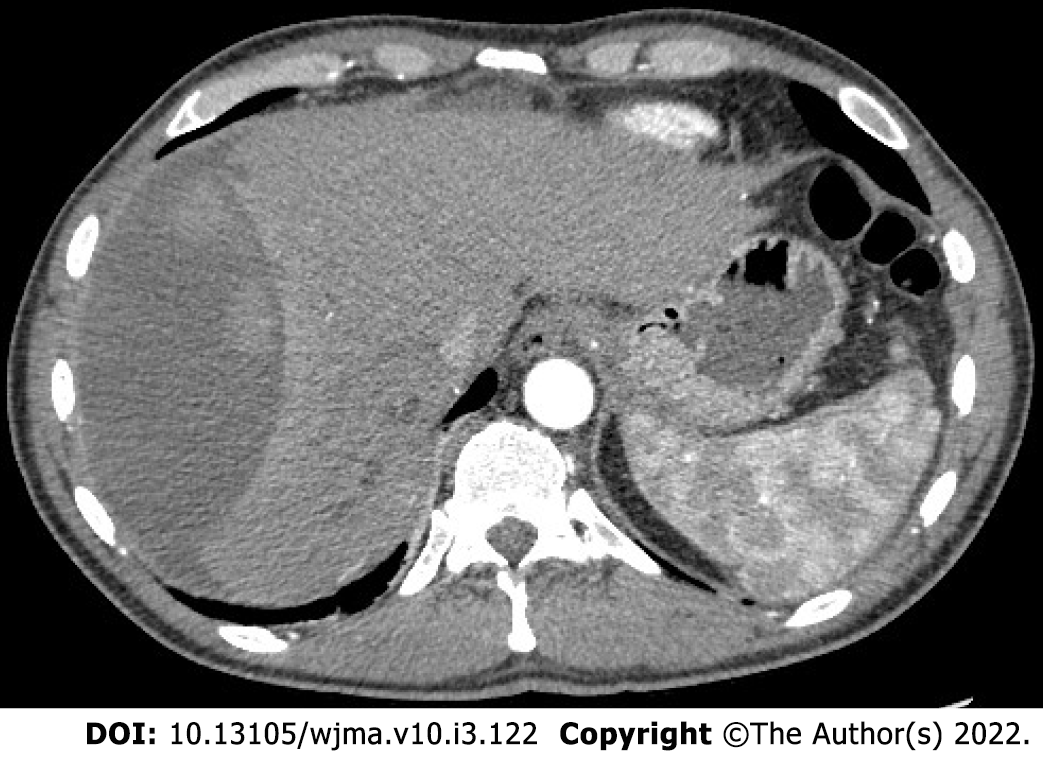
Subcapsular hepatic hematoma is an incidental but potentially dangerous complication. The pathological mechanism of this unique event might be explained by accidental puncture and laceration of small parenchymal vessels by an endoscopic guide wire[19] (Figure 1).
Subcapsular hepatic hematoma as a post-ERCP complication was first presented in 2000 by Ortega et al[20]. ERCP was performed on an 81-year-old man due to choledocholithiasis. Following the procedure, the patient presented abdominal pain and a computed tomography (CT) scan revealed a hepatic hematoma. Drainage was the management chosen in this case, with a catheter left for 3 wk after the puncture. According to Pivetta et al[21], a total of 61 cases were reported worldwide as for the year 2020.
The latest case, not included in the Pivetta report, presented by Petrucci et al[22], considers a 43-year-old woman who underwent ERCP for stent removal. The abdominal pain in the right upper quadrant appeared the following day and a CT scan revealed a subcapsular hepatic hematoma affecting most of the right lobe. The management was conservative at first, but as the pain reappeared accompanied by fever, the patient underwent series of procedures, including interventional radiology guided drainage, laparoscopic washout, and laparotomy with necrosectomy of the liver capsule.
Subcapsular hepatic hematoma should be considered in case of post-ERCP clinical symptoms such as persistent abdominal pain, peritoneal symptoms, and hypotension. Although significant, the laboratory test results should not be considered as main indicators of this complication, except for a decrease of haematocrit and haemoglobin levels. Imaging, such as computed tomography and ultrasound, is a helpful tool to confirm the diagnosis and evaluate the necessity of a surgical intervention[23]. With various possibilities of action, a decision must be made based on the clinical and hemodynamic status of the patient. In most cases concerning hemodynamically stable patients, a conservative management is the treatment of choice. This includes the use of prophylactic antibiotics due to the risk of an infection of the hematoma, and continuing the monitoring of the patient’s hemodynamic status[24]. In the event of instability of the patient’s status, a more invasive treatment should be introduced. Procedures such as selective embolization of a branch of the hepatic artery or percutaneous drainage of the hematoma might be helpful in cases of active bleeding and decrease of haemoglobin and haematocrit levels[25]. In rare situations of advanced hematoma with haemorrhage, surgical intervention in the form of laparotomy drainage with haemostasis must be considered after analysis of the patient’s hemodynamic and clinical status[26,27]. In those cases, it is necessary to monitor the patient in the postoperative period with instruments such as computed tomography or ultrasound.
According to the studies performed in the last decade, the incidence of ERCP-related perforation ranges from 0.08% to 0.7%, with endoscopic sphincterotomy and guidewire injury being the most assumed etiologies[28,29]. Suggested risk factors associated with post-ERCP duodenal perforation include biliary stricture dilatation, sphincterotomy, sphincter of Oddi dysfunction, and common bile duct dilation. Patients with surgically altered anatomy (i.e., due to the previous Billroth II or Roux-en-Y operation) are at higher risk of bowel perforation[30].
ERCP-related perforations can be divided into four different types, according to the cause mechanism and the need of a surgical intervention. Types of ERCP-related perforations according to Stapfer et al[31] are shown in Table 2.
| TYPE I | Perforation of the lateral/medial duodenal wall, caused by the endoscope. It usually results in a large leak and requires immediate surgical treatment |
| TYPE II | Sphincterotomy related periampullary perforations of various severity. |
| TYPE III | Bile duct or duodenal perforation caused by migrating stents or biliary baskets presenting with a smaller-size leakage |
| TYPE IV | Guide-wire related perforation with retroperitoneal air present in the X-ray. It usually does not require surgical intervention |
In terms of prevention, it is crucial to recognize the risk factors before the procedure. Complicated cases should be handled by skillful and experienced endoscopists. Patients with a history of previous surgical anatomy alterations might be considered for “endoscopic scanning” in order to evaluate the conditions before the main procedure. A balloon dilatation over the guidewire might be helpful in preparing the way for a duodenoscope into the strictures[32]. Type II perforations can be avoided by a cautiously performed sphincterotomy with stepwise incisions.
Surgery is usually required in cases of type I or type II perforations, though the decision should be made taking into account the clinical state of the patient and the severity of the leak. Endoscopic treatment is possible for smaller-range perforations where endoloop application combined with clipping or placing a covered metal stent prevents the need of a surgical intervention[33,34]. Type III duodenal perforations, including the ones related to the migration of the stents, can also be treated with endoscopic clipping[35].
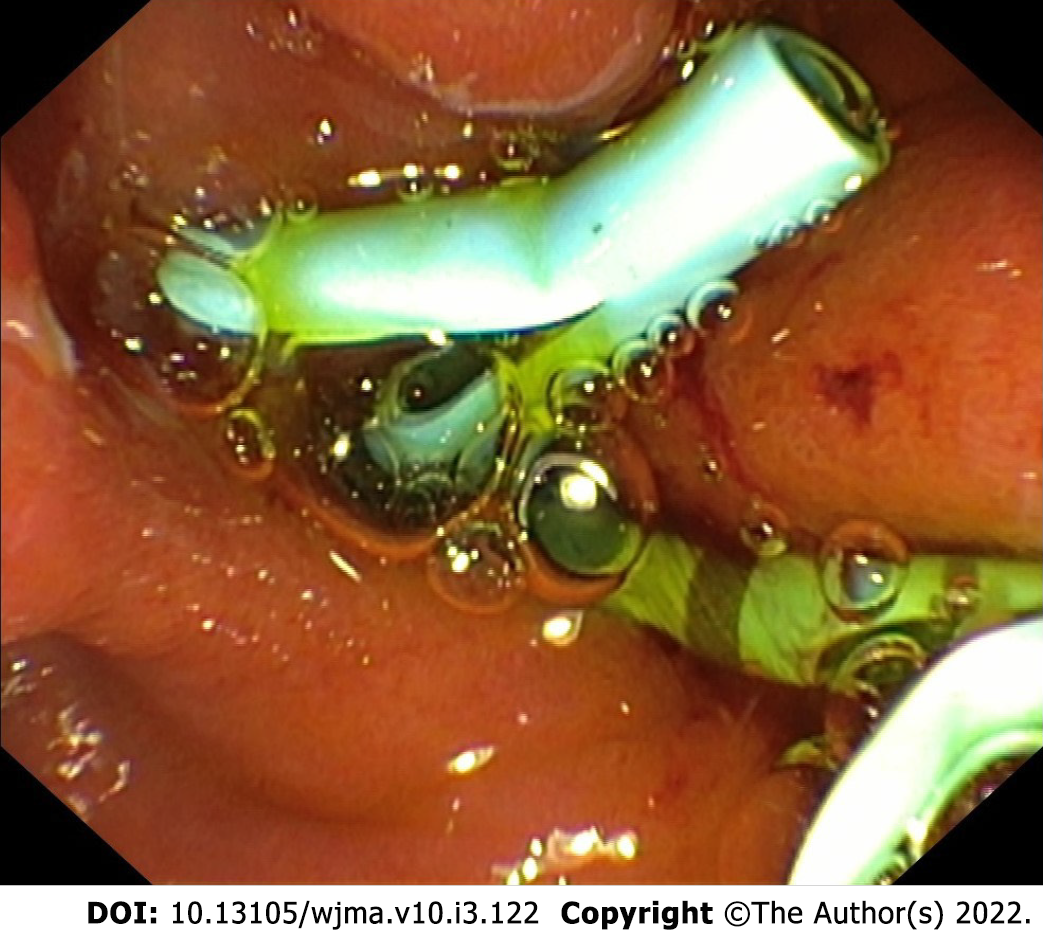
Occlusion is one of the most common complications resulting from inserting plastic or metal biliary and pancreatic stents during the procedure of ERCP. In cases of malignant strictures, this rather late negative outcome is a result of the progression of the primary disease[36]. The group of rare complications related to stenting include migration, misplacement, and dislodgement, with the latter resulting, in some cases, in intestinal hemorrhage[37,38] (Figure 2).
Patients undergoing endoscopic stent placement are at a risk of stent migration in approximately 3.5%, with the risk factors including bile duct benign stenosis, stenosis of the lower bile duct, and bile duct diameter being less than 10 mm[39]. A migrating stent can lead to the formation of different types of fistulas, such as bronchobiliary, bile duct-duodenum, and pancreatic-gastric[40,41]. Other possible and less common complications due to a migrating stent include the previously mentioned perforation of the duodenum and further parts of the gut.
An example of a duodenum injury caused by a migrating stent can be found in a recent case reported by Perez et al[42], considering a young female who underwent ERCP stenting due to hepatobiliary tuberculosis. Due to severe abdominal pain, the patient underwent a laparotomy with peritoneal lavage and tube jejunostomy. The operation confirmed a duodenal perforation from a biliary stent migration. The complication led to bacterial peritonitis resulting in a septic shock and the death of the patient. In another case of a migrating stent, described by Paikos et al[43], a patient diagnosed with cholangiocarcinoma required ERCP due to the progressive obstructive jaundice. The procedure involved placement of a plastic stent. Nevertheless, the jaundice persisted despite the procedure. The second ERCP revealed an active ulcer of the duodenum with the stent trapped in it. The patient’s condition rapidly worsened, resulting in respiratory arrest and heart failure.
The conventional treatment for choledocholithiasis includes papillotomy and extracting the stones with a Dormia basket. Removal of larger stones might require additional techniques in which the stone is mechanically fragmented before the extraction[44]. Lithotripsy is effective in 79%-92% of the choledocholithiasis cases[45,46] with the success of the procedure depending mostly on the stone size/bile duct size ratio[47]. One of the rare complications that might occur during the procedure is the impaction of the biliary basket, with a incidence rate of 0.26%[4]. The point of the impaction is usually located at the ampulla but it may also be localized in the main pancreatic duct or the intrahepatic ducts[48,49].
The retrieval of the basket might become impossible due to different reasons, not only the size of the deposit. The calcification of the stone causes its hardening to the point where a lithotriptor is unable to crush it. Cases like this require surgical management, such as choledochomy with cholecystectomy[50]. In rare situations, the extraction of the basket might not be possible via choledochotomy and duodenotomy, and must be performed during an emergency operation[51]. Laparoscopic management of impacted Dormia baskets has been presented in a few reports describing common bile duct exploration with choledochoscope and retrieving the trapped basket with a grasper or another biliary basket[52,53].
Rare post-ERCP complications have a low incidence rate but should not be underestimated, since the possible outcomes might be unpredictable. It is important to be aware of the uncommon adverse effects and their clinical presentation in order to diagnose the problem as soon as possible, and implement the relevant treatment. Are we able to avoid those infrequent complications completely though?
The prevention starts before the ERCP procedure itself by acknowledging the risk factors and recognizing cases more exposed to rare, but potentially dangerous incidents. This relates especially to patients with a history of previous abdominal operations (adhesions as a risk factor of splenic injury, and prior Billroth II procedure increasing the risk of post-ERCP bowel perforation)[12,30]. In demanding cases, procedures should be carefully performed by experienced and skillful endoscopists with expertise in the matter[54]. Technical difficulties, though challenging, can be overcome by choosing an appropriate approach, suitable for the specific problem. As most of the rare complications are unexpected, it is very important to pay close attention to the patient’s post-ERCP condition and hemodynamic status. In cases of a splenic or hepatic injury, manifestations such as abdominal pain in the left or right upper quadrant, respectively, indicate the need for further investigation, especially when combined with peritoneal symptoms and decrease of the haemoglobin level[18,23]. When unexpected complications occur, a decision needs to be made on whether the management of the problem should be conservative or surgical, and the physician must be prepared to adopt adequate treatment immediately.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Poland
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Kim KH, South Korea; Spadaccini M, Italy A-Editor: Wang JL, United States S-Editor: Liu JH L-Editor: Wang TQ P-Editor: Liu JH
| 1. | Loperfido S, Angelini G, Benedetti G, Chilovi F, Costan F, De Berardinis F, De Bernardin M, Ederle A, Fina P, Fratton A. Major early complications from diagnostic and therapeutic ERCP: a prospective multicenter study. Gastrointest Endosc. 1998;48:1-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 801] [Cited by in RCA: 779] [Article Influence: 28.9] [Reference Citation Analysis (1)] |
| 2. | Christensen M, Matzen P, Schulze S, Rosenberg J. Complications of ERCP: a prospective study. Gastrointest Endosc. 2004;60:721-731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 305] [Cited by in RCA: 299] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 3. | Masci E, Toti G, Mariani A, Curioni S, Lomazzi A, Dinelli M, Minoli G, Crosta C, Comin U, Fertitta A, Prada A, Passoni GR, Testoni PA. Complications of diagnostic and therapeutic ERCP: a prospective multicenter study. Am J Gastroenterol. 2001;96:417-423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 625] [Cited by in RCA: 613] [Article Influence: 25.5] [Reference Citation Analysis (0)] |
