Published online Sep 26, 2017. doi: 10.5662/wjm.v7.i3.108
Peer-review started: February 8, 2017
First decision: June 12, 2017
Revised: July 22, 2017
Accepted: August 2, 2017
Article in press: August 2, 2017
Published online: September 26, 2017
Processing time: 240 Days and 15.1 Hours
To study the usefulness of orbital ultrasonography in the diagnosis of papilledema.
Fifty patients who were referred to the neurophthalmology clinic and clinically suspected to have papilledema were selected. Thorough, clinical examination with slitlamp biomicroscopy and visual acuity assessment was done. These patients underwent ultrasonography to demonstrate the crescent sign. The patients were further evaluated with the neurologist and magnetic resonance imaging (MRI) thus confirming the diagnosis of papilledema. The results of our ultrasonographic evaluation were correlated with final diagnosis after thorough clinical evaluation, imaging and the neurologist’s opinion.
Out of 50 patients diagnosed having papilledema on MRI, 46 (92%) showed crescent sign on B scan ultrasonography. Headache was most common presenting complaint in 47 (94%) and idiopathic intracranial hypertension was most common underlying cause of papilledema in 30 (60%) cases.
“Crescent sign” seen on ultrasonography is a sensitive tool for diagnosis of papilledema. It is cost effective, less cumbersome and effective tool to differentiate between papilledema and pseudo papilledema before subjecting the patients to costly investigations like MRI. A positive crescent sign should always be followed by MRI to find out the cause of papilledema.
Core tip: It is a retrospective study of 50 clinically diagnosed cases of papilledema where 46 cases showed a positive crescent sign on ocular ultrasonography. With an accuracy of 92%, ocular ultrasonography could be a cheaper and useful tool to confirm papilledema before subjecting these patients for MRI scans.
- Citation: Bhosale A, Shah VM, Shah PK. Accuracy of crescent sign on ocular ultrasound in diagnosing papilledema. World J Methodol 2017; 7(3): 108-111
- URL: https://www.wjgnet.com/2222-0682/full/v7/i3/108.htm
- DOI: https://dx.doi.org/10.5662/wjm.v7.i3.108
Patients of papilledema have acquired bilateral, optic nerve head swelling due to increased intracranial pressure[1]. Papilledema is an important reason of referral of patients to neuro-ophthalmology clinic. Suspicion of papilledema warrants timely ascertaining of its diagnosis, evaluation and management[2]. Differentiation between papilledema and pseudopapilledema is important as patients with papilledema need thorough work up whereas patients with pseudopapilledema often only need reassurance monitoring and follow-up. The presentation of papilledema patients is varied, some present with headache, transient visual blurring, etc. Pseudopapilledema might present with more severe and acute visual presentation. To differentiate these and confirmation of diagnosis is usually done by magnetic resonance imaging (MRI). MRI is a tedious, costly investigation. Ultrasonography is a safe, cost-effective, easily available, non-cumbersome modality for diagnosis of papilledema. There are very few studies done which demonstrate the value of ocular ultrasonography in diagnosis of papilledema. Some studies have shown increased optic nerve sheath width by orbital ultrasonography correlating well with the final diagnosis of papilledema or pseudo papilledema[3-5]. However all these studies measured the optic nerve width ranging anywhere from 3 mm to 3.3 mm to 5.7 mm along with 30° test. Measuring the optic nerve width and 30° test is difficult and requires an experienced ultrasonographer. None of the studies emphasized on the presence of “crescent” or “doughnut” sign alone, which is easier to elicit and does not require a very experienced or skilled ultrasonographer. Our study shows the effectiveness of eliciting the “crescent” sign on ocular ultrasonography in diagnosing papilledema, before subjecting them to costly investigations like MRI.
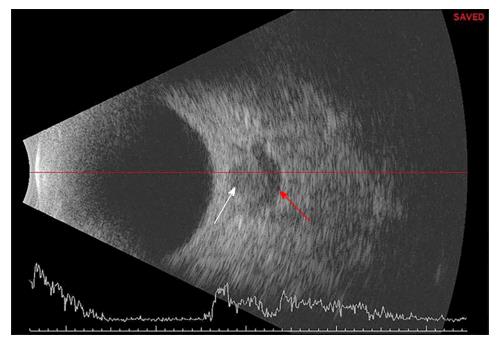
This was a retrospective study done in our institute from August 2015 to July 2016. Fifty patients diagnosed to have papilledema clinically, were included in this study. For each patient age, sex, duration of complaints, headache if present, associated systemic conditions were recorded. After measuring the visual acuity, all patients were clinically examined first by torch light, followed by slit lamp examination, intraocular pressure recording by applanation tonometry and a dilated fundus examination using 90 diopter lens. Informed consent was taken from all patients. Ocular ultrasonography using a 10 MHz probe (Sonomed Escalon E-Z Scan B5500+, Wayne, PA, United States) was performed on all in a supine position. If fluid was seen around the optic nerve, within the sheath, then it was noted as “crescent” or “doughnut” sign positive and it indicated presence of papilledema (Figure 1). All patients were referred to a neurologist and all crescent sign positive cases were subjected to neuro imaging. SPSS version 16.0 software was used for the statistical analysis.
The average age of presentation was 30 years (range 6 to 60 years). There were 37 (74%) females and only 13 (26%) males. Headache was the most common presenting complaint seen in 47/50 (94%) cases. Transient visual loss and diplopia were other complaints in very few cases. The duration of symptoms ranged from four days to 4 years. The most common systemic association was hypertension and diabetes mellitus in 3 patients (6%) each. Seventy-six percent (n = 38) patients out of 50 had no systemic disease.
Out of the 50 diagnosed cases of papilledema 46 showed positive “crescent sign” on ultrasonography. Thus the sensitivity of orbital ultrasonography in diagnosing papilledema was 92% (n = 46). Neuro imaging was done in all these cases and the most common cause of papilledema on MRI was idiopathic intracranial hypertension (IIHT) in 30 cases (60%) followed by space occupying lesions (SOL) in 8 (16%). Of the SOL cases, four had tumours in posterior cranial fossa, one in frontal lobe, two had meningiomas and one had craniopharyngioma. Sinus thrombosis was seen in 9 cases (18%). The common sinuses involved were sagittal sinus, sigmoid sinus and transverse sinus. Two patients had Grade IV hypertension retinopathy associated papilledema while one patient had multilocular hydrocephalus post shunt surgery. All these three cases along with one case of IIHT had normal ultrasonography (false negatives).
Papilledema is an important reason for emergency referral for patient to neurophthalmology clinic[6]. However, sometimes it is difficult to differentiate papilledema from pseudo papilledema and patient has to be subjected MRI for confirmation of diagnosis[7]. Cost, time duration, difficulties in claustrophobic and metal implants patients make it a tedious investigation. Ocular ultrasonographic measurement of optic disc width along with 30° test and presence of fluid around the optic nerve as a “crescent” or “doughnut” sign has been shown to be useful in confirming papilledema. However these tests, especially measurement of optic disc width and 30° test, require a cooperative patient with an experienced ultrasonographer and these tests are also time consuming. Eliciting the crescent sign alone is faster, has a shorter learning curve and can be done even by a less experienced ultrasonographer. In our study crescent sign was seen in 46/50 cases with a 92% sensitivity, which proves ultrasound B scan is a sensitive tool in initial diagnosis of papilledema. Sensitivity was 90%, 95% and 100% in studies by Neudorfer et al[3], Carter et al[4] and Mehrpour et al[5] respectively. However all these studies took a combination of measuring optic nerve width, 30° test and presence of crescent sign. Our study shows that presence of crescent sign alone has a good sensitivity of 92%. The advantage of eliciting the crescent sign is that it is faster and easier to perform compared to the other two tests. Four cases in our study had false negative scans. Of these two had grade IV hypertensive retinopathy (where we don’t expect to have positive crescent sign), one case was with IIHT and another one had hydrocephalus post shunt surgery. In a single case by Sadda et al[8] the patient had bilateral disc edema with positive crescent sign on ocular ultrasonography but the patient was symptomless with normal intracranial pressure and normal MRI. None of our cases showed false positivity.
Other investigative modalities like optical coherence tomography (OCT) and fluorescein angiography have also been studied in the diagnosis of papilledema[9,10]. However, retro orbital anatomy cannot be imaged by OCT and fluorescein angiography has disadvantage of being invasive.
In conclusion, our study demonstrates, “crescent sign” on ultrasound for diagnosis of papilledema a highly sensitive tool in differentiating papilledema from pseudo papilledema before subjecting the patients to more costly, tedious and time consuming investigative modalities like MRI. A positive crescent sign should always be followed by MRI to find out the cause of papilledema.
Papilledema is a critical ocular sign which could be devastating and can lead to permanent disability. Confirmation of diagnosis is usually done by magnetic resonance imaging (MRI), which is a tedious, costly investigation.
Ocular ultrasonography is a cost-effective, easily available, non-cumbersome, safe modality for diagnosis of papilledema.
There are very few studies done which demonstrate the value of ocular ultrasonography in diagnosis of papilledema. However all these studies measured the optic nerve width along with 30° test. Measuring the optic nerve width and 30° test is difficult and requires an experienced ultrasonographer. None of the studies emphasized on the presence of “crescent” or “doughnut” sign alone, which is easier to elicit and does not require a very experienced or skilled ultrasonographer. This study shows the effectiveness of eliciting the “crescent” sign on ocular ultrasonography in diagnosing papilledema.
The study results suggest that “crescent sign” seen on ocular ultrasonography is a sensitive and cost effective tool for diagnosis of papilledema.
Papilledema is a serious condition of the eye which can have devastating complications. The infective organisms reach the ocular tissues via the blood stream. Ocular ultrasonography is readily available instrument with ophthalmologists. It is less cumbersome and can be quickly performed.
This study has valuable data that would be of interest if published.
Manuscript source: Invited manuscript
Specialty type: Medical laboratory technology
Country of origin: India
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Ni Y, Nowak MS S- Editor: Kong JX L- Editor: A E- Editor: Li D
| 1. | Friedman DI. Papilledema. Walsh and Hoyt’s Clinical Neuro-Ophthalmology, 6th Ed. Baltimore: Lippincott Williams and Wilkins 2005; 237-291. |
| 2. | Savino PJ, Glaser JS. Pseudopapilledema versus papilledema. Int Ophthalmol Clin. 1977;17:115-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 13] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Neudorfer M, Ben-Haim MS, Leibovitch I, Kesler A. The efficacy of optic nerve ultrasonography for differentiating papilloedema from pseudopapilloedema in eyes with swollen optic discs. Acta Ophthalmol. 2013;91:376-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 31] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 4. | Carter SB, Pistilli M, Livingston KG, Gold DR, Volpe NJ, Shindler KS, Liu GT, Tamhankar MA. The role of orbital ultrasonography in distinguishing papilledema from pseudopapilledema. Eye (Lond). 2014;28:1425-1430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 5. | Mehrpour M, Oliaee Torshizi F, Esmaeeli S, Taghipour S, Abdollahi S. Optic nerve sonography in the diagnostic evaluation of pseudopapilledema and raised intracranial pressure: a cross-sectional study. Neurol Res Int. 2015;2015:146059. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 6. | Tso MO, Hayreh SS. Optic disc edema in raised intracranial pressure. IV. Axoplasmic transport in experimental papilledema. Arch Ophthalmol. 1977;95:1458-1462. [PubMed] |
| 7. | Agid R, Farb RI, Willinsky RA, Mikulis DJ, Tomlinson G. Idiopathic intracranial hypertension: the validity of cross-sectional neuroimaging signs. Neuroradiology. 2006;48:521-527. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 178] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 8. | Sadda SR, DiBernardo C, Miller NR. Anomalous optic disc elevation associated with ultrasonographic evidence of increased subarachnoid fluid. J Neuroophthalmol. 2000;20:25-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Pineles SL, Arnold AC. Fluorescein angiographic identification of optic disc drusen with and without optic disc edema. J Neuroophthalmol. 2012;32:17-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 64] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 10. | Sakata LM, Deleon-Ortega J, Sakata V, Girkin CA. Optical coherence tomography of the retina and optic nerve - a review. Clin Exp Ophthalmol. 2009;37:90-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 170] [Article Influence: 10.6] [Reference Citation Analysis (0)] |