Published online Sep 20, 2024. doi: 10.5662/wjm.v14.i3.91497
Revised: May 14, 2024
Accepted: May 29, 2024
Published online: September 20, 2024
Processing time: 178 Days and 20.9 Hours
Retinoscopy is arguably the most important method in the eye clinic for diagn
To discuss the history of retinoscopes and examine current literature on the subject.
A search was conducted on the PubMed and with the reference citation analysis (https://www.referencecitationanalysis.com) database using the term “Retino
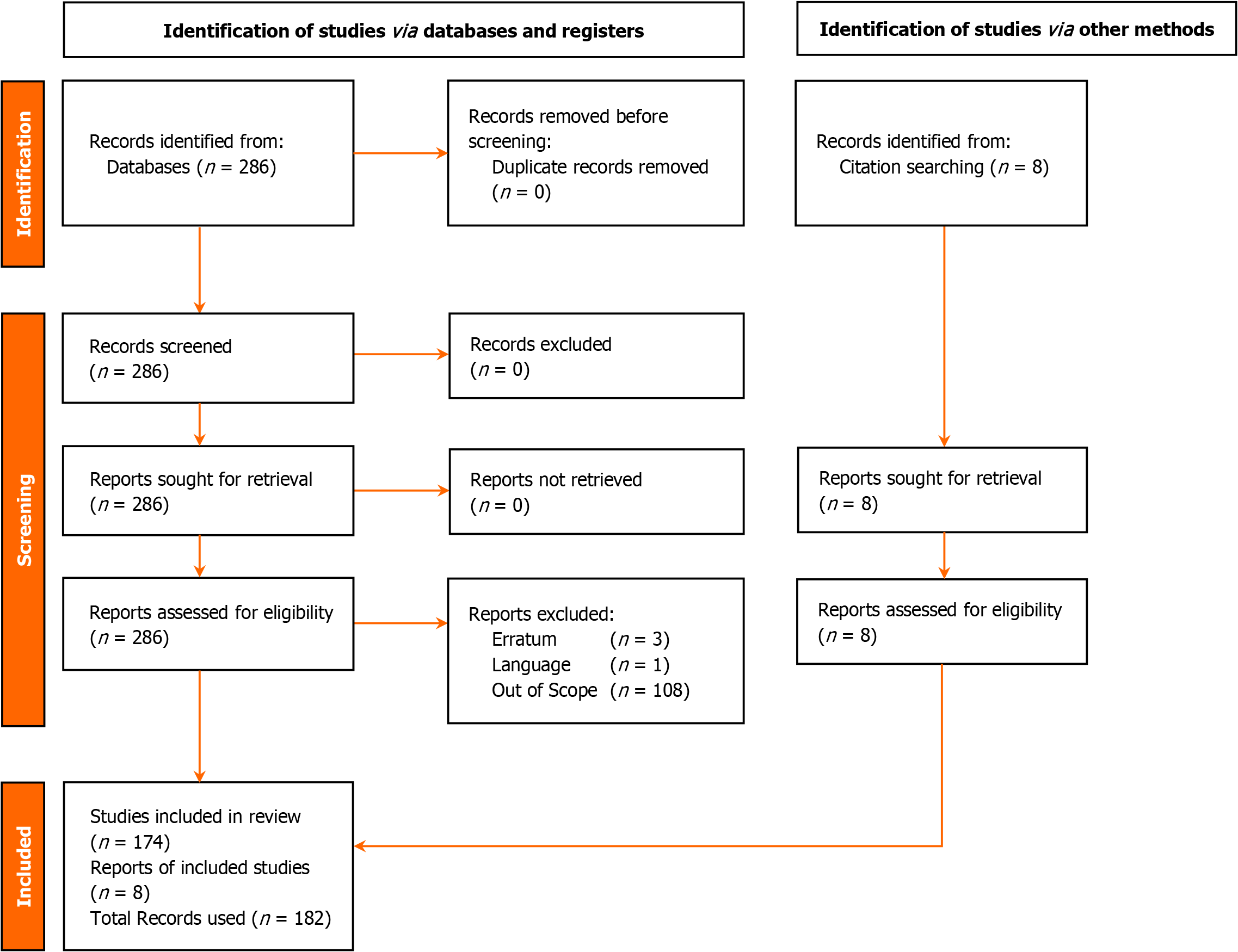
This systematic review included a total of 286 records. Publications reviewed iterations of the retinoscope into autorefractors, infrared photo retinoscope, television retinoscopy, and the Wifi enabled digital retinoscope.
The retinoscope has evolved significantly since its discovery, with a significant improvement in its diagnostic capabilities. While it has advantages such as non-invasiveness and broad applicability, limitations exist, and the need for skilled interpretation remains. With ongoing research, including the integration of artificial intelligence, retinoscopy is expected to continue advancing and playing a vital role in eye care.
Core Tip: Retinoscopy is an important method used in the eye clinic for identifying and treating refractive problems. It has several benefits, such as being non-invasive, evaluating patients of all ages, and being helpful for individuals with poor cooperation or communication abilities. It is very helpful in the diagnosis of diseases like cataracts and amblyopia. New features have been added to retinoscopes as a result of technological advances. Contemporary retinoscopes come with digital screens, which make it simpler to analyze the findings. Others have combined the advantages of both with integrated autorefractor capabilities. Retinoscopes have evolved in the past decades to meet the current clinic needs.
- Citation: Musa M, Enaholo E, Bale BI, Salati C, Spadea L, Zeppieri M. Retinoscopes: Past and present. World J Methodol 2024; 14(3): 91497
- URL: https://www.wjgnet.com/2222-0682/full/v14/i3/91497.htm
- DOI: https://dx.doi.org/10.5662/wjm.v14.i3.91497
Refractive errors are the leading cause of visual impairment worldwide[1]. Estimation of refractive errors can be carried out objectively or subjectively. Objectively, refraction is carried out by retinoscopy and auto-refractometry.
The retinoscope works on the principle of detecting the movement of a light beam reflected from the patient's retina. By analyzing the direction and speed of the reflected light, clinicians can determine the refractive error, such as myopia, hyperopia, or astigmatism. By their optical function, retinoscopes may also be improvised for the detection of multiple unestablished anterior segment pathologies, including aiding differential diagnosis of several subtypes of immature cataracts in low-resource clinical ophthalmic settings by observing differences in motions exhibited by lens opacities against the background red reflex. All illuminated portable devices can be used for this subjective assessment.
The retinoscope, particularly when used in cycloplegic conditions, proves to be a valuable tool for epidemiological purposes, aiding in screening for the distribution and development of refractive errors in infants and young children[2-4]. Furthermore, it acts as the benchmark for creating alternative tests or procedures aimed at enhancing the measurement or identification of clinically relevant refractive errors in the pediatric population[5]. Significant refractive errors contribute to avoidable vision impairment and amblyopia among pediatric age groups[6]. Regarding targeting commun
The optics of retinoscopy can be explained using Foucault's principle[9]. The retinoscope can also be used to measure leads and lags of accommodation at near using the Monocular Estimated Method of retinoscopy[10]. While it may not be employed frequently, the retinoscope has practical applications in clinical settings for measuring the amplitude of accommodation[11]. There are various tools for subjective refinement of astigmatic correction, including astigmatic fan dial, Jackson cross-cylinder[12], etc. Stenopaic slit refraction enables the refinement of moderate astigmatism in lower resource settings[13]. This paper sought to summarize the historical background and importance of this technique while highlighting the evolution of this procedure and the current advancements being made.
A search was conducted on the PubMed and with the reference citation analysis (https://www.referencecitationana
The search string returned a total of 286 records. Articles not in English language were excluded. Three records were excluded as they were erratum to other publications, and one was excluded as it was not in English. A total of 108 records were classified as out of scope and were therefore not included. The authors then searched the references and citations of the remaining 178 studies, further harvesting an additional eight studies reviewed in this paper.
Refractive errors like hyperopia and myopia are lower-order aberrations generated via properties of the ocular refractive media in relation to globe anatomy[15]. The magnitude of either positive spherical defocus (with myopia)[16] or negative spherical defocus (with hyperopia) accounts for their visual significance[17]. "Astigmatism" is a second-order aberration contributed by differences between the eye's principal meridians[18]. Lower-order aberrations are corrected optically with spherical or spherocylindrical lenses. Clinical refraction is essential for deriving optimal corrections. Retinoscopy and the use of the auto-refractometer are good objective techniques for estimating magnitudes of spherocylindrical corrections. However, retinoscopy permits more procedural variability[19,20]. Novel self-contained darkroom refractive screeners have been shown to measure spherical equivalents similar to values determined from routine cycloplegic retinoscopy[21]; both tests reportedly varied only in magnitudes of spherical and cylindrical components[21]. The spherical-equivalent value represents an algebraic sum of the spherical component and the half of the cylinder in an optical prescription[22].
During retinoscopy and other reliable refraction procedures, the principal meridians are orthogonal in cases of regular astigmatism. The power meridian is steepest, while the axis meridian is flattest. When performing minus-cylinder refraction, neutralizing the power meridian via retinoscopy requires a less myopic/more hyperopic spherical component. An adequate cylindrical component then neutralizes the axis meridian[23]. On the other hand, the magnitude of a cylindrical component can be derived from the algebraic difference of both parts on an optical cross. Against-the-rule astigmatism exists with a minus cylinder axis along 90 degrees. Astigmatism is with-the-rule (WTR) when the minus cylinder axis favors 180 degrees. WTR astigmatism is more tolerable[12] and common among younger demographic groups[24-27].
After retinoscopy, good subjective refraction is needed to account for objective over- or under-correction[28]. Amblyopia is a huge consequence of uncorrected or inadequately corrected refractive error[6]. Accurate determination of the magnitude and orientation of both manifest and cycloplegic astigmatism is essential to assuring good visual outcomes following keratorefractive surgery. When utilizing vector analysis in preparation for keratorefractive and refractive lens implant-based procedures, the preoperative best-correction is factored in determining optimal treatment parameters such as target-induced astigmatism and surgical-induced astigmatism (when retreatment protocols become necessary).
On-the-axis retinoscopy as a refractive technique is important in the examination, as well as the treatment of refractive errors and amblyopia[29]. Higher-degree refractive errors are more amblyogenic[30]. The maximum correction of significant refractive errors is essential in amblyopia prevention measures[31]; data acquired from amblyopia screening among preschoolers suggested that hyperopia > 2 D, astigmatism > 1 D, and anisometropia > 0.5 D were unilateral amblyogenic refractive factors[32]. On the other hand, bilateral amblyopia was most associated with bilateral hyperopia ≥ 3 D[32].
For very young child with significant refractive errors, refraction techniques can be optimized to aid favorable emmetropization[33,34]. In the setting of long-term optometric care, consistently greater-than-expected longitudinal increase in myopic spherical equivalents can aid in early diagnosis of progressive myopia, such that timely myopia control therapies can be instituted[35,36]. Among pediatric populations, myopia is more prevalent post-emmetropization[36], and can be worsened by dim light and near work[37]. Accordingly, hyperopia prevalence is inversely associated with pediatric age[38]. Preterm children may be an exception to this trend[39].
Modern autorefractors yield higher minus-powered spheres and lower plus-powered spheres/spherical equivalents[40]. To avoid over- or under-correction, good fogging techniques are a key step in carrying out subjective refraction. Binocular balancing techniques, although not the subjective refraction endpoint, can help stabilize the relative binocular accommodative stimulus. The Humphriss immediate contrast and prism-dissociated red-green balance methods enable better consistency of results[41].
Conducting refractive screenings for newborns allows for the early detection of refractive conditions' distribution, which could serve as risk factors for amblyopia[42] and other congenital ocular conditions like retinopathy of prematurity[43-45] and retinoblastoma[46]. For young children managed for retinopathy of prematurity, accurate cycloplegic retinoscopy post-treatment enables early detection and good long-term comparison of unwanted refractive consequences[47]. Pathologic changes in adults may also present with a shift in refractive values which may be picked up by retinos
Early retinoscopy systems were cumbersome, and they consisted of a wall-mounted illumination source: Initially a lamp or lit candle. The handheld unit consisted of a reflecting mirror which was then held perpendicular to the wall-mounted unit and the visual axis of the patient[23].
The irregular reflex seen in the eye when illuminated was first reported in 1859[49]. Cuignet had earlier characterized the changes in this reflex as the illuminating source changed in direction and location[49] but it was not until 1878 that Parent published the objective refraction technique[49]. Since then, retinoscopy has been the most reliable tool for determining objective refraction values. Schaeffel et al[50] developed the infrared retinoscope in 1987[50]. These earlier units enabled spot retinoscopy only. Over time, self-illuminated retinoscopes were developed, with the evolution of Copeland’s streak retinoscope being a major landmark in the adoption of retinoscopy for broader modern-practice applications[23]. While the early models featured a simple mirror system, modern retinoscopes often employ complex optical designs, such as the streak retinoscope. Over time, retinoscopes have become more refined and user-friendly. These newer instruments offer improved accuracy and ease of use.
The recently introduced "Mirza" tele-lens retinoscopy emerges as a more precise and accurate refractive assessment method for evaluating refractive errors in young, uncooperative children and infants compared to the standard retinoscopy, proving effective in both non-cycloplegic and cycloplegic conditions[51].
Certain portable autorefraction devices are valuable substitutes for retinoscopy when screening and diagnosing refractive errors, particularly in low-income communities with constrained financial resources and a shortage of trained eye care professionals[52]. With tendencies similar to those observed during retinoscopy, non-cycloplegic and cycloplegic autorefraction yields distinct spherical equivalent values when employed for examining children and adolescents: Post-cycloplegic myopic readings often decrease in magnitude while post-cycloplegic hyperopic values increase in magnitude[53].
Retinoscopy-based screening tools have enabled epidemiological studies incorporating larger sample sizes of school-aged children[54]. The availability of more device options also offers variability for examining special-needs children; these advancements have also enabled the acquisition of more epidemiological data regarding vision problems among children with Down syndrome[55]. A streak retinoscope connected to a smartphone-based display system enabled trainer-trainee ‘video-refractive retinoscopy’ for easy description of retinoscope reflex properties in various refractive states and several other associated optical phenomena[56]. Other developments and the subsequent changes to advancement provided to the retinoscopic technique[50-62] are listed in Table 1.
| Year | Authors | Instrument | Advancement |
| 1987 | Schaeffel et al[50] | Infrared photo retinoscope | Ability to refract off-axis and peripheral areas of the cornea |
| 1987 | Miller et al[58] | Television retinoscopy | This setup used a live television camera to gather retinoscope reflex images for the purpose of teaching |
| 2014 | Chen et al[57] | Infrared retinoscopy | Extend the detection range of illuminating eccentricity making aberrations easier to detect |
| 2014 | Chan et al[60] | Digital retinoscope | Authors developed a digital retinoscope by connecting a smartphone to a streak retinoscope for training and demonstration |
| 2019 | Arnold et al[59] | School bus accommodation relaxing skiascopy | School bus accommodation relaxing skiascopy precisely estimates refractive errors including astigmatism in children without the need for cycloplegia |
| 2022 | Langue and Ajay[61] | Wifi enabled digital retinoscope | Authors attached a Wifi enabled camera to a retinoscope, allowing reflex to be viewed on other video terminals wirelessly for training |
| 2022 | Musch et al[62] | Welch Allyn spot vision screener model VS-100 | This novel equipment detects refractive error binocularly. However, false negatives were noted |
Autorefractors began to come on the scene within the last 30 years[63]. An "auto-refracto-keratometer" denotes a unified device that combines the functionalities of an autorefractor and a keratometer, offering details on refractive error and corneal curvature[64]. Several autorefractometer devices have shown good levels of consistency[65]. Refraction outcomes from autorefractor models produced by reputable stalwart ophthalmic device companies have been com
Autorefractors can be described as closed-field or open-field. The closed-field equipment has a target generated inside the autorefractor while in the open-field versions, the patient is encouraged to look through a clear opening[66]. Specialized camera-based equipment for screening amblyogenic factors such as ametropias, ocular deviations, and opacities like the medical technology and innovations photo screener and Fortune video refractor emerged at the turn of the century[67]. Screening devices such as the Retinomax autorefractor and SureSight Vision Screener showed good sensitivity for detecting significant refractive errors compared to non-cycloplegic retinoscopy[68].
The Plusoptix autorefractor emerged in 2004 and has been researched to show good agreement with cycloplegic retinoscopy[69,70]. Yet, additional research conducted by Saini et al reveals that in comparison to cycloplegic retinoscopy, the utilization of Plusoptix proves to be a more dependable method for determining the axis of the cylindrical component of refractive error in children[71]. The PlusoptiX photo screener has shown greater suitability for the detection of myopia[72]. However, both Pedia Vision and Plusoptix photo-screeners were found to overestimate the magnitude of myopia and astigmatism while also yielding underestimates of hyperopia[73].
The retinoscope is the most reliable tool for obtaining refractive values in children and individuals who cannot communicate optimally[74-83], and even newborns[84-90]. Retinoscopy is reported to be the most sensitive (78.6%) with a negative predictive value of 96.6%[91].
For assessing the spherical equivalent of subjective refraction in children, cycloplegic retinoscopy proves to be a superior method compared to autorefraction[92]. However, Akil et al[93] concluded that there is a strong correlation between cycloplegic retinoscopy and autorefraction values[93]. In situations where it is deemed necessary, non-cycloplegic retinoscopy proves beneficial for evaluating subjective refraction, particularly within school eye health programs[94-97]. In the pediatric ophthalmic examination, retinoscopy after cycloplegia is also more suitable for attaining optimal correction of hyperopia compared to other methods of objective refraction[98]. Among adults, retinoscopy also reduces the probability of hyperopic spherical equivalent under-correction compared to objective results from autorefractors[99]. Dynamic retinoscopy has also been used to determine near addition power in presbyopes[100].
Patients are required to fulfill less strict postural demands during retinoscopy compared to using common table-top autorefractors. Hence, retinoscopy is adaptable to the examination of those afflicted with significant musculoskeletal disorders, as well as children and adolescents presenting with signs of attention-deficit hyperactivity disorder and autism spectrum disorder (ASD), all of whom may have acquired abnormal head posture[101,102]. Special-needs children and young adolescents may also be hyper-reactive to closed-field autorefraction[102]. Young patients with less manifest ASD may also have suboptimal vergence/pseudo-vergence facility findings that may be missed when closed-field autorefraction is relied upon[103]. Evidence suggests that retinoscopes are useful tools for complementing several aspects of clinical research, or knowledge generation in the fields of vision science and translation to optometric practice[104,105].
In animal experiments aimed at studying refractive errors, retinoscopy is an accurate and rapid method of achieving this[106-119]. For this purpose, retinoscopy has been used to study spherical equivalent changes in guinea pigs to understand cellular mechanisms of axial length elongation, choroidal dynamics, and several specific exogenous associations[120-122]. In murine models, continuous retinoscopy under ametropic conditions has also been theorized with the construction of a skull-secured trial frame[123]. Retinoscopic values are also useful in intraocular lens calculations during equine cataract surgery[124].
The outbreak of coronavirus disease 2019 (COVID-19) and its resultant pandemic changed the practice policy of many clinics worldwide. Valuable in-person training hours were lost during the COVID-19 pandemic[125-127]. Thakur et al[128] also published a case series showing changes in the retinoscopy-based objective refraction endpoint after recovering from COVID-19[128]. Because the retinoscopic procedure requires that the clinician sit directly in front of patients and make multiple contacts with lenses and equipment used by patients, several authors recommended discontinuing the procedure in favor of automated objective refractometry[129]. Photophobic patients may also become uncomfortable from the bright light of the retinoscope. Coulter et al[102], however, described using the Luneau Retinoscopy Rack and a video target at 10 feet to capture the attention of kids[102].
Gaining proficiency in performing retinoscopy portends slow learning curves, requiring a high volume of procedural repetitions[130]. Good clinical guidance and supervision of novice technicians by more experienced personnel serve to overcome challenges associated with the quality of patient care[131]. Also, the cooperation level of patients and the experience of the clinician can influence variations in retinoscopy findings[132]. Failure to attain optimal retinoscopic correction predisposes hyperopic school-aged children to accommodative and vergence anomalies[133].
Examiners’ proficiency and experience are important factors influencing the accuracy of retinoscopy[134]. Bharadwaj et al[134] described a psychometric technique for predicting individual retinoscopists’ accuracy of results[134]. Very high refractive errors can result in an atypically blurred ‘starting-point’ reflex, thus confusing the inexperienced examiner[23].
The choice of topical agents used for cycloplegic retinoscopy in young children and early adolescents can also result in variability, particularly for young hyperopic children[135]. Mydriatic agents such as tropicamide are listed in several works of literature as cycloplegics for pediatric ocular assessment; however, they exert weaker cycloplegic effects for young children (< 5 years) presenting with accommodative esotropia and high hyperopia[135]. To avert severe adverse events, it remains prudent to select concentrations of topical cycloplegic drops following due consideration of age, body weight, and pre-existing hypersensitivities for individual pediatric patients[136]. Marked pupil miosis associated with senescence, can make the retinoscopy reflex appear obscured, hence limiting accuracy[137,138].
It is, however, noted that retinoscopy is not the endpoint of the refractive process for the majority of patients and there are subjective steps to fine-tune the refractive prescription[139-141].
Generally, refraction is the mainstay for detecting the presence and magnitude of ametropias[142,143]. Refractive errors include hyperopia, myopia, and astigmatism. Retinoscopy is also especially useful in determining the presence and magnitude of astigmatism. Astigmatism may also be regular or irregular[144]. Pre- and cycloplegic retinoscopy findings are crucial in the differential diagnosis of near reflex spasm[145]. Objective refraction with cycloplegics is the standard of care among pediatric patients with significant visual anomalies[146]. Comparing non-cycloplegic and cycloplegic retinoscopy findings can help detect and diagnose accommodative dysfunctions[147]. Cycloplegia is attained by instilling drugs such as cyclopentolate, homatropine, and atropine to eliminate accommodation in the eye before refraction. Cycloplegia usually sets in about 30-40 min after the eyedrop has been instilled[148].
Cycloplegic/wet retinoscopy allows objective assessment of the eye's absolute refractive state[149]. Cyclopentolate, with its faster effect and shorter duration of recovery, is a better option for high-volume outpatient practices[150]. Research conducted by Groth et al[151] has suggested (albeit in a canine model) that cycloplegia may not produce statistically different results in retinoscopy[151]. Vasudevan et al[152] researched into differences in spherical endpoint between static retinoscopy in the dark as compared to cycloplegic retinoscopy. Their results show that there was no statistical difference between the two methods[152].
Mohindra near retinoscopy proves to be a beneficial technique for consistently screening the refractive status of children under 12 years old, providing reliable results comparable to those achieved with cycloplegic refraction[153].
Retinoscopy via the monocular estimation method is a subjective measure of the accommodative response (lead: With over-responsiveness, or lag: With under-responsiveness)[154]. The presence of a lead on accommodation seems to be a factor in myopic progression[155] and the development of amblyopia[156]. Another retinoscopic method applied in clinical settings is dynamic Nott retinoscopy, which assesses the precision of accommodation and proves beneficial for examining accommodative and binocular vision disorders at a point in time[157] or longitudinally[158]. The reduced accommodative facility at near and higher lag of accommodation was believed to predict myopia progression in adults[159]. In Nott’s method, the patient wears his distance prescription and is asked to fixate on a target mounted on a calibrated ruler. The examiner observes the retinoscopic light reflex in the eye and adjusts his position forward and close to the patient or away from the eye until the refractive error is neutralized[160]. Notts retinoscopy is especially useful in screening for refractive errors in children with Down’s syndrome[161]. Off-axis retinoscopy has gained some credence as a potential hypothetical measure of peripheral refraction[162].
The presence of a scissor-like reflex on the cornea during retinoscopy is one of the classical signs of keratoconus[163-165], a condition seen frequently among patients with long-standing vernal keratoconjunctivitis[166]. Yet, authors have suggested that this simple tool is not regularly used in the diagnosis of keratoconus[167]. In advanced keratoconus cases, a paracentral corneal oil-droplet sign and marked scissor reflex are confirmatory correlations with other non-retinoscopic clinical signs which include: Fleischer’s ring, Munson and Rizzuti signs, Vogt’s striae, and subepithelial apical scarring[168]. On the other hand, for earlier diagnosis of subclinical or ‘Forme Fruste’ keratoconus, patient groups with scissor retinoscopy reflexes, normal intraocular findings, and moderate-to-high astigmatism with corrected distance visual acuity < 6/9 require further assessment of central/apical corneal thickness, as well as biometry of the anterior and posterior corneal curvatures[168]. When available, Placido disc topography (for the air-tear-epithelial interface), scanning slit topography, and Scheimpflug imaging (capable of assessing posterior corneal elevation) are adjunctive to retinoscopy screening cues for true confirmation of preclinical/subclinical keratoconus[169]. This scissor-like retinoscopic reflex may serve as a useful lower-resource marker of irregular astigmatism[170].
In patients with unintended thicker flaps post-laser-assisted keratomileusis, a scissor motion seen on retinoscopy may be the first postoperative indication of wrong preoperative corneal biometry values[171]. In patients suspected of having a spasm of near reflex, a finding of > 2 diopters difference between standard and cycloplegic retinoscopy confirms the condition[172].
Although cycloplegic retinoscopy is still considered the primary method for diagnosing refractive errors, challenges such as difficulty in obtaining cooperation from pediatric patients and the clinician's level of expertise have led to the emergence of modern technological alternatives, such as auto-refractometers[173]. Regarding autorefractors, while they are faster and demand less cooperation when used without cycloplegia, they produce more myopic outcomes that lack repeatability, especially within the pediatric population[174,175]. Likewise, photo-refractors, by accurately assessing refractive errors and amblyopic risk factors while overestimating myopia in children and hyperopia in adults, serve as a valuable and reliable alternative technology, particularly in communities with limited or no access to eye care services[176]. SureSight photo-refractors/Vision Screeners are advantageous for detecting hyperopia[177]. Photo-refractor technicians should, however, take individual and ethnic differences when calibrating for a refractive error measurement[178].
There is a possibility that automated devices, like the Plusoptix Power Refractor II, utilizing the eccentric photorefraction principle for detecting significant hyperopia in children, may lack the required level of accuracy in vision screening programs[179]. While the Plusoptix A09 photo screener serves as a beneficial tool for screening refractive errors in 5-to-15-year-old children, its effectiveness, particularly for myopic and astigmatic conditions, could be enhanced by combining it with retinoscopy[180]. Similar to other photorefraction technologies such as the Retinomax, Plusoptix, iScreen Vision Screener, and Adaptica 2WIN, the Spot Vision Screener captures and assesses images of the red reflex in the eyes to detect ametropia (primarily leaning towards myopia) in children starting from 6 mo old[181,182].
Compared to cycloplegic retinoscopy, the 2WIN-S photo-refractometer stands out as a highly dependable, swift, and portable device for evaluating refractive status in pediatric screening[183]. However, total reliance on the refraction measurements of screening tools can be unideal for making precise spectacle prescriptions[184]. The instaref R20, a portable/handheld auto refractometer manufactured based on the principles of Hartmann-Shack wavefront aberrometry, a wavefront sensor-based technology with high clinical usability over the years, showed good reliability and agreement with standard retinoscopy for use in pediatric evaluation[185]. A United States-based company created the Near Eye Tool for Refractive Assessment, a portable device attachable to smartphones, rapidly estimating refractive errors by displaying red-green line patterns through a pinhole optic aligned by the user[186,187]. Open-field autorefractors, such as the Shin-Nippon NVision-K 5001, provide a more dependable and precise assessment of refractive errors, specifically in children with hyperopia and oblique astigmatism, when compared to closed-field autorefractors like the Topcon KR-800[187].
The emerging Binocular Wavefront Optometer employs wavefront aberration principles and adaptive optics technology to efficiently and accurately assess children's refractive status, surpassing traditional autorefraction and retinoscopy under cycloplegic conditions with a superior 0.05 D-interval resolution compared to the standard 0.25 D-interval in optometry[188]. When compared to retinoscopy and autorefraction, the SVOne, a portable Hartmann-Shack wavefront aberrometer utilizing wavefront sensors and capable of connecting to a smartphone, objectively assesses the eye's refractive error[189].
QuickSee is an affordable and portable autorefractor utilizing wavefront aberrometry, capable of providing a satisfactory assessment of the eye's refractive status[190].
Utilizing wavefront aberrometry technology, the E-see autorefractor delivers a refractive error estimation that is more precise and consistent with retinoscopy compared to alternative autorefraction methods[191]. The SureSight Vision Screener, utilizing wavefront analytic technology, shows promise in evaluating the refractive status of children under three years old comparable to cycloplegic retinoscopy, albeit needing additional validation[192].
While the wavefront-based autorefraction measurements of children's refractive status in both non-cycloplegic and cycloplegic conditions show consistent astigmatic data, there exists a 0.5 D disparity in the spherical equivalent of the non-cycloplegic measurement, which can be mitigated through repeated measurements[193].
Geremias et al's study revealed the Spot Vision Screener as an advanced and effective automated photo screening tool, proving superior in accurately measuring the refractive status of children below 3 years old (a risk factor of amblyopia) under cycloplegia conditions compared to retinoscopy, particularly beneficial in low-resource settings[194]. Likewise, additional research has affirmed the high reliability of the Spot Vision Screener in evaluating amblyopic risk factors among children with neurodevelopmental disabilities[195].
The Plusoptix S12-C photo screener proves to be a valuable and efficient tool for screening amblyogenic risk factors in children as young as 6 mo old, particularly in low-income communities[196]. Similarly, the Plusoptix A12-C photo screener is effective in detecting refractive amblyopia risk factors but not strabismic risk factors in children aged 3 to 4 years[197,198].
Integrating artificial intelligence (AI) into modern objective refraction techniques can be outlined to serve the following functions: Optimizing technical/operator training, and reducing patient/subject waiting time and discomfort[199-201].
The challenges with in-person examination created by the COVID-19 pandemic necessitated objective refraction simulations[126]. Chandrakanth et al[199] proposed a smartphone-based application for documenting retinoscopy called the Gimbalscope[199]. This device combines a smartphone with a traditional retinoscope and can be used as a teaching tool for clinicians wanting to understand the reflex patterns seen during the procedure.
Researchers have experimented with integrating AI modalities with portable vision screeners. Handheld infrared eccentric automated refractors have also been implemented with advanced AI/deep learning algorithms which help minimize environmental and motion artifacts influencing their utility[200]. Similarly, pediatric vision screeners that measure perifoveal retinal birefringence have been optimized with artificial neural networks which detect central fixation and thus, obtain more accurate refraction measures in the setting of amblyopia and strabismus[201]. The development of predictive analytics for ocular refraction is an evolving research area in medical AI. The clinical significance of the Fusion Model-Based Deep Learning System (FMDLS), utilizing Retina Fundus Photographs, has been established in detecting spherical, cylindrical, and axis components of refractive errors, mirroring the effectiveness of cycloplegic refraction[202] while reducing human error. This particular retinal fundus photograph of the FMDLS correlated common features of the optic nerve head, fovea, and subretinal vascular reflectivity among myopes as predictors of the refractive error. As an improvement upon previous AI systems which yield output in spherical equivalent values, the FMDLS algorithm further highlighted optic disc orientation and macular area morphology as regions of interest in differentiating “WTR” from oblique forms of astigmatism; interracial variation was unaccounted for[202]. Training future advanced AI models of ocular refraction with datasets obtainable from wavefront sensor devices may help equate, or even surpass standard refractive measures acquirable with non-machine learning approaches.
In conclusion, the retinoscope has evolved significantly since its inception, adapting to changing technology and improving diagnostic capabilities. While it has advantages such as non-invasiveness and broad applicability, limitations exist and the need for skilled interpretation remains. Amblyopia is a main consequence of inappropriate refractive error correction during early childhood. Retinoscopy still represents a useful tool for ameliorating inadequate pediatric refractive error screening coverage in remote and underserved areas.
This study search was limited to retinoscopy. While this is a very common procedure, there is a paucity of related published data and a good number of studies returned by the search only mentioned it in passing while discussing entirely different topics. Widening the search criteria to include refraction could potentially have yielded more studies to review.
| 1. | Musa MJ, Zeppieri M. Principles and Technique of Fogging During Subjective Refraction. 2023 Jul 19. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. [PubMed] |
| 2. | Bothun ED, Cleveland J, Lynn MJ, Christiansen SP, Vanderveen DK, Neely DE, Kruger SJ, Lambert SR; Infant Aphakic Treatment Study. One-year strabismus outcomes in the Infant Aphakia Treatment Study. Ophthalmology. 2013;120:1227-1231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 39] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 3. | Yahya AN, Sharanjeet-Kaur S, Akhir SM. Distribution of Refractive Errors among Healthy Infants and Young Children between the Age of 6 to 36 Months in Kuala Lumpur, Malaysia-A Pilot Study. Int J Environ Res Public Health. 2019;16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 4. | Carter MJ, Lansingh VC, Schacht G, Río del Amo M, Scalamogna M, France TD. Visual acuity and refraction by age for children of three different ethnic groups in Paraguay. Arq Bras Oftalmol. 2013;76:94-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Esteves Leandro J, Meira J, Ferreira CS, Santos-Silva R, Freitas-Costa P, Magalhães A, Breda J, Falcão-Reis F. Adequacy of the Fogging Test in the Detection of Clinically Significant Hyperopia in School-Aged Children. J Ophthalmol. 2019;2019:3267151. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Jafarzadehpur E, Kermani RM, Mohhamadi AR, Nateghi MR, Fazeli AS, Kashi KM. Ocular Manifestations in Infants Resulted from Assisted Reproductive Technology (ART). J Family Reprod Health. 2013;7:181-186. [PubMed] |
| 7. | Lan W, Zhao F, Lin L, Li Z, Zeng J, Yang Z, Morgan IG. Refractive errors in 3-6 year-old Chinese children: a very low prevalence of myopia? PLoS One. 2013;8:e78003. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 64] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 8. | Ying GS, Maguire MG, Cyert LA, Ciner E, Quinn GE, Kulp MT, Orel-Bixler D, Moore B; Vision In Preschoolers (VIP) Study Group. Prevalence of vision disorders by racial and ethnic group among children participating in head start. Ophthalmology. 2014;121:630-636. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 80] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 9. | Hallak J. Reflections on retinoscopy. Am J Optom Physiol Opt. 1976;53:224-228. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 10. | Momeni-Moghaddam H, Goss DA, Sobhani M. Accommodative response under monocular and binocular conditions as a function of phoria in symptomatic and asymptomatic subjects. Clin Exp Optom. 2014;97:36-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 11. | Burns DH, Allen PM, Edgar DF, Evans BJW. Sources of error in clinical measurement of the amplitude of accommodation. J Optom. 2020;13:3-14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 12. | Asiedu K, Kyei S, Ampiah EE. Autorefraction, Retinoscopy, Javal's Rule, and Grosvenor's Modified Javal's Rule: The Best Predictor of Refractive Astigmatism. J Ophthalmol. 2016;2016:3584137. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 13. | Dhiman S, Stokkermans TJ. Subjective Refraction Technique: Stenopeic Slit. 2023 Jul 15. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. [PubMed] |
| 14. | Musa M, Zeppieri M, Enaholo ES, Chukwuyem E, Salati C. An Overview of Corneal Transplantation in the Past Decade. Clin Pract. 2023;13:264-279. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 15. | Ramírez-Ortiz MA, Amato-Almanza M, Romero-Bautista I, Klunder-Klunder M, Aguirre-Luna O, Kuzhda I, Resnikoff S, Eckert KA, Lansingh VC. A large-scale analysis of refractive errors in students attending public primary schools in Mexico. Sci Rep. 2023;13:13509. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 16. | Smith EL 3rd, Hung LF, Huang J, Arumugam B. Effects of local myopic defocus on refractive development in monkeys. Optom Vis Sci. 2013;90:1176-1186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 91] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 17. | Arumugam B, Hung LF, To CH, Holden B, Smith EL 3rd. The effects of simultaneous dual focus lenses on refractive development in infant monkeys. Invest Ophthalmol Vis Sci. 2014;55:7423-7432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 45] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 18. | Al Wadaani FA, Amin TT, Ali A, Khan AR. Prevalence and pattern of refractive errors among primary school children in Al Hassa , Saudi Arabia. Glob J Health Sci. 2012;5:125-134. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 50] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 19. | Aboumourad R, Anderson HA. Comparison of Dynamic Retinoscopy and Autorefraction for Measurement of Accommodative Amplitude. Optom Vis Sci. 2019;96:670-677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 20. | Phu J, Wang H, Miao S, Zhou L, Khuu SK, Kalloniatis M. Neutralizing Peripheral Refraction Eliminates Refractive Scotomata in Tilted Disc Syndrome. Optom Vis Sci. 2018;95:959-970. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 21. | Wei X, Li L, Jiang L, Lu H, Huang H, Zhong D, Pan L, Wei D, Han Y, Lin H, Chen Q. Comparison of the new self-contained darkroom refractive screener versus table-top autorefractor and cycloplegia retinoscopy in detecting refractive error. BMC Ophthalmol. 2023;23:487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 22. | Enaholo ES, Musa MJ, Zeppieri M. The Spherical Equivalent. 2023 May 11. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. [PubMed] |
| 23. | Enaholo ES, Musa MJ, Zeppieri M. Objective Refraction Technique: Retinoscopy. 2023 Oct 28. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. [PubMed] |
| 24. | Hashemi H, Asharlous A, Khabazkhoob M, Yekta A, Emamian MH, Fotouhi A. The profile of astigmatism in 6-12-year-old children in Iran. J Optom. 2021;14:58-68. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 25. | Hashemi H, Rezvan F, Beiranvand A, Papi OA, Hoseini Yazdi H, Ostadimoghaddam H, Yekta AA, Norouzirad R, Khabazkhoob M. Prevalence of Refractive Errors among High School Students in Western Iran. J Ophthalmic Vis Res. 2014;9:232-239. [PubMed] |
| 26. | Huang J, Maguire MG, Ciner E, Kulp MT, Cyert LA, Quinn GE, Orel-Bixler D, Moore B, Ying GS; Vision in Preschoolers (VIP) Study Group. Risk factors for astigmatism in the Vision in Preschoolers Study. Optom Vis Sci. 2014;91:514-521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 36] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 27. | Ziaei H, Katibeh M, Solaimanizad R, Hosseini S, Gilasi HR, Golbafian F, Javadi MA. Prevalence of refractive errors; the yazd eye study. J Ophthalmic Vis Res. 2013;8:227-236. [PubMed] |
| 28. | Chaurasiya RK. Refractive changes during off-the-axis retinoscopy in myopia. Indian J Ophthalmol. 2022;70:779-781. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 29. | Vodencarevic AN, Jusufovic V, Halilbasic M, Alimanovic E, Terzic S, Cabric E, Drljevic A, Burgic M. Amblyopia in Children: Analysis Among Preschool and School Children in the City of Tuzla, Bosnia and Herzegovina. Mater Sociomed. 2017;29:164-167. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 30. | Vonor K, Ayena KD, Dzidzinyo K, Amedome KM, Santos M, Maneh N, Kuaovi Koko RA, Banla M, Balo KP. [Severe ametropia in children in Lomé (Togo)]. Med Sante Trop. 2014;24:219-220. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 31. | Wang J, Feng L, Wang Y, Zhou J, Hess RF. Binocular benefits of optical treatment in anisometropic amblyopia. J Vis. 2018;18:6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 32. | Pascual M, Huang J, Maguire MG, Kulp MT, Quinn GE, Ciner E, Cyert LA, Orel-Bixler D, Moore B, Ying GS; Vision In Preschoolers (VIP) Study Group. Risk factors for amblyopia in the vision in preschoolers study. Ophthalmology. 2014;121:622-9.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 114] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 33. | Mutti DO, Sinnott LT, Lynn Mitchell G, Jordan LA, Friedman NE, Frane SL, Lin WK. Ocular Component Development during Infancy and Early Childhood. Optom Vis Sci. 2018;95:976-985. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 85] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 34. | Somer D, Karabulut E, Cinar FG, Altiparmak UE, Unlu N. Emmetropization, visual acuity, and strabismus outcomes among hyperopic infants followed with partial hyperopic corrections given in accordance with dynamic retinoscopy. Eye (Lond). 2014;28:1165-1173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 35. | Lum E. Progressive anisometropia and orthokeratology: a case report. Clin Exp Optom. 2018;101:599-600. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 36. | Ore L, Garozli HJ, Schwartz N, Cohen-Dar M. Factors influencing prevalence of vision and ocular abnormalities among Jewish and Arab Israeli schoolchildren. Isr Med Assoc J. 2014;16:553-558. [PubMed] |
| 37. | Chhabra S, Rathi M, Sachdeva S, Rustagi IM, Soni D, Dhania S. Association of near work and dim light with myopia among 1400 school children in a district in North India. Indian J Ophthalmol. 2022;70:3369-3372. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 38. | Castagno VD, Fassa AG, Carret ML, Vilela MA, Meucci RD. Hyperopia: a meta-analysis of prevalence and a review of associated factors among school-aged children. BMC Ophthalmol. 2014;14:163. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 66] [Cited by in RCA: 55] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 39. | Al Oum M, Donati S, Cerri L, Agosti M, Azzolini C. Ocular alignment and refraction in preterm children at 1 and 6 years old. Clin Ophthalmol. 2014;8:1263-1268. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 40. | Krishnacharya PS. Study on accommodation by autorefraction and dynamic refraction in children. J Optom. 2014;7:193-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 41. | Momeni-Moghaddam H, Goss DA. Comparison of four different binocular balancing techniques. Clin Exp Optom. 2014;97:422-425. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 42. | Al-Salem KM, Saleem MS, Ereifej I, Alrawashdeh HM, Obeidat RFH, Abdlmohdi AA, Al-Momani RZ, Hammad LM, Al-Habahbeh OA, Assassfeh YM, Al-Qsous LRN, Nasraween AHA, AlMaaitah TA, Aqeel DMH, Alabdulrazzg IEA, Murad AMM, Al-Zurqan AJF, Jaradat EJM, Aldhoon SES, Dmour AM, Asassfeh AT, Halaseh JA, Daoud AAA, Alkasasbeh WA, Matar KG. Amblyopia screening for first and second-grade children in Jordan. Int J Ophthalmol. 2022;15:352-356. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 43. | Semeraro F, Forbice E, Nascimbeni G, Cillino S, Bonfiglio VME, Filippelli ME, Bartollino S, Costagliola C. Ocular Refraction at Birth and Its Development During the First Year of Life in a Large Cohort of Babies in a Single Center in Northern Italy. Front Pediatr. 2019;7:539. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 44. | Dikopf MS, Machen LA, Hallak JA, Chau FY, Kassem IS. Zone of retinal vascularization and refractive error in premature eyes with and without spontaneously regressed retinopathy of prematurity. J AAPOS. 2019;23:211.e1-211.e6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 45. | Quinn GE, Dobson V, Davitt BV, Wallace DK, Hardy RJ, Tung B, Lai D, Good WV; Early Treatment for Retinopathy of Prematurity Cooperative Group. Progression of myopia and high myopia in the Early Treatment for Retinopathy of Prematurity study: findings at 4 to 6 years of age. J AAPOS. 2013;17:124-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 67] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 46. | Villegas VM, Wu SC, Murray TG, Cavuoto KM, Capo H, McKeown CA. Prevalence of refractive errors in children with retinoblastoma. Clin Ophthalmol. 2019;13:431-435. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 47. | Simmons M, Wang J, Leffler JN, Li S, Morale SE, de la Cruz A, Birch EE. Longitudinal Development of Refractive Error in Children Treated With Intravitreal Bevacizumab or Laser for Retinopathy of Prematurity. Transl Vis Sci Technol. 2021;10:14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 48. | Musa M, Aluyi-Osa G, Zeppieri M. Foster Kennedy Syndrome (FKS): A Case Report. Clin Pract. 2022;12:527-532. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Reference Citation Analysis (0)] |
| 49. | Miller JM. The Retinoscopy Book: An Introductory Manual for Eye Care Professionals. 5th ed. Am J Ophthalmol. 2003;136:788. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 50. | Schaeffel F, Farkas L, Howland HC. Infrared photoretinoscope. Appl Opt. 1987;26:1505-1509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 85] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 51. | Mirzajani A, Amini Vishteh R, Khalilian M. Introducing a new method of retinoscopy for refraction of infants and young children: The "Mirza" tele lens retinoscopy. J Optom. 2021;14:254-262. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 52. | Agarwal A, Bloom DE, deLuise VP, Lubet A, Murali K, Sastry SM. Comparing low-cost handheld autorefractors: A practical approach to measuring refraction in low-resource settings. PLoS One. 2019;14:e0219501. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 53. | Zhu D, Wang Y, Yang X, Yang D, Guo K, Guo Y, Jing X, Pan CW. Pre- and Postcycloplegic Refractions in Children and Adolescents. PLoS One. 2016;11:e0167628. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 38] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 54. | Joseph E, Ck M, Kumar R, Sebastian M, Suttle CM, Congdon N, Sethu S, Murthy GV; REACH Research Group. Prevalence of refractive errors among school-going children in a multistate study in India. Br J Ophthalmol. 2023;108:143-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 55. | Hashemi H, Mehravaran S, Asgari S, Dehghanian Nasrabadi F. Refractive and Vision Status in Down Syndrome: A Comparative Study. Turk J Ophthalmol. 2021;51:199-205. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 56. | Schrimpf B, Dalby M, Mülhaupt M, Michel F, Holschbach A, Schiefer U, Ungewiss J. [Interactive training using a smartphone video retinoscope : Video article]. Ophthalmologe. 2020;117:384-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 57. | Chen YL, Shi L, Lewis JWL, Wang M. Infrared Retinoscopy. Photonics. 2014;1:303-322. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 58. | Miller KM, Simons K, Guyton DL. Television retinoscopy with a slit-aperture retinoscope and a highly sensitive camera. Ophthalmology. 1987;2:22-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 59. | Arnold AW, Arnold SL, Sprano JH, Arnold RW. School bus accommodation-relaxing skiascopy. Clin Ophthalmol. 2019;13:1841-1851. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 60. | Chan WO, Crabb M, Sia D, Taranath D. Creating a digital retinoscope by combining a mobile smartphone camera and a retinoscope. J AAPOS. 2014;18:387-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 61. | Langue M, Soni A. A novel device for digital retinoscopy. J AAPOS. 2022;26:141-142. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 62. | Musch DC, Andrews CA, Schumann RA, Baker JD. A Comparative Study of Two Photoscreening Devices With Manual Vision Screening Involving Preschool Children. J Pediatr Ophthalmol Strabismus. 2022;59:46-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 63. | Gurnani B, Kaur K. Autorefractors. 2023 Jun 11. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. [PubMed] |
| 64. | Kadhim YJ, Farhood QK. Central corneal thickness of Iraqi population in relation to age, gender, refractive errors, and corneal curvature: a hospital-based cross-sectional study. Clin Ophthalmol. 2016;10:2369-2376. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 65. | Simsek M, Oral Y, Erogul O, Sabaner MC, Simsek C, Yorukoglu S. Comparison of the results of four different refraction measurement devices in children with retinoscopy. Rom J Ophthalmol. 2022;66:337-343. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 66. | Nagra M, Akhtar A, Huntjens B, Campbell P. Open versus closed view autorefraction in young adults. J Optom. 2021;14:86-91. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 67. | Cooper CD, Gole GA, Hall JE, Colville DJ, Carden SM, Bowling FG. Evaluating photoscreeners II: MTI and fortune videorefractor. Aust N Z J Ophthalmol. 1999;27:387-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 68. | Kulp MT, Ying GS, Huang J, Maguire M, Quinn G, Ciner EB, Cyert LA, Orel-Bixler DA, Moore BD. Accuracy of noncycloplegic retinoscopy, retinomax autorefractor, and SureSight vision screener for detecting significant refractive errors. Invest Ophthalmol Vis Sci. 2014;55:1378-1385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 26] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 69. | Mirzajani A, Heirani M, Jafarzadehpur E, Haghani H. A comparison of the Plusoptix S08 photorefractor to retinoscopy and cycloretinoscopy. Clin Exp Optom. 2013;96:394-399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 70. | Ozdemir O, Özen Tunay Z, Petriçli IS, Ergintürk Acar D, Erol MK. Comparison of non-cycloplegic photorefraction, cycloplegic photorefraction and cycloplegic retinoscopy in children. Int J Ophthalmol. 2015;8:128-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 71. | Saini V, Raina UK, Gupta A, Goyal JL, Anjum R, Saini P, Gupta SK, Sharma P. Comparison of Plusoptix S12R photoscreener with cycloplegic retinoscopy and autorefraction in pediatric age group. Indian J Ophthalmol. 2019;67:1555-1559. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 72. | Yan Q, Li R, Qian Y, Lin X, Zhu H, Wang Y, Zhao X, Zhang X, Sun Q, Hao Q, Tong H, Zhu Y, Li Z, Liu H, Huang D. Instrument referral criteria for PlusoptiX and SureSight based on 2021 AAPOS guidelines: A population-based study. Front Public Health. 2022;10:959757. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 73. | Peterseim MM, Papa CE, Wilson ME, Cheeseman EW, Wolf BJ, Davidson JD, Trivedi RH. Photoscreeners in the pediatric eye office: compared testability and refractions on high-risk children. Am J Ophthalmol. 2014;158:932-938. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 37] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 74. | Al Bahhawi T, Makeen AM, Daghreeri HH, Tobaigy MF, Adawi AM, Guhal FM, Akkur MA, Alotayfi MJ, Otayf MM, Bajoned MS, Mahfouz MS. Refractive Error among Male Primary School Students in Jazan, Saudi Arabia: Prevalence and Associated Factors. Open Ophthalmol J. 2018;12:264-272. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 75. | Alsaqr AM, Ibrahim G, Sharha AA, Fagehi R. Investigating the Visual Status Of Preschool Children in Riyadh, Saudi Arabia. Middle East Afr J Ophthalmol. 2017;24:190-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 76. | Bingöl Kızıltunç P, İdil A, Atilla H, Topalkara A, Alay C. Results of Screening in Schools for Visually Impaired Children. Turk J Ophthalmol. 2017;47:216-220. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 77. | Gessesse SA, Teshome AW. Prevalence of myopia among secondary school students in Welkite town: South-Western Ethiopia. BMC Ophthalmol. 2020;20:176. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 78. | Kara S, Yalniz-Akkaya Z, Yeniaras A, Örnek F, Bilge YD. Ocular findings on follow-up in children who received phototherapy for neonatal jaundice. J Chin Med Assoc. 2017;80:729-732. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 79. | Kaur K, Gurnani B. Subjective Refraction Techniques. 2023 Jun 11. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. [PubMed] |
| 80. | Majumder C, Afnan H. Amplitude of Accommodation among Students of a Malaysian Private University as Assessed Using Subjective and Objective Techniques. Korean J Ophthalmol. 2020;34:219-226. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 81. | Vinekar A, Mangalesh S, Jayadev C, Bauer N, Munusamy S, Kemmanu V, Kurian M, Mahendradas P, Avadhani K, Shetty B. Macular edema in Asian Indian premature infants with retinopathy of prematurity: Impact on visual acuity and refractive status after 1-year. Indian J Ophthalmol. 2015;63:432-437. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 28] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 82. | Wang X, Liu D, Feng R, Zhao H, Wang Q. Refractive error among urban preschool children in Xuzhou, China. Int J Clin Exp Pathol. 2014;7:8922-8928. [PubMed] |
| 83. | Wang Y, Pi LH, Zhao RL, Zhu XH, Ke N. Refractive status and optical components of premature babies with or without retinopathy of prematurity at 7 years old. Transl Pediatr. 2020;9:108-116. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 84. | Kaur G, Thomas S, Jindal M, Bhatti SM. Visual Function and Ocular Status in Children with Disabilities in Special Schools of Northern India. J Clin Diagn Res. 2016;10:NC01-NC04. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 85. | Li LH, Li N, Zhao JY, Fei P, Zhang GM, Mao JB, Rychwalski PJ. Findings of perinatal ocular examination performed on 3573, healthy full-term newborns. Br J Ophthalmol. 2013;97:588-591. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 67] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 86. | Li Y, Liu J, Qi P. The increasing prevalence of myopia in junior high school students in the Haidian District of Beijing, China: a 10-year population-based survey. BMC Ophthalmol. 2017;17:88. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 86] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 87. | Mao J, Lao J, Liu C, Wu M, Yu X, Shao Y, Zhu L, Chen Y, Shen L. Factors That Influence Refractive Changes in the First Year of Myopia Development in Premature Infants. J Ophthalmol. 2019;2019:7683749. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 88. | Ruan L, Shan HD, Liu XZ, Huang X. Refractive status of Chinese with laser-treated retinopathy of prematurity. Optom Vis Sci. 2015;92:S3-S9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 89. | Uprety S, Morjaria P, Shrestha JB, Shrestha GS, Khanal S. Refractive Status in Nepalese Pre-Term and Full-Term Infants Early in Life. Optom Vis Sci. 2017;94:957-964. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 90. | Yu SJ, Liu GH, Liu Y, Huang J, Han ML, Zhao BJ, Gai ZT. The evolution of refractive status in Chinese infants during the first year of life and its affected factors. Int J Ophthalmol. 2017;10:1290-1294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 91. | Chottopadhyay T, Kaur H, Shinde AJ, Gogate PM. Why are we not doing retinoscopy in the school eye screening? Saudi J Ophthalmol. 2021;35:320-324. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 92. | Mukash SN, Kayembe DL, Mwanza JC. Agreement Between Retinoscopy, Autorefractometry and Subjective Refraction for Determining Refractive Errors in Congolese Children. Clin Optom (Auckl). 2021;13:129-136. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 93. | Akil H, Keskin S, Çavdarli C. Comparison of the refractive measurements with hand-held autorefractometer, table-mounted autorefractometer and cycloplegic retinoscopy in children. Korean J Ophthalmol. 2015;29:178-184. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 94. | Garcia-Lievanos O, Sanchez-Gonzalez L, Espinosa-Cruz N, Hernandez-Flores LA, Salmeron-Leal L, Torres-Rodriguez HD. Myopia in schoolchildren in a rural community in the State of Mexico, Mexico. Clin Optom (Auckl). 2016;8:53-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 95. | Khurana R, Tibrewal S, Ganesh S, Tarkar R, Nguyen PTT, Siddiqui Z, Dasgupta S. Accuracy of noncycloplegic refraction performed at school screening camps. Indian J Ophthalmol. 2018;66:806-811. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 96. | Ntodie M, Saunders KJ, Little JA. Correction of Low-Moderate Hyperopia Improves Accommodative Function for Some Hyperopic Children During Sustained Near Work. Invest Ophthalmol Vis Sci. 2021;62:6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 97. | Zhou Z, Chen T, Jin L, Zheng D, Chen S, He M, Silver J, Ellwein L, Moore B, Congdon NG. Self-refraction, ready-made glasses and quality of life among rural myopic Chinese children: a non-inferiority randomized trial. Acta Ophthalmol. 2017;95:567-575. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 98. | Adhikari S, Nepal BP, Shrestha JK, Khandekar R. Magnitude and determinants of refractive error among school children of two districts of Kathmandu, Nepal. Oman J Ophthalmol. 2013;6:175-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 99. | Vilaseca M, Arjona M, Pujol J, Peris E, Martínez V. Non-cycloplegic spherical equivalent refraction in adults: comparison of the double-pass system, retinoscopy, subjective refraction and a table-mounted autorefractor. Int J Ophthalmol. 2013;6:618-625. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 100. | Yazdani N, Khorasani AA, Moghadam HM, Yekta AA, Ostadimoghaddam H, Shandiz JH. Evaluating Three Different Methods of Determining Addition in Presbyopia. J Ophthalmic Vis Res. 2016;11:277-281. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 101. | Chen L, Sun L, Xue C, Li S, Wang J, Shen X, Gao S, Zhou Z, Xu Y, Huang S, Li Z, Yang X, Guo Y, Zhang W. Refractive errors and ocular findings in children and adolescents with mental disorders: a retrospective study. BMC Ophthalmol. 2023;23:4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 102. | Coulter RA, Bade A, Tea Y, Fecho G, Amster D, Jenewein E, Rodena J, Lyons KK, Mitchell GL, Quint N, Dunbar S, Ricamato M, Trocchio J, Kabat B, Garcia C, Radik I. Eye examination testability in children with autism and in typical peers. Optom Vis Sci. 2015;92:31-43. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 103. | Coulter RA, Bade A, Jenewein EC, Tea YC, Mitchell GL. Near-point Findings in Children with Autism Spectrum Disorder and in Typical Peers. Optom Vis Sci. 2021;98:384-393. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 104. | Diress M, Getnet M, Akalu Y, Dagnew B, Belsti Y, Gela YY, Chilot D, Belay DG, Bitew DA, Terefe B, Getahun AB. Myopia and its associated factors among pregnant women at health institutions in Gondar District, Northwest Ethiopia: A multi-center cross-sectional study. Front Glob Womens Health. 2022;3:1078557. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 105. | Zhong W, Lan C, Gu Z, Tan Q, Xiang X, Zhou H, Liao X. The Mechanosensitive Piezo1 Channel Mediates Mechanochemical Transmission in Myopic Eyes. Invest Ophthalmol Vis Sci. 2023;64:1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 106. | Bueno JM, Lo Sapio M, Sanes JM, Seva J. Analysis of the Ocular Refractive State in Fighting Bulls: Astigmatism Prevalence. Biomed Res Int. 2017;2017:8203269. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 107. | de Oliveira JK, Bortolini M, Schaller M, Schuchmann RK, Moore BA, Montiani-Ferreira F. The ophthalmic health and refractive state of working dogs in South Brazil. Open Vet J. 2020;10:22-30. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 108. | Dillingham CM, Guggenheim JA, Erichsen JT. Disruption of the centrifugal visual system inhibits early eye growth in chicks. Invest Ophthalmol Vis Sci. 2013;54:3632-3643. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 109. | Jiang L, Garcia MB, Hammond D, Dahanayake D, Wildsoet CF. Strain-Dependent Differences in Sensitivity to Myopia-Inducing Stimuli in Guinea Pigs and Role of Choroid. Invest Ophthalmol Vis Sci. 2019;60:1226-1233. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 110. | Li RQ, Lan WZ, Li XN, Wu HR, Xu QL, Zhong H, Li WT, Yang ZK. Effects of the long wavelength-filtered continuous spectrum on natural refractive development in juvenile guinea pigs. Int J Ophthalmol. 2019;12:883-891. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 111. | Pucker AD, Jackson AR, McHugh KM, Mutti DO. Morphological ciliary muscle changes associated with form deprivation-induced myopia. Exp Eye Res. 2020;193:107963. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 112. | Smith EL 3rd, Hung LF, Arumugam B, Holden BA, Neitz M, Neitz J. Effects of Long-Wavelength Lighting on Refractive Development in Infant Rhesus Monkeys. Invest Ophthalmol Vis Sci. 2015;56:6490-6500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 120] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 113. | Smith EL 3rd, Hung LF, Arumugam B, Huang J. Negative lens-induced myopia in infant monkeys: effects of high ambient lighting. Invest Ophthalmol Vis Sci. 2013;54:2959-2969. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 89] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 114. | Smith Iii EL, Arumugam B, Hung LF, She Z, Beach K, Sankaridurg P. Eccentricity-dependent effects of simultaneous competing defocus on emmetropization in infant rhesus monkeys. Vision Res. 2020;177:32-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 33] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 115. | Swiatczak B, Feldkaemper M, Schraermeyer U, Schaeffel F. Demyelination and shrinkage of axons in the retinal nerve fiber layer in chickens developing deprivation myopia. Exp Eye Res. 2019;188:107783. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 116. | Tian L, Guo YT, Ying M, Liu YC, Li X, Wang Y. Co-existence of myopia and amblyopia in a guinea pig model with monocular form deprivation. Ann Transl Med. 2021;9:110. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 117. | Wahl C, Li T, Howland H. Plasticity in the growth of the chick eye: emmetropization achieved by alternate morphologies. Vision Res. 2015;110:15-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 118. | Woods J, Guthrie SE, Keir N, Dillehay S, Tyson M, Griffin R, Choh V, Fonn D, Jones L, Irving E. Inhibition of defocus-induced myopia in chickens. Invest Ophthalmol Vis Sci. 2013;54:2662-2668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 119. | Zi Y, Deng Y, Zhao J, Ji M, Qin Y, Deng T, Jin M. Morphologic and biochemical changes in the retina and sclera induced by form deprivation high myopia in guinea pigs. BMC Ophthalmol. 2020;20:105. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 120. | El-Nimri NW, Jiang L, Dahanayake D, Sweidan S, Smith BE, Wildsoet CF. Effect of topical latanoprost on choroidal thickness and vessel area in Guinea pigs. Exp Eye Res. 2022;225:109286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 121. | Yang Y, Wu J, Wu D, Wei Q, Zhong T, Yang J, Yang X, Zeng M, Zhong X. Intravitreal brimonidine inhibits form-deprivation myopia in guinea pigs. Eye Vis (Lond). 2021;8:27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 122. | Luo X, Li B, Li T, Di Y, Zheng C, Ji S, Ma Y, Zhu J, Chen X, Zhou X. Myopia induced by flickering light in guinea pig eyes is associated with increased rather than decreased dopamine release. Mol Vis. 2017;23:666-679. [PubMed] |
| 123. | Gu Y, Xu B, Feng C, Ni Y, Wu Q, Du C, Hong N, Li P, Ding Z, Jiang B. A Head-Mounted Spectacle Frame for the Study of Mouse Lens-Induced Myopia. J Ophthalmol. 2016;2016:8497278. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 124. | Meister U, Görig C, Murphy CJ, Haan H, Ohnesorge B, Boevé MH. Intraocular lens power calculation for the equine eye. BMC Vet Res. 2018;14:123. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 125. | Salvetat ML, Musa M, Pellegrini F, Salati C, Spadea L, Zeppieri M. Considerations of COVID-19 in Ophthalmology. Microorganisms. 2023;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 1] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 126. | Musa M, Okoye GS, Akpalaba RUE, Atuanya GN. Managing in early COVID-19: The Nigerian optometry experience. Scand J Optom Vis Sci. 2021;14:1-7. [DOI] [Full Text] |
| 127. | Musa MJ, Akpalaba RU, Atuanya GN, Akpalaba IO. Challenges and Successes of Virtual Learning: An Emerging Trend. Benin J Educ Stud. 2021;26:192-199. [DOI] [Full Text] |
| 128. | Thakur M, Panicker T, Satgunam P. Refractive error changes and associated asthenopia observed after COVID-19 infection: Case reports from two continents. Indian J Ophthalmol. 2023;71:2592-2594. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 129. | Kaur K, Muralikrishnan J, Hussaindeen JR, Deori N, Gurnani B. Impact of Covid-19 on Pediatric Ophthalmology Care: Lessons Learned. Pediatric Health Med Ther. 2023;14:309-321. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 130. | Estay AM, Plaza-Rosales I, Torres HR, Cerfogli FI. Training in retinoscopy: learning curves using a standardized method. BMC Med Educ. 2023;23:874. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 131. | Paudel P, Cronjé S, O'Connor PM, Rao GN, Holden BA. Selection considerations when using a 'standard optometrist' to evaluate clinical performance of other eye-care personnel. Clin Exp Optom. 2014;97:426-432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 132. | Yazdani N, Sadeghi R, Momeni-Moghaddam H, Zarifmahmoudi L, Ehsaei A. Comparison of cyclopentolate versus tropicamide cycloplegia: A systematic review and meta-analysis. J Optom. 2018;11:135-143. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 72] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 133. | Ntodie M, Saunders K, Little JA. Accuracy and stability of accommodation and vergence responses during sustained near tasks in uncorrected hyperopes. Sci Rep. 2023;13:14389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 134. | Bharadwaj SR, Malavita M, Jayaraj J. A psychophysical technique for estimating the accuracy and precision of retinoscopy. Clin Exp Optom. 2014;97:164-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 135. | Yoo SG, Cho MJ, Kim US, Baek SH. Cycloplegic Refraction in Hyperopic Children: Effectiveness of a 0.5% Tropicamide and 0.5% Phenylephrine Addition to 1% Cyclopentolate Regimen. Korean J Ophthalmol. 2017;31:249-256. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 136. | Sefi-Yurdakul N, Sancakli Ö. Tropicamide and anaphylaxis: A case report. Saudi J Ophthalmol. 2021;35:71-72. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 137. | Kasthurirangan S, Glasser A. Age related changes in the characteristics of the near pupil response. Vision Res. 2006;46:1393-1403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 54] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 138. | Radhakrishnan H, Charman WN. Age-related changes in static accommodation and accommodative miosis. Ophthalmic Physiol Opt. 2007;27:342-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 36] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 139. | Aluyi-Osa G, Musa MJ, Zeppieri M. Jackson Cross Cylinder. 2023 May 22. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. [PubMed] |
| 140. | Chukwuyem EC, Musa MJ, Zeppieri M. Subjective Refraction Technique: Duochrome Test. 2023 May 11. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. [PubMed] |
| 141. | Musa MJ, Zeppieri M. Subjective Refraction Technique: Astigmatic Dial. 2023 May 11. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. [PubMed] |
| 142. | Musa MJ, Zeppieri M. Spectacle Correction of Ametropias. 2023 May 11. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. [PubMed] |
| 143. | Verkicharla PK, Kammari P, Das AV. Myopia progression varies with age and severity of myopia. PLoS One. 2020;15:e0241759. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 81] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 144. | Gurnani B, Kaur K. Astigmatism. 2023 Jun 26. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. [PubMed] |
| 145. | Mejía G, Guevara S, Salgado Y, Tello A. SEVERE NEAR REFLEX SPASM IN A HEALTHY TEENAGER. A CASE REPORT. Cesk Slov Oftalmol. 2023;79:97-100. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 146. | Kaur K, Gurnani B. Cycloplegic and Noncycloplegic Refraction. 2023 Jun 11. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. [PubMed] |
| 147. | Enaholo ES, Musa MJ, Zeppieri M. Accommodative Insufficiency. 2023 May 31. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. [PubMed] |
| 148. | Ying GS, Huang J, Maguire MG, Quinn G, Kulp MT, Ciner E, Cyert L, Orel-Bixler D; Vision in Preschoolers Study Group. Associations of anisometropia with unilateral amblyopia, interocular acuity difference, and stereoacuity in preschoolers. Ophthalmology. 2013;120:495-503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 27] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 149. | Morgan IG, Iribarren R, Fotouhi A, Grzybowski A. Cycloplegic refraction is the gold standard for epidemiological studies. Acta Ophthalmol. 2015;93:581-585. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 135] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 150. | Singh RP, Amitava AK, Sharma N, Gupta Y, Raza SA, Bose A, Meena GS. Comparison of cycloplegia with atropine 1% versus cyclopentolate 1. Indian J Ophthalmol. 2023;71:3633-3636. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 151. | Groth AD, Hollingsworth SR, Ofri R, Kass PH, Reed Z, Murphy CJ. Clinical comparison of the Welch Allyn SureSight™ handheld autorefractor vs. streak retinoscopy in dogs. Vet Ophthalmol. 2013;16:319-323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 152. | Vasudevan B, Ciuffreda KJ, Meehan K, Grk D, Cox M. Comparison of objective refraction in darkness to cycloplegic refraction: a pilot study. Clin Exp Optom. 2016;99:168-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 153. | Kauser F, Gupta Y, Amitava AK, Saxena J, Raza SA, Masood A, Alam MS. Do all children need a cycloplegic refraction? A comparison of Mohindra's versus cycloplegic refraction. Indian J Ophthalmol. 2020;68:2458-2461. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 154. | Atiya A, Hussaindeen JR, Kasturirangan S, Ramasubramanian S, Swathi K, Swaminathan M. Frequency of undetected binocular vision anomalies among ophthalmology trainees. J Optom. 2020;13:185-190. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 155. | Czepita M, Czepita D, Lubiński W. The Influence of Environmental Factors on the Prevalence of Myopia in Poland. J Ophthalmol. 2017;2017:5983406. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 156. | Ale Magar JB, Shah SP. Accommodative Lag Persistence in Treated Anisometropic, Strabismic, and Mixed Amblyopia. J Ophthalmol. 2022;2022:2133731. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 157. | Nguyen AT, Wayne JL, Ravikumar A, Manny RE, Anderson HA. Accommodative accuracy by retinoscopy versus autorefraction spherical equivalent or horizontal meridian power. Clin Exp Optom. 2018;101:778-785. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 158. | Chen AM, Manh V, Candy TR. Longitudinal Evaluation of Accommodation During Treatment for Unilateral Amblyopia. Invest Ophthalmol Vis Sci. 2018;59:2187-2196. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 159. | Ramamurthy D, Radhakrishnan H, Pardhan S. Associations between Accommodative Facility, Age, and Refractive Errors in Early, Older Adolescent Myopes and Emmetropes. Br Ir Orthopt J. 2023;19:15-25. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 160. | Manh V, Chen AM, Tarczy-Hornoch K, Cotter SA, Candy TR. Accommodative performance of children with unilateral amblyopia. Invest Ophthalmol Vis Sci. 2015;56:1193-1207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 161. | Ozdemir O, Tunay ZO, Acar DE, Acar U. Refractive errors and refractive development in premature infants. J Fr Ophtalmol. 2015;38:934-940. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 162. | Taneja M. Commentary: Renewed interest in off-axis retinoscopy and peripheral refraction for it's role in control of myopia progression. Indian J Ophthalmol. 2022;70:781-782. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 163. | Mohaghegh S, Kangari H, Masoumi SJ, Bamdad S, Rahmani S, Abdi S, Fazil N, Shahbazi S. Prevalence and risk factors of keratoconus (including oxidative stress biomarkers) in a cohort study of Shiraz university of medical science employees in Iran. BMC Ophthalmol. 2023;23:188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 164. | Naderan M, Jahanrad A, Farjadnia M. Clinical biomicroscopy and retinoscopy findings of keratoconus in a Middle Eastern population. Clin Exp Optom. 2018;101:46-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 165. | Zhang LJ, Traish AS, Dohlman TH. Temporal keratoconus in a pediatric patient. Am J Ophthalmol Case Rep. 2023;32:101900. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 166. | Thiagarajan D, Zainal S, Alias R, Bastion MC. Clinical Study on Corneal Topographical Changes in Vernal Keratoconjunctivitis by Using OCULUS Pentacam®. Cureus. 2023;15:e33798. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 167. | Rashid ZA, Moodley VR, Mashige KP. Diagnosis and management of keratoconus by eye care practitioners in Kenya. BMC Ophthalmol. 2023;23:37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 168. | Serdarogullari H, Tetikoglu M, Karahan H, Altin F, Elcioglu M. Prevalence of keratoconus and subclinical keratoconus in subjects with astigmatism using pentacam derived parameters. J Ophthalmic Vis Res. 2013;8:213-219. [PubMed] |
| 169. | Vohra V, Tuteja S, Gurnani B, Chawla H. Collagen Cross Linking for Keratoconus. 2023 Jun 11. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. [PubMed] |
| 170. | Somer D, Karabulut E, Cinar FG, Altiparmak UE, Ünlü N. The Role of Dynamic Retinoscopy in Predicting Infantile Accommodative Esotropia and Influencing Emmetropization. J Binocul Vis Ocul Motil. 2018;68:54-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 171. | Mohammadpour M, Khorrami-Nejad M. Post-LASIK keratectasia in the context of a thicker than intended flap detected by anterior segment optical coherence tomography. SAGE Open Med Case Rep. 2021;9:2050313X211050462. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 172. | Papageorgiou E, Kardaras D, Kapsalaki E, Dardiotis E, Mataftsi A, Tsironi EE. Spasm of the near reflex: a common diagnostic dilemma? Int J Ophthalmol. 2021;14:541-546. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 173. | Seymen Z, Vural E, Eris E, Vural A, Ogreden T, Aslan O, Celebi ARC, Perente I. HandyRef-K: Comparison of the Latest Handheld Auto Refracto-keratometer with Retinomax and Plusoptix in Patients Younger than Three Years of Age. Beyoglu Eye J. 2019;4:32-37. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 174. | Guha S, Shah S, Shah K, Hurakadli P, Majee D, Gandhi S. A comparison of cycloplegic autorefraction and retinoscopy in Indian children. Clin Exp Optom. 2017;100:73-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 175. | Hernandez-Moreno L, Vallelado-Alvarez A, Martin R. Repeatability of ARK-30 in a pediatric population. Indian J Ophthalmol. 2018;66:1262-1267. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 176. | Panda L, Barik U, Nayak S, Barik B, Behera G, Kekunnaya R, Das T. Performance of Photoscreener in Detection of Refractive Error in All Age Groups and Amblyopia Risk Factors in Children in a Tribal District of Odisha: The Tribal Odisha Eye Disease Study (TOES) # 3. Transl Vis Sci Technol. 2018;7:12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 177. | Paff T, Oudesluys-Murphy AM, Wolterbeek R, Swart-van den Berg M, de Nie JM, Tijssen E, Schalij-Delfos NE. Screening for refractive errors in children: the plusoptiX S08 and the Retinomax K-plus2 performed by a lay screener compared to cycloplegic retinoscopy. J AAPOS. 2010;14:478-483. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 52] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 178. | Sravani NG, Nilagiri VK, Bharadwaj SR. Photorefraction estimates of refractive power varies with the ethnic origin of human eyes. Sci Rep. 2015;5:7976. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 30] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 179. | Maguire MG, Ying GS, Ciner EB, Kulp MT, Candy TR, Moore B; Vision in Preschoolers (VIP) Study Group. Detection of Significant Hyperopia in Preschool Children Using Two Automated Vision Screeners. Optom Vis Sci. 2022;99:114-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 180. | Prabhu AV, Thomas J, Ve RS, Biswas S. Performance of Plusoptix A09 Photo Screener in Refractive Error Screening in School Children Aged between 5 and 15 Years in the Southern Part of India. J Curr Ophthalmol. 2020;32:268-273. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 181. | Mu Y, Bi H, Ekure E, Ding G, Wei N, Hua N, Qian X, Li X. Performance of Spot Photoscreener in Detecting Amblyopia Risk Factors in Chinese Pre-school and School Age Children Attending an Eye Clinic. PLoS One. 2016;11:e0149561. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 39] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 182. | Yakar K. Anterior chamber depth and axial length affect clinical performance of Spot Vision Screener. Arq Bras Oftalmol. 2020;83:43-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 183. | Liu Z, Pazo EE, Ye H, Yu C, Xu L, He W. Comparing School-Aged Refraction Measurements Using the 2WIN-S Portable Refractor in Relation to Cycloplegic Retinoscopy: A Cross-Sectional Study. J Ophthalmol. 2021;2021:6612476. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 184. | Tuncer I, Zengin MO, Karahan E. Comparison of the Retinomax hand-held autorefractor versus table-top autorefractor and retinoscopy. Int J Ophthalmol. 2014;7:491-495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 185. | Rao DP, Negiloni K, Gurunathan S, Velkumar S, Sivaraman A, Baig AU, B K, Murali K. Validation of a Simple-to-Use, Affordable, Portable Wavefront Aberrometry-Based Auto Refractometer in a Paediatric Population. Clin Ophthalmol. 2022;16:4281-4291. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 186. | Ohlendorf A, Leube A, Wahl S. Steps towards Smarter Solutions in Optometry and Ophthalmology-Inter-Device Agreement of Subjective Methods to Assess the Refractive Errors of the Eye. Healthcare (Basel). 2016;4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 187. | Kuo YC, Wang JH, Chiu CJ. Comparison of open-field autorefraction, closed-field autorefraction, and retinoscopy for refractive measurements of children and adolescents in Taiwan. J Formos Med Assoc. 2020;119:1251-1258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 188. | Lei Y, Chen X, Cheng M, Li B, Jiang Y, Xu Y, Wang X. Comparisons of objective and subjective refraction with and without cycloplegia using binocular wavefront optometer with autorefraction and retinoscopy in school-age children. Graefes Arch Clin Exp Ophthalmol. 2023;261:1465-1472. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 189. | Ciuffreda KJ, Rosenfield M. Evaluation of the SVOne: A Handheld, Smartphone-Based Autorefractor. Optom Vis Sci. 2015;92:1133-1139. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 37] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 190. | Joseph S, Varadaraj V, Dave SR, Lage E, Lim D, Aziz K, Dudgeon S, Ravilla TD, Friedman DS. Investigation of the Accuracy of a Low-Cost, Portable Autorefractor to Provide Well-Tolerated Eyeglass Prescriptions: A Randomized Crossover Trial. Ophthalmology. 2021;128:1672-1680. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 191. | Padhy D, Bharadwaj SR, Nayak S, Rath S, Das T. Does the Accuracy and Repeatability of Refractive Error Estimates Depend on the Measurement Principle of Autorefractors? Transl Vis Sci Technol. 2021;10:2. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 192. | Kara C, Petricli IS. Accuracy of Photorefraction and Wavefront-Based Autorefraction in Children Under 3 Years of Age. Beyoglu Eye J. 2021;6:54-61. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 193. | Rauscher FG, Lange H, Yahiaoui-Doktor M, Tegetmeyer H, Sterker I, Hinz A, Wahl S, Wiedemann P, Ohlendorf A, Blendowske R. Agreement and Repeatability of Noncycloplegic and Cycloplegic Wavefront-based Autorefraction in Children. Optom Vis Sci. 2019;96:879-889. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 194. | Geremias A, Garcia NP, Moreira CAS, Barboza GNC, Barboza MNC. Clinical correlation between automated vision screening under cycloplegia and retinoscopy in young children. Arq Bras Oftalmol. 2023;86:232-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 195. | Neena R, Gopan A, Nasheetha A, Giridhar A. Can photoscreening effectively detect amblyogenic risk factors in children with neurodevelopmental disability? Indian J Ophthalmol. 2022;70:228-232. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 196. | Kaur K, Kannusamy V, Mouttapa F, Gurnani B, Venkatesh R, Khadia A. To assess the accuracy of Plusoptix S12-C photoscreener in detecting amblyogenic risk factors in children aged 6 months to 6 years in remote areas of South India. Indian J Ophthalmol. 2020;68:2186-2189. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 197. | Huang D, Chen X, Zhang X, Wang Y, Zhu H, Ding H, Bai J, Chen J, Fu Z, Wang Z, Liu H. Pediatric vision screening using the plusoptiX A12C photoscreener in Chinese preschool children aged 3 to 4 years. Sci Rep. 2017;7:2041. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 198. | Yan XR, Jiao WZ, Li ZW, Xu WW, Li FJ, Wang LH. Performance of the Plusoptix A09 photoscreener in detecting amblyopia risk factors in Chinese children attending an eye clinic. PLoS One. 2015;10:e0126052. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 34] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 199. | Chandrakanth P, Gosalia H, Verghese S, Narendran K, Narendran V. The Gimbalscope - A novel smartphone-assisted retinoscopy technique. Indian J Ophthalmol. 2022;70:3112-3115. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 200. | Cao YT, Che DY, Pan YL, Lu YL, Wang CY, Zhang XL, Yang YF, Zhao KK, Zhou JB. Artificial intelligence improves accuracy, efficiency, and reliability of a handheld infrared eccentric autorefractor for adult refractometry. Int J Ophthalmol. 2022;15:628-634. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 201. | Gramatikov BI. Detecting central fixation by means of artificial neural networks in a pediatric vision screener using retinal birefringence scanning. Biomed Eng Online. 2017;16:52. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 202. | Zou H, Shi S, Yang X, Ma J, Fan Q, Chen X, Wang Y, Zhang M, Song J, Jiang Y, Li L, He X, Jhanji V, Wang S, Song M. Identification of ocular refraction based on deep learning algorithm as a novel retinoscopy method. Biomed Eng Online. 2022;21:87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |