Published online Sep 20, 2024. doi: 10.5662/wjm.v14.i3.91169
Peer-review started: December 26, 2023
First decision: January 4, 2024
Revised: January 23, 2024
Accepted: March 11, 2024
Article in press: March 11, 2024
Published online: September 20, 2024
Processing time: 181 Days and 22.9 Hours
The aim of this study is to illustrate the complexity of pain management in chronic pancreatitis (CP). In this context, pain represents the most common and debilitating symptom, and it deeply affects patient’s quality of life. Multiple rating scales (unidimensional, bidimensional and multidimensional) have been prop
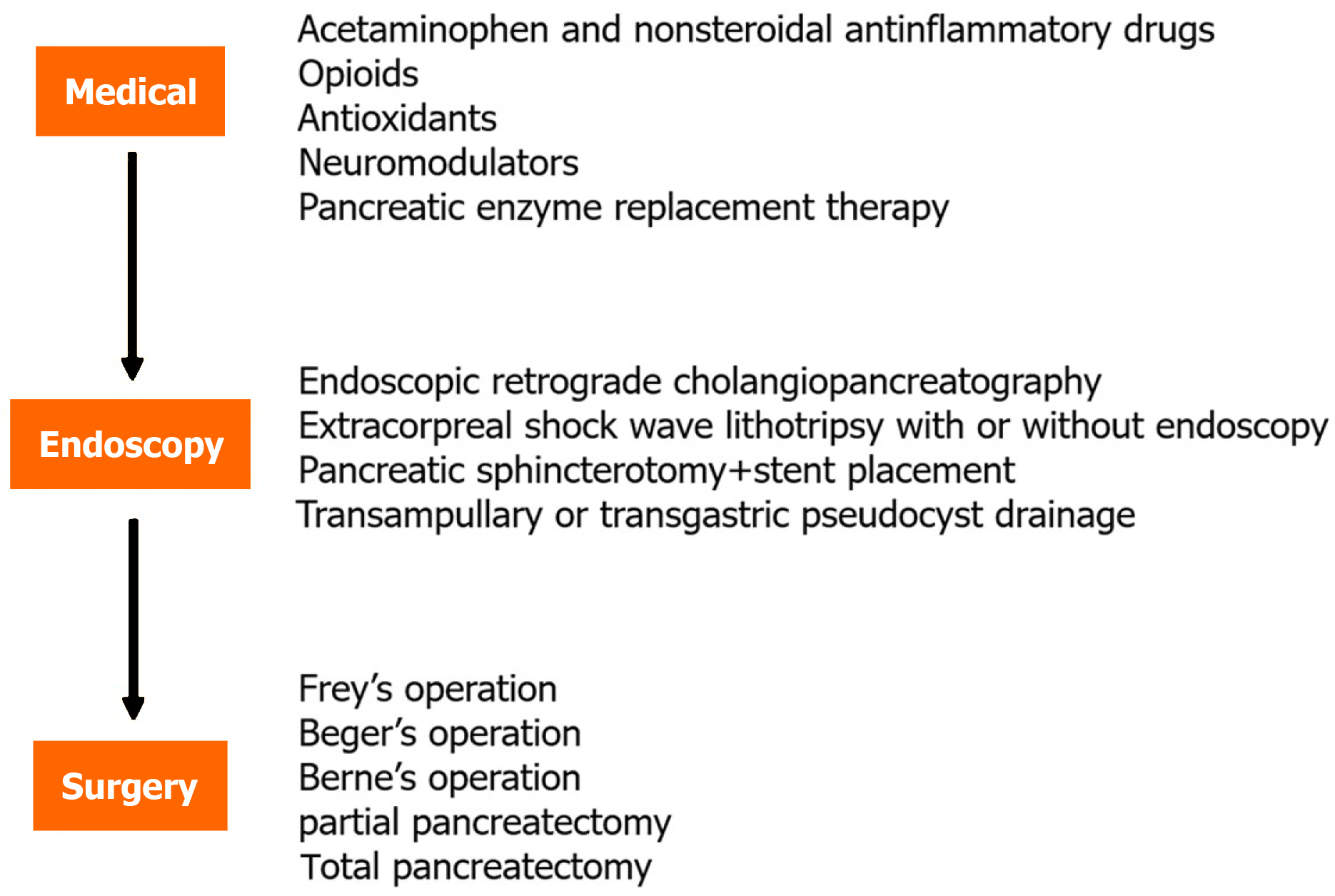
Core Tip: The aim of this review is to analyse and discuss treatment options in chronic pancreatitis management. Lifestyle change represents the starting point in uncomplicated chronic pancreatitis (CP). Medical treatment should be the first considered in a stepwise approach. The use of nonsteroidal anti-inflammatory drugs is the gold standard, but opioids, antioxidants, neuromodulators have important roles as well. Endoscopic retrograde cholangiopancreatography, extracorporeal shock wave lithotripsy with or without endoscopy, sphincterotomy with stent placement or transgastric drainage can be chosen in complicated CP patients with obstructions or pseudocysts. A decompressive or resection operation can be chosen in surgical treatment. In conclusion, CP pain management is an ongoing challenge because of lack of international consensus on protocols. Nowadays, a tailored step-up treatment discussed in a multidisciplinary setting is considered the best approach.
- Citation: Binetti M, Tonini V. Pain in chronic pancreatitis: What can we do today? World J Methodol 2024; 14(3): 91169
- URL: https://www.wjgnet.com/2222-0682/full/v14/i3/91169.htm
- DOI: https://dx.doi.org/10.5662/wjm.v14.i3.91169
Chronic pancreatitis (CP) is a progressive pancreatic disorder characterized by inflammation and fibrosis. The incidence and prevalence of CP remain low. The incidence is estimated about 4-12 per 100000 persons/year; while the prevalence is about 37-42 per 100000 persons/year. Abdominal pain represents its most disabling manifestation, and its prevalence in CP is about 80% of patients; painless pancreatitis only presents in 10%-20% of cases. In painless CP steatorrhea, malabsorption and endocrine dysfunction often develop[1].
In addition, acute and chronic pancreatitis represents a leading cause of hospital admissions[1]. Both genetic and environmental factors contribute to CP[2]. CP risk factors are summarised by the TIGAR-O acronym: T = Toxic (alcohol abuse, tobacco smoking, medications or toxins), I = Idiopathic (not associated with any known gene), G = Gene Mutation (complex genetics or modifying genes, ex. PRSS1, CFTR, SPINK1), A = Autoimmune (steroid responsive chronic pancreatitis), R = Recurrent (CP due to vascular diseases and post-irradiation damage), O = Obstructive (CP associated with pancreas divisum, Sphincter of Oddi disorder and duct obstruction)[3] and the M-ANNHEIM acronym includes: Alcohol and nicotine consumption, nutritional and hereditary factors, Efferent duct, Immunological, Miscellaneous and rare metabolic factors[4].
CP generally occurs together with mid-epigastric abdominal pain associated with nausea and vomiting[5]. In fact, abdominal pain represents the most frequent and debilitating symptom of chronic pancreatitis[6], and up to the 80% of patients with CP present recurrent episodes[2]. It is usually described starting in the epigastric zone with radiation to the back but may present variability[7]. The possible complete resolution of pain after the ongoing loss of pancreatic exocrine function remains a controversial topic[5]. CP presence could be associated to new onset diabetes (20%), steatorrhea (19%) and weight loss (16%) in painless patients[8]. CP patients can experience increased pain after eating, potentially leading to poor nutrition intake[9]. According to a recent review by Lukic et al[10] “chronic” abdominal pain persists for more than 3 mo.
Pain in CP has both somatic and visceral components. The afferent nerves of viscera terminate at various levels of the spinal cord, leading to a diffuse pain feeling. Part of the nerve projections involve sympathetic fibres, leading to nausea, diarrhoea and early satiety[11]. Considering CP clinical presentation, pain represents the most debilitating factor[3]. It has a great effect on quality of life (QoL). Pain severity can present as mild-moderate (18%) or severe (67%), and pain frequency can be intermittent (32%) or constant (53%)[2]. The aim of this study is to illustrate the complexity of pain management in CP. The underlying mechanisms of pain have been analysed, both in neuropathic and nociceptive components. The genetic role has been also described. After CP pain diagnosis, some unidimensional, bidimensional or multidimensional scales may be used to quantify the chronic pain. International guidelines have not been published yet. However, medical treatment is recommended as a first approach. In case of failure, endoscopic options can be tested. Surgical options should be chosen only in case of medical and endoscopic failure.
The diagnosis of CP remains a clinical challenge[12]. According to the United European Gastroenterology evidence-based Guidelines about CP diagnosis, endoscopic ultrasonography (US) recruits the highest possible number of patients, while endoscopic retrograde cholangiopancreatography (ERCP) and transabdominal US have the highest and lowest sensitivity, respectively[12].
Different scales can be used for pain assessment. The Numerical Pain Rating Scale is a one-dimensional rating scale and it is widely recommended, but multidimensional ones such as the Brief Pain Inventory and the McGill Pain Questionnaire are preferred[12]. General pain assessment tools can differentiate between[13]: Unidimensional tools: Pain visual analogue scale (VAS), pain numerical rating scale, pain intensity categories (mild, moderate, severe), pain improvement/relief categories, pain pattern (constant/intermitted), postprandial pain (yes/no or intensity); Bidimensional tools: Daily pain duration median pain VAS, number of days with pain median pain VAS, number of hours of pain median pain VAS, degree of frequency median pain VAS, pain frequency pain severity; Multidimensional tools: McGill Pain Questionnaire (full and short-form), PainDetect Questionnaire, pain score (intensity, frequency and consequences of pain). Some specific pain assessment tools in CP are reported: Izbicki pain score, Ammann (Type A&B), Type A-E, Group 1e3 pain patterns, QLQ-PAN28[13].
The mechanism of CP abdominal pain is complex. Although pancreatic damage represents a fundamental component, it also involves both nociceptive function and central pain perception[14,15].
Regarding pancreatic damage, acinar cell injury and pancreatic duct obstruction cause parenchymal ischemia, which is the base of abdominal pain in CP. This local ischemia induces inflammation that causes nociceptive stimulation of peripancreatic nerves. Repetitive stimulations can lead to permanent changes in spinal cord and cerebral cortex[7].
Nociceptive pain occurs after primary afferent neuron activation due to chemical or mechanical stimuli[16,17]. The exact nature of factors that actually activate intrapancreatic nociceptors is still unknown[18].
Neuropathy is an important component of CP pain. The continuous sensitization of central nociceptive receptors may result in a self-perpetuating pain state, which is independent from peripheral input[19]. Intrapancreatic nerves both increase in size (neural hypertrophy) and in number (neural invasion)[20].
In 2010, some authors analysed cortical reorganization in CP patients. They showed prolonged latencies of evoked potentials in the frontal region and in insular dipole localization. These findings showed that prolonged pain in CP patients leads to central reorganization[21]. The constant stimulation of afferent pathways leads to neuroplastic changes in the central nervous system (CNS) with overactivity of pain-related structures in a chronic activation setting. Various CNS areas are involved, such as the medial thalamus, the somatosensory cortex, the parietoinsular cortical regions and limbic areas[22].
Some biochemical studies have analysed specific molecules implicated in CP pain mechanisms. According to some authors, pancreatic nociceptor involvement with an increased excitability seems to be related to K+ current downregulation. TRPV1, nerve growth factor and protease activated receptor 2 seem to be involved[23]. Biochemical and histopathological characteristics in CP patients are similar to those observed in patients with other nerve fibre lesions[24]. Compared to healthy controls, CP patients also have increased glutamate/creatine (glu/cre) levels in the anterior cingulate cortex, while they have reduced N-acetylaspartete/creatine (NAA/cre) levels[25]. These mechanisms have been revealed by cerebral spectroscopy.
Chronic pancreatitis’ genetic profile has also been analysed. It plays an important role in pain perception and tolerance. Serum levels of transforming growth factor beta 1 seem to be higher in patients with nociceptive pain, while GP130 seems to be marker for neuropathic pain[26]. Some studies also suggest a role for neuromodulator drugs in the treatment of pain based on genetic susceptibility[27].
Over the years, many different theories have been proposed about the origin of pain in CP. It represents a multifactorial process. “Pancreatic duct hypertension” is considered one of the most accredited theories[28]. A direct relationship between pain and duct hypertension was first described by White et al[29]. It has been reproduced by infusing saline infusion with ductal pressure exceeding 25 mmHg.
In addition to histological changes, there are also CP-related functional changes[30], including maldigestion, diarrhea, weight loss and diabetes mellitus following islet-cell dysfunction[28].
The official guidelines for CP pain treatment have been prepared following CP clinical and diagnostic criteria revisions. The first guideline was created in 2009[31] and the second one in 2015[32]. The third edition was published in 2022, “Evidence-based clinical practice guidelines for chronic pancreatitis”[33], after the redefinition of CP as a pathogenic fibro-inflammatory syndrome.
The guidelines for pain management of pain In chronic pancreatitis (2017) contain recommendations from the Working Group for the International Consensus Guidelines for Chronic Pancreatitis in collaboration with the International Association of Pancreatology, American Pancreatic Association, Japan Pancreas Society and European Pancreatic Club[6].
The European Society for Gastrointestinal Endoscopy Guidelines recommend, in case of obstruction of pancreas head or body, endoscopic therapy with Extracorporeal shock wave lithotripsy with or without endoscopy (ESWL) as first treatment, followed by re-evaluation 6-8 wk later[34].
However, absolute indications about CP treatment are missing due to the lack of standardized protocols. International guidelines recognise a lack of international consensus about diagnostic tools and validated assessment in CP pain management.
Abdominal pain is a complex symptom and requires a tailored treatment[7]. Traditional pain management starts with lifestyle changes, such as cessation of both smoking and alcohol consumption[5,35]. According to 2017 guidelines abstinence from smoking has a weak recommendation, while abstinence from alcohol has a moderate recommendation[6]. Correct treatment of CP pain involves either anatomic and neurologic contribution to pain[7].
The World Health Organization recommends a stepwise approach[4]. To examinate CP pain management, it is useful to differentiate: CP Simple abdominal pain/back pain management; Complicated CP management: pancreatic pseudocyst, internal pancreatic fistula, biliary stenosis (Figure 1).
Abdominal or back pain are the most frequent presentation in uncomplicated CP.
Medical therapies are recommended for patients without pancreatic duct obstruction, with a lower severity of pain[7] according to a “pain relief ladder” principle, as proposed by the World Health Organization[19].
A stepwise CP pain management approach begins with acetaminophen and non-steroidal anti-inflammatory drugs, followed by low potency and longer acting opioids[4].
Acetaminophen: For many authors it is the first choice[36]. However, according to other authors, Paracetamol is safe but does not result in satisfactory pain relief[37].
Nonsteroidal anti-inflammatory drugs: According to the majority of authors, nonsteroidal anti-inflammatory drugs (NSAIDs) represent the first choice for analgesia in CP pain control. Only few studies evaluated the efficacy of various analgesics[38].
Opioids: Opioid analgesics are additive therapy in case of persistent or increasing pain. In this context, opioid use disorder is a risk. The careful selection of CP patients who would benefit from opioid therapy and predicting the risk of potential misuse should be applied[36]. According to Ratnayake et al[39], spinal cord stimulation is effective on reducing CP pain and has a potential effective role in reducing opioid use.
Antioxidants: Many antioxidants including vitamin A, C, E, selenium and methionine have been proven. The goal of antioxidant use is to decrease ‘ischemia-induced inflammation’, which could represent a peri-pancreatic nerve stimulus[4]. A sufficient dose of antioxidants should be recommended. However, according to some other authors, antioxidants are not related to better CP pain control[6,40]. A recent study concludes that a combination of antioxidants and Pregabalin significantly reduces CP pain[41].
Neuromodulators: Pregabalin, gabapentin, tricyclic antidepressants: Pregabalin was shown to reduce daily pain scores compared to placebo in a randomized study[7]. Considering 64 enrolled total patients, 36% of Pregabalin-treated patients against 24% Placebo-treated patients reported pain relief[15]. According to Cochrane Library, short-term use of Pregabalin decreases pain scores and opiate use but increases adverse events compared to placebo[42].
Pancreatic enzyme replacement therapy: Exogenous enzyme therapy may decrease enzyme secretion and improve malabsorption in patients with exocrine insufficiency. In addition, it is a non-invasive therapy with no adverse effects[43]. However, according to the most recent CP management guidelines, pancreatic enzyme replacement therapy (PERT) is not recommended but is useful for some abdominal symptoms, such as abdominal distension and flatulence in pancreatic exocrine dysfunction[33]. Decreased pancreatic secretion can be used if symptoms persist[44]. In regard to PERT therapy, doses of 1000 USP units of lipase × kg of patient body weight are advised to achieve nutritional parameter improvement[44].
Endoscopic or surgical therapy requires careful patient detection, especially regarding pancreatic anatomy. Patients with pancreatic duct dilatation may benefit from endoscopic or surgical therapies[45]. Therefore, patients may be classified as patients with structural abnormalities (called big-duct disease) and patients without anatomical abno
The advantages of endotherapy have been largely reported. In fact, endoscopic interventions can be repeated, if required, keeping surgical option valid[46]. International Guidelines[6] recommend ESWL as a safe and effective procedure for uncomplicated painful CP.
Endoscopic complications are divided into early and late complications. Early complications include cholangitis (especially related to sphincterotomy’s procedure), pseudocyst infection or pancreatic duct damage[46]. However, endoscopic therapy for CP appears to be a safe and effective option[47]. In the last decade, endoscopic-ultrasound (EUS) guided celiac plexus neurolysis role has been redefined, rediscussing both the technique and patient selection[48].
Surgical treatment is recommended for patients when endoscopic treatment has failed for pain relief[33]. Some authors tried to prepare a classification system to establish an international system of pain and QoL surveillance (M-ANNHEIM score)[19].
A recent randomized clinical trial (ESCAPE trial) showed that surgical treatment could be more effective than endoscopic first approach for mid-term and long-term pain relief[49]. In this study, a later pancreaticjejunostomy according to Partington and Rochelle is recommended in patients with non-enlarged pancreatic head (< 4 cm). On the other hand, a resection with duodenum preserving is performed for patients with enlarged pancreatic head (> 4 cm)[49].
According to Ratnayake et al[50], the Frey procedure is considered the best surgical treatment considering post-operative QoL improvement. It is also considered the procedure with lower complications considering POPF (post-operative pancreatic fistula) and PEI (post-operative exocrine insufficiency).
Pancreatic pseudocyst: 20%-40% of CP cases present with pseudocyst. The exact pathogenesis is still unknown. The blockage of the main pancreatic duct and ongoing pancreatic secretion seems to lead to pseudocyst formation[51].
Internal pancreatic fistula: A pancreatic fistula may present both in chronic and acute pancreatitis. It may occur as an asymptomatic cyst or sepsis from infected fluid collection. Minor leaks could be treated in a conservative way. In other cases, an interventional radiologist, skilled endoscopist or a surgeon should be involved[52].
Biliary stenosis: Progressive and irreversible fibrosis of the pancreatic parenchyma in CP leads to benign biliary strictures. In this context, first line therapy is interventional endoscopy with stenting[53].
Pseudoaneurysm: Pseudoaneurysm is a rare complication of CP due to the erosion of peripancreatic vessels by lipolytic and proteolytic enzymes. CP pseudoaneurysms are more common in patients with alcohol abuse[54].
The aim of an endoscopic approach is to remove obstructing pancreatic obstacles. Endoscopy strategies can achieve therapeutic benefits related to pancreatic outflow obstruction relief to alleviate pain[44]. Significant pain relief can be obtained when ductal irregularities are corrected, stones are extracted and strictures eliminated[44].
All endoscopic interventions are performed by expert endoscopists under consciousness sedation. Some strategies are:
ERCP: Patients with stones and ductal strictures can benefit from drainage procedures[2]. However, ductal stones or strictures often occur in the late stages of disease[45]. They are common both in alcoholic and hereditary pancreatitis. A dilatation with stenting procedure is required or a removal of main duct stones could be chosen in patients with non-enlarged pancreatic head (< 4 cm).
ESWL: It is indicated for disintegrated stones in main pancreatic duct, which are impossible to remove with other endoscopic therapies[19].
According to the 2017 Guidelines[6], ESWL for pancreatic stones is only recommended for ductal stones of 2-5 mm calcified or radiolucent stones. The SCHOKE (Extracorporeal Shock Wave Lithotripsy and Endotherapy for Pain in Chronic Pancreatitis) trial is a randomized controlled trial that demonstrated the effectiveness of external lithotripsy in pancreatic duct decompression and pain relief[55].
Pancreatic sphincterotomy and stent placement for pain relief: An important topic is the role of pancreatic duct stenting in CP. Nowadays, the “on demand stent replacement” instead of “intervals stent replacement” is preferred. The first choice might provide good palliation in CP pain[56].
Transampullary or transgastric drainage of pseudocyst: Pseudocyst drainage should be restricted to patients with important sequelae, such as infection, early satiety and weight loss. According to recent literature, endoscopic pseudocyst treatment has lower mortality and higher success rate than a surgical approach[47]. Both transpapillary and transmural approaches can be used. An EUS-guided transmural approach is preferred for large pseudocysts (d > 5 cm)[47].
All procedures have been studied in adult CP patients and no prospective or randomized controlled trials about CP endoscopic therapy in children have been published[57].
Pain represents the most common indication for operative CP management[4]. Some authors consider early surgery as the best choice. According to these authors an early surgical intervention is associated with improved pain control[58]. A proposed cutoff of early surgery is 26.5 mo from symptom onset.
A surgical approach should be suggested: (1) In the 1st 2/3 years after clinical symptoms onset; (2) For patients with five or less endoscopic procedures; and (3) For patients without opioid medical treatment.
Generally, the surgical procedures for pain treatment in CP patients can be divided in: Decompressive procedures, focused on ductal hypertension; Resection procedures, focused on inflammatory masses/stones in the pancreas head. The pancreatic head is the most innervated part of the organ. In this context, surgical removal of pancreatic head results in outflow amelioration. The removal of the inflamed pancreatic head leads to pain relief because it removes the enlarged nerves and improves outflow obstruction[30]. In regard to pancreatic resections, there are many options. The classic Whipple operation or pylorus sparing sacrifices extensive pancreatic resection. Limited pancreatic head resection is involved in Beger’s operation and a more extensive drainage procedure is done in Frey operation, combining a longitudinal incision of pancreatic duct and excavation. The Berne procedure (a modified Beger procedure) does not include pancreatic head detachment[59].
In 2022, Waage et al[60] generated a CP surgical treatment algorithm considering firstly the presence of pancreatic duct dilatation. DPPHR (duodenum-preserving pancreatic head resection) is necessary in the case of pancreatic duct dilatation with pancreatic head pseudotumor or parenchymal calcification. Among DPPHR, the Frey’s procedure is preferred. A pancreatic-jejunostomy is chosen in case of pancreatic duct dilatation but in the absence of pseudotumor/parenchymal calcification[61]. On the other hand, total pancreatectomy procedure is achieved in small duct disease. Distal pancreatectomy with or without splenectomy is indicated for CP tail pathology[60].
According to Skube et al[62], Frey’s procedure is indicated for patients with main pancreatic duct dilatation and pancreatic head disease. On the other hand, Beger and Berne modification are indicated in patients with pancreatic head or duodenum and/or common bile duct disease involvement.
Chronic pancreatitis represents a leading cause of hospitalization. One of the most important and common symptoms related to CP is pain[63]. It usually involves the upper abdomen, often radiating to the back and worsened by meals[16,28].
According to some authors, pain level is also related to CP etiology[28]. In alcohol-induced CP, pain is a constant symptom, while in “senile” or delayed-onset CP, the painless course is more frequent (50%). According to Amman et al[64], two different patterns are recognised: Type A: Characterised by recurrent episodes of abdominal pain; Type B: Characterised by prolonged or persistent pain.
Type A is characterised by short periods of pain and long pain-free intervals. Patients with type A pain are managed medically. On the other hand, type B has been hypothesised to be due to local complications, needing surgical intervention to achieve pain relief[65]. Completely painless chronic pancreatitis is a very rare form of CP[8].
However, according to a recent study by Kempeneers et al[66], the continuous and intermittent pain patterns in CP seem not to be two different pathophysiological entities. In fact, no differences in imaging and disease duration have been highlighted. According to the same study, different sub-patterns can be identified in the continuous: Persistent pain with slight fluctuation, persistent pain with pain attacks and pain attacks with pain between them. All of these different pain patterns can be mixed with each other.
At the beginning of 2000, CP mechanisms have been largely analysed and two different theories have been proposed: The neurogenic theory and the intraductal/intraparenchymal hypertension theory. According to the first one, CP is generated by a result of increased pressures, like in compartment syndrome. While, according to the second one, pain is generated by noxious substances on peripancreatic nerves[67]. However, nowadays, the complexity of CP is well recognised.
The most important effect of pain is the worsening of QoL. Psychiatric comorbidities are prevalent in CP patients. The effect of anxiety seems to be mediated via pain, while depression is independently related to QoL[68,69].
Pain has a central role in CP treatment[70]. An increasing number of studies elucidated the efficacy of a mechanism-based-treatment with specific analgesic protocol[71].
The optimal management of CP involves several specialties and, similar to cancer patients, may benefit from a multidisciplinary team[60,72].
In the past, many different surgical approaches to CP pain treatments have been proposed, such as the DuVal procedure, involving pancreatic tail resection with splenectomy followed by pancreatic jejunostomy, in order to improve retrograde drainage and pain[4]. However, a conservative step-up approach is currently considered the gold standard[73].
Alcohol and smoking cessation is suggested and a low-fat diets is also useful[37]. The medical treatment is considered the first approach[74]. The “three-step ladder” is largely adopted in this context. The first medical step is NSAID use. Opioid analgesics are commonly used, but they cannot be used for long-term treatment protocols, because of dependence risk and complications[37]. A combined antioxidant therapy seems to be safe and effective in CP pain relief[75].
A non-conservative approach is then attempted in case of conservative treatment failure. Endoscopy is considered a good alternative to surgery since the early years of 2000[76]. During the last 2 decades, the advancement of pancreatic endotherapy has given a significant contribution to the management of pancreatic pain.
In CP, main pancreatic duct obstruction caused by stricture or stones or by a combination of both requires interventional endoscopy or surgical approach[56]. These interventions and decreasing intraductal pancreatic pressure, can provide pain relief[77]. Pain represents the most common indication for operative CP management[4].
Among endoscopic therapies, an ERCP including dilatation with stenting procedure is required. An expertise endo
On the other hand, the surgical approach involves decompressive or resection procedures. The first ones focus on ductal hypertension, while the second ones focus on inflammatory masses/stones. Among surgical procedures, the Frey operation combines a longitudinal incision of pancreatic duct and parenchyma excavation, the Beger procedure is a limited pancreatic head resection, while Berne modification procedure involves a more limited pancreatic head resection[62]. In case of intraductal papillary mucinous neoplasm or suspected malignancy, a partial pancreatectomy is indicated. In the case of intractable disease, hereditary pancreatitis or small duct disease a total pancreatectomy should be necessary[62].
Some observational studies have suggested that the early surgery could reduce a disease progression, preserving pancreatic function[49].
An important challenge is the difficulty to compare different treatment efficacies in pain relief because of the lack of an international scale for pain comparison[11]. However, the Pancreatitis-Quantitative Sensory Testing consortium is working on meta-analysis comparing endoscopic and surgical treatments[17].
A recent systematic review including only randomized clinical trials comparing short-term and long-term outcomes showed superior results in surgical interventions compared to endoscopic ones. The number of complications is similar in both groups[77]. However, no definitive or international consensus has been achieved.
The new frontiers of interests in CP pain treatment have been reported in an article by Maydeo et al[78]. Being less invasive with acceptable complications, they prefer endoscopic approaches as first treatment. They also consider endotherapy the best in cost-effectiveness, because of biodegradable stents that reduce overall cost.
In conclusion, CP pain management is an ongoing challenge. Many different mechanisms are involved in CP pain onset. A tailored treatment for each patient allows for faster and effective pain control. Much progress has been made in CP pain comprehension and treatment, but the lack of international treatment protocols remains a major problem[79]. Nowadays, a step-up tailored treatment discussed in a multidisciplinary setting is considered the gold standard.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Sanayeh EB, Lebanon S-Editor: Liu JH L-Editor: Filipodia P-Editor: Yu HG
| 1. | Strum WB, Boland CR. Advances in acute and chronic pancreatitis. World J Gastroenterol. 2023;29:1194-1201. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Cited by in RCA: 15] [Article Influence: 7.5] [Reference Citation Analysis (2)] |
| 2. | Joyce C, Marsh RW, Thompson GB. The prevalence of mental handicap in New Zealand. N Z Med J. 1988;101:660-662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 299] [Article Influence: 49.8] [Reference Citation Analysis (0)] |
| 3. | Kleeff J, Whitcomb DC, Shimosegawa T, Esposito I, Lerch MM, Gress T, Mayerle J, Drewes AM, Rebours V, Akisik F, Muñoz JED, Neoptolemos JP. Chronic pancreatitis. Nat Rev Dis Primers. 2017;3:17060. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 255] [Cited by in RCA: 310] [Article Influence: 38.8] [Reference Citation Analysis (0)] |
| 4. | Maatman TK, Zyromski NJ. Chronic Pancreatitis. Curr Probl Surg. 2021;58:100858. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 5. | Lew D, Afghani E, Pandol S. Chronic Pancreatitis: Current Status and Challenges for Prevention and Treatment. Dig Dis Sci. 2017;62:1702-1712. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 87] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 6. | Drewes AM, Bouwense SAW, Campbell CM, Ceyhan GO, Delhaye M, Demir IE, Garg PK, van Goor H, Halloran C, Isaji S, Neoptolemos JP, Olesen SS, Palermo T, Pasricha PJ, Sheel A, Shimosegawa T, Szigethy E, Whitcomb DC, Yadav D; Working group for the International (IAP – APA – JPS – EPC) Consensus Guidelines for Chronic Pancreatitis. Guidelines for the understanding and management of pain in chronic pancreatitis. Pancreatology. 2017;17:720-731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 241] [Cited by in RCA: 197] [Article Influence: 24.6] [Reference Citation Analysis (0)] |
| 7. | Hart PA, Conwell DL. Chronic Pancreatitis: Managing a Difficult Disease. Am J Gastroenterol. 2020;115:49-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 87] [Article Influence: 17.4] [Reference Citation Analysis (0)] |
| 8. | Amodio A, De Marchi G, de Pretis N, Crinò SF, D'Onofrio M, Gabbrielli A, Ciccocioppo R, Frulloni L. Painless chronic pancreatitis. Dig Liver Dis. 2020;52:1333-1337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 9. | O'Brien SJ, Omer E. Chronic Pancreatitis and Nutrition Therapy. Nutr Clin Pract. 2019;34 Suppl 1:S13-S26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 27] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 10. | Lukic S, Mijac D, Filipovic B, Sokic-Milutinovic A, Tomasevic R, Krstic M, Milosavljevic T. Chronic Abdominal Pain: Gastroenterologist Approach. Dig Dis. 2022;40:181-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 11. | Kuhlmann L, Olesen SS, Drewes AM. Assessment of visceral pain with special reference to chronic pancreatitis. Front Pain Res (Lausanne). 2022;3:1067103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 12. | Beyer G, Habtezion A, Werner J, Lerch MM, Mayerle J. Chronic pancreatitis. Lancet. 2020;396:499-512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 308] [Article Influence: 61.6] [Reference Citation Analysis (1)] |
| 13. | McBride RL, Feringa ER, Garver MK, Williams JK Jr. Prelabeled red nucleus and sensorimotor cortex neurons of the rat survive 10 and 20 weeks after spinal cord transection. J Neuropathol Exp Neurol. 1989;48:568-576. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 14. | Dunbar EK, Saloman JL, Phillips AE, Whitcomb DC. Severe Pain in Chronic Pancreatitis Patients: Considering Mental Health and Associated Genetic Factors. J Pain Res. 2021;14:773-784. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 15. | Gupte A, Goede D, Tuite R, Forsmark CE. Chronic pancreatitis. BMJ. 2018;361:k2126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 16. | Puylaert M, Kapural L, Van Zundert J, Peek D, Lataster A, Mekhail N, van Kleef M, Keulemans YC. 26. Pain in chronic pancreatitis. Pain Pract. 2011;11:492-505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 17. | Rose EH. The high-tech hand surgery interface. Clin Plast Surg. 1986;13:333-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 20] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 18. | Demir IE, Tieftrunk E, Maak M, Friess H, Ceyhan GO. Pain mechanisms in chronic pancreatitis: of a master and his fire. Langenbecks Arch Surg. 2011;396:151-160. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 66] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 19. | Schneider A, Hirth M. Pain Management in Chronic Pancreatitis: Summary of Clinical Practice, Current Challenges and Potential Contribution of the M-ANNHEIM Classification. Drugs. 2021;81:533-546. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 20. | Demir IE, Friess H, Ceyhan GO. Neural plasticity in pancreatitis and pancreatic cancer. Nat Rev Gastroenterol Hepatol. 2015;12:649-659. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 179] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 21. | Olesen SS, Frøkjær JB, Lelic D, Valeriani M, Drewes AM. Pain-associated adaptive cortical reorganisation in chronic pancreatitis. Pancreatology. 2010;10:742-751. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 48] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 22. | Fregni F, Pascual-Leone A, Freedman SD. Pain in chronic pancreatitis: a salutogenic mechanism or a maladaptive brain response? Pancreatology. 2007;7:411-422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 34] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 23. | Pasricha PJ. Unraveling the mystery of pain in chronic pancreatitis. Nat Rev Gastroenterol Hepatol. 2012;9:140-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 75] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 24. | Drewes AM, Krarup AL, Detlefsen S, Malmstrøm ML, Dimcevski G, Funch-Jensen P. Pain in chronic pancreatitis: the role of neuropathic pain mechanisms. Gut. 2008;57:1616-1627. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 126] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 25. | Hansen TM, Muthulingam JA, Drewes AM, Olesen SS, Frøkjær JB. Cingulate glutamate levels associate with pain in chronic pancreatitis patients. Neuroimage Clin. 2019;23:101925. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 26. | Saloman JL, Li Y, Stello K, Li W, Li S, Phillips AE, Hall K, Fogel EL, Vege SS, Li L, Andersen DK, Fisher WE, Forsmark CE, Hart PA, Pandol SJ, Park WG, Topazian MD, Van Den Eeden SK, Serrano J, Conwell DL, Yadav D; Consortium for the Study of Chronic Pancreatitis, Diabetes, and Pancreatic Cancer (CPDPC). Serum Biomarkers of Nociceptive and Neuropathic Pain in Chronic Pancreatitis. J Pain. 2023;24:2199-2210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 27. | Faghih M, Drewes AM, Singh VK. Psychiatric Disease Susceptibility and Pain in Chronic Pancreatitis: Association or Causation? Am J Gastroenterol. 2021;116:2026-2028. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 28. | Fasanella KE, Davis B, Lyons J, Chen Z, Lee KK, Slivka A, Whitcomb DC. Pain in chronic pancreatitis and pancreatic cancer. Gastroenterol Clin North Am. 2007;36:335-364, ix. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 56] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 29. | White TT, Bourde J. A new observation on human intraductal pancreatic pressure. Surg Gynecol Obstet. 1970;130:275-278. [PubMed] |
| 30. | Demir E, Safak O, Friess H, Demir IE. Pain in chronic pancreatitis: mechanics or molecules? Pain Manag. 2020;10:205-208. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 31. | Shimosegawa T, Kataoka K, Kamisawa T, Miyakawa H, Ohara H, Ito T, Naruse S, Sata N, Suda K, Hirota M, Takeyama Y, Shiratori K, Hatori T, Otsuki M, Atomi Y, Sugano K, Tanaka M. The revised Japanese clinical diagnostic criteria for chronic pancreatitis. J Gastroenterol. 2010;45:584-591. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 141] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 32. | Ito T, Ishiguro H, Ohara H, Kamisawa T, Sakagami J, Sata N, Takeyama Y, Hirota M, Miyakawa H, Igarashi H, Lee L, Fujiyama T, Hijioka M, Ueda K, Tachibana Y, Sogame Y, Yasuda H, Kato R, Kataoka K, Shiratori K, Sugiyama M, Okazaki K, Kawa S, Tando Y, Kinoshita Y, Watanabe M, Shimosegawa T. Evidence-based clinical practice guidelines for chronic pancreatitis 2015. J Gastroenterol. 2016;51:85-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 107] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 33. | Shimizu K, Ito T, Irisawa A, Ohtsuka T, Ohara H, Kanno A, Kida M, Sakagami J, Sata N, Takeyama Y, Tahara J, Hirota M, Fujimori N, Masamune A, Mochida S, Enomoto N, Shimosegawa T, Koike K. Evidence-based clinical practice guidelines for chronic pancreatitis 2021. J Gastroenterol. 2022;57:709-724. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 37] [Reference Citation Analysis (0)] |
| 34. | Dumonceau JM, Delhaye M, Tringali A, Dominguez-Munoz JE, Poley JW, Arvanitaki M, Costamagna G, Costea F, Devière J, Eisendrath P, Lakhtakia S, Reddy N, Fockens P, Ponchon T, Bruno M. Endoscopic treatment of chronic pancreatitis: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2012;44:784-800. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 203] [Cited by in RCA: 188] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 35. | Olesen SS, Kuhlmann L, Novovic S, Nøjgaard C, Kalaitzakis E, Jensen NM, Engjom T, Dimcevski G, Waage A, Haas SL, Vujasinovic M, Riauka R, Pukitis A, Ozola-Zālīte I, Okhlobystin A, Parhiala M, Laukkarinen J, Drewes AM; Scandinavian Baltic Pancreatic Club. Association of multiple patient and disease characteristics with the presence and type of pain in chronic pancreatitis. J Gastroenterol Hepatol. 2020;35:326-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 36. | Shah I, Sheth SG, Kothari DJ. Pain management in chronic pancreatitis incorporating safe opioid practices: Challenge accepted. World J Gastroenterol. 2021;27:3142-3147. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 7] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (1)] |
| 37. | Singh VK, Drewes AM. Medical Management of Pain in Chronic Pancreatitis. Dig Dis Sci. 2017;62:1721-1728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 38. | Sharma V, Rana SS, Bhasin DK. Medical management of pain in chronic pancreatitis. Trop Gastroenterol. 2014;35:205-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 39. | Ratnayake CB, Bunn A, Pandanaboyana S, Windsor JA. Spinal Cord Stimulation for Management of Pain in Chronic Pancreatitis: A Systematic Review of Efficacy and Complications. Neuromodulation. 2020;23:19-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 40. | Rustagi T, Njei B. Antioxidant therapy for pain reduction in patients with chronic pancreatitis: a systematic review and meta-analysis. Pancreas. 2015;44:812-818. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 32] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 41. | Sureshkumar S, Omang A, Anandhi A, Rajesh BS, Abdulbasith KM, Vijayakumar C, Palanivel C, Pazhanivel M, Kate V. Efficacy of Pregabalin and Antioxidants Combination in Reducing Pain in Chronic Pancreatitis: A Double Blind Randomized Trial. Dig Dis Sci. 2021;66:4017-4025. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 42. | Gurusamy KS, Lusuku C, Davidson BR. Pregabalin for decreasing pancreatic pain in chronic pancreatitis. Cochrane Database Syst Rev. 2016;2:CD011522. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 43. | Hobbs PM, Johnson WG, Graham DY. Management of pain in chronic pancreatitis with emphasis on exogenous pancreatic enzymes. World J Gastrointest Pharmacol Ther. 2016;7:370-386. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 18] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (3)] |
| 44. | Kichler A, Jang S. Chronic Pancreatitis: Epidemiology, Diagnosis, and Management Updates. Drugs. 2020;80:1155-1168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 44] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 45. | Chauhan S, Forsmark CE. Pain management in chronic pancreatitis: A treatment algorithm. Best Pract Res Clin Gastroenterol. 2010;24:323-335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 49] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 46. | Khanna S, Tandon RK. Endotherapy for pain in chronic pancreatitis. J Gastroenterol Hepatol. 2008;23:1649-1656. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 47. | Moran RA, Elmunzer BJ. Endoscopic treatment of pain in chronic pancreatitis. Curr Opin Gastroenterol. 2018;34:469-476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 48. | Wyse JM, Sahai AV. Endoscopic Ultrasound-Guided Management of Pain in Chronic Pancreatitis and Pancreatic Cancer: an Update. Curr Treat Options Gastroenterol. 2018;16:417-427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 49. | Issa Y, Kempeneers MA, Bruno MJ, Fockens P, Poley JW, Ahmed Ali U, Bollen TL, Busch OR, Dejong CH, van Duijvendijk P, van Dullemen HM, van Eijck CH, van Goor H, Hadithi M, Haveman JW, Keulemans Y, Nieuwenhuijs VB, Poen AC, Rauws EA, Tan AC, Thijs W, Timmer R, Witteman BJ, Besselink MG, van Hooft JE, van Santvoort HC, Dijkgraaf MG, Boermeester MA; Dutch Pancreatitis Study Group. Effect of Early Surgery vs Endoscopy-First Approach on Pain in Patients With Chronic Pancreatitis: The ESCAPE Randomized Clinical Trial. JAMA. 2020;323:237-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 160] [Article Influence: 32.0] [Reference Citation Analysis (0)] |
| 50. | Ratnayake CBB, Kamarajah SK, Loveday BPT, Nayar M, Oppong K, White S, French JJ, Windsor JA, Pandanaboyana S. A Network Meta-analysis of Surgery for Chronic Pancreatitis: Impact on Pain and Quality of Life. J Gastrointest Surg. 2020;24:2865-2873. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 51. | Andrén-Sandberg A, Dervenis C. Pancreatic pseudocysts in the 21st century. Part I: classification, pathophysiology, anatomic considerations and treatment. JOP. 2004;5:8-24. [PubMed] |
| 52. | Larsen M, Kozarek R. Management of pancreatic ductal leaks and fistulae. J Gastroenterol Hepatol. 2014;29:1360-1370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 77] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 53. | Ramchandani M, Pal P, Costamagna G. Management of Benign Biliary Stricture in Chronic Pancreatitis. Gastrointest Endosc Clin N Am. 2023;33:831-844. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 54. | Mitrovic M, Dugalic V, Kovac J, Tadic B, Milosevic S, Lukic B, Lekic N, Cvetic V. Successful Embolization of Posterior Inferior Pancreaticoduodenal Artery Pseudoaneurysm on the Grounds of Chronic Pancreatitis-Case Report and Literature Review. Medicina (Kaunas). 2020;56. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 55. | Olesen SS, Drewes AM, Gaud R, Tandan M, Lakhtakia S, Ramchandani M, Rao GV, Reddy DN, Talukdar R. Combined extracorporeal shock wave lithotripsy and endoscopic treatment for pain in chronic pancreatitis (SCHOKE trial): study protocol for a randomized, sham-controlled trial. Trials. 2020;21:338. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 56. | Etik DO, Parlak E, Oguz D, Oztas E, Kacar S, Onder FO, Sasmaz N, Sahin B. On demand pancreatic stenting in chronic pancreatitis might provide good palliation of pain. Acta Gastroenterol Belg. 2019;82:401-406. [PubMed] |
| 57. | Perito ER, Pohl JF, Bakker C, Armfield MA, Barth B, Cuneo A, Mascarenhas M, Mehta M, Schwarzenberg SJ. Outpatient Pain Management in Children With Chronic Pancreatitis: A Scoping Systematic Review. Pancreas. 2022;51:135-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 58. | Yang CJ, Bliss LA, Freedman SD, Sheth S, Vollmer CM, Ng SC, Callery MP, Tseng JF. Surgery for chronic pancreatitis: the role of early surgery in pain management. Pancreas. 2015;44:819-823. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 35] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 59. | Mihaljevic AL, Kleeff J, Friess H. Beger's operation and the Berne modification: origin and current results. J Hepatobiliary Pancreat Sci. 2010;17:735-744. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 60. | Waage A, Vinge-Holmquist O, Labori KJ, Paulsen V, Aabakken L, Lenz H, Felix Magnus HC, Tholfsen T, Hauge T. Tailored surgery in chronic pancreatitis after implementation of a multidisciplinary team assessment; a prospective observational study. HPB (Oxford). 2022;24:2157-2166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 61. | Yin Z, Sun J, Yin D, Wang J. Surgical treatment strategies in chronic pancreatitis: a meta-analysis. Arch Surg. 2012;147:961-968. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 37] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 62. | Skube ME, Beilman GJ. Surgical treatment of pain in chronic pancreatitis. Curr Opin Gastroenterol. 2018;34:317-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 63. | Rosendahl J. Understanding pain in chronic pancreatitis: not yet the end of the story? Gut. 2022;71:2378-2379. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 64. | Ammann RW, Muellhaupt B. The natural history of pain in alcoholic chronic pancreatitis. Gastroenterology. 1999;116:1132-1140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 284] [Cited by in RCA: 234] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 65. | Vipperla K, Kanakis A, Slivka A, Althouse AD, Brand RE, Phillips AE, Chennat J, Papachristou GI, Lee KK, Zureikat AH, Whitcomb DC, Yadav D. Natural course of pain in chronic pancreatitis is independent of disease duration. Pancreatology. 2021;21:649-657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 66. | Kempeneers MA, Issa Y, Verdonk RC, Bruno M, Fockens P, van Goor H, Alofs E, Bollen TL, Bouwense S, van Dalen ASHM, van Dieren S, van Dullemen HM, van Geenen EJ, Hoge C, van Hooft JE, Kager LM, Keulemans Y, Nooijen LE, Poley JW, Seerden TCJ, Tan A, Thijs W, Timmer R, Vleggaar F, Witteman B, Ahmed Ali U, Besselink MG, Boermeester MA, van Santvoort HC; Dutch Pancreatitis Study Group. Pain patterns in chronic pancreatitis: a nationwide longitudinal cohort study. Gut. 2021;70:1724-1733. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 35] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 67. | Sakorafas GH, Tsiotou AG, Peros G. Mechanisms and natural history of pain in chronic pancreatitis: a surgical perspective. J Clin Gastroenterol. 2007;41:689-699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 28] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 68. | Phillips AE, Faghih M, Drewes AM, Singh VK, Yadav D, Olesen SS; Pancreatic Quantitative Sensory Testing (P-QST) Consortium. Psychiatric Comorbidity in Patients With Chronic Pancreatitis Associates With Pain and Reduced Quality of Life. Am J Gastroenterol. 2020;115:2077-2085. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 46] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 69. | Parasar K, Mohan S, John AG, Anand U. Pain in Chronic Pancreatitis During the COVID-19 Lockdown: Has It Given Us a New Dimension for Treatment? Cureus. 2021;13:e13423. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 70. | Buscaglia JM, Chang L. Pain Phenotypes in Chronic Pancreatitis: Beginning to Fine-tune Our Approach to Treatment. Clin Gastroenterol Hepatol. 2022;20:28-30. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 71. | Kuhlmann L, Olesen SS, Olesen AE, Arendt-Nielsen L, Drewes AM. Mechanism-based pain management in chronic pancreatitis - is it time for a paradigm shift? Expert Rev Clin Pharmacol. 2019;12:249-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 72. | van Esch AA, Wilder-Smith OH, Jansen JB, van Goor H, Drenth JP. Pharmacological management of pain in chronic pancreatitis. Dig Liver Dis. 2006;38:518-526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 40] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 73. | Issa Y, van Santvoort HC, van Goor H, Cahen DL, Bruno MJ, Boermeester MA. Surgical and endoscopic treatment of pain in chronic pancreatitis: a multidisciplinary update. Dig Surg. 2013;30:35-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 28] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 74. | Gachago C, Draganov PV. Pain management in chronic pancreatitis. World J Gastroenterol. 2008;14:3137-3148. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 62] [Cited by in RCA: 48] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 75. | Cai GH, Huang J, Zhao Y, Chen J, Wu HH, Dong YL, Smith HS, Li YQ, Wang W, Wu SX. Antioxidant therapy for pain relief in patients with chronic pancreatitis: systematic review and meta-analysis. Pain Physician. 2013;16:521-532. [PubMed] |
| 76. | de Silva M. Management of pain in chronic pancreatitis. New solutions to an old problem. Ceylon Med J. 2008;53:1-3. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 77. | Mendieta PJO, Sagae VMT, Ribeiro IB, de Moura DTH, Scatimburgo MVCV, Hirsch BS, Rocha RSP, Visconti TAC, Sánchez-Luna SA, Bernardo WM, de Moura EGH. Pain relief in chronic pancreatitis: endoscopic or surgical treatment? a systematic review with meta-analysis. Surg Endosc. 2021;35:4085-4094. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (1)] |
| 78. | Maydeo A, Kamat N, Dalal A, Patil G. Advances in the Management of Pain in Chronic Pancreatitis. Curr Gastroenterol Rep. 2023;25:260-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Reference Citation Analysis (0)] |
| 79. | Anderson MA, Akshintala V, Albers KM, Amann ST, Belfer I, Brand R, Chari S, Cote G, Davis BM, Frulloni L, Gelrud A, Guda N, Humar A, Liddle RA, Slivka A, Gupta RS, Szigethy E, Talluri J, Wassef W, Wilcox CM, Windsor J, Yadav D, Whitcomb DC. Mechanism, assessment and management of pain in chronic pancreatitis: Recommendations of a multidisciplinary study group. Pancreatology. 2016;16:83-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 65] [Article Influence: 7.2] [Reference Citation Analysis (0)] |