| 4. | Katsinelos P, Lazaraki G, Chatzimavroudis G, Gkagkalis S, Vasiliadis I, Papaeuthimiou A, Terzoudis S, Pilpilidis I, Zavos C, Kountouras J. Risk factors for therapeutic ERCP-related complications: an analysis of 2,715 cases performed by a single endoscopist. Ann Gastroenterol. 2014;27:65-72. [PubMed] |
| 5. | Ding X, Zhang F, Wang Y. Risk factors for post-ERCP pancreatitis: A systematic review and meta-analysis. Surgeon. 2015;13:218-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 98] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 6. | Cao J, Peng C, Ding X, Shen Y, Wu H, Zheng R, Wang L, Zou X. Risk factors for post-ERCP cholecystitis: a single-center retrospective study. BMC Gastroenterol. 2018;18:128. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 30] [Article Influence: 4.3] [Reference Citation Analysis (1)] |
| 7. | Ye X, Zhang Y, Wan X, Deng T. Analysis of Risk Factors in Endoscopic Retrograde Cholangiopancreatography-Related Immediate and Delayed Hemorrhage. Dig Dis Sci. 2021;66:4467-4474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Andriulli A, Loperfido S, Napolitano G, Niro G, Valvano MR, Spirito F, Pilotto A, Forlano R. Incidence rates of post-ERCP complications: a systematic survey of prospective studies. Am J Gastroenterol. 2007;102:1781-1788. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 669] [Cited by in RCA: 772] [Article Influence: 42.9] [Reference Citation Analysis (0)] |
| 9. | Kingsley DD, Schermer CR, Jamal MM. Rare complications of endoscopic retrograde cholangiopancreatography: two case reports. JSLS. 2001;5:171-173. [PubMed] |
| 10. | Gaffney RR, Jain V, Moyer MT. Splenic Injury and ERCP: A Possible Risk for Patients with Advanced Chronic Pancreatitis. Case Rep Gastroenterol. 2012;6:162-165. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Lee R, Huelsen A, Saad N, Hodgkinson P, Hourigan LF. Splenic Injury Following Endoscopic Retrograde Cholangiopancreatography: A Case Report and Literature Review. Case Rep Gastroenterol. 2017;11:241-249. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | Zyromski NJ, Camp CM. Splenic injury: a rare complication of endoscopic retrograde cholangiopancreatography. Am Surg. 2004;70:737-739. [PubMed] |
| 13. | Moore EE, Cogbill TH, Jurkovich GJ, Shackford SR, Malangoni MA, Champion HR. Organ injury scaling: spleen and liver (1994 revision). J Trauma. 1995;38:323-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 872] [Cited by in RCA: 762] [Article Influence: 25.4] [Reference Citation Analysis (0)] |
| 14. | Trondsen E, Rosseland AR, Moer A, Solheim K. Rupture of the spleen following endoscopic retrograde cholangiopancreatography (ERCP). Case report. Acta Chir Scand. 1989;155:75-76. [PubMed] |
| 15. | Lo AY, Washington M, Fischer MG. Splenic trauma following endoscopic retrograde cholangiopancreatography (ERCP). Surg Endosc. 1994;8:692-693. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 20] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 16. | Bajwa KS, Madabhushi AK, Jafri N, Shah SK, Felinski MM. Splenic Hematoma as a Rare Complication of Endoscopic Retrograde Cholangiopancreatography. J Clin Gastroenterol Treat. 2020;4:078. [DOI] [Full Text] |
| 17. | Luke JL, Reay DT. The perils of investigating and certifying deaths in police custody. Am J Forensic Med Pathol. 1992;13:98-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 34] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 18. | Grammatopoulos A, Moschou M, Rigopoulou E, Katsoras G. Splenic injury complicating ERCP. Ann Gastroenterol. 2014;27:177-178. [PubMed] |
| 19. | Chi KD, Waxman I. Subcapsular hepatic hematoma after guide wire injury during endoscopic retrograde cholangiopancreatography: management and review. Endoscopy. 2004;36:1019-1021. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 20] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 20. | Ortega Deballon P, Fernández Lobato R, García Septiem J, Nieves Vázquez MA, Martínez Santos C, Moreno Azcoita M. Liver hematoma following endoscopic retrograde cholangiopancreatography (ERCP). Surg Endosc. 2000;14:767. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 21. | Pivetta LGA, da Costa Ferreira CP, de Carvalho JPV, Konichi RYL, Kawamoto VKF, Assef JC, Ribeiro MA. Hepatic subcapsular hematoma post-ERCP: Case report and literature review. Int J Surg Case Rep. 2020;72:219-228. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 22. | Petrucci R, Das A. Subcapsular Hepatic Hematoma Post-Endoscopic Retrograde Cholangiopancreatography Requiring Surgical Necrosectomy. J Med Cases. 2021;12:186-189. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 23. | Klímová K, Suárez C, Asanza C, Peña A, Arregui E, Alonso A. Subcapsular Hepatic Hematoma after ERCP: A Case Report and Revision of Literature. Case Reports in Clinical Medicine. 2014;3:161-166. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 24. | Del Pozo D, Moral I, Poves E, Sanz C, Martín M. Subcapsular hepatic hematoma following ERCP: case report and review. Endoscopy. 2011;43 Suppl 2 UCTN:E164-E165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 25. | Fei BY, Li CH. Subcapsular hepatic haematoma after endoscopic retrograde cholangiopancreatography: an unusual case. World J Gastroenterol. 2013;19:1502-1504. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 30] [Cited by in RCA: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 26. | Priego P, Rodríguez G, Mena A, Losa N, Aguilera A, Ramiro C, Lisa E, Conde S, Fresneda V. [Subcapsular liver hematoma after ERCP]. Rev Esp Enferm Dig. 2007;99:53-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 27. | Pérez-Legaz J, Santos J, Ruiz-Tovar J, Moya-Forcén P, Armañanzas L, Gómez M, Oller I, Arroyo A, Calpena R. Subcapsular hepatic hematoma after ERCP (endoscopic retrograde cholangipancreatography). Rev Esp Enferm Dig. 2011;103:550-551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 28. | Dubecz A, Ottmann J, Schweigert M, Stadlhuber RJ, Feith M, Wiessner V, Muschweck H, Stein HJ. Management of ERCP-related small bowel perforations: the pivotal role of physical investigation. Can J Surg. 2012;55:99-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 32] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 29. | Assalia A, Suissa A, Ilivitzki A, Mahajna A, Yassin K, Hashmonai M, Krausz MM. Validity of clinical criteria in the management of endoscopic retrograde cholangiopancreatography related duodenal perforations. Arch Surg. 2007;142:1059-1064. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 41] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 30. | Enns R, Eloubeidi MA, Mergener K, Jowell PS, Branch MS, Pappas TM, Baillie J. ERCP-related perforations: risk factors and management. Endoscopy. 2002;34:293-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 179] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 31. | Stapfer M, Selby RR, Stain SC, Katkhouda N, Parekh D, Jabbour N, Garry D. Management of duodenal perforation after endoscopic retrograde cholangiopancreatography and sphincterotomy. Ann Surg. 2000;232:191-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 242] [Cited by in RCA: 239] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 32. | Prachayakul V, Aswakul P. Endoscopic retrograde cholangiopancreatography-related perforation: Management and prevention. World J Clin Cases. 2014;2:522-527. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 17] [Cited by in RCA: 16] [Article Influence: 1.5] [Reference Citation Analysis (2)] |
| 33. | Kwon CI, Song SH, Hahm KB, Ko KH. Unusual complications related to endoscopic retrograde cholangiopancreatography and its endoscopic treatment. Clin Endosc. 2013;46:251-259. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 45] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 34. | Park WY, Cho KB, Kim ES, Park KS. A case of ampullary perforation treated with a temporally covered metal stent. Clin Endosc. 2012;45:177-180. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 35. | Nam HS, Kim GH, Kim DU, Choi MK, Yi YS, Hwang JM, Kim S. [A case of duodenal perforation caused by biliary plastic stent treated with approximation using endoclip and detachable snare]. Korean J Gastroenterol. 2011;57:129-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 36. | Gargouri D, Kochlef A, Ouekaa A, Elloumi H, Kilani A, Romani M, Kharrat J, Ghorbel A. [Biliary stent occlusion]. Tunis Med. 2010;88:462-466. [PubMed] |
| 37. | Nicholson AA, Martin DF. Misplacement of endoscopic biliary endoprostheses. Endoscopy. 1997;29:125-127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 38. | Wong SY, Ng FH. Lower intestinal hemorrhage due to a dislodged metallic stent. Endoscopy. 1997;29:407-408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 39. | Kawaguchi Y, Ogawa M, Kawashima Y, Mizukami H, Maruno A, Ito H, Mine T. Risk factors for proximal migration of biliary tube stents. World J Gastroenterol. 2014;20:1318-1324. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 27] [Cited by in RCA: 33] [Article Influence: 3.0] [Reference Citation Analysis (2)] |
| 40. | Hady HR, Baniukiewicz A, Luba M, Rogalski P, Dabrowski A, Dadan J. Bronchobiliary fistula as a complication after long-term stenting of hepatic ducts, applied by ERCP after hepatobiliary surgery due to hydatid cyst. Endoscopy. 2011;43 Suppl 2 UCTN:E178-E179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 41. | Heyries L, Desjeux A, Sahel J. Bile duct-duodenum and pancreatic-gastric fistulas: two exceptional complications of biliary and pancreatic stenting. Gastrointest Endosc. 1999;50:571-574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 42. | Perez AR, Del Mundo HJF, Viray BAG, Abon JC, Resurreccion DC. Duodenal perforation secondary to stent migration after ERCP for hepatobiliary tuberculosis: Case report of a lethal complication in a young patient. Int J Surg Case Rep. 2021;88:106510. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 43. | Paikos D, Gatopoulou A, Moschos J, Soufleris K, Tarpagos A, Katsos I. Migrated biliary stent predisposing to fatal ERCP-related perforation of the duodenum. J Gastrointestin Liver Dis. 2006;15:387-388. [PubMed] |
| 44. | Troncone E, Mossa M, De Vico P, Monteleone G, Del Vecchio Blanco G. Difficult Biliary Stones: A Comprehensive Review of New and Old Lithotripsy Techniques. Medicina (Kaunas). 2022;58. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 27] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 45. | Garg PK, Tandon RK, Ahuja V, Makharia GK, Batra Y. Predictors of unsuccessful mechanical lithotripsy and endoscopic clearance of large bile duct stones. Gastrointest Endosc. 2004;59:601-605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 93] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 46. | Shaw MJ, Mackie RD, Moore JP, Dorsher PJ, Freeman ML, Meier PB, Potter T, Hutton SW, Vennes JA. Results of a multicenter trial using a mechanical lithotripter for the treatment of large bile duct stones. Am J Gastroenterol. 1993;88:730-733. [PubMed] |
| 47. | Cipolletta L, Costamagna G, Bianco MA, Rotondano G, Piscopo R, Mutignani M, Marmo R. Endoscopic mechanical lithotripsy of difficult common bile duct stones. Br J Surg. 1997;84:1407-1409. [PubMed] |
| 48. | Cutler AF, Hassig WM, Schubert TT. Basket impaction at the pancreatic head. Gastrointest Endosc. 1992;38:520-521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 49. | Mutignani M, Gabbrielli A, Murali N, Perri V, Costamagna G. Novel methods of management of trapped dormia baskets in the pancreatic and biliary ducts. Endoscopy. 1997;29:129-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 50. | Fukino N, Oida T, Kawasaki A, Mimatsu K, Kuboi Y, Kano H, Amano S. Impaction of a lithotripsy basket during endoscopic lithotomy of a common bile duct stone. World J Gastroenterol. 2010;16:2832-2834. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 11] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 51. | Abu Shakra I, Bez M, Bickel A, Badran M, Merei F, Ganam S, Kassis W, Kakiashvili E. Emergency open surgery with a duodenotomy and successful removal of an impacted basket following a complicated endoscopic retrograde cholangiopancreatography procedure: a case report. J Med Case Rep. 2021;15:93. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 52. | Varshney VK, Sreesanth KS, Gupta M, Garg PK. Laparoscopic retrieval of impacted and broken dormia basket using a novel approach. J Minim Access Surg. 2020;16:415-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 53. | O'Brien JW, Tyler R, Shaukat S, Harris AM. Laparoscopic Common Bile Duct Exploration for Retrieval of Impacted Dormia Basket following Endoscopic Retrograde Cholangiopancreatography with Mechanical Failure: Case Report with Literature Review. Case Rep Surg. 2017;2017:5878614. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 54. | Aliperti G. Complications related to diagnostic and therapeutic endoscopic retrograde cholangiopancreatography. Gastrointest Endosc Clin N Am. 1996;6:379-407. [PubMed] |