Published online Mar 20, 2025. doi: 10.5662/wjm.v15.i1.92943
Revised: August 16, 2024
Accepted: August 26, 2024
Published online: March 20, 2025
Processing time: 229 Days and 13.6 Hours
Pain in the back or pelvis or fear of back pain may affect the timing or co-contraction of the core muscles. In both static and dynamic movements, the Sahrmann core stability test provides an assessment of core muscle activation and a person's ability to stabilize the lumbopelvic complex. Preparatory cues and images can be used to increase the activation of these muscles. To attain optimal movement patterns, it will be necessary to determine what cueing will give the most effective results for core stability.
To investigate the effects of external and internal cues on core muscle activation during the Sahrmann five-level core stability test.
Total 68 participants (21.83 ± 3.47 years) were randomly allocated to an external
Linear mixed effects model analysis showed that cueing had a significant effect on core muscle activation (P = 0.001); however, there was no significant difference between cue types (internal or external) (P = 0.130).
Both external and internal cueing have significant effects on core muscle activation during the Sahrmann five-level core stability test and the PBU does not create higher muscle activation than internal cueing.
Core Tip: Lumbopelvic pain can alter optimal sequencing of muscle activation leading to inadequate synergies and disrupted biomechanics within the lumbopelvic region. Retraining to regain optimal sequencing through external and internal cues can help an individual return to their prior level of function and improve optimal movement patterns. Although this study was conducted in healthy young subjects, we conclude that the use of internal and/or external cues when retraining abdominal core muscles in individuals with lumbopelvic pain would be beneficial to increase core muscle activation.
- Citation: Stifter S, McCaffrey J, Nichols T, Ozcan Edeer A, Ward J. Effect of external and internal cues on core muscle activation during the Sahrmann five-level core stability test. World J Methodol 2025; 15(1): 92943
- URL: https://www.wjgnet.com/2222-0682/full/v15/i1/92943.htm
- DOI: https://dx.doi.org/10.5662/wjm.v15.i1.92943
The core is defined as the area of the body between the diaphragm and pelvic floor and consists of two layers[1]. The superficial layer embodies the rectus abdominis (RA), internal oblique (IO), and external oblique (EO), while underneath lies the deep musculature which consists of the diaphragm, pelvic floor, multifidus, and the transverse abdominis (TA)[1]. These muscles work together in a prescribed sequence to provide the lumbopelvic region stability during movement. More specifically, the transverse abdominis is shown to pre-activate 30-100 ms prior to the prime mover during upper or lower extremity movement. In those with lumbopelvic pain, this pre-activating mechanism is shown to be dormant, leading to the presentation of pain[2]. Research has shown that lumbopelvic pain can alter optimal sequencing of muscle activation, which leads to inadequate synergies, as well as disrupted biomechanics within the lumbopelvic region[1,3]. After an individual no longer has pain, deficits within the core stability muscles are still present, and therefore must be retrained. If training is not done properly, the continued use of non-optimal strategies can lead to further deficits, pain, or inability to return to one’s prior level of functioning[1]. There are a variety of ways to retrain these muscles, but the best method is still unknown.
One of the main priorities during the rehabilitation process is to regain a healthy and stable lumbopelvic complex, as lack of core stability has been shown to be a key contributor in causing lumbopelvic pain. Core stability is defined as the ability of the lumbopelvic-hip complex to return to equilibrium following a perturbation without buckling of the vertebral column[4]. The muscles that play a key role in maintaining this equilibrium are the superficial IO, EO, and RA, and the deep TA. These muscles must work in synchrony to provide stability to the skeletal structures in the lumbopelvic region[1].
The Sahrmann five-level core stability test consists of five levels of different lower extremity movements that gradually increase the challenge to the core stability muscles[4,5]. This test has been shown to provide a means of evaluating core muscle activation, and a person’s ability to stabilize the lumbopelvic complex during both static and dynamic movements[6,7]. Traditionally, the Sahrmann five-level core stability test is used as an assessment tool to help guide treatment planning. The test's movements can then be used as a core stabilization exercise for individuals with non-optimal lumbo-pelvic stabilization. Physical therapists use techniques, such as facilitation, to improve the performance of core muscles. These techniques include palpation, muscle stretching, and verbal commands, as well as contraction of different muscle groups to utilize over-flow into the target muscle[1,8].
Lee[1] suggests the use of preparatory cues during retraining for proper activation of each muscle. Of the many cues and strategies rehabilitation therapists use to improve muscle activation, this study focuses on the use of internal and external cues. An internal cue focuses on the movement, whereas an external cue focuses on the effect or outcome of a movement[7,9,10]. Electromyography (EMG) activity has measured both increases and decreases to muscle activation dependent on the type of facilitatory technique used[8]. The effects of external and internal focus of attention during vertical jumping were investigated by Wulf et al[9], and it was found that external focus increased neuromuscular coordination in lower extremities.
Researchers have found that the pressure biofeedback unit (PBU) can be used to evaluate core stability during lower extremity movements, and it has a good intra-examiner and inter-examiner reliability when assessing lumbopelvic stability during lower extremity movements (ICC > 0.75)[11,12]. A PBU can be used when assessing treatment outcomes that are directed towards improving lumbopelvic stability[12].
No study to date has explored the effects that external and internal cues have on muscle activation during the Sahrmann five-level core stability test. The authors hypothesized that an external cue would yield greater core muscle activation when given during the Sahrmann five-level core stability test, compared to an internal cue. Therefore, the purpose of this study was to investigate the effect of external and internal cues on core muscle activity of the RA, EO, and transverse abdominis/internal oblique (TA/IO) during the Sahrmann five-level core stability test and provide updated wisdom to health professionals to further improve rehabilitation techniques for enhancing core stability.
Total 77 healthy young subjects were recruited from May 2021 to November 2021. Data from 68 subjects was used for the statistical analysis for this randomized clinical study. Two participants were excluded based on exclusion criteria, and seven participants were excluded due to lost data on the EMG WorksAnalysis software. Participants were included if they were 18-35 years old. Participants were excluded if they had recent abdominal surgery, spinal operations, hip abnormalities that limited hip range of motion, neurological disorders, excessive subcutaneous abdominal tissue, history of low back pain within the last three months or were pregnant at the time of the study or two years prior[4,13-15]. Researcher 2 instructed each participant to choose a folded piece of paper that contained a hidden number out of a box which randomly allocated participants into two groups. All participants received cueing based on original group allocation. Group 1 received an external cue and group 2 received an internal cue. The mean age of group 1 was 21.86 ± 3.16 years old, and the mean age of group 2 was 21.79 ± 3.08 years old. Table 1 presents the participants’ demographics. Informed consent was signed electronically, and a demographic information sheet was filled out by each participant prior to participation in the study. All data collection occurred at Dominican University of New York in Orangeburg, NY, United States. No harm was caused to any participants during data collection.
| Group 1 (External cue) | Group 2 (Internal cue) | ||||
| n | % | n | % | ||
| Gender | Male | 13 | 37.14 | 11 | 33.33 |
| Female | 22 | 62.68 | 22 | 66.67 | |
| Athlete | Yes | 13 | 37.15 | 10 | 30.3 |
| No | 22 | 62.85 | 23 | 69.70 | |
| Exercise | 0 days/week | 8 | 22.86 | 6 | 18.18 |
| 1-2 days/week | 11 | 31.42 | 13 | 39.4 | |
| 3-4 days/week | 12 | 34.29 | 12 | 36.36 | |
| 5-7 days/week | 4 | 11.43 | 2 | 6.06 | |
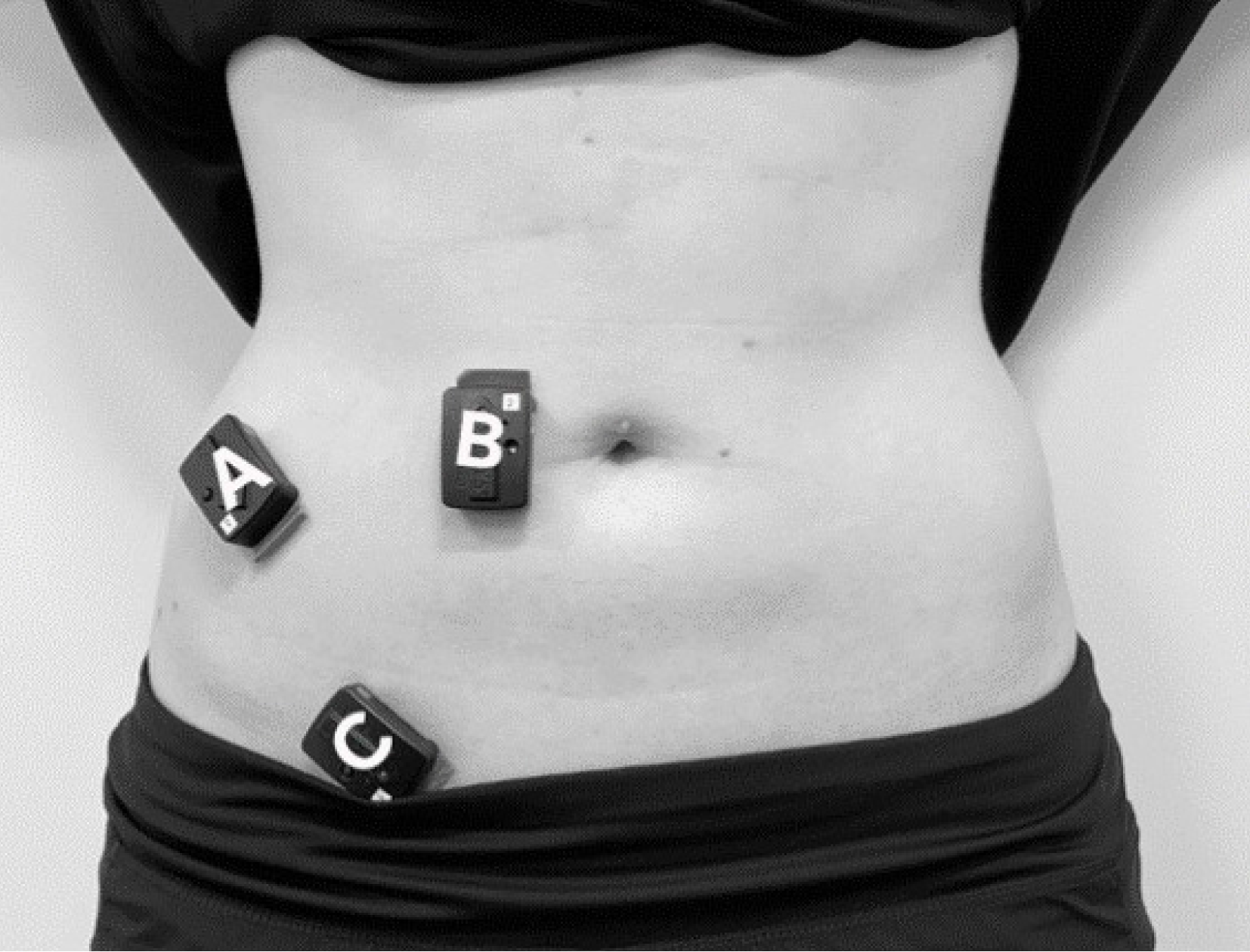
The muscle activation of RA, TA/IO, and EO muscles was measured using the wireless TrignoTM surface electro
Both groups performed the Sahrmann five-level core stability test two times: Pre-intervention, and post-intervention (external or internal cue). For the pre-intervention test, all five levels were presented through a video which demonstrated how to correctly perform each exercise. Level 1 video was presented, then the participant performed the exercise. Once in the final position of the level, the exercise was held for 10 seconds. There was a 1-minute rest period between each of the five levels, which was when the video for the next exercise was shown[4]. This procedure was then repeated for the remaining four levels. Baseline measurements (pre-intervention) were taken for each of the five levels of the Sahrmann core stability test. Once baseline EMG measurements were taken and after the 1-minute-resting-period, the entire testing process occurred with the addition of one of the two interventions based on group allocation.
The independent variables in this study were internal and external cues. To ensure consistent delivery of each cue, researcher 1 pre-recorded each cue, which were then presented to each participant depending on the group assignment. Group 1 received an audio of the external cue which utilized the PBU. Group 2 received an audio of the internal cue which focused on activation of the core and pelvic floor muscles.
For group 1 (external cue), the PBU was placed at lumbar spine segments L4-L5 by researcher 2. In a supine position, the objective was to help individuals maintain core muscle activation during each level of exercise (Figure 2). Prior to inflation, the participants were asked to position themselves into level 1 exercise of the Sahrmann five levels where the PBU was then inflated to 40 mmHg[1,8]. Once each participant was ready to perform the exercise, the pre-recorded external cue instructed the participants to “keep the dial within 10 mmHg from the original 40 mmHg”[6].
Group 2 (internal cue) received a combination of two internal cues via pre-recorded audio, one focused on core muscle activation, “bring your anterior superior iliac spine together,” and one focused on pelvic floor muscle activation, “draw your anus to your pubic bone.”
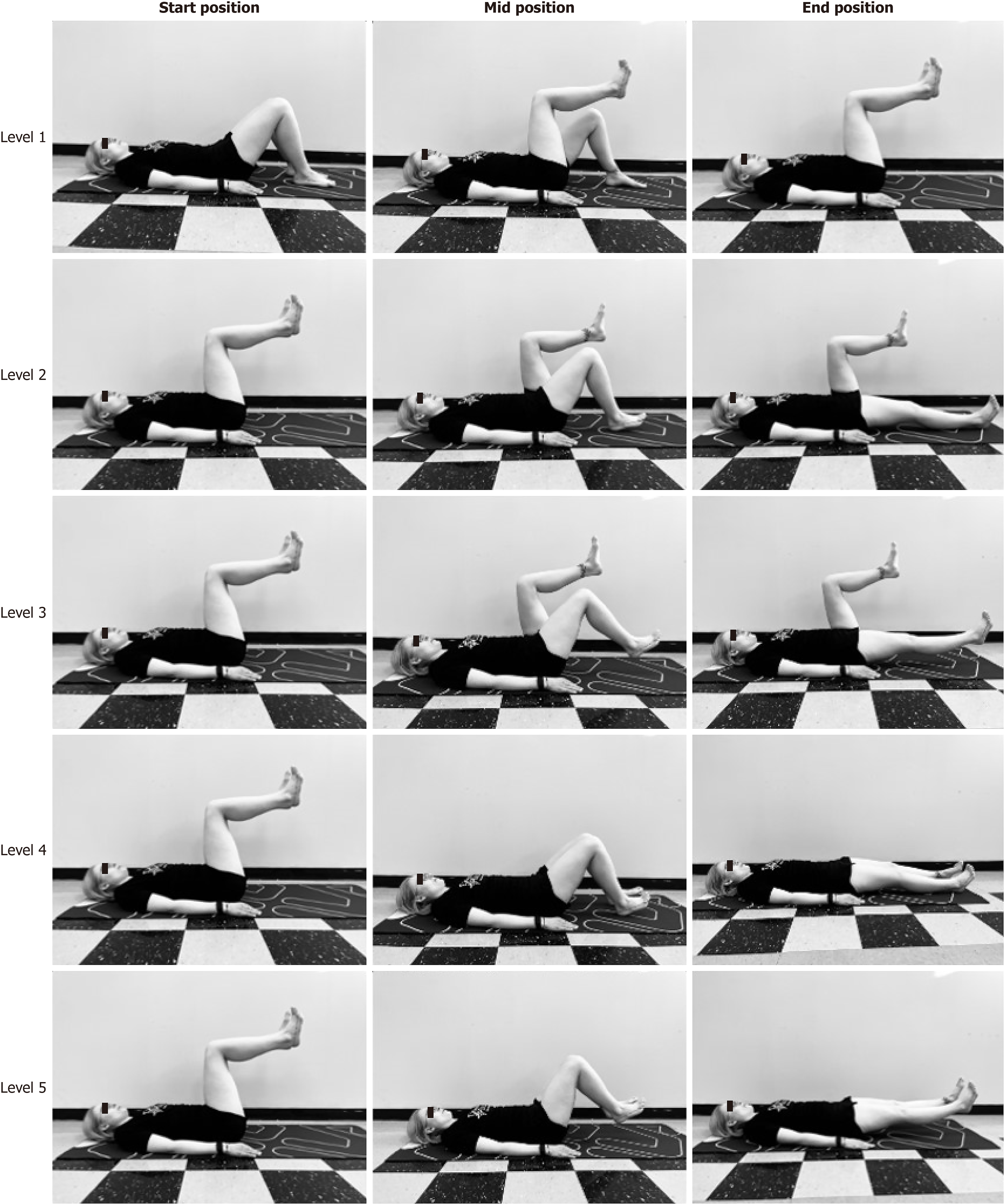
The internal or external audio cue was played for each participant prior to the video demonstrating the exercise during the 1-minute rest-period. Researcher 3 performed all required tasks using the sEMG machine and data software. Table 2 and Figure 3 provide a description and picture of each exercise level respectively.
| Levels | Description |
| Level 1 | The participant will slowly raise one leg to a position of approximately 90º hip flexion and 90º knee flexion. The participant will then attempt to bring the opposite leg to the same position in the same manner (i.e. “final position”) |
| Level 2 | From the final position of level 1, the participant will slowly lower one leg, so the heel contacts the ground/plinth. Then the leg will slide out until the knee is fully extended |
| Level 3 | From the final position of level 1, the participant will slowly lower one leg, so the heel is approximately 12 cm above the plinth. Then the leg will slide out until the knee is fully extended |
| Level 4 | From the final position of level 1, the participant will slowly lower both legs together as the heels are contacting the plinth. Then the legs will slide out until the knee is fully extended |
| Level 5 | From the final position of level 1, the participant will slowly lower both legs simultaneously until they are approximately 12 cm above the plinth. Then the legs will slide out until the knees are fully extended |
sEMG data were recorded by the EMGWorks® Acquisition program and then processed and analyzed using the EMGWorks Analysis program (Trigno, Delsys, Boston, United States) during the Sahrmann five-level core stability test. Root mean square data was recorded as millivolt (mV) for data analysis. Baseline data were collected at each level, then again with a cue as interventional data. Data was collected while the participants held the final position for 10 seconds. Data from EMGWorks Analysis was exported to Microsoft Office Excel (Redmond, WA, United States) and reviewed by all researchers to detect and exclude outliers prior to data analysis. Standard deviations of the data were used to detect outliers, with the lower limit being three standard deviations below the mean and the upper limit being three standard deviations above the mean. Data points falling outside this range were detected as outliers.
Linear mixed effects model with BOBYQA optimization and REML estimation was used for statistical analysis where muscle activation (mV) was included as the dependent variable and repeated measurements in participants included as random grouping factor. Cueing (with cue and without cue), exercise levels (1 to 5) and muscles (TA/IO, EO and RA) were included as fixed grouping factors. Degrees of freedom were obtained by the Satterthwaite method. Bonferroni correction was used for post-hoc tests following significant main and interaction effects. The robustness of the main analysis was evaluated by the inspection of the distribution of residuals and by QQ plots. R programming was used for statistical analyses. The significance value was set at P < 0.05.
The study started with 77 participants with a sample consisting of 68 (44 female, 64.7%) after considering exclusion criteria and lost data (Table 3). The effects of cueing (with and without cue), exercise levels (1 to 5) and muscle groups (TA/IO, EO, RA) were analyzed to assess the change in muscle activation (mV). The main effects of cueing (F(1, 1922.96) = 5.998, P = 0.0014), muscle groups (F(2, 1922.97) = 19.807, P < 0.0001 and exercise levels (F(4, 1922.96) = 67.199, P < 0.0001) were statistically significant on the muscle activation (mV). The model accounted for 34% of the variance in muscle activity. There were statistically significant interaction effects between cueing and exercise levels (F(4, 1922.93) = 3.346, P = 0.009), and muscles and exercise levels (F(8, 1922.94) = 2.303, P = 0.018) (see Table 3 for main effects and interactions).
| Effect | P value | df | F |
| Cueing (with and without cue) | 0.014a | 1, 1922.96 | 5.99 |
| Cue type (external and internal cue) | 0.1306 | 1, 2.3438 | 65.80 |
| Muscle groups (TA/IO, EO and RA) | 0.000b | 2, 1922.97 | 19.80 |
| Exercise levels (level 1, II, III, IV, V) | 0.0001b | 4, 1922.96 | 67.19 |
| Cueing and muscle interaction | 0.177 | 2, 1922.95 | 1.73 |
| Cueing and exercise level interaction | 0.009a | 4, 1922.93 | 3.35 |
| Muscle and exercise level interaction | 0.018a | 4, 1922.93 | 2.30 |
| Cueing and muscle and exercise level interactions | 0.091 | 4, 1922.93 | 1.71 |
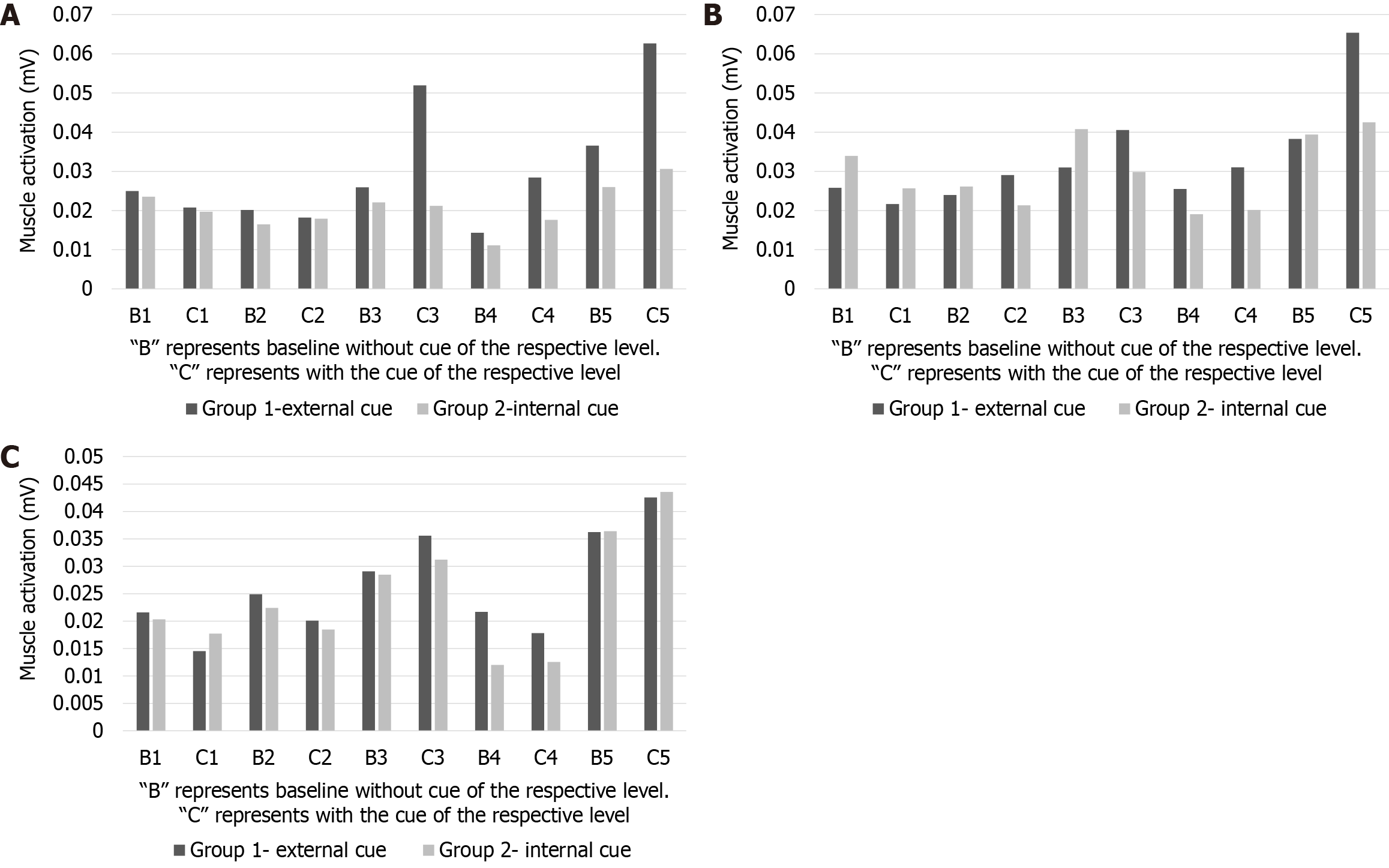
Further inspections of main effects showed that the muscle activation (mV) is higher in “with cue” than “without cue” (MD = -0.002, SE = 0.001, df = 1923, P = 0.0144). However, there was no significant effect of cue type (internal or external) (F(1, 65.80) = 2.3438, P = 0.1306) on the muscle activation (mV).
The breakdown of the main effect of muscle groups on the muscle activation (mV) showed that RA > EO = TA/IO and RA vs TA/IO comparisons (P < 0.0001). The further analysis of muscle to exercise level interactions within the same exercise level revealed that the activation in RA muscle is significantly higher than TA muscle at level 5 exercise only (P < 0.001).
Post-hoc comparisons showed that the effects of exercise levels on muscle activation were significantly different (Level 1 = Level 2 = Level 4 < Level 3 < Level 5, P < 0.001 for all significant comparisons).
All muscles, RA, TA/IO, EO showed similar muscle activation during each level exercise, there was no statistically significant muscle X level interactions (P > 0.05) (Figure 4A-C).
The primary endpoint of this study was to determine whether internal or external cueing had a greater effect on core abdominal muscle activity during the Sahrmann five-level core stability test. This study specifically looked at the RA, TA/IO, and EO muscle activations throughout each of the five levels using a sEMG. In our study, both internal and external cues were found to increase muscle activation at all five levels, with no significant differences when comparing internal and external cues.
It has been suggested that levels 1-5 of the Sahrmann five-level core stability test sequentially increase the demand of abdominal muscle activation[4-6]. A previous study assessed abdominal muscle activity during the Sahrmann five-level core stability test and found levels 5 and 3 have significantly higher abdominal EMG signals than levels 4, 2, and 1[4,5]. This prior study supports the findings in our study, although our study showed level 5 to have significantly higher muscle activation compared to all other levels, followed by level 3, with and without cueing. Similarly, in Chan et al’s study level 5 and 3 created statistically significantly more muscle activation than level 1, 2, and 4[4]. Our study revealed level 1, 2, and 4 to have no statistically significant differences in muscle activation when comparing all three muscles with and without cueing. It could be hypothesized that during levels 1, 2 and 4, since the heels are in constant contact with the floor, there is not as high of a demand for muscle activation secondary to the lower extremities being supported. In contrast, during levels 3 and 5, there is a higher demand for muscle activation due to unsupported lower extremities and gravity forces acting against the muscles.
The results of our study showed that internal and external cueing significantly increased EMG muscle activation at all levels; however, there were no significant differences in muscle activation when comparing the internal cue vs. the external cue. A PBU can be used when assessing treatment outcomes that are directed towards improving lumbopelvic stability[12]. Our study also suggests that a PBU is a good instrument to provide as an external cue, as it helped to improve core muscle activation, however the improvements in muscle activation were similar to the internal cue. Therefore, we conclude that during core stability exercises either internal or external cues can help to increase core muscle activation.
Zachry et al[10] compared an external (basket) and internal (wrist motion) cue on the EMG activity of the upper extremity muscles during a basketball free throw. The authors concluded that an external focus of attention enhances movement economy as they found the external focus of attention reduced EMG activity. It can be argued that the disparity between Zachry et al's and our study can be explained by the fact that in our study, internal and external cues were administered specifically to optimize EMG muscle activation during the specific Sahrmann five-level core stability exercises, while Zachry et al's study focused on movement results[10]. A study conducted by Kristiansen et al[19] found that both internal and external cues increased mean and peak EMG activity when performing a bench press exercise. Similar to our study, they concluded that neither an internal or external cue was superior to increasing muscle activation.
An abdominal drawing in maneuver (ADIM) is another technique to engage core musculature, specifically the TA, to increase lumbopelvic stabilization by creating, “an inward movement of the lower abdominal wall”[20]. Lynders found participants responded better when an ADIM was provided as an external cue, compared to Mani et al[20] who found an internal cue created better core activation[21]. Although the cues provided are not the exact same, the goal of the ADIM is similar to that of the internal and external cues provided in our study, which all aim to increase core stabilization[21]. Mani et al[20] found when an internal cue is mastered, an ADIM can train the anatomical girdle to fire automatically, providing dynamic spinal stabilization during routine and athletic activities. A study by Selkow et al[22] found ADIM’s to increase activation and timing of TA during exercises using real-time ultrasound and found a carryover effect following a 4-week training period. Our study revealed that when internal or external cues were used to activate the core muscles during a single session of the Sahrmann five-level core stability test, the core muscles were activated more with cues than without cues. The movements of the Sahrmann five-level core stability test can be used as an exercise to improve lumbo-pelvic stability in various patient populations. We can hypothesize that if individuals perform the Sahrmann five-level core stability exercises with internal and external cues over a 4-week period, there is a potential for carryover effect of muscle activation which can cause optimal improvements on lumbopelvic stabilization. This hypothesis is supported by Hlaing et al[23], who found using a PBU with ADIM improves abdominal muscle activation through real-time ultrasound, which improved balance and spinal stability.
The whole core, including the pelvic floor muscles, diaphragm, RA, TA/ IO and EO must be coactivated to magnify the potential for maximal core stabilization[4]. In a systematic review on core muscle activity during physical fitness exercises by Oliva-Lozano and Muyor[24], it is indicated there is a lack of research regarding TA activation, as the research studies in the literature used the sEMG muscle activations obtained mainly from RA, EO, IO muscles. Since TA is a deep core muscle, an intramuscular EMG electrode is required to detect isolated TA muscle activation. We used a surface EMG sensor to detect TA muscle activation with the combination of IO muscle activation defined by Chan et al[4]. In our study, it is possible that the EMG signals using a surface electrode from the TA/IO electrode were largely from the superficial IO muscle rather than the deep TA muscle.
When comparing the different muscles during a single exercise level, our findings revealed that RA muscle activation was significantly more prominent when compared to EO and TA/IO. Our findings slightly differ from Oliva-Lozano and Muyor's systematic review, which showed RA, EO, and erector spinae muscles had the greatest activity during free-weight exercises, and IO muscles had the greatest activity during core stability exercises[17]. One way to explain our findings is that the Sahrmann five-level core stability exercises consist of five levels of different lower extremity movements and have a higher alignment with RA muscle activation such as trunk flexion and drawing the pubic symphysis toward sternum, and does not require active trunk rotations, which is more aligned with IO and EO muscle activations.
This study has a few limitations that need to be addressed. Although TA is considered a primary stabilizer of the lumbar spine, we couldn’t collect data directly from TA using wired intramuscular (EMG) electrodes. The pelvic floor muscles are also an integral part of the core stabilization system. We were unable to measure EMG activity of the pelvic floor muscles due to lack of available surface or internal EMG sensors, and the potential perceived invasive nature of measuring this muscle group in our study population. Additionally, all participants in our study were healthy, young subjects, and we therefore cannot generalize our results to other populations. We must also acknowledge the audio cues used in our study may be difficult to generalize to the broader population. The cues, “bring your anterior superior iliac spine together,” and “draw your anus to your pubic bone,” were appropriate for our study population, as most of the participants were physical therapy students with a baseline understanding of human anatomy. However, in future studies, it would be recommended to use cueing such as, “roll your abdominals inward as if you are zipping up a tight pair of pants”, or “imagine as if you are trying to stop the flow of urine.” Our study used both internal and external cues, while some other learning styles were not considered, including kinesthetic and tactile learning. As there may be differences in learning styles among individuals, when teaching exercise or movement patterns to different populations, it is important to consider their personal perception/learning. Another minor limitation noted during this study was increased perspiration which occasionally warranted replacement of the adhesive strips on the electrodes mid-study.
Recommendations for future studies include: (1) Examine the effects of internal and external cueing during the Sahrmann five-level core stability test in those with lumbopelvic dysfunction; (2) Assess deep core muscles’ activation through intramuscular EMG sensors; and (3) Provide better visual depiction of when the heels need to be in contact with the ground, specifically between levels 2 and 3 and levels 4 and 5.
This is the first study that investigates the effects of internal and external cues on abdominal muscle activation during the Sahrmann five-level core stability test and highlights the importance of using cues to improve core muscle activation in healthy subjects. The literature is clear that activation patterns of core musculature are altered in individuals with lumbopelvic pain. The use of internal and external cues during therapeutic exercise is a skilled intervention unique to physical therapists and is particularly important when treating individuals with lumbopelvic instability and/or hypermobility.
To conclude, our intervention of cueing was found to have statistical significance on muscle activation across all levels of exercise. Although our results were statistically significant, it cannot be concluded whether an internal or external cue has a greater effect on core muscle activation. Optimizing core activation through external or internal cueing can help augment effects of core exercises and improve disrupted biomechanics within the lumbopelvic region.
The authors thank Dr. Umit Tural for his statistical analysis and advice on experimental design, and Kaeli Ward for editing the manuscript.
| 1. | Lee D. Core training vs strengthening. Retrieved February 28, 2021. Available from: https://dianeleephysio.com/education/core-training-vs-strengthening/. |
| 2. | Marshall P, Murphy B. The validity and reliability of surface EMG to assess the neuromuscular response of the abdominal muscles to rapid limb movement. J Electromyogr Kinesiol. 2003;13:477-489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 183] [Cited by in RCA: 190] [Article Influence: 8.6] [Reference Citation Analysis (1)] |
| 3. | Kumar T, Kumar S, Nezamuddin M, Sharma VP. Efficacy of core muscle strengthening exercise in chronic low back pain patients. J Back Musculoskelet Rehabil. 2015;28:699-707. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 35] [Article Influence: 3.9] [Reference Citation Analysis (2)] |
| 4. | Chan EWM, Hamid MSA, Nadzalan AM, Hafiz E. Abdominal muscle activation: An EMG study of the Sahrmann five-level core stability test. Hong Kong Physiother J. 2020;40:89-97. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (1)] |
| 5. | Sahrmann S. Diagnosis and Treatment of Movement Impairment Syndromes. 1st ed. St. Louis, MO: Mosby, 2002. Available from: https://evolve.elsevier.com/cs/product/9780801672057?role=student. |
| 6. | Faries MD, Greenwood M. Core Training: Stabilizing the Confusion. J Strength Cond. 2007;29:10. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Porter JM, Anton PM, Wikoff NM, Ostrowski JB. Instructing skilled athletes to focus their attention externally at greater distances enhances jumping performance. J Strength Cond Res. 2013;27:2073-2078. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 39] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 8. | Critchley D. Instructing pelvic floor contraction facilitates transversus abdominis thickness increase during low-abdominal hollowing. Physiother Res Int. 2002;7:65-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 86] [Article Influence: 3.7] [Reference Citation Analysis (1)] |
| 9. | Wulf G, Dufek JS, Lozano L, Pettigrew C. Increased jump height and reduced EMG activity with an external focus. Hum Mov Sci. 2010;29:440-448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 128] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 10. | Zachry T, Wulf G, Mercer J, Bezodis N. Increased movement accuracy and reduced EMG activity as the result of adopting an external focus of attention. Brain Res Bull. 2005;67:304-309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 266] [Cited by in RCA: 232] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 11. | Aggarwal A, Kumar S, Madan R, Kumar R. Relationship among different tests of evaluating low back core stability. J Musculoskelet Res. 2011;14:1250004. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Azevedo DC, Lauria AC, Pereira AR, Andrade GT, Ferreira ML, Ferreira PH, Van Dillen L. Intraexaminer and interexaminer reliability of pressure biofeedback unit for assessing lumbopelvic stability during 6 lower limb movement tests. J Manipulative Physiol Ther. 2013;36:33-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 13. | Ferreira PH, Ferreira ML, Hodges PW. Changes in recruitment of the abdominal muscles in people with low back pain: ultrasound measurement of muscle activity. Spine (Phila Pa 1976). 2004;29:2560-2566. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 326] [Cited by in RCA: 306] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 14. | Krause DA, Youdas JW, Hollman JH, Smith J. Abdominal muscle performance as measured by the double leg-lowering test. Arch Phys Med Rehabil. 2005;86:1345-1348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 28] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 15. | Wu WH, Meijer OG, Uegaki K, Mens JM, van Dieën JH, Wuisman PI, Ostgaard HC. Pregnancy-related pelvic girdle pain (PPP), I: Terminology, clinical presentation, and prevalence. Eur Spine J. 2004;13:575-589. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 418] [Cited by in RCA: 328] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 16. | Trigno Wireless Biofeedback System User Guide. 2021. Available from: https://www.delsys.com/downloads/USERSGUIDE/trigno/wireless-biofeedback-system.pdf. |
| 17. | Merletti R, Aventaggiato M, Botter A, Holobar A, Marateb H, Vieira TM. Advances in surface EMG: recent progress in detection and processing techniques. Crit Rev Biomed Eng. 2010;38:305-345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 99] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 18. | Escamilla RF, Babb E, DeWitt R, Jew P, Kelleher P, Burnham T, Busch J, D'Anna K, Mowbray R, Imamura RT. Electromyographic analysis of traditional and nontraditional abdominal exercises: implications for rehabilitation and training. Phys Ther. 2006;86:656-671. [PubMed] [DOI] [Full Text] |
| 19. | Kristiansen M, Samani A, Vuillerme N, Madeleine P, Hansen EA. External and Internal Focus of Attention Increases Muscular Activation During Bench Press in Resistance-Trained Participants. J Strength Cond Res. 2018;32:2442-2451. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 20. | Mani P. Abdominal Drawing in Maneuver: Effect on Gait Parameters and Pain Reduction in Patients with Chronic Low Back Pain. Int J Physiother. 2016;3. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 21. | Lynders C. The Critical Role of Development of the Transversus Abdominis in the Prevention and Treatment of Low Back Pain. HSS J. 2019;15:214-220. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 22. | Selkow NM, Eck MR, Rivas S. Transversus abdominis activation and timing improves following core stability training: A randomized trial. Int J Sports Phys Ther. 2017;12:1048-1056. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 23. | Hlaing SS, Puntumetakul R, Khine EE, Boucaut R. Effects of core stabilization exercise and strengthening exercise on proprioception, balance, muscle thickness and pain related outcomes in patients with subacute nonspecific low back pain: a randomized controlled trial. BMC Musculoskelet Disord. 2021;22:998. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 74] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 24. | Oliva-Lozano JM, Muyor JM. Core Muscle Activity During Physical Fitness Exercises: A Systematic Review. Int J Environ Res Public Health. 2020;17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 56] [Article Influence: 11.2] [Reference Citation Analysis (0)] |