Published online Dec 20, 2024. doi: 10.5662/wjm.v14.i4.95210
Revised: May 18, 2024
Accepted: June 13, 2024
Published online: December 20, 2024
Processing time: 112 Days and 22.9 Hours
The remission of type 2 diabetes mellitus (T2DM) is a topic that has been widely discussed recently, and it gives new hope for people with T2DM. Achievement of normal blood glucose levels or levels below the diagnostic threshold for T2DM without pharmacotherapy among people with T2DM after metabolic surgery and carbohydrate or calorie-restricted diet paved the way for more enthusiastic research in this area. There is a lot of confusion regarding the appropriate terminology and definition of remission of T2DM. In this short review, we briefly analyzed the emerging concepts and proposed criteria for diagnosing remission of T2DM, which will be helpful for healthcare providers and people with T2DM.
Core Tip: There is a lot of confusion regarding the criteria for remission of type 2 diabetes mellitus (T2DM), as it is described differently by various professional bodies. Therefore, we proposed criteria that will be useful for healthcare professionals worldwide for diagnosing remission. Five components should be satisfied to diagnose remission of T2DM: Previous diagnosis of T2DM; blood sugar normalization or level below the diagnostic threshold for T2DM; withdrawal of pharmacotherapy or inter
- Citation: Raveendran AV. Remission of type 2 diabetes mellitus: Emerging concepts and proposed diagnostic criteria. World J Methodol 2024; 14(4): 95210
- URL: https://www.wjgnet.com/2222-0682/full/v14/i4/95210.htm
- DOI: https://dx.doi.org/10.5662/wjm.v14.i4.95210
The remission of type 2 diabetes mellitus (T2DM) is a topic that is widely discussed not only among healthcare professionals but also among the public[1]. Present reports of achievement of normal glucose levels without pharmacotherapy among people with T2DM after metabolic surgery and carbohydrate or calorie-restricted diet paved the way to more enthusiastic research in this area. There is a lot of confusion regarding the appropriate terminology. Various professional bodies define remission of T2DM differently, again adding to the confusion among healthcare providers and the public[2].
Various terminologies used in this aspect include reversal, resolution, cure and remission. T2DM resolution implies that an entirely normal state has been established permanently. Cure of T2DM gives the impression that the patho
| Terminology | Word meaning | Blood sugar target for remission | Pathophysiological status | Follow-up |
| Resolution | The subsidence of a pathological state | Attained | Permanent normalization | No |
| Cure | A complete or permanent solution | Attained | Permanent normalization | No |
| Reversal | A change from one state to the opposite state | Attained | Permanent normalization | No |
| Remission | An abatement or reduction in intensity or degree (as in the manifestations of a disease) | Attained | Improvement | Yes |
In people with T2DM, insulin resistance, hyperinsulinemia, and subsequent hyperglycemia are the predominant pathophysiology in the early stages followed by deterioration of beta cell function and insulinopenia in the later part of the disease. Any measures reducing insulin resistance like weight reduction will result in improvement in hyperglycemia and even normalization of blood sugar value. Similarly, any measures that improve insulin secretion also improve hyperglycemia in people with T2DM. In addition, reduction in the insulin requirement will also help to control blood glucose value even at the stage of insulinopenia.
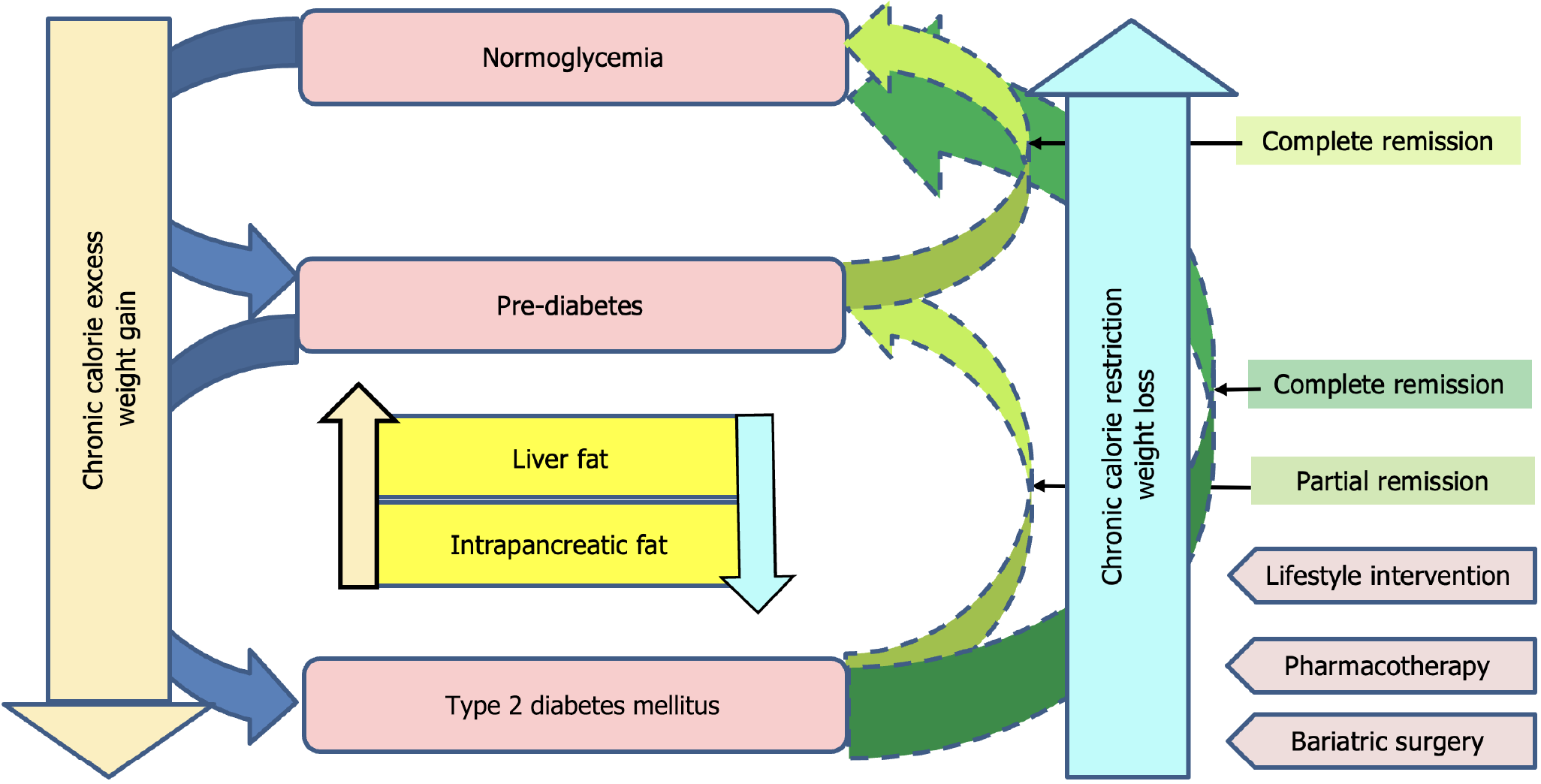
As per the twin cycle hypothesis, chronic calorie excess leads to the accumulation of fat in the liver and subsequently in the pancreas[6] (Figure 1). Accumulation of fat in the liver leads to hepatic insulin resistance and in the pancreas leads to impaired insulin secretion. When fat deposition exceeds the “personal fat threshold” of that person, they develop T2DM[7].
Based on the twin cycle hypothesis, weight reduction is associated with improvement in fatty infiltration of the liver and pancreas, thereby improving insulin resistance and insulin secretion, which is responsible for remission of T2DM as per the current concepts[8]. Significant weight loss (about 15 kg) is an important factor in predicting the chance of remission.
The remission of T2DM is not just the normalization of glycemic status in the absence of active therapeutic intervention. Improvement in glycemic status is the reflection of improvement in the pathophysiological aspect of T2DM, i.e. improvement in insulin secretion and insulin resistance. Therefore, the extent and duration of normalization of blood sugar depends upon the extent of improvement of insulin resistance and improvement in insulin secretion. Hence people with T2DM who achieved remission require regular monitoring to identify the re-emergence or relapse of T2DM.
The extent of normalization of glycemic status remission can either be partial remission or complete remission[9] (Figure 1). Depending upon the duration of remission achieved we classify it into transient remission, short-term remission, long-term remission, and prolonged remission. Those without established T2DM, i.e. pre-diabetes, can also achieve normalization of glycemic status, usually as complete remission.
Euglycemia achieved because of continuous carbohydrate restriction only lasts as long as carbohydrate restriction is maintained. This is called ‘state of mitigation’ and has to be differentiated from remission[10].
In people with T2DM, normalization of the blood sugar value can persist for variable periods after temporary use of pharmacotherapy because of improvement in the deleterious effect of poor metabolic control on insulin secretion and action (e.g., glucotoxicity and lipotoxicity) without altering the basic pathophysiology of T2DM. This should not be confused with remission, as there is no improvement in the pathophysiologic mechanism. Remission of T2DM has to be differentiated from mere normalization of blood glucose levels.
To define remission, people with previously diagnosed T2DM should have sustained normal blood glucose values (complete remission) or below the diagnostic threshold for T2DM (partial remission) by any means like blood glucose testing [fasting blood sugar (FBS), post prandial blood sugar (PPBS), random blood sugar, oral glucose tolerance test], glycated hemoglobin (HbA1c), continuous glucose monitoring (CGM) values, estimated A1c (eA1c level), or glucose management indicator (GMI). Each method has its advantages and limitations.
Blood sugar values (e.g., FBS, PPBS, random blood sugar) undergo wide fluctuation and show significant variation between repeated measurements. Similarly, 2-h post-glucose after 75 g oral glucose load is also associated with high variability between repeated measurements[11]. FBS and CGM values are more variable, and some experts recommend repeated testing to confirm remission. In those with post-bariatric surgery, there is early hyperglycemia followed by later hypoglycemia making interpretation of 2-h post-glucose value difficult[5].
HbA1c is an inaccurate indicator of glycemic status in certain conditions like anemia, with abnormalities of red blood cell survival, those with hemoglobin variants, splenomegaly, asplenia, uremia, severe hypertriglyceridemia, etc[12,13].
CGM values can be used to diagnose remission. eA1c or GMI can be calculated from it and used to establish remission. HbA1c of < 48 mmol/mol (< 6.5%) calculated from 24-h CGM values can be used to denote remission[5].
Ideally, HbA1c, FPG, 2-h PPBS, CGM, eA1c, and GMI all should be within normal limits or below the level for the diagnosis of T2DM to diagnose remission. However, it is practically very difficult and time-consuming to measure all these parameters to establish remission. There is a subset of people with T2DM having normal FBS and high 2-h PPBS. If we measure only FBS in such individuals and diagnose remission, it will be a false diagnosis of remission. A similar situation can happen in people with high FBS and normal 2-h PPBS levels. Even though it is not practical to do all these measurements, it is always better to select the test that has the maximum chance to detect any blood sugar value above the cutoff in that particular patient. If there is any probability of getting a false value with any of the above methods, another alternative modality has to be used to confirm remission.
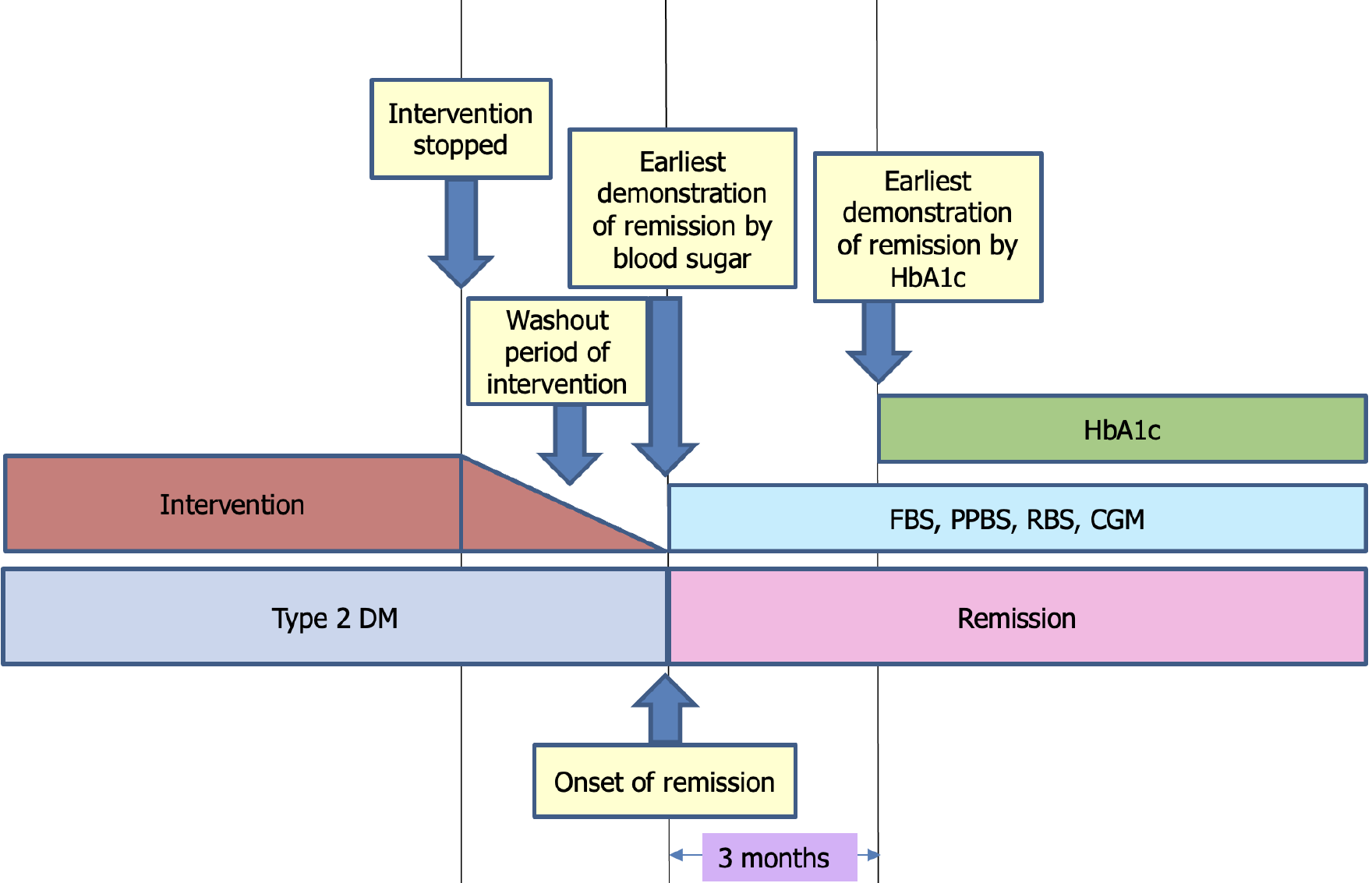
While selecting a particular test to demonstrate normoglycemia, one should consider the inherent property of the test, like the duration of the glycemic status that particular test represents (Figure 2). For example, HbA1c reflects the glycemic status of the last 3-4 mo. Therefore, if we do HbA1c before 3 mo of stopping anti-diabetic treatment, we will get a false low HbA1c, indicating remission even when it is actually not present. HbA1c has to be done after a minimum of 3 mo after the washout period of a particular intervention.
Similarly, tests to assess normoglycemia should not be performed before completing the washout period of a pharmacotherapy or intervention (Figure 2). For almost complete elimination of any medication, it usually takes four to five half-life periods (t ½). For example, the t ½ of metformin is 17.6 h, and usually it will take five t ½ (5 × 17.6 h = 98.6 h) for the medicine to be almost completely eliminated from the body[14]. So FBS, PPBS, and CGM should not be done to demonstrate normoglycemia after stopping therapy before 98.6 h in people who stopped metformin.
Once remission is achieved, it is difficult to predict how long it will persist. But there are a lot of factors like duration of T2DM, body weight, β cell function, etc that help to assess the feasibility of remission. The duration of remission is a retrospective assessment. Those who maintain 5 years of remission are said to have achieved prolonged remission[9].
The durability of remission varies with the interventions, and bariatric surgery usually gives long-lasting remission compared to other modalities[15]. It is better to mention the intervention adopted to achieve remission than simply mentioning remission of T2DM (e.g., remission of T2DM achieved by bariatric surgery).
Diet control and exercise are integral parts of treatment of T2DM. Hence it is called non-pharmacological therapy, medical nutrition therapy, etc. Another important concern while defining criteria for remission of T2DM is whether one can continue non-pharmacological therapy like dietary intervention and exercise.
In an ideal condition, remission of T2DM requires persistent normalization of blood sugar values even after withdrawal of all the interventions (pharmacological and non-pharmacological), so that its direct blood sugar-lowering action will be washed out. However, all the current definitions do not require the withdrawal of non-pharmacological interventions like diet control and exercise to define remission[1,2]. In our opinion, it is better to add maintained with diet control and/or exercise to the diagnosis of T2DM remission to understand the ongoing interventions and to emphasize the need for continuing diet control and exercise to maintain remission.
Another important concern is about the withdrawal of interventions or pharmacotherapy. Some guideline says that the patient should be off all anti-diabetic medication, while others say it is ok to continue medication like metformin if it was started for a non-glycemic indication[1,2]. Examples of such medications, started for a non-glycemic indication that have beneficial effects on blood sugar levels include liraglutide for obesity, SGLT-2 inhibitors for heart failure and renal protection, and metformin for polycystic ovary syndrome.
Even if the drugs that reduce blood sugar are started for non-glycemic indications, it is not advisable to stop these drugs just to confirm remission, which would increase the risk of complications of the underlying problem for which the medication was started. But for those who are on these medications, even if the blood glucose parameters are within normal limits, we cannot ideally consider it as remission and is better categorized as incomplete remission.
The effect of pharmacotherapy or bariatric surgery is evident quickly. However, lifestyle intervention is slow (requires more time), and it may require up to 6 mo to stabilize the effect[5]. Again, 3 mo is required for the HbA1c to reflect these changes[5]. Follow-up HbA1c monitoring should not be done more frequently than every 3 mo and not less than every year. Compared to HbA1c, FBS or eA1c derived from CGM stabilizes early and can be used to monitor early. However, as these values are more variable, it should be confirmed by repeated measurement. Even though we need a 3-mo period to diagnose remission, tests that reflect glycemic control early can be used to document remission after the washout period of pharmacotherapy/intervention, even before completing the 3-mo period.
For those with poorly controlled T2DM, rapid reduction in blood sugar and HbA1c may result in worsening of microvascular complications like retinopathy[5]. Hence rapid reduction of HbA1c in people with retinal changes beyond microaneurysms (more than background retinopathy) is not advised. However, this risk is less after metabolic surgery[17].
Weight gain, stress, poor sleep, and inability to maintain a healthy lifestyle and diet may result in relapse of T2DM in those who already achieved remission. Metabolic memory-like phenomena can occur even after remission, resulting in the development of classical complications of T2DM after remission. Those who achieved remission need regular medical supervision not only to monitor glycemic status but also complications like retinopathy, neuropathy, nephropathy, and cardiovascular complications[5,16].
We reviewed the literature on remission of T2DM and found that there are no clear-cut criteria to diagnose remission, though partial and complete remission is already described. To diagnose remission, first we have to confirm T2DM, for which we adopted the American Diabetes Association diagnostic criteria to define T2DM and pre-diabetes[18]. Those achieving blood sugar below the cutoff for T2DM and pre-diabetes are defined as partial and complete remission, respectively. Since there is no clear consensus about the duration of normalization of blood sugar, the interventions adapted to achieve remission, any ongoing interventions, and improvement in pathophysiological mechanisms, we tried to define these parameters. Any conditions resulting in transient hyperglycemia can be misdiagnosed as remission of T2DM. To avoid this, we defined exclusion criteria for the diagnosis of remission. We expect that the proposed criteria will be helpful for healthcare providers and people with T2DM worldwide.
Our diagnostic criteria contain five components, and all five components should be satisfied to make a diagnosis of remission of T2DM (Table 2).
| A: Establishing the diagnosis of T2DM/pre-diabetes | ||||
| Documented evidence of T2DM based on established criteria like ADA criteria | ||||
| Diagnosis | HbA1c | FPG | 2-h PG | |
| T2DM | ≥ 6.5%; ≥ 48 mmol/mol | ≥ 126 mg/dL; ≥ 7 mmol/L | ≥ 200 mg/dL; ≥ 11.1 mmol/L | |
| Pre-diabetes | 5.7% to 6.4%; 39 to 47 mmol/mol | 100 to 125 mg/dL; 5.6 to 6.9 mmol/L | 140 to 199 mg/dL; 7.8 to 11.0 mmol/L | |
| B: Evidence of maintenance of blood sugar below the threshold for T2DM or normal range (biochemical remission) in people with established T2DM even after the withdrawal of pharmacotherapy/active intervention | ||||
| Remission | HbA1c | FPG | 2-h PG | |
| Partial | 5.7% to 6.4%; 39 to 47 mmol/mol | 100 to 125 mg/dL; 5.6 to 6.9 mmol/L | 140 to 199 mg/dL; 7.8 to 11.0 mmol/L | |
| Complete | < 5.7%; < 39 mmol/mol | < 100 mg/dL; < 5.6 mmol/L | < 140 mg/dL; < 7.8 mmol/L | |
| One or more components needed to establish remission | ||||
| C: Duration criteria for the intervention and for the test | ||||
| Normoglycemia persists even after the withdrawal of glucose-lowering intervention (pharmacotherapy/active intervention), which is documented after a reasonable washout period | ||||
| Glucose-lowering intervention can be non-pharmacological (medical nutrition therapy or physical activity) or pharmacological intervention (medication or surgical intervention) | ||||
| No ongoing pharmacological or surgical procedure (ongoing procedures like repeated placement of endoluminal devices or intragastric balloon) | ||||
| If any medication that can reduce blood sugar is continued for non-glycemic indication, it is considered incomplete remission | ||||
| Duration criteria for the intervention | ||||
| Drugs after washout period (after five t ½ of the drug) | ||||
| Lifestyle modification takes 3-6 mo to stabilize its effect | ||||
| Duration criteria for the tests | ||||
| HbA1c after 3 mo of washout period of intervention | ||||
| FBS/PPBS/RBS/CGM after 24 h of washout period of intervention | ||||
| Duration of remission is a retrospective assessment. Depending upon the duration of remission | ||||
| Normoglycemia persisting | ||||
| 3-6 mo: Transient remission | ||||
| 6 mo-1 yr: Short-term remission | ||||
| 1-5 yr: Long-term remission | ||||
| More than 5 yr: Prolonged remission | ||||
| D: Evidence of improvement of the pathophysiological mechanism | ||||
| Improvement in insulin resistance and β cell function | ||||
| Indirect evidence of this is significant weight loss, about 15 kg | ||||
| E: Satisfy exclusion criteria | ||||
| Normalization of blood sugar value in people with T2DM is not due to any complications (e.g., nephropathy or hepatic dysfunction) or comorbid disease that causes reduced appetite, weight loss, or hypoglycemia (e.g., sepsis, adrenal or pituitary disease, malignancy) | ||||
| Exclusion of stress hyperglycemia, gestational diabetes, or transient hyperglycemia | ||||
| Exclusion of hyperglycemia due to any medications: Drug-induced diabetes (e.g., steroid, anti-malarial drugs, atypical antipsychotics, protease inhibitors) | ||||
Establishing the diagnosis of T2DM/ pre-diabetes: As per the criteria, a clear diagnosis of T2DM is a prerequisite for the diagnosis of remission. We use the American Diabetes Association diagnostic criteria to define T2DM[18]. Any transient hyperglycemia misdiagnosed as T2DM results in an erroneous diagnosis of remission.
Evidence of maintenance of normal blood sugar or blood sugar below the threshold for T2DM: Biochemical remission in people with established T2DM in the absence of any active intervention. Demonstration of normal glycemic parameters or blood sugar below the threshold for T2DM is an essential component of the diagnosis of remission. Various parameters like FBS, PPBS, HbA1c, eA1c, CGM, GMI, etc can be used to document remission. All these tests are associated with their own merits and limitations. If there is any chance for a false result of a particular test in the patient (e.g., HbA1c in people with anemia), an alternative test has to be done to demonstrate remission. A single type of test (e.g., PPBS) may not reflect glycemic status in some patients. In such a situation, multiple types of tests are required (e.g., PPBS may be low in people who underwent metabolic surgery, and FBS or CGM may sometimes pick up abnormal blood sugar values).
Duration criteria: For the intervention and for the test. Persistence of normoglycemia even after the withdrawal of glucose-lowering intervention (pharmacotherapy/active intervention) is documented after a reasonable period to wash out the direct effect of medication or intervention. The glucose-lowering intervention can be non-pharmacological (medical nutrition therapy or physical activity) or pharmacological intervention (medication or surgical intervention). There should not be any ongoing pharmacological or surgical procedures (ongoing procedures like repeated placement of endoluminal devices or intragastric balloons). However, non-pharmacological (medical nutrition therapy or physical activity) interventions are continued in most of the reports of remission. Should non-pharmacological interventions (medical nutrition therapy or physical activity) be discontinued to diagnose remission? Ideally, the answer is yes. But for all practical purposes, the answer is no. In our opinion in people who achieved remission and continue non-pharmacological interventions, it is better to mention that remission is maintained with diet control and/or exercise.
The testing should be scheduled in such a way that the value must reflect the glycemic status after the washout period of the intervention (e.g., HbA1c after 3 mo of washout period of intervention). Similarly, the washout period of the intervention also has to be considered while scheduling the test. Usually after pharmacological therapy washout period is after five t ½ of that particular drug.
Duration of remission is a retrospective assessment. A minimum of 3 mo of maintenance of blood sugar below the specified level is required to categorize it as remission. Remission for more than 5 years is called prolonged remission. We classify remission as transient, short-term, long-term, and prolonged if it lasts less than 6 mo, 6 mo to 1 year, 1-5 years, and more than 5 years, respectively.
Evidence of improvement of the pathophysiological mechanism: Normalization of the blood sugar value as a result of improvement in insulin secretion and insulin resistance helps to differentiate remission from mitigation. Significant weight loss is considered as indirect evidence of loss of fat from the liver and pancreas resulting in improvement in insulin secretion and insulin resistance. Therefore, weight loss is considered as evidence of improvement of the pathophysiological mechanism.
Satisfy exclusion criteria: Exclusion of transient hyperglycemia and improvement after removal of precipitating event or drugs (e.g., stress hyperglycemia, drug-induced hyperglycemia), normalization of blood sugar due to complications (e.g., diabetic kidney disease), and comorbidities or concomitant illness (like malignancy, sepsis, or endocrine disorders) are important to avoid false categorization as remission of T2DM.
In a person with established T2DM, if there is an achievement of glycemic status below the pre-diabetes range (partial remission) or within the normal limit (complete remission) and satisfying duration, pathophysiological improvement, and exclusion criteria, we can categorize it as remission (Table 3). Those not satisfying pathophysiological improvement criteria have to be categorized as T2DM mitigation. Those satisfying all these criteria but medications that can reduce blood sugar are continued for the non-glycemic indication are categorized as incomplete remission (incomplete partial remission if blood sugar is in the pre-diabetes range and incomplete remission if blood sugar is in the normal range).
| Diagnosis of T2DM/pre-diabetes | Evidence of biochemical remission | Antidiabetic treatment/ongoing intervention | Duration criteria | Reversal of pathophysiologic mechanism | Exclusion criteria | Interpretation |
| Yes | Complete | No | + | + | + | Complete remission |
| Partial | Partial remission | |||||
| Yes | Complete | Yes, but for non-glycemic indication | + | + | + | Incomplete remission |
| Partial | Incomplete partial remission | |||||
| No | Complete/partial | No | +/- | +/- | +/- | Transient hyperglycemia. No remission. Improvement in risk factors |
| Yes | Complete/partial | No | + | - | + | State of mitigation/T2DM mitigation |
Achievement of normal glucose levels or levels below the threshold for the diagnosis of pre-diabetes without pharmacotherapy among people with T2DM after metabolic surgery and carbohydrate or calorie-restricted diet can result in remission. The twin cycle hypothesis helps to understand the pathophysiological mechanism leading to remission. The lack of clear-cut criteria for diagnosing remission is a challenge healthcare professionals are facing now. As per our proposed criteria, five components should be satisfied to diagnose remission of T2DM. Our proposed criteria will be useful for healthcare professionals worldwide for diagnosing remission.
| 1. | Holst JJ, Madsbad S. What is Diabetes Remission? Diabetes Ther. 2021;12:641-646. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (74)] |
| 2. | Kalra S, Singal A, Lathia T. What's in a Name? Redefining Type 2 Diabetes Remission. Diabetes Ther. 2021;12:647-654. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 3. | “Remission.” Merriam-Webster.com Dictionary, 2024; Merriam-Webster, Accessed 8 Jun. 2024. Available from: https://www.merriam-webster.com/dictionary/remission. |
| 4. | "Remission." Available from: Vocabulary.com Dictionary, 2024; Vocabulary.com, Accessed 08 Jun. 2024. https://www.vocabulary.com/dictionary/remission. |
| 5. | Riddle MC, Cefalu WT, Evans PH, Gerstein HC, Nauck MA, Oh WK, Rothberg AE, le Roux CW, Rubino F, Schauer P, Taylor R, Twenefour D. Consensus Report: Definition and Interpretation of Remission in Type 2 Diabetes. Diabetes Care. 2021;44:2438-2444. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 91] [Cited by in RCA: 242] [Article Influence: 60.5] [Reference Citation Analysis (0)] |
| 6. | Taylor R. Pathogenesis of type 2 diabetes: tracing the reverse route from cure to cause. Diabetologia. 2008;51:1781-1789. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 209] [Cited by in RCA: 215] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 7. | Taylor R, Holman RR. Normal weight individuals who develop type 2 diabetes: the personal fat threshold. Clin Sci (Lond). 2015;128:405-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 84] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 8. | Taylor R, Ramachandran A, Yancy WS Jr, Forouhi NG. Nutritional basis of type 2 diabetes remission. BMJ. 2021;374:n1449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 29] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 9. | Buse JB, Caprio S, Cefalu WT, Ceriello A, Del Prato S, Inzucchi SE, McLaughlin S, Phillips GL 2nd, Robertson RP, Rubino F, Kahn R, Kirkman MS. How do we define cure of diabetes? Diabetes Care. 2009;32:2133-2135. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 726] [Cited by in RCA: 728] [Article Influence: 45.5] [Reference Citation Analysis (0)] |
| 10. | Brown A, McArdle P, Taplin J, Unwin D, Unwin J, Deakin T, Wheatley S, Murdoch C, Malhotra A, Mellor D. Dietary strategies for remission of type 2 diabetes: A narrative review. J Hum Nutr Diet. 2022;35:165-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 37] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 11. | Garonzi C, Maguolo A, Maffeis C. Pros and Cons of Current Diagnostic Tools for Risk-Based Screening of Prediabetes and Type 2 Diabetes in Children and Adolescents with Overweight or Obesity. Horm Res Paediatr. 2023;96:356-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 13] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 12. | Alzahrani BA, Salamatullah HK, Alsharm FS, Baljoon JM, Abukhodair AO, Ahmed ME, Malaikah H, Radi S. The effect of different types of anemia on HbA1c levels in non-diabetics. BMC Endocr Disord. 2023;23:24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 16] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 13. | Sherwani SI, Khan HA, Ekhzaimy A, Masood A, Sakharkar MK. Significance of HbA1c Test in Diagnosis and Prognosis of Diabetic Patients. Biomark Insights. 2016;11:95-104. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 792] [Cited by in RCA: 685] [Article Influence: 76.1] [Reference Citation Analysis (0)] |
| 14. | Hallare J, Gerriets V. Half Life. [Updated 2023 Jun 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK554498/. |
| 15. | Isaman DJ, Rothberg AE, Herman WH. Reconciliation of Type 2 Diabetes Remission Rates in Studies of Roux-en-Y Gastric Bypass. Diabetes Care. 2016;39:2247-2253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (1)] |
| 16. | Murphy R, Jiang Y, Booth M, Babor R, MacCormick A, Hammodat H, Beban G, Barnes RM, Vincent AL. Progression of diabetic retinopathy after bariatric surgery. Diabet Med. 2015;32:1212-1220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 44] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 17. | Singh RP, Gans R, Kashyap SR, Bedi R, Wolski K, Brethauer SA, Nissen SE, Bhatt DL, Schauer P. Effect of bariatric surgery vs intensive medical management on diabetic ophthalmic outcomes. Diabetes Care. 2015;38:e32-e33. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 18. | American Diabetes Association Professional Practice Committee. 2. Diagnosis and Classification of Diabetes: Standards of Care in Diabetes-2024. Diabetes Care. 2024;47:S20-S42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 316] [Cited by in RCA: 640] [Article Influence: 640.0] [Reference Citation Analysis (1)] |