Published online Jan 26, 2025. doi: 10.12998/wjcc.v13.i3.98104
Revised: October 1, 2024
Accepted: October 29, 2024
Published online: January 26, 2025
Processing time: 147 Days and 3.9 Hours
Complicated crown–root fracture (CRF) involves severe injury to the crown, root, and pulp, and may be accompanied by multiple root fractures. The loss of a tooth has lifelong consequences for children and teenagers, but the maintenance of pulp health and the calcific healing of multiple root fractures are rarely reported in the literature.
This case reports healing of a permanent tooth with complicated crown–root and additional root fractures, in which pulp health was maintained. A 10-year-old girl fell and fractured the root of her maxillary left central incisor at the cervical level. After the coronal fragment was repositioned, the tooth was splinted until the tooth was no longer mobile, 2 years later. Eight years after treatment, the tooth has remained asymptomatic with vital pulp and localized gingival overgrowth. Cone-beam computed tomography revealed not only calcified healing of the CRF but also spontaneous healing in an additional undiagnosed root fracture. The fracture line on the enamel could not be healed by hard tissue and formed a groove in the cervical crown. It was speculated that the groove was related to the localized gingival overgrowth.
This case provides a clinical perspective of the treatment of a tooth with a complicated CRF and an additional root fracture.
Core Tip: This case describes the conservative management of a complicated crown–root fracture with an additional root fracture that did not receive any surgical or endodontic treatment. A satisfactory outcome was achieved with an 8-year follow-up. The case report offers significant insights into the management of such dental injuries.
- Citation: Li N, Ren YY, Tang Y, Yang Q, Meng TT, Li S, Zhang J. Pulp health and calcific healing of a complicated crown–root fracture with additional root fracture in a maxillary incisor: A case report. World J Clin Cases 2025; 13(3): 98104
- URL: https://www.wjgnet.com/2307-8960/full/v13/i3/98104.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i3.98104
Trauma to the teeth may result in a complicated crown–root fracture (CRF), which is defined as a fracture that originates labially in the crown portion and extends apically and palatally in an oblique direction accompanied by pulp exposure[1]. One of the most challenging fracture patterns in a tooth with a complicated CRF occurs when the main fracture is accompanied by an additional root fracture[2,3]. The additional root fracture extends vertically within the root and backward in an apical direction while a separate fragment splinters from the root. Diagonal fracture lines within the root are difficult to detect on radiographs, especially if the fragments are touching and the fracture surfaces overlap. A combination of different types of injuries occurring concurrently to the same tooth will be more detrimental, creating a negative synergistic effect, and is the most common reason for extraction.
Few treatment options exist for the management of CRF cases with both CRF and additional root fractures. Several treatment techniques described in the literature, such as surgical extrusion[4,5], fragment reattachment[2,6], and intentional replantation[7-9], have been reported to preserve teeth with a complicated CRF. However, an additional root fracture is considered to be a contraindication for any of these treatments, and surgical extraction is usually considered an option. Nevertheless, extraction should not be the first choice of treatment in children and teenagers, for whom the loss of a tooth has lifelong consequences. Early loss of teeth in the anterior region may lead to the loss of alveolar bone in this area, compromising future treatment and creating esthetic and emotional problems[10]. Hence, management of this type of injury is challenging for clinicians.
This report describes in detail the management of a case of a complicated CRF with an additional root fracture that did not receive any surgical or endodontic treatment. A satisfactory prognosis was achieved with an 8-year follow-up. We hope this case report will provide useful clinical information on the management of teeth with multiple fractures.
A 10-year-old girl was referred to our hospital with a chief complaint of pain and mobility of her maxillary left central incisor (tooth 21) in August 2013.
Her mother reported that the patient had fallen, hitting her teeth on the ground, 24 hours before referral. The parents drove from a county town to the provincial capital to seek treatment 1 day after the trauma occurred.
The patient’s medical history was normal.
The patient had no significant prior family history.
An extra-oral examination showed some soft tissue bruises on the lips and hands. The intra-oral examination revealed an enamel fracture with no dentin involvement on the maxillary right central incisor (tooth 11) with lip and gum soft tissue bruising. The maxillary left central incisor (tooth 21) showed minimal displacement palatally, slight bleeding from the gingival sulcus, grade 2 mobility, sensitivity to percussion, and sensitivity to cold in the coronal segment, but no fracture lines were observed buccally or palatally.
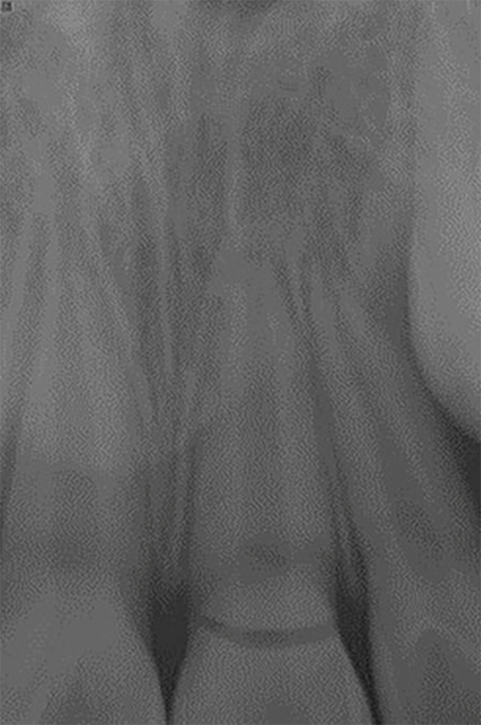
A periapical radiograph revealed an obvious horizontal fracture line located in the cervical crown of tooth 21, slightly coronal to the level of the alveolar crest. Developing roots were also detected in both central and lateral incisors (Figure 1).
On the basis of the examinations, we assumed that fractures of tooth 21 extended subgingivally toward the palatal side, involving the pulp cavity. Thus, the clinical diagnosis was complicated CRF of tooth 21, with an uncomplicated crown fracture on tooth 11.
The treatment option chosen was fixed appliance therapy for the fractured tooth 21 and direct restoration for tooth 11. The treatment plan, which involved emergency stabilization of the mobile coronal fragment[11], was discussed with the patient and her parents, who provided informed consent.
Tooth 21 was stabilized in the first session. The tooth was anesthetized, and the crown was repositioned into its original position by gentle finger pressure and stabilized using a flexible splint placed between the maxillary left lateral and right central incisors. The occlusion was checked to avoid early contacts. The patient and parents were informed about the care of the injured tooth for optimal healing and the patient was advised not to participate in contact sports. They were also instructed to maintain meticulous oral hygiene and to return for regular clinical and radiographic follow-up visits at 1, 3, 6, and 12 months, and then annually thereafter.
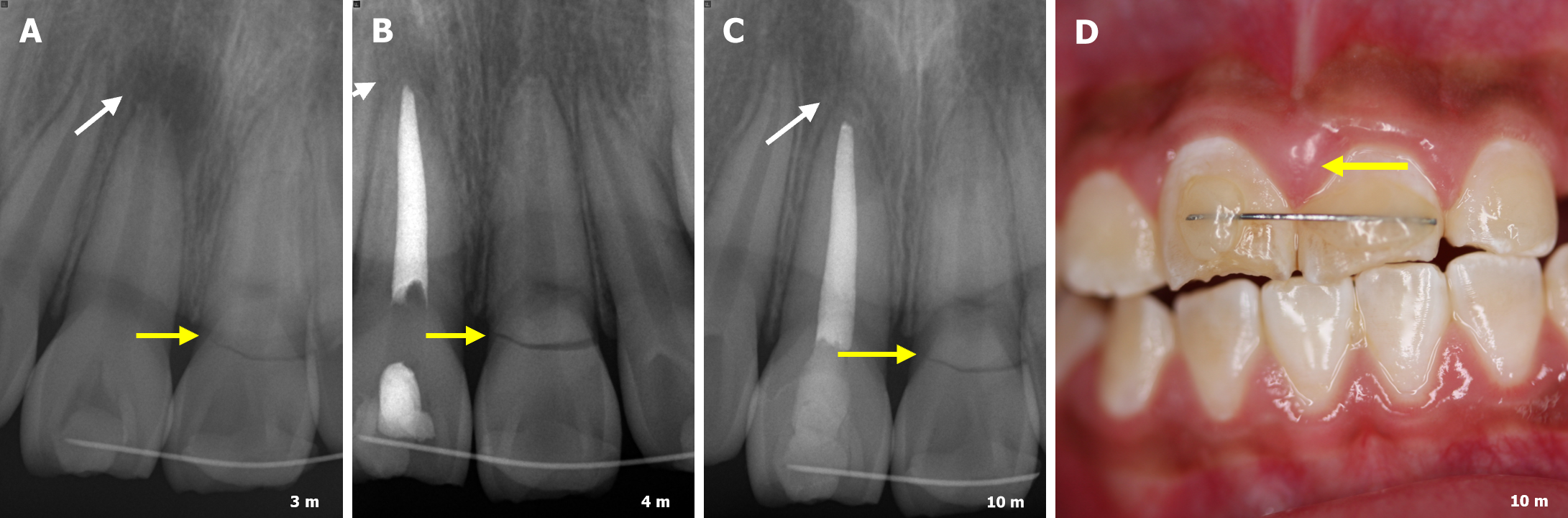
Tooth 11 received an apexification at the second session after 3 months, because clinical signs of pulp necrosis and radiographic evidence of a periapical lesion were observed (Figure 2A). The tooth was isolated with a rubber dam, and the root canal was prepared chemo-mechanically and dressed with a calcium hydroxide-based paste at 1-month intervals (Figure 2B). After 7 months, a calcified barrier had formed at the apex and complete periapical healing had occurred, so the root canal was filled with gutta-percha (Figure 2C).
During the recall period, misalignment of the crown of tooth 21 and localized gingival overgrowth became evident. The facial gingiva of tooth 21, including the gingival margin and papilla, was hyperplastic, but not sensitive on palpation. Tooth 11 appeared larger than tooth 21 (Figure 2D). No plaque or calculus were detected, and the periodontal probing depth was normal. In agreement with the patient’s parents, we followed up on the gingival overgrowth and further instructed the patient on home oral hygiene procedures.
Because the fractured crown still showed grade 1 mobility at the 1-year follow-up, a splint was replaced on the adjacent tooth 11 for long-term esthetic stabilization. The direct restoration of tooth 11 was delayed to reduce the misalignment esthetically (Figure 2D). The patient was encouraged to attend for recall every year.
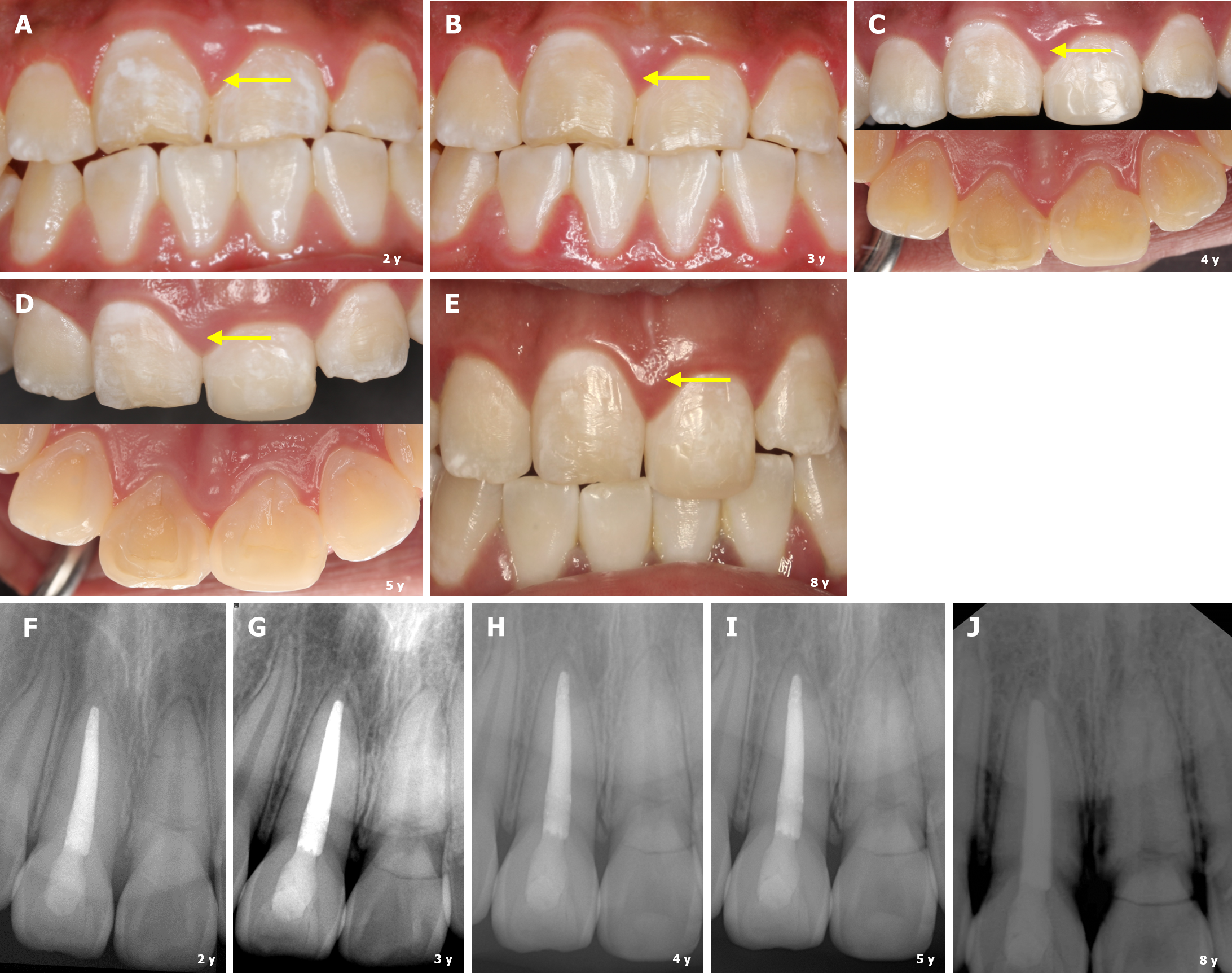
Teeth 11 and 21 were clinically and radiologically evaluated 2-years after the trauma. All teeth remained asymptomatic and the bonded orthodontic retainer did not require replacement. Tooth 21 was equally responsive to electrical pulp testing as the lateral incisor, and mobility testing indicated a similar degree of movement compared with the right incisor (tooth 11). Clinical examination also revealed no fistulae or pain on percussion or palpation (Figure 3A). Additionally, no signs of apical periodontitis or surrounding bone change were seen in the periapical radiographs. The radiographs all showed further healing of the fracture sites and completion of root development of tooth 21 (Figure 3F). These findings led us to a working diagnosis of healed root fracture, and the splint was removed. Periodontal evaluation revealed the localized gingival overgrowth clearly overlapped the cervical crown of tooth 21, and it seemed that tooth 21 was smaller than tooth 11. To reduce the visual differences, the edge of tooth 11 was smoothed instead of directly restoring it (Figure 3).
The patient has been attending annual follow-up visits for 8 years (Figure 3B-E). All teeth have remained asymptomatic, and the fractured root has not developed any radiographic signs of progressive root canal obliteration. The root canal is still visible, with a developed, apically closed root (Figure 3G-J). Chronological clinical and radiographic examinations are summarized in Table 1.
| Time | Tooth | Visual | Percussion | Mobility | Cold test/EPT | Radiology | Diagnosis/treatment |
| Pre-operative | #11 | Enamel fracture | + | 1 | + | - | Enamel fracture |
| #21 | Gingival bleeding | + | 2 | + | Fracture line | Complicated CRF/reposition, splint | |
| 3-month | #11 | - | + | 1 | - | Periapical radiolucency | Apical periodontitis/apexification |
| #21 | - | - | 1 | + | - | Splinting | |
| 10-month | #11 | - | - | 0 | - | Calcified barrier | Root canal filling |
| #21 | Gingival overgrowth | - | 1 | + | - | Prolonged splinting | |
| 2 year | #11 | - | - | 0 | - | - | Smoothing edge |
| #21 | Gingival overgrowth | - | 0 | + | - | Removing splint | |
| 3-8 year | #11 | - | - | 0 | - | - | - |
| #21 | Gingival overgrowth | - | 0 | + | Fracture calcified healing | Complicated CRF with additional root fracture |
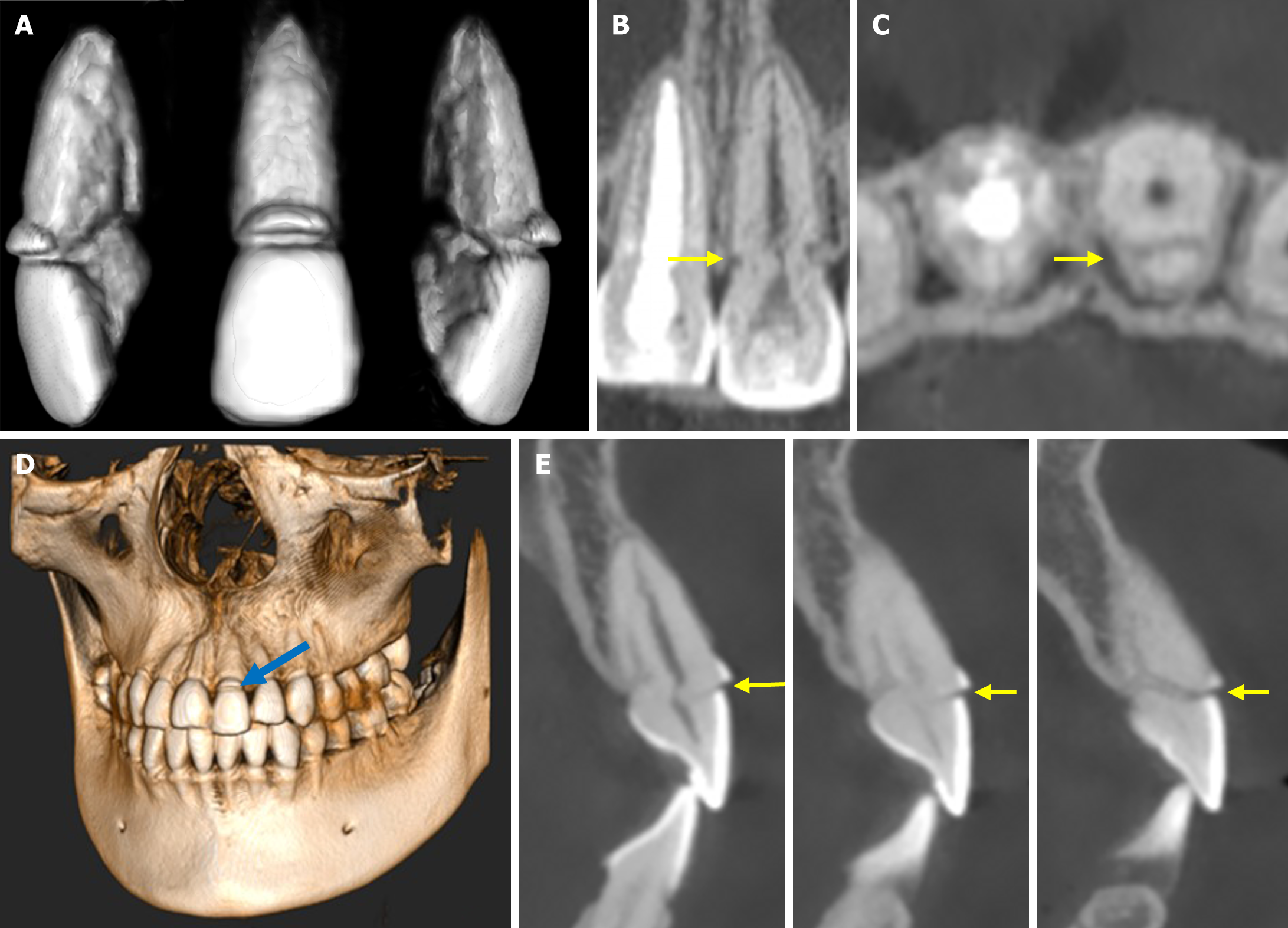
To understand the reason for the localized gingival overgrowth around tooth 21, cone-beam computed tomography (CBCT) images were taken 8 years after the trauma. The images indicated that tooth 21 had a complicated CRF (Figure 4). The healed fracture line began a few millimeters above the cementoenamel junction facially and followed an oblique course below the level of the alveolar bone crest palatally. The CBCT images also revealed an additional undiagnosed root fracture in which spontaneous healing had occurred by the interposition of calcified tissue (Figure 4B, C, and E). Based on the CBCT images, the final diagnosis was a complicated CRF combined with an additional root fracture. The CBCT images simultaneously revealed that the fracture line on the enamel had not been healed by hard tissue, forming a groove in the cervical crown. We speculated that the groove was related to the localized gingival overgrowth (Figure 4A and D).
To our knowledge, no other cases of successful healing of multiple complicated CRFs have been reported in the literature. Sarath et al[12] reported a case of a complicated CRF with an additional horizontal root fracture that was successfully managed with invasive interventions. The only management used in this case was repositioning of the coronal fragment and prolonged splinting of the tooth. As with the present case, they employed a simple, conservative treatment approach in a case of cervical horizontal root fracture by repositioning the coronal fragment, but the fractured root presented radiographic sign of progressive root canal obliteration over time[13]. This case report provides clinical information for the management of complicated CRF with an additional root fracture, in which the fracture line was located beyond the alveolar crest subgingivally. Nevertheless, calcified tissue healing of the complicated CRF occurred, and spontaneous healing occurred in the additional root fracture in tooth 21 (Figure 4). Pulp sensitivity testing combined with the assessment of the degree of root canal calcification indicated that the pulp was healthy. The patient and her parents expressed satisfaction with the treatments they received.
The key to successful healing of root fractures is to effectively maintain a healthy pulp and periodontium. Andreasen and Cvek confirmed that young age, immature root formation, and positive pulp sensitivity at the time of injury are significantly and positively related to both pulpal healing and hard tissue repair of fractures[10,11,14,15]. Odontoblasts from the pulp are spontaneously responsible for the healing process, as has been described in histological reports[16]. Zhou et al[17] observed spontaneous healing in two pediatric cases of CRF. In this case, the patient was 10 years old, and the tooth was developing with a wider apex, indicating the higher healing capacity of the dental pulp. Additionally, one of the suitable conditions we created could relate to the emergency management of complete repositioning of the fragment and splinting provided an important stimulus for pulpal healing. Thus, the sections of the CBCT scan confirmed that multiple fracture lines had been obliterated by calcified tissue (Figure 4C-F). Cervical root fractures are more difficult to manage, because of their greater susceptibility to further injury and the likelihood of subsequent infection of the root canal system[18]. Another suitable condition we created could relate to the stability created by prolonged splinting of the fractured tooth to the adjacent tooth until the tooth was no longer mobile. Some case reports of cervical root fractures have described splinting for periods ranging from 4 to 7 years[13,19]. In the present case, when we observed continued mobility of the coronal fragment following the removal of the splint after 10 months, we prolonged the splinting period until the tooth was no longer mobile, 2 years later. This long-term stabilization may prevent further injury, which may protect the pulp from bacterial invasion from the gingival sulcus and favor hard tissue healing of the fracture. Hence, the treatment strategy we chose not only provided minimally invasive treatment but also optimized healing conditions, thus increasing the chance of successful healing for both the CRF and the undiagnosed additional root fracture.
CBCT was used to investigate the localized gingival overgrowth in tooth 21. The radiological evidence revealed that the original fracture extended from 1–2 mm above the cementoenamel junction on the labial surface to 2–3 mm below it on the palatal surface. This CBCT evidence may explain why there was gingival overgrowth in this case. As observed by Heithersay and Kahler[16], the healing of the fracture line on the enamel can be attributed solely to pulpal deposition, thus leaving a narrow unfilled enamel gutter or deficiency cervically and labially (Figure 4A and D). We speculated that the enamel groove provided a site for bacterial accumulation in the cervical portion during active tooth eruption. The groove is a narrow, plaque-retentive area that is difficult to instrument and serves as microbial storage, leading to persistent inflammation along the groove. Considering the age at which the original injury occurred, a gingival proliferative response to inflammation seems likely. To address this difficult issue, we will make a multidisciplinary plan to achieve the desired result.
Unfortunately, no clinical photos of the case were taken at the initial appointment 8 years ago, and limited examination records are available from that time. In hindsight, the diagnosis of complicated CRF in tooth 21 should have been made from multiple radiographs. On the other hand, the limitation of this case report is that the treatment option of prolonged splinting we used was not based on the IADT guidelines. Further study is needed to compare different treatments.
This case of pulp and calcified healing of multiple crown–root fractures achieved a satisfactory prognosis with an 8-year follow-up. It should be emphasized that conservative treatments can lead to favorable outcomes even in complex cases, and this case report offers valuable insights into the long-term healing processes of this type of dental injury.
We would like to thank the patient. We extend our thanks to the Radiology Departments of the College and Hospital of Stomatology, Anhui Medical University for facilitating the acquisition of the relevant materials.
| 1. | Bourguignon C, Cohenca N, Lauridsen E, Flores MT, O'Connell AC, Day PF, Tsilingaridis G, Abbott PV, Fouad AF, Hicks L, Andreasen JO, Cehreli ZC, Harlamb S, Kahler B, Oginni A, Semper M, Levin L. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 1. Fractures and luxations. Dent Traumatol. 2020;36:314-330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 307] [Article Influence: 61.4] [Reference Citation Analysis (0)] |
| 2. | Soliman S, Lang LM, Hahn B, Reich S, Schlagenhauf U, Krastl G, Krug R. Long-term outcome of adhesive fragment reattachment in crown-root fractured teeth. Dent Traumatol. 2020;36:417-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Andreasen JO, Andreasen FM, Andersson L. Textbook and color atlas of traumatic injuries to the teeth. 5th ed. Oxford: United Kingdom: John Wiley and Sons Ltd, 2019: 252-282. |
| 4. | Kirzioğlu Z, Karayilmaz H. Surgical extrusion of a crown-root fractured immature permanent incisor: 36 month follow-up. Dent Traumatol. 2007;23:380-385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Das B, Muthu MS. Surgical extrusion as a treatment option for crown-root fracture in permanent anterior teeth: a systematic review. Dent Traumatol. 2013;29:423-431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 32] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 6. | Andreasen FM, Norén JG, Andreasen JO, Engelhardtsen S, Lindh-Strömberg U. Long-term survival of fragment bonding in the treatment of fractured crowns: a multicenter clinical study. Quintessence Int. 1995;26:669-681. [PubMed] |
| 7. | Moura LF, Lima MD, Moura MS, Carvalho PV, Cravinhos JC, Carvalho CM. Treatment of a crown-root fracture with intentional replantation - case report with 16-year follow-up. Int Endod J. 2012;45:955-960. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Yuan LT, Duan DM, Tan L, Wang XJ, Wu LA. Treatment for a complicated crown-root fracture with intentional replantation: a case report with a 3.5-year follow up. Dent Traumatol. 2013;29:474-478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Chaniotis A, Kouimtzis TH. Intentional replantation and Biodentine root reconstruction. A case report with 10-year follow-up. Int Endod J. 2021;54:988-1000. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 10. | Andreasen JO, Andreasen FM, Mejàre I, Cvek M. Healing of 400 intra-alveolar root fractures. 1. Effect of pre-injury and injury factors such as sex, age, stage of root development, fracture type, location of fracture and severity of dislocation. Dent Traumatol. 2004;20:192-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 116] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 11. | Cvek M, Andreasen JO, Borum MK. Healing of 208 intra-alveolar root fractures in patients aged 7-17 years. Dent Traumatol. 2001;17:53-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 80] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 12. | Sarathy S, Arul B, Balasubramanian HP, Natanasabapathy V, Suresh N. A novel two-staged single-visit treatment of a maxillary central incisor with complicated crown-root fracture with additional horizontal mid-root fracture - A case report with a 5-year follow-up. J Conserv Dent Endod. 2023;26:484-489. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (1)] |
| 13. | Andreasen JO, Ahrensburg SS, Tsilingaridis G. Root fractures: the influence of type of healing and location of fracture on tooth survival rates - an analysis of 492 cases. Dent Traumatol. 2012;28:404-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 39] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 14. | Cvek M, Tsilingaridis G, Andreasen JO. Survival of 534 incisors after intra-alveolar root fracture in patients aged 7-17 years. Dent Traumatol. 2008;24:379-387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 53] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 15. | Cvek M, Mejàre I, Andreasen JO. Healing and prognosis of teeth with intra-alveolar fractures involving the cervical part of the root. Dent Traumatol. 2002;18:57-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 54] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 16. | Heithersay GS, Kahler B. Healing responses following transverse root fracture: a historical review and case reports showing healing with (a) calcified tissue and (b) dense fibrous connective tissue. Dent Traumatol. 2013;29:253-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 17. | Zhou ZL, Gao L, Sun SK, Li HS, Zhang CD, Kou WW, Xu Z, Wu LA. Spontaneous healing of complicated crown-root fractures in children: Two case reports. World J Clin Cases. 2022;10:6298-6306. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (1)] |
| 18. | Özler CÖ, Cehreli ZC. Conservative management of a cervical horizontal root fracture by long-term stabilisation: A case report. Aust Endod J. 2022;48:338-341. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 19. | Nandini S, Velmurugan N, Kandaswamy D. Calcific healing of a crown root fracture of a maxillary central incisor evaluated with spiral computed tomography and hounsfield units: a case report. Dent Traumatol. 2008;24:e96-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |