Published online May 26, 2024. doi: 10.12998/wjcc.v12.i15.2614
Revised: February 8, 2024
Accepted: April 8, 2024
Published online: May 26, 2024
Processing time: 114 Days and 3.9 Hours
The stent embedded in the esophageal mucosa is one of the complications after stenting for esophageal stricture. We present a case of stent adjustment with the aid of a transparent cap after endoscopic injection of an esophageal varices stent.
A 61-year-old male patient came to the hospital with discomfort of the chest after the stent implanted for the stenosis because of endoscopic injection of esophageal varices. The gastroscopy was performed, and the stent embedded into the esophageal mucosa. At first, we pulled the recycling line for shrinking the stent, however, the mucosa could not be removed from the stent. Then a forceps was performed to remove the mucosa in the stent, nevertheless, the bleeding form the mucosa was obvious. And then, we used a transparent cap to scrape the mucosa along the stent, and the mucosa were removed successfully without bleeding.
A transparent cap helps gastroscopy to remove the mucosa embedded in the stent after endoscopic injection of the esophageal varices stent.
Core Tip: Esophageal stenosis is one of the complications of endoscopic injection for treatment of esophageal varices. The stent embedding into the esophageal mucosa is one of the complications after stenting for esophageal stricture. We present a case of stent adjustment with the aid of a transparent cap after endoscopic injection of an esophageal varices stent.
- Citation: Zhang FL, Xu J, Zhu YD, Wu QN, Shi Y, Fang L, Zhou D, Wang H, Huang CJ, Zhou CH, Zhu Q. Transparent cap adjusted the stent placed for stenosis after endoscopic injection of esophageal varices: A case report. World J Clin Cases 2024; 12(15): 2614-2620
- URL: https://www.wjgnet.com/2307-8960/full/v12/i15/2614.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i15.2614
Esophageal stenosis is one of the complications of endoscopic injection for treatment of esophageal varices, and the incidence is between 2%-10%[1]. There was no report on the use of self-expanding metal stents (SEMS) for the treatment of esophageal strictures after endoscopic injection for esophageal varices. The stent embedding in the esophageal mucosa is one of the serious complications of SEMS for the treatment of esophageal strictures. We present in this article a case in which a transparent cap adjusted the stent implanted for the stenosis after endoscopic injection of cyanoacrylate (CYA) and sclerotherapy for esophageal varices.
A 61-year-old male patient presented to the hospital with discomfort of the chest for one month.
One month ago, the stent was implanted for the patient with esophageal stenosis who underwent endoscopic injection of cyanoacrylate and sclerotherapy for esophageal varices.
The patient suffered surgery for hepatocellular carcinoma 3 years ago.
All other personal and family medical history was normal.
Diseased liver face, no yellowing of the skin or sclera, clear breath sounds on both lungs auscultation, no dry or wet rales, heart rate of 76 beats/min, regular heart rhythm, soft abdomen, no tenderness or rebound pain, the spleen and the ribs were accessible, and there was no edema in either lower limb.
The laboratory result showed prothrombin time, alanine aminotransferase, creatine kinase (CK), CK-MB, creatinine, carbohydrate antigen (CA) 199, carcinoembryonic antigen, glucose, C-reactive protein, cholesterol, triglyceride and lipase were in normal range. White blood cell, Hemoglobin, platelet, dimer, amylase, total bilirubin, alpha-fetoprotein and CA125 were not in normal. HbsAg, hepatitis C antibody, human immunodefciency virus antibody, syphilis antibody, anti-nuclear anti-bodies were all negative (Table 1).
| Laboratory result | Normal | |
| WBC (109/L) | 2.22 | (3.4-9.5) |
| HB (g/L) | 80 | (115-150) |
| Platelet (109/L) | 31 | (125-350) |
| PT(s) | 13.5 | (9.7-13.5) |
| Dimer (mg/L) | 4.36 | (0-0.55) |
| ALT (u/L) | 23 | (9-50) |
| TB (umol/L) | 20.89 | (3-20) |
| CK (u/L) | 30 | (20-180) |
| CK-MB (u/L) | 20 | (0-30) |
| Cr (umol/L) | 67 | (40-80) |
| CA199 (kU/L) | 6.20 | (0-35) |
| CEA (ug/L) | 1.90 | (0-5) |
| AFP (ug/L) | 12.48 | (0-9) |
| CA125 (ug/L) | 101.10 | (0-35) |
| CRP (mg/L) | 9.50 | (0-10) |
| Triglyceride (mmol/L) | 0.60 | (0-1.7) |
| Cholesterol (mmol/L) | 2.87 | (2.86-5.98) |
| Amylase (U/L) | 201 | (35-135) |
| Lipase (U/L) | 106 | (0-190) |
| Glucose (mmol/L) | 5.41 | 3.0-6.1 |
| HbsAg | Negative | Negative |
| HIV Ab | Negative | Negative |
| Sp Ab | Negative | Negative |
| ANA | Negative | Negative |
| Hc Ab | Negative | Negative |
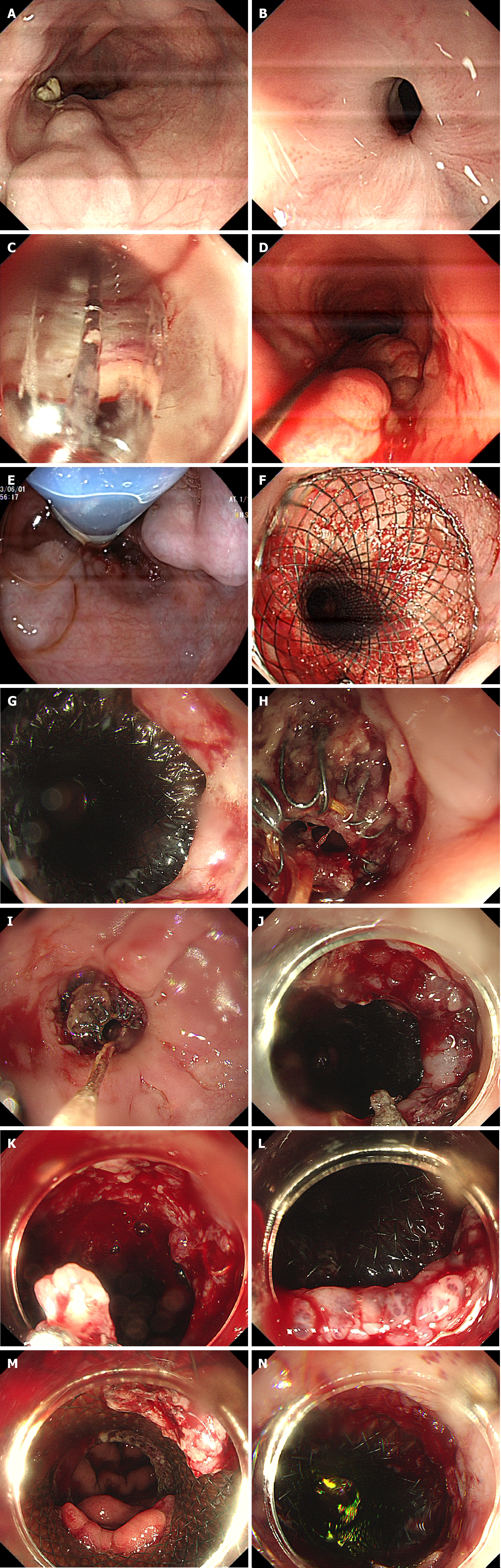
The computed tomography of chest and electrocardiogram were normal. We used an endoscope (EG-760R, diameter 9.3 mm, FUJIFILM, Japan) to observe retention in the esophageal cavity (Figure 1A), paying close attention to residual varices (Figure 1A) as we removed the residue. When the esophageal stricture was exposed (Figure 1B), we performed balloon dilatation (18 mm 55 mm, Nanjing Minimally Invasive Medical Technology Co, Ltd, Nanjing, China) to dilate the stricture (Figure 1C) until the body of the endoscope could smoothly pass through the stenosis. We inserted a semi
The gastroscopy showed that the anal side of the stent was normal; however, the oral side of the stent was embedded into the esophageal mucosa (Figure 1G). First, we attempted to pull the recycling line to shrink the SEMS to remove the mucosa embedded in the stent (Figure 1H and I); however, the mucosa could not be removed from the stent (Figure 1J). Then, forceps were used to remove the mucosa in the stent, but the patient experience obvious esophageal bleeding (Figure 1K). We then used a transparent cap to scrape the mucosa embedded in the stent along the SEMS (Figure 1L and M), and the mucosa was removed successfully without further bleeding (Figure 1N).
The esophageal mucosa embedded the stent which was implanted for the stenosis after endoscopic injection of esophageal varices.
We used a transparent cap to scrape the mucosa embedded the stent along the SEMS and the mucosa were removed successfully without bleeding.
The patient experienced relief from chest pain, and there was no infection, bleeding or perforation after adjusting the SEMS and removing the mucosa embedded in the stent. The patient was discharged from the hospital the next day.
Endoscopic sclerotherapy was considered the main treatment for esophageal varices[2]. In recent years cyanoacrylate injection was performed successfully for esophageal varices without any bleeding recurrence[3]. Esophageal stricture is one of the complication after endoscopic injection cyanoacrylate and/or sclerotherapy esophageal varices. Esophageal stricture is related to local inflammation, ulceration, and fibrosis caused by multiple injection[4]. The standard treatment for esophageal stricture after injection for esophageal varices is not mentioned in international guidelines[5]. European society of gastrointestinal endoscopy[6] recommended that the use of esophageal stent for the treatment of benign esophageal strictures had mainly been investigated in the context of refractory or recurrent benign esophageal strictures, and esophageal stent placement had a potential benefit because of its continuous expansion force, which may lead to stricture remodeling. Stent placement will extend the esophageal stricture, however, we should be alert to the complications, such as chest pain, reflux esophagitis, displacement or detachment, and tissue embedded stents[7-9].
Tissue embedded stents and chest pain are the common complications of esophageal stent placement. In this case, we used a transparent cap to assist the gastroscopy to successfully remove mucosa embedded the stent which was implanted for the stenosis after endoscopic injection esophageal varices with CYA and sclerotherapy. The advantages of the transparent cap for adjusting the stent are as follows: (1) The transparent cap is small and allows for a clear field of vision close to the stent; (2) the mucosa embedded in the stent could not be removed by shrinking the SEMS with the recycling line alone, but the transparent cap could easily scrape the tissue; (3) removing the tissue with forceps may lead to bleeding; On the other hand, if forceps are hooked into the SEMS, it is difficult to remove the forceps; (4) if esophageal bleeding occurs, a transparent cap can be used to effectively suppress the bleeding; (5) the tissue could be scraped and pushed into the stomach along the SEMS with a transparent cap, which could reduce the likelihood of complication by aspiration pneumonia; and (6) the front of the transparent cap is soft and flexible, which is safe for interacting with residual varices. However, there are several limitations for using the transparent cap to adjust the stent: (1) Although the transparent cap can assist gastroscopy in successfully removing mucosa embedded in the stent, the stent may become embedded in the tissue again afterwards; and (2) if the patient often suffers from chest pain, gastroscopy may need to be performed regularly to observe the situation of the stent.
A transparent cap could assist the gastroscopy to remove the mucosa embedded the stent which was implanted for the stenosis after endoscopic injection of esophageal varices.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s classification
Scientific Quality: Grade C, Grade D
Novelty: Grade B, Grade D
Creativity or Innovation: Grade B, Grade C
Scientific Significance: Grade B, Grade C
P-Reviewer: Takemura N, Japan; Ueda H, Japan S-Editor: Liu H L-Editor: A P-Editor: Zhang XD
| 1. | de Franchis R, Primignani M. Endoscopic treatments for portal hypertension. Semin Liver Dis. 1999;19:439-455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 128] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 2. | Eisen GM, Baron TH, Dominitz JA, Faigel DO, Goldstein JL, Johanson JF, Mallery JS, Raddawi HM, Vargo JJ, Waring JP, Fanelli RD, Wheeler-Harbaugh J; Standards Practice Committe, American Society for Gastrointestinal Endoscopy. The role of endoscopic therapy in the management of variceal hemorrhage. Gastrointest Endosc. 2002;56:618-620. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Kalista KF, Hanif SA, Nababan SH, Lesmana CRA, Hasan I, Gani R. The Clinical Role of Endoscopic Ultrasound for Management of Bleeding Esophageal Varices in Liver Cirrhosis. Case Rep Gastroenterol. 2022;16:295-300. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 4. | Linghu EQ. [Endoscopic diagnosis and treatment of upper gastrointestinal hemorrhage caused by esophagus-gastric varice]. Zhonghua Xiaohuabing Yu Yingxiang Zazhi. 2012;2:1-3. [DOI] [Full Text] |
| 5. | Sami SS, Haboubi HN, Ang Y, Boger P, Bhandari P, de Caestecker J, Griffiths H, Haidry R, Laasch HU, Patel P, Paterson S, Ragunath K, Watson P, Siersema PD, Attwood SE. UK guidelines on oesophageal dilatation in clinical practice. Gut. 2018;67:1000-1023. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 103] [Cited by in RCA: 95] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 6. | Spaander MCW, van der Bogt RD, Baron TH, Albers D, Blero D, de Ceglie A, Conio M, Czakó L, Everett S, Garcia-Pagán JC, Ginès A, Jovani M, Repici A, Rodrigues-Pinto E, Siersema PD, Fuccio L, van Hooft JE. Esophageal stenting for benign and malignant disease: European Society of Gastrointestinal Endoscopy (ESGE) Guideline - Update 2021. Endoscopy. 2021;53:751-762. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 82] [Article Influence: 20.5] [Reference Citation Analysis (0)] |
| 7. | Fugazza A, Lamonaca L, Mercante G, Civilini E, Pradella A, Anderloni A, Repici A. The worst adverse event for an endoscopist after esophageal stent placement: an aortoesophageal fistula. Endoscopy. 2022;54:E44-E45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Singla V, Khare S, Arora A, Kumar A, Sharma P, Bansal N, Anikhindi SA. Use of loop and clips to prevent migration of esophageal stent. Endoscopy. 2021;53:E421-E422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Ou Y, Chen L, Li J, Ye Y, Chen Z, Cai L, Liao J. Endoscopic removal of a migrated esophageal covered self-expandable metal stent: the nylon loop pusher-assisted method. Endoscopy. 2022;54:E744-E745. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |