Published online Feb 28, 2022. doi: 10.13105/wjma.v10.i1.12
Peer-review started: August 5, 2021
First decision: September 4, 2021
Revised: September 16, 2021
Accepted: December 31, 2021
Article in press: December 31, 2021
Published online: February 28, 2022
Processing time: 206 Days and 20.8 Hours
Despite the Middle East and North Africa (MENA) Region reported to have the highest prevalence of hepatitis C virus (HCV) globally, HCV infection levels in the majority of MENA countries remain inadequately characterized. Blood donor data have been previously used as a proxy to assess levels and trends of HCV in the general population, however, it is unclear how comparable these populations are in MENA and whether blood donors provide an appropriate proxy.
To delineate HCV epidemiology among blood donors and the general population in the MENA.
The data source was the systematically gathered MENA HCV Epidemiology Synthesis Project Database. Random-effects meta-analyses and meta-regressions were conducted. For comparison, analyses were conducted for Europe, utilizing the Hepatitis C Prevalence Database of the European Centre for Disease Prevention and Control.
One thousand two hundred and thirteen HCV antibody prevalence measures and 84 viremic rate measures were analyzed for MENA. Three hundred and seventy-seven antibody prevalence measures were analyzed for Europe. In MENA, pooled mean prevalence was 1.58% [95% confidence interval (CI): 1.48%–1.69%] among blood donors and 4.49% (95%CI: 4.10%–4.90%) in the general population. In Europe, pooled prevalence was 0.11% (95%CI: 0.10%–0.13%) among blood donors and 1.59% (95%CI: 1.25%–1.97%) in the general population. Prevalence in the general population was 1.72-fold (95%CI: 1.50–1.97) higher than that in blood donors in MENA, but it was 15.10-fold (95%CI: 11.48–19.86) higher in Europe. Prevalence was declining at a rate of 4% per year in both MENA and Europe [adjusted risk ratio: 0.96 (95%CI: 0.95–0.97) in MENA and 0.96 (95%CI: 0.92–0.99) in Europe]. Pooled mean viremic rate in MENA was 76.29% (95%CI: 67.64%–84.02%) among blood donors and 65.73% (95%CI: 61.03%–70.29%) in the general population.
Blood donor data provide a useful proxy for HCV infection in the wider population in MENA, but not Europe, and could improve HCV burden estimations and assess progress toward HCV elimination by 2030.
Core tip: We investigated hepatitis C virus (HCV) epidemiology among blood donors and the wider general population in Middle East and North Africa (MENA). For comparison, similar analyses were performed for Europe. Our results indicated that HCV antibody prevalence in the population of MENA and Europe appears to be declining by 4% per year. Blood donor data in MENA (but not in Europe) were found to provide a useful proxy for HCV infection levels and trends in the general population. Thus, the data can be utilized in HCV estimates and to assess, track and validate progress towards World Health Organization elimination goals for HCV.
- Citation: Mahmud S, Chemaitelly H, Alaama AS, Hermez JG, Abu-Raddad L. Hepatitis C virus among blood donors and general population in Middle East and North Africa: Meta-analyses and meta-regressions. World J Meta-Anal 2022; 10(1): 12-24
- URL: https://www.wjgnet.com/2308-3840/full/v10/i1/12.htm
- DOI: https://dx.doi.org/10.13105/wjma.v10.i1.12
In the Middle East and North Africa (MENA) an estimated 15 million individuals are chronically infected with hepatitis C virus (HCV), making it the global region most affected by HCV infection[1]. Left untreated, chronic HCV infection may lead to several morbidities, including liver cancer, fibrosis, and cirrhosis[2]. Prompted by development of highly efficacious direct-acting antivirals (DAAs), the World Health Organization (WHO) has set a global target to eliminate HCV as a public health problem by 2030[3].
Despite disproportionally high HCV infection levels in specific MENA countries, e.g., Egypt[4-7] and Pakistan[8-11], relative to global levels[1,12], only three countries in this region have conducted nationally representative population-based surveys[13-15]. HCV infection levels in the remaining countries remain inadequately characterized[1].
Blood donors have been used as a proxy population to provide a crude estimate of HCV infection levels in the general population[16,17]. However, in developed countries, such as the United States[18] and countries of the European Union[16], blood donors are not considered representative of the wider general population. In these countries, strict donor selection and blood safety regulations[19] have resulted in a large disparity in HCV infection levels between blood donors and the general populations. This raises two questions: How comparable are HCV infection levels between blood donors and the general population in MENA? Are blood donor data, which are readily available, thanks to blood screening, an appropriate proxy for the general population in this region?
In this context, objectives of this study were to delineate HCV epidemiology in blood donors and general populations in MENA, and to assess how representative blood donor data are of HCV antibody (Ab) prevalence in the general population of this region. The study was also conducted to infer programmatic implications on blood safety in the region. These objectives were accomplished through analyses of a large, systematically gathered database, including 2622 HCV Ab prevalence measures on 49.8 million individuals by: (1) Estimating the pooled mean prevalence among blood donors and in general populations (henceforth the general population); and (2) Identifying predictors and trends of prevalence in these populations and sources of between-study heterogeneity. We further conducted similar analyses for Europe, a region in which stringent donor selection and blood safety processes have been implemented[19], for comparison. We did so by utilizing a large systematically gathered database including 419 HCV Ab prevalence measures for 25.7 million individuals[20], to compare outcomes with results for MENA.
This study was conducted as part of the MENA HCV Epidemiology Synthesis Project[1], an ongoing project with the aim of delineating HCV epidemiology and informing key public health research, policy, and programming priorities in MENA. The source of data was the MENA HCV Epidemiology Synthesis Project Database[1]. The database included 685 HCV Ab prevalence measures on 46 634 214 blood donors and 528 measures on 2 358 944 individuals of the general population, such as pregnant women, healthy adults, and children. The database also included eight HCV viremic rate measures on 58 986 blood donors and 76 measures on 14 936 individuals of the general population. HCV viremic rate was defined as the proportion of those who had tested Ab positive that are subsequently confirmed to be chronically infected by testing positive for HCV RNA – the proportion of those HCV RNA positive among HCV Ab-positive individuals[21,22].
The database was populated through a series of systematic reviews for HCV infection across MENA that were previously conducted as part of this project[5,6,8,23-28]. All reviews followed a standardized methodology, and specific details such as literature search strategy, databases searched, and eligibility criteria can be found in each of these reviews[5,6,8,23-28]. The methodology used for these reviews was informed by the Cochrane Collaboration Handbook[29], and all findings were reported using the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA)[30]. Literature searches were conducted to identify primary data on HCV measures in international and national/regional databases, the MENA HIV/AIDS Epidemiology Synthesis Project Database[31,32], abstract archives of international conferences, and grey literature, including public health reports and routine data reporting. Literature searches were broad, with no language restrictions to ensure inclusiveness. All records reporting HCV measures after 1989, the year in which the virus was officially identified[33], were included in the reviews[5,6,8,23-28].
Blood donors are typically a diverse group with different rates of HCV Ab prevalence depending on the rigor of the donor selection process[19]. The vast majority of HCV Ab prevalence studies in MENA did not specify the type of blood donors, and therefore the term blood donors in the present analysis encompassed the different blood donor types, including regular voluntary nonremunerated donors, one-time voluntary nonremunerated donors, family replacement donors, and paid donors.
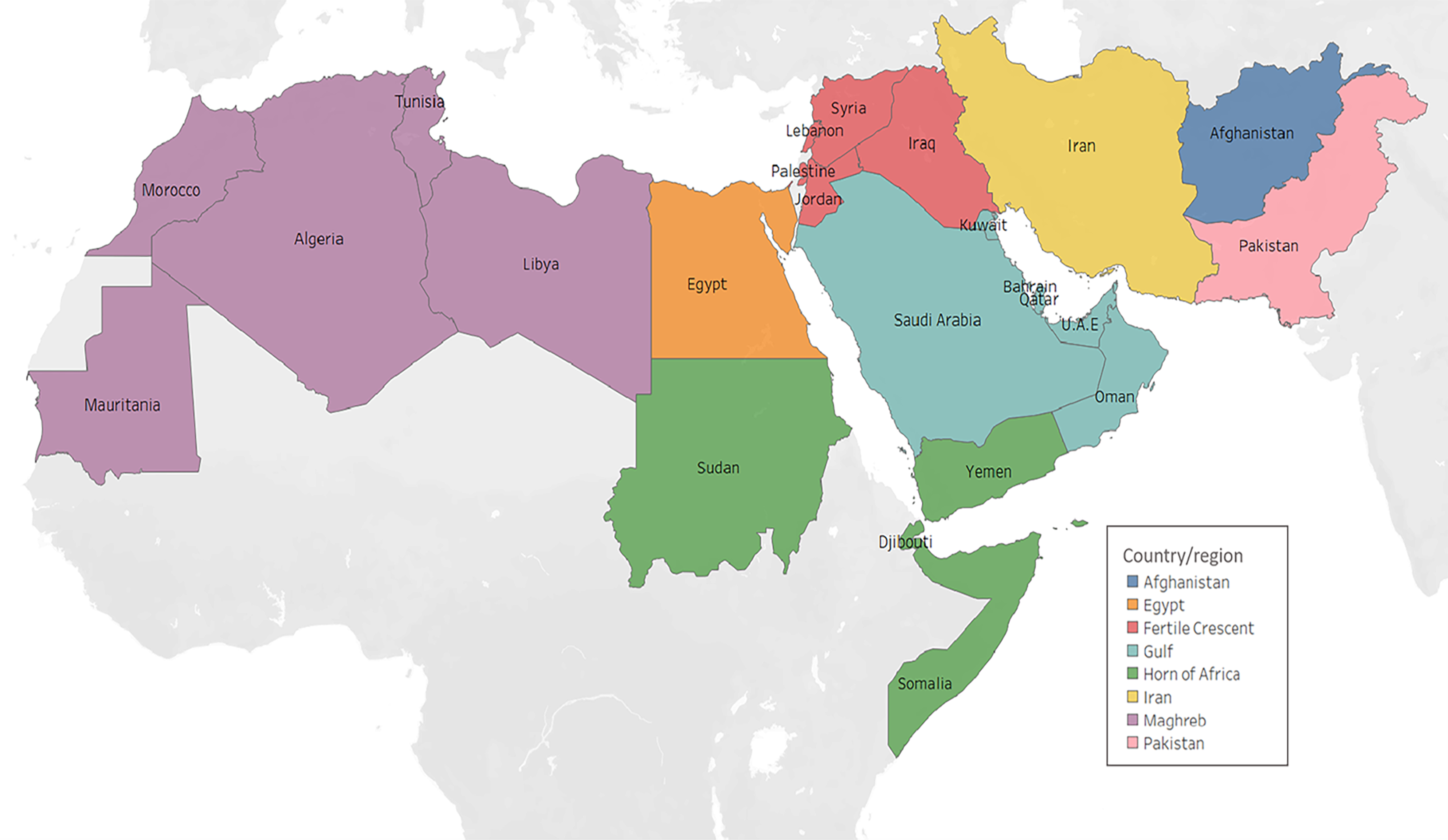
For the MENA HCV Epidemiology Synthesis Project, the MENA region was defined to include 24 countries (Figure 1). Given the distinctive nature of the HCV epidemics in Egypt[4-7] and Pakistan[8-11], relative to other MENA countries, separate analyses were performed for each of these countries.
HCV measures in blood donors and the general population were also analyzed for Europe, a region in which stringent donor selection and blood safety regulations have been implemented for decades[19], for comparison with MENA outcomes. Europe’s HCV Ab prevalence measures were retrieved from the Hepatitis C Prevalence Database of the European Centre for Disease Prevention and Control[20]. The database was populated through a systematic review[16] and multiple reports[34,35]. The database included 257 HCV Ab prevalence measures on 25 232 790 blood donors and 120 measures on 410 444 individuals of the general population, such as pregnant women and healthy adults.
Meta-analyses for countries and subregions were performed to pool HCV Ab prevalence in blood donors and the general population, whenever three or more measures were available, and a minimum sample size of 25 participants was met. Random-effects meta-analyses were performed using the DerSimonian–Laird method[36], with inverse-variance weighting to pool measures[36]. Freeman–Tukey type arcsine square-root transformation was used to stabilize the variance of each measure, factoring knowledge regarding the applicability of this transformation[37,38]. Heterogeneity was formally assessed[36]. Forest plots were generated and examined visually, and Cochran’s Q-test was conducted. Statistical significance of heterogeneity was indicated whenever P was < 0.10[36,39]. The I2 and its confidence interval (CI) were calculated to assess the percentage of variance that is explained by true differences in prevalence across studies, rather than chance[36]. Prediction intervals were also determined to describe the distribution of prevalence around the pooled mean estimate[36]. Meta-analyses were also used to estimate the pooled mean HCV viremic rate among blood donors and in the general population. Meta-analyses and forest plots were generated using R version 3.4.3.
Univariable and multivariable random-effects meta-regressions were conducted following established methodology[29]. A priori relevant independent variables in meta-regressions included subpopulation (blood donors vs the general population), country/subregion, and year of data collection. Factors associated with HCV Ab prevalence at P ≤ 0.20 in the univariable analysis qualified for inclusion in the multivariable analysis. Here, an adjusted relative risk (ARR) P ≤ 0.05 was considered to indicate strong evidence for an association.
In studies in which the year of data collection variable was missing, the variable was imputed. This was done by first subtracting the year of data collection (when available) from the year of publication for each study, and using the median of these values in imputing the year of data collection. Sensitivity analysis was performed without the imputed observations to determine the impact of the imputation on the results, confirming the results of the original meta-regression. Meta-regressions were performed on STATA version 13 using the metan command.
Studies on HCV Ab prevalence among blood donors and the general population in MENA are listed in Supplementary Tables 1 and 2. HCV Ab prevalence data were available for 23 of the 24 MENA countries. The largest number of data points were retrieved from Egypt, followed by the Gulf and Fertile Crescent Subregions. HCV Ab prevalence in blood donors ranged from 0 to 38.20%, with a median of 0.86% (Table 1). Studies reporting the highest HCV Ab prevalence were reported from parts of Egypt in the 1990s, a period during which HCV infection was widespread following the parenteral antischistosomal therapy (PAT) campaigns that contributed in a major way to the HCV epidemic in Egypt[5-7,40]. The pooled mean prevalence was 1.58% (95%CI: 1.48%–1.69%). It was lowest in the Fertile Crescent Subregion at 0.21% (95%CI: 0.18%–0.25%) and highest in Egypt at 10.40% (95%CI: 9.59%–11.23%), followed by Pakistan at 3.47% (95%CI: 2.96%–4.02%). HCV Ab prevalence in the general population ranged from 0 to 73.38%, with a median of 3.14%. The pooled mean prevalence was 4.49% (95%CI: 4.10%–4.90%). It was lowest in Iran at 0.33% (95%CI: 0.21%–0.47%) and highest in Egypt at 13.08% (95%CI: 11.51%–14.73%), followed by Pakistan at 8.81% (95%CI: 7.62%–10.06%). All outlier high HCV Ab prevalence measures were investigated and found to reflect blood donors or general populations in specific settings that were affected by high exposure to the virus, such as specific villages in the Nile delta in Egypt following the PAT era[5-7,40]. There was strong evidence for heterogeneity in HCV Ab prevalence in all meta-analyses (P < 0.01), with almost all variation being attributed to true variation in prevalence across studies rather than chance (I2 > 99.4%). Heterogeneity was also confirmed by the estimated prediction intervals (Table 1).
| Population | Studies | Samples | HCV Ab prevalence | Pooled HCV Ab prevalence | Heterogeneity measures | ||||
| Total (n) | Total (n) | Range (%) | Median (%) | Mean (%) | 95%CI | Q (P value)1 | I² (confidence limits)2 | Prediction interval (%)3 | |
| Blood donors | |||||||||
| Afghanistan | 40 | 737407 | 0.00-7.19 | 0.60 | 0.75 | 0.57-0.96 | 3046.03 (P < 0.01) | 98.7% (98.6%-98.9%) | 0.02-2.41 |
| Egypt | 116 | 1566669 | 0.00-38.20 | 10.97 | 10.40 | 9.59-11.23 | 24513.7 (P < 0.01) | 99.5% (99.5%-99.6%) | 3.64-19.96 |
| Fertile Crescent4 | 157 | 3488952 | 0.00-3.95 | 0.27 | 0.21 | 0.18-0.25 | 3674.2 (P < 0.01) | 95.8% (95.4%-96.1%) | 0.00-0.67 |
| Gulf5 | 156 | 20891379 | 0.00-27.19 | 0.89 | 0.78 | 0.71-0.86 | 29882.0 (P < 0.01) | 99.5% (99.5%-99.5%) | 0.20-1.69 |
| Horn of Africa6 | 22 | 48076 | 0.0-6.03 | 1.0 | 0.97 | 0.57-1.45 | 327.8 (P < 0.01) | 93.6% (91.5%-95.2%) | 0.00-3.78 |
| Iran | 73 | 15971802 | 0.00-3.13 | 0.24 | 0.31 | 0.22-0.40 | 55740.9 (P < 0.01) | 99.9% (99.9%-99.9%) | 0.00-1.43 |
| Maghreb7 | 49 | 2145044 | 0.11-6.58 | 0.65 | 0.68 | 0.49-0.91 | 13475.9 (P < 0.01) | 99.6% (99.6%-99.7%) | 0.00-2.82 |
| Pakistan | 73 | 1797644 | 0.01-20.79 | 3.00 | 3.47 | 2.96-4.02 | 24753.7 (P < 0.01) | 99.7% (99.7%-99.7%) | 0.38-9.32 |
| All countries/subregions | 686 | 46646973 | 0.00-38.2 | 0.86 | 1.58 | 1.48-1.69 | 481819.0 (P < 0.01) | 99.9% (99.9%-99.9%) | 0.01-5.18 |
| General population | |||||||||
| Afghanistan | 6 | 12048 | 0.00-4.03 | 0.88 | 0.61 | 0.20-1.18 | 21.7 (P < 0.01) | 76.9% (48.5%-89.6%) | 0.00-2.68 |
| Egypt | 147 | 110603 | 0.00-54.10 | 11.82 | 13.08 | 11.51-14.73 | 8457.0 (P < 0.01) | 98.3% (98.1-98.4%) | 0.62-36.45 |
| Fertile Crescent4 | 64 | 189456 | 0.00-8.87 | 0.19 | 0.42 | 0.24-0.64 | 1117.8 (P < 0.01) | 94.4% (93.4%-95.2%) | 0.00-2.39 |
| Gulf5 | 85 | 222829 | 0.00-22.54 | 0.83 | 1.41 | 1.0-1.88 | 5343.3 (P < 0.01) | 98.4% (98.3%-98.6%) | 0.00-7.66 |
| Horn of Africa6 | 27 | 29552 | 0.00-8.50 | 1.53 | 1.86 | 1.26-2.57 | 262.0 (P < 0.01) | 90.1% (86.8%-92.6%) | 0.00-6.13 |
| Iran | 50 | 101677 | 0.00-2.35 | 0.45 | 0.33 | 0.21-0.47 | 206.9 (P < 0.01) | 76.3% (69.0%-81.9%) | 0.00-1.25 |
| Maghreb7 | 42 | 1378206 | 0.00-6.16 | 0.62 | 0.87 | 0.55-1.26 | 7595.3 (P < 0.01) | 99.5% (99.5%-99.5%) | 0.00-4.38 |
| Pakistan | 106 | 301814 | 0.44-73.38 | 6.82 | 8.81 | 7.62-10.06 | 13619.0 (P < 0.01) | 99.2% (99.2%-99.3%) | 0.60-24.62 |
| All countries/subregions | 527 | 2346185 | 0.00-73.38 | 3.14 | 4.49 | 4.10-4.90 | 83750.3 (P < 0.01) | 99.4% (99.4%-99.4%) | 0.00-16.88 |
HCV Ab prevalence data were available for 30 countries in Europe. HCV Ab prevalence in blood donors ranged from 0 to 3.28%, with a median of 0.06% (Table 2). The pooled mean prevalence was 0.11% (95%CI: 0.10%–0.13%). Prevalence in the general population ranged from 0 to 16.83%, with a median of 1.11%. The pooled mean prevalence was 1.59% (95%CI: 1.25%–1.97%). There was strong evidence for heterogeneity in HCV Ab prevalence (P < 0.01), with the majority of variation being attributed to true variation in prevalence across studies rather than chance (I2 > 98.7%).
| Subpopulation | Studies | Samples | HCV Ab prevalence | Pooled HCV Ab prevalence | Heterogeneity measures | ||||
| Total (n) | Total (n) | Range (%) | Median (%) | Mean (%) | 95%CI | Q (P value)1 | I² (confidence limits)2 | Prediction interval (%)3 | |
| Blood donors | 257 | 25232790 | 0.0-3.28 | 0.06 | 0.11 | 0.10-0.13 | 35657.5 (P < 0.01) | 99.3 (99.3-99.3) | 0.00-0.51 |
| The general population | 120 | 410444 | 0.0-16.83 | 1.11 | 1.59 | 1.25-1.97 | 9176.9 (P < 0.01) | 98.7 (98.6-98.8) | 0.0-7.57 |
The HCV viremic rate of blood donors in different MENA countries ranged from 61.84% to 93.33%, with a median of 70.78% (Supplementary Table 3). The pooled mean for the entire MENA region was 76.29% (95%CI: 67.64%–84.02%), indicating that approximately three-quarters of Ab-positive blood donors are chronically infected. The viremic rate ranged from 22.73% to 100% in the general population in different MENA countries, with a median of 68.27% (Supplementary Table 3). The pooled mean for the entire MENA region was 65.73% (95%CI: 61.03%–70.29%). There was strong evidence for heterogeneity in the viremic rates (P < 0.01), with most variation being attributed to true variation in the viremic rate across studies rather than chance (I2 > 77.4%).
The meta-regressions for MENA indicated that HCV Ab prevalence in the general population was 1.72-fold (95%CI: 1.50–1.97) higher than that in blood donors (Table 3). They also indicated substantial variation in prevalence by country and subregion with Egypt and Pakistan having a higher prevalence than the rest of MENA countries. Importantly, the analyses indicated that HCV Ab prevalence has been declining over the last three decades at an average rate of 4% per year (ARR of 0.96; 95%CI: 0.95–0.97). Subgroup analyses were conducted on the above results. The same regressions were repeated, but for Egypt, Pakistan and other MENA countries individually (Table 4). These analyses indicated that HCV Ab prevalence in the general population was 1.30-fold (95%CI: 1.07–1.59) higher than that among blood donors in Egypt, 2.52-fold (95%CI: 1.89–3.36) higher in Pakistan, and 1.73-fold (95%CI: 1.42–2.11) higher in the remaining MENA countries. The analyses also confirmed the same rate of decline for prevalence at 4% in the rest of MENA countries. The rate of decline was slightly higher in Egypt at 6%. There was no evidence for a decline in prevalence, however, in Pakistan.
| Studies | Samples | Univariable analysis | Multivariable analysisb | ||||||
| Total (n) | Total (n) | RR (95%CI) | P value | F P valuea | Variance explained R2 (%) | ARR (95%CI) | P value | ||
| Subpopulations | |||||||||
| Blood donors | 686 | 46646973 | 1 | - | 1 | - | |||
| The general population | 527 | 2346185 | 2.92 (2.41-3.55) | < 0.001 | < 0.001 | 10.73 | 1.72 (1.50-1.97) | < 0.001 | |
| Country/subregion | |||||||||
| Afghanistan | 46 | 749455 | 1 | - | 1 | - | |||
| Egypt | 263 | 1677272 | 14.89 (10.2-21.8) | < 0.001 | 9.48 (6.54-13.75) | < 0.001 | |||
| Fertile Crescent1 | 221 | 3678408 | 0.52 (0.35-0.77) | < 0.001 | 0.49 (0.34-0.72) | < 0.001 | |||
| Gulf2 | 241 | 21114208 | 1.24 (0.84-1.82) | 0.280 | 0.82 (0.56-1.19) | 0.398 | |||
| Horn of Africa3 | 49 | 77628 | 2.05 (1.25-3.37) | 0.005 | 1.33 (0.82-2.15) | 0.244 | |||
| Iran | 123 | 16073479 | 0.50 (0.33-0.77) | < 0.001 | 0.42 (0.28-0.63) | < 0.001 | |||
| Maghreb4 | 91 | 3523250 | 1.02 (0.66-1.56) | 0.936 | 0.77 (0.51-1.16) | 0.207 | |||
| Pakistan | 179 | 2099458 | 6.96 (4.71-10.29) | < 0.001 | < 0.001 | 58.39 | 5.44 (3.73-7.93) | < 0.001 | |
| Year of data collection | 1213 | 48993158 | 0.95 (0.94-0.97) | < 0.001 | < 0.001 | 3.71 | 0.96 (0.95-0.97) | < 0.001 | |
| Studies | Samples | Univariable analysis | Multivariable analysisb | |||||
| Total (n) | Total (n) | RR (95%CI) | P value | F P valuea | Variance explained R2 (%) | ARR (95%CI) | P value | |
| Egypt | ||||||||
| Subpopulations | ||||||||
| Blood donors | 116 | 1566669 | 1 | - | 1 | - | ||
| The general population | 147 | 110603 | 1.25 (1.00-1.57) | 0.049 | 0.087 | 2.05 | 1.30 (1.07-1.59) | 0.008 |
| Year of data collection | 263 | 1677272 | 0.94 (0.93-0.95) | < 0.001 | < 0.001 | 24.48 | 0.94 (0.93-0.95) | < 0.001 |
| Pakistan | ||||||||
| Subpopulations | ||||||||
| Blood donors | 73 | 1797644 | 1 | - | - | - | ||
| The general population | 106 | 301814 | 2.52 (1.89-3.36) | < 0.001 | < 0.001 | 19.03 | - | - |
| Year of data collection | 179 | 2099458 | 1.00 (0.98-1.03) | 0.648 | 0.648 | 0.00 | - | - |
| Rest of MENA countries | ||||||||
| Subpopulations | ||||||||
| Blood donors | 497 | 43282660 | 1 | - | - | 1 | - | |
| The general population | 274 | 1933768 | 1.80 (1.47-2.21) | < 0.001 | < 0.001 | 5.44 | 1.73 (1.42-2.11) | < 0.001 |
| Country/subregion | ||||||||
| Afghanistan | 46 | 749455 | 1 | - | - | 1 | - | |
| Fertile Crescent1 | 221 | 3678408 | 0.53 (0.35-0.81) | 0.003 | 0.50 (0.33-0.75) | 0.001 | ||
| Gulf2 | 241 | 21114208 | 1.26 (0.83-1.91) | 0.273 | 0.86 (0.56-1.30) | 0.462 | ||
| Horn of Africa3 | 49 | 77628 | 2.08 (1.22-3.54) | 0.007 | 1.37 (0.81-2.32) | 0.247 | ||
| Iran | 123 | 16073479 | 0.51 (0.33-0.81) | 0.004 | 0.43 (0.28-0.67) | < 0.001 | ||
| Maghreb4 | 91 | 3523250 | 1.04 (0.65-1.64) | 0.883 | < 0.001 | 11.48 | 0.79 (0.50-1.24) | 0.298 |
| Year of data collection | 771 | 45216428 | 0.95 (0.94-0.96) | < 0.001 | < 0.001 | 6.22 | 0.96 (0.95-0.98) | < 0.001 |
In a sensitivity analysis, the same regressions were also repeated, but excluding all blood donor data (not shown). The analyses indicated that HCV Ab prevalence in MENA is declining at a rate of 5% per year (ARR of 0.95; 95%CI: 0.93–0.97), indicating a marginally higher rate of decline in the general population.
The meta-regressions for Europe indicated that HCV Ab prevalence in the general population is 15.10-fold (95%CI: 11.48–19.86) higher than that in blood donors (Table 5). The analyses indicated further that HCV Ab prevalence has been declining over the last three decades at a similar rate to that of MENA, at 4% per year (ARR of 0.96; 95%CI: 0.92–0.99).
| Studies | Samples | Univariable analysis | Multivariable analysisb | |||||
| Total (n) | Total (n) | RR (95%CI) | P value | F P valuea | Variance explained R2 (%) | ARR (95%CI) | P value | |
| Subpopulations | ||||||||
| Blood donors | 257 | 25232790 | 1 | 1 | ||||
| The general population | 120 | 410444 | 15.57 (11.83-20.49) | < 0.001 | < 0.001 | 53.62 | 15.10 (11.48-19.86) | < 0.001 |
| Year of data collection | 377 | 25643234 | 0.93 (0.88-0.98) | 0.004 | 0.005 | 2.17 | 0.96 (0.92-0.99) | 0.020 |
A sensitivity analysis was conducted on the above results. The same regressions were repeated, but excluding all blood donor data (not shown). The analyses indicated that HCV Ab prevalence in Europe is declining at a rate of 10% per year (ARR of 0.90; 95%CI: 0.85–0.96), higher than that in MENA.
Levels and trends of HCV Ab prevalence in blood donors and in the general population of MENA were assessed using a large standardized database. There was large variability in HCV Ab prevalence by country and subregion, with Egypt and Pakistan, the largest countries in MENA by population size, having several fold higher prevalence than the rest of MENA countries. HCV Ab prevalence in the remaining MENA countries was at about 1% or less, similar to that in Europe and most other countries globally[12,41]. These results confirm our understanding of HCV epidemiology across MENA countries and subregions[4-11,21-28,42-49].
Strikingly, HCV Ab prevalence is declining rapidly in both MENA and Europe, and at a similar rate of about 4% per year. The exception to this downward trend was Pakistan where there was no evidence for a decline. These declines may be reflective, in part, of the declining incidence of HCV infection within these regions through improvements to infection control following the discovery of this virus three decades ago, and scale-up of HCV treatment worldwide[3]. They also may reflect the progressive improvement in effective blood donor selection, such as by motivating and retaining voluntary nonremunerated donors to donate regularly[19].
A major finding of this study is that HCV Ab prevalence in blood donors in MENA was similar to HCV Ab prevalence in the general population; unlike the situation in Europe. While HCV Ab prevalence in the general population was almost twofold higher than that of HCV Ab prevalence in blood donors in MENA, it was 15-fold higher in Europe (Table 3vs Table 5). HCV Ab prevalence in blood donors in MENA appears to closely reflect the background prevalence in the wider population. Of note that HCV Ab prevalence in blood donors is a function of not only the prevalence in the general population, but also of the effectiveness of blood donation programs to collect blood from regular voluntary nonremunerated blood donors[19]. This finding suggests that risk reduction strategies through selection and retention of safer blood donors (regular voluntary nonremunerated blood donors) are not yet effectively implemented widely in MENA as in Europe[19], where the source of blood largely comes from such donors. Indeed regulatory framework (including legislation, regulation, policies and standards) and a functioning regulatory authority to enforce the regulatory framework is largely at its infancy in MENA[19], where, as of 2016, only 55% of MENA countries had legislation covering safety and quality of blood transfusions, and only two countries had achieved 100% voluntary nonremunerated blood donations[19,50]. Furthermore, HCV Ab prevalence in blood donors may be reflective of people in the general population unaware of their HCV infection status, in the context of which an individual aware of their positive HCV infection status would not donate blood.
Nevertheless, contingent on the quality of blood donor management systems implemented within countries of MENA, this finding indicates that HCV Ab prevalence in blood donors in MENA (unlike in North America[18] and Europe[16]) can be used for the time being as a proxy to estimate infection levels in the general population. This outcome has important consequences. With the lack of nationally representative population-based surveys in most countries of this region, blood donor data, which are readily available, can be easily used to assess levels and trends of this infection in the wider population. They can also be used to generate other estimates, such as those related to the disease burden of HCV sequelae, and can be leveraged to assess, track and validate progress toward the WHO elimination goals for this infection[3]. The present study also provides adjustment factors to improve use of blood donor data (Table 2), so that they better reflect HCV levels in the wider population. These adjustment factors can be used at a regional level, or can be fine-tuned so as to be specific for individual countries.
This study had several limitations. Availability of data varied across MENA, with HCV Ab prevalence data being unavailable for Bahrain. The majority of HCV viremia data were collected at times before the launch of DAA treatment programs (Supplementary Table 3); thus, they may not represent the current viremic rate in blood donors and in the general population. Analysis for the different blood donor types was not conducted as the specification of blood donor type was not available for the vast majority of HCV Ab prevalence measures. The sample size of blood donors was larger than that of the general population; however, the sample size in the general population was still substantial at 2.3 million. Despite these limitations, an immense volume of data was acquired, allowing various analyses and an array of consequential inferences to be drawn. While high heterogeneity was found, most (63%) of it was subsequently explained in meta-regression analyses in terms of prevalence variation by country and subregion within MENA.
HCV Ab prevalence in the wider population of MENA and Europe appears to be rapidly declining by 4% per year. Blood donor data in MENA (but not in Europe) provide a useful proxy for HCV infection levels and trends in the general population; at least in countries where effective blood donor selection and blood donor management programs are not in place. Thus, the data can be utilized in HCV infection and disease burden estimates and to assess, track and validate progress toward WHO elimination goals for this infection. While these findings are specific for MENA, they may also apply to resource-limited countries of other regions.
The Middle East and North Africa (MENA) Region is the most affected by hepatitis C virus (HCV) infection, with approximately 20% of the global chronically infected individuals residing in this region. Despite this, only three countries conducted national population-based surveys to delineate HCV infection levels in the general population.
HCV infection in blood donors have been used as a proxy for HCV infection levels in the general population. However, it is unclear how comparable blood donors are to the general population in countries in MENA and whether they are a suitable proxy population.
To delineate HCV epidemiology in blood donors and in the general population in MENA.
The MENA HCV Epidemiology Synthesis Project Database was used as a data source. Studies reporting HCV in blood donors and in the general population were retrieved, and random-effects meta-analyses and random-effects meta-regressions were performed. For regional comparison, similar analyses were performed for countries in Europe, using the Hepatitis C Prevalence Database from the European Centre for Disease Prevention and Control (ECDC).
A total of 1213 HCV Ab prevalence measures and 84 viremic rate measures were retrieved from the MENA HCV Epidemiology Synthesis Project, and 377 HCV Ab prevalence measures were retrieved from the ECDC. The pooled mean prevalence in MENA was 1.58% [95% confidence interval (CI): 1.48%–1.69%] in blood donors and 4.49% (95%CI: 4.10%–4.90%) in the general population, and in Europe was 0.11% (95%CI: 0.10%–0.13%) among blood donors and 1.59% (95%CI: 1.25%–1.97%) in the general population. In MENA, the prevalence in the general population was 1.72-fold (95%CI: 1.50–1.97) higher than that in blood donors, and in Europe it was 15.10-fold (95%CI: 11.48–19.86) higher. HCV prevalence appeared to be declining by 4% annually in both MENA and Europe.
Blood donor data in MENA (but not in Europe) appears to be comparable with that in the general population and therefore can be used as a useful proxy for HCV infection levels and trends in the general population, at least in countries where effective blood donor selection and blood donor management programs are not yet firmly in place. Blood donor data may be used to estimate HCV infection and disease burden and to assess, track, and validate progress toward World Health Organization elimination goals for this infection.
With the lack of nationally representative population-based surveys in most countries in MENA and beyond, blood donor data, which are readily available, can be easily used to assess levels and trends of this infection in the wider population. The study rationalizes and facilitates generation of estimates at low costs and demands for resources, even in resource-limited settings where population-level data are most scarce. While these findings are specific for MENA, they may also apply and be of relevance to other global regions.
The authors thank the European Centre for Disease Prevention and Control (ECDC) for their efforts in compiling the ECDC Hepatitis C Prevalence Database and for making this database publicly available in the service of science. The authors also thank Dr Yetmgeta E. Abdella for his valuable insights and feedback on this manuscript. The authors are also grateful for infrastructure support provided by the Biostatistics, Epidemiology, and Biomathematics Research Core at Weill Cornell Medicine-Qatar.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Infectious diseases
Country/Territory of origin: Qatar
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): E
P-Reviewer: Maslennikov R, Moreno-Gómez-Toledano R, Saha S S-Editor: Liu M L-Editor: Kerr C P-Editor: Liu M
| 1. | World Health Organization. Epidemiology of hepatitis C virus in the WHO Eastern Mediterranean Region: implications for strategic action. [cited 20 May 2021]. Available from: https://apps.who.int/iris/bitstream/handle/10665/336174/9789290222866-eng.pdf. |
| 2. | Lauer GM, Walker BD. Hepatitis C virus infection. N Engl J Med. 2001;345:41-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2042] [Cited by in RCA: 2025] [Article Influence: 84.4] [Reference Citation Analysis (0)] |
| 3. | World Health Organization. Global health sector strategy on viral hepatitis 2016-2021. Towards ending viral hepatitis. [cited 20 May 2021]. Available from: https://apps.who.int/iris/bitstream/handle/10665/246177/WHO-HIV-2016.06-eng.pdf. |
| 4. | Ayoub HH, Abu-Raddad LJ. Impact of treatment on hepatitis C virus transmission and incidence in Egypt: A case for treatment as prevention. J Viral Hepat. 2017;24:486-495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 55] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 5. | Kouyoumjian SP, Chemaitelly H, Abu-Raddad LJ. Characterizing hepatitis C virus epidemiology in Egypt: Systematic reviews, meta-analyses, and meta-regressions. Sci Rep. 2018;8:1661. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 94] [Cited by in RCA: 126] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 6. | Mohamoud YA, Mumtaz GR, Riome S, Miller D, Abu-Raddad LJ. The epidemiology of hepatitis C virus in Egypt: A systematic review and data synthesis. BMC Infect Dis. 2013;13:288. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 234] [Cited by in RCA: 251] [Article Influence: 20.9] [Reference Citation Analysis (0)] |
| 7. | Ayoub HH, Chemaitelly H, Kouyoumjian SP, Abu-Raddad LJ. Characterizing the historical role of parenteral antischistosomal therapy in hepatitis C virus transmission in Egypt. Int J Epidemiol. 2020;49:798-809. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 8. | Al Kanaani Z, Mahmud S, Kouyoumjian SP, Abu-Raddad LJ. The epidemiology of hepatitis C virus in Pakistan: Systematic review and meta-analyses. R Soc Open Sci. 2018;5:180257. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 66] [Cited by in RCA: 72] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 9. | Ayoub HH, Abu-Raddad LJ. Treatment as prevention for hepatitis C virus in Pakistan: mathematical modelling projections. BMJ Open. 2019;9:e026600. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 10. | Mahmud S, Al Kanaani Z, Abu-Raddad LJ. Characterization of the hepatitis C virus epidemic in Pakistan. BMC Infect Dis. 2019;19:809. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 29] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 11. | Ayoub HH, Al Kanaani Z, Abu-Raddad LJ. Characterizing the temporal evolution of the hepatitis C virus epidemic in Pakistan. J Viral Hepat. 2018;25:670-679. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 12. | Gower E, Estes C, Blach S, Razavi-Shearer K, Razavi H. Global epidemiology and genotype distribution of the hepatitis C virus infection. J Hepatol. 2014;61:S45-S57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1325] [Cited by in RCA: 1362] [Article Influence: 123.8] [Reference Citation Analysis (0)] |
| 13. | Qureshi H, Bile KM, Jooma R, Alam SE, Afridi HU. Prevalence of hepatitis B and C viral infections in Pakistan: findings of a national survey appealing for effective prevention and control measures. East Mediterr Health J. 2010;16 Suppl:S15-S23. [PubMed] |
| 14. | El-Zanaty FH, Way AA. Egypt demographic and health survey. 5th ed. Cairo: Ministry of Health and Population, 2005. |
| 15. | Daw MA, El-Bouzedi A; In association with Libyan Study Group of Hepatitis & HIV. Prevalence of hepatitis B and hepatitis C infection in Libya: results from a national population based survey. BMC Infect Dis. 2014;14:17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 40] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 16. | Hofstraat SHI, Falla AM, Duffell EF, Hahné SJM, Amato-Gauci AJ, Veldhuijzen IK, Tavoschi L. Current prevalence of chronic hepatitis B and C virus infection in the general population, blood donors and pregnant women in the EU/EEA: a systematic review. Epidemiol Infect. 2017;145:2873-2885. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 73] [Cited by in RCA: 93] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 17. | Tognon F, Sevalie S, Gassimu J, Sesay J, Hann K, Sheku M, Bearse E, Di Gennaro F, Marotta C, Pellizzer G, Putoto G, Lado M, Franke MF, Dibba Y, Gevao S, Beynon F, Mesman AW. Seroprevalence of hepatitis B and hepatitis C among blood donors in Sierra Leone: A multi-year retrospective study. Int J Infect Dis. 2020;99:102-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 18. | Denniston MM, Jiles RB, Drobeniuc J, Klevens RM, Ward JW, McQuillan GM, Holmberg SD. Chronic hepatitis C virus infection in the United States, National Health and Nutrition Examination Survey 2003 to 2010. Ann Intern Med. 2014;160:293-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 529] [Cited by in RCA: 579] [Article Influence: 52.6] [Reference Citation Analysis (0)] |
| 19. | World Health Organization. Global status report on blood safety and availability 2016. [cited 15 May 2021]. Available from: https://apps.who.int/iris/bitstream/handle/10665/254987/9789241565431-eng.pdf. |
| 20. | European Centre for Disease Prevention and Control. Hepatitis C Prevalence Database. [cited 15 March 2021]. Available from: https://www.ecdc.europa.eu/en/all-topics-z/hepatitis-c/tools/hepatitis-c-prevalence-database. |
| 21. | Harfouche M, Chemaitelly H, Kouyoumjian SP, Mahmud S, Chaabna K, Al-Kanaani Z, Abu-Raddad LJ. Hepatitis C virus viremic rate in the Middle East and North Africa: Systematic synthesis, meta-analyses, and meta-regressions. PLoS One. 2017;12:e0187177. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 22. | Ayoub HH, Chemaitelly H, Omori R, Abu-Raddad LJ. Hepatitis C virus infection spontaneous clearance: Has it been underestimated? Int J Infect Dis. 2018;75:60-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 23. | Chemaitelly H, Chaabna K, Abu-Raddad LJ. The Epidemiology of Hepatitis C Virus in the Fertile Crescent: Systematic Review and Meta-Analysis. PLoS One. 2015;10:e0135281. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 48] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 24. | Chemaitelly H, Mahmud S, Rahmani AM, Abu-Raddad LJ. The epidemiology of hepatitis C virus in Afghanistan: systematic review and meta-analysis. Int J Infect Dis. 2015;40:54-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 36] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 25. | Fadlalla FA, Mohamoud YA, Mumtaz GR, Abu-Raddad LJ. The epidemiology of hepatitis C virus in the Maghreb region: systematic review and meta-analyses. PLoS One. 2015;10:e0121873. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 48] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 26. | Chaabna K, Kouyoumjian SP, Abu-Raddad LJ. Hepatitis C Virus Epidemiology in Djibouti, Somalia, Sudan, and Yemen: Systematic Review and Meta-Analysis. PLoS One. 2016;11:e0149966. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 41] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 27. | Mohamoud YA, Riome S, Abu-Raddad LJ. Epidemiology of hepatitis C virus in the Arabian Gulf countries: Systematic review and meta-analysis of prevalence. Int J Infect Dis. 2016;46:116-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 55] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 28. | Mahmud S, Akbarzadeh V, Abu-Raddad LJ. The epidemiology of hepatitis C virus in Iran: Systematic review and meta-analyses. Sci Rep. 2018;8:150. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 80] [Cited by in RCA: 83] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 29. | Higgins J, Green S. Cochrane handbook for systematic reviews of interventions. John Wiley & Sons, 2011. |
| 30. | Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52948] [Cited by in RCA: 47158] [Article Influence: 2947.4] [Reference Citation Analysis (0)] |
| 31. | Abu-Raddad L AF, Semini I, Reidner G, Wilson D, Tavil O. Characterizing the HIV/AIDS epidemic in the Middle East and North Africa: Time for strategic action. Washington DC: The World Bank Press, 2010. |
| 32. | Abu-Raddad LJ, Hilmi N, Mumtaz G, Benkirane M, Akala FA, Riedner G, Tawil O, Wilson D. Epidemiology of HIV infection in the Middle East and North Africa. AIDS. 2010;24 Suppl 2:S5-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 109] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 33. | Kuo G, Choo QL, Alter HJ, Gitnick GL, Redeker AG, Purcell RH, Miyamura T, Dienstag JL, Alter MJ, Stevens CE. An assay for circulating antibodies to a major etiologic virus of human non-A, non-B hepatitis. Science. 1989;244:362-364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2495] [Cited by in RCA: 2343] [Article Influence: 65.1] [Reference Citation Analysis (0)] |
| 34. | European Centre for Disease Prevention Control. Epidemiological assessment of hepatitis B and C among migrants in the EU/EEA. [cited 13 April 2021]. Available from: https://www.ecdc.europa.eu/sites/portal/files/media/en/publications/Publications/epidemiological-assessment-hepatitis-B-and-C-among-migrants-EU-EEA.pdf. |
| 35. | European Directorate for the Quality of Medicines & Healthcare (EDQM). Report on the Collection, Testing and Use of Blood and Blood Components in Europe. [cited 13 April 2021]. Available from: https://www.edqm.eu/en/blood-transfusion-reports-70.html. |
| 36. | Borenstein M, Hedges LV, Higgins JP, Rothstein HR. Introduction to meta-analysis. John Wiley & Sons, 2011. |
| 37. | Freeman MF, Tukey JW. Transformations related to the angular and the square root. Ann Math Stat. 1950;21:607-611. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1674] [Cited by in RCA: 1682] [Article Influence: 22.4] [Reference Citation Analysis (0)] |
| 38. | Schwarzer G, Chemaitelly H, Abu-Raddad LJ, Rücker G. Seriously misleading results using inverse of Freeman-Tukey double arcsine transformation in meta-analysis of single proportions. Res Synth Methods. 2019;10:476-483. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 190] [Cited by in RCA: 388] [Article Influence: 64.7] [Reference Citation Analysis (0)] |
| 39. | Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39087] [Cited by in RCA: 46497] [Article Influence: 2113.5] [Reference Citation Analysis (3)] |
| 40. | Frank C, Mohamed MK, Strickland GT, Lavanchy D, Arthur RR, Magder LS, El Khoby T, Abdel-Wahab Y, Aly Ohn ES, Anwar W, Sallam I. The role of parenteral antischistosomal therapy in the spread of hepatitis C virus in Egypt. Lancet. 2000;355:887-891. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 694] [Cited by in RCA: 684] [Article Influence: 27.4] [Reference Citation Analysis (0)] |
| 41. | Messina JP, Humphreys I, Flaxman A, Brown A, Cooke GS, Pybus OG, Barnes E. Global distribution and prevalence of hepatitis C virus genotypes. Hepatology. 2015;61:77-87. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1077] [Cited by in RCA: 1145] [Article Influence: 114.5] [Reference Citation Analysis (0)] |
| 42. | Chemaitelly H, Mahmud S, Kouyoumjian SP, Al-Kanaani Z, Hermez JG, Abu-Raddad LJ. Who to Test for Hepatitis C Virus in the Middle East and North Africa? Hepatol Commun. 2019;3:325-339. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 43. | Chemaitelly H, Mahmud S, Mumtaz GR, Benova L, Ayoub HH, Kouyoumjian SP. Hepatitis C Virus in the Middle East and North Africa. In: Handbook of Healthcare in the Arab World. Laher I, editor. Cham: Springer International Publishing, 2019: 1-27.. |
| 44. | Harfouche M, Chemaitelly H, Mahmud S, Chaabna K, Kouyoumjian SP, Al Kanaani Z, Abu-Raddad LJ. Epidemiology of hepatitis C virus among hemodialysis patients in the Middle East and North Africa: systematic syntheses, meta-analyses, and meta-regressions. Epidemiol Infect. 2017;145:3243-3263. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 45. | Mahmud S, Al-Kanaani Z, Chemaitelly H, Chaabna K, Kouyoumjian SP, Abu-Raddad LJ. Hepatitis C virus genotypes in the Middle East and North Africa: Distribution, diversity, and patterns. J Med Virol. 2018;90:131-141. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 40] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 46. | Mahmud S, Chemaitelly HS, Kouyoumjian SP, Al Kanaani Z, Abu-Raddad LJ. Key associations for hepatitis C virus genotypes in the Middle East and North Africa. J Med Virol. 2020;92:386-393. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 47. | Mahmud S, Kouyoumjian SP, Al Kanaani Z, Chemaitelly H, Abu-Raddad LJ. Individual-level key associations and modes of exposure for hepatitis C virus infection in the Middle East and North Africa: a systematic synthesis. Ann Epidemiol. 2018;28:452-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 48. | Mahmud S, Chemaitelly H, Al Kanaani Z, Kouyoumjian SP, Abu-Raddad LJ. Hepatitis C Virus Infection in Populations With Liver-Related Diseases in the Middle East and North Africa. Hepatol Commun. 2020;4:577-587. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 49. | Mahmud S, Mumtaz GR, Chemaitelly H, Al Kanaani Z, Kouyoumjian SP, Hermez JG, Abu-Raddad LJ. The status of hepatitis C virus infection among people who inject drugs in the Middle East and North Africa. Addiction. 2020;115:1244-1262. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 27] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 50. | World Health Organization. Global Database on Blood Safety. GDBS Summary Report 2011. [cited 15 March 2021]. Available from: https://www.who.int/bloodsafety/global_database/GDBS_Summary_Report_2011.pdf. |