Published online Mar 20, 2024. doi: 10.5662/wjm.v14.i1.90930
Peer-review started: December 17, 2023
First decision: January 10, 2024
Revised: January 12, 2024
Accepted: February 20, 2024
Article in press: February 20, 2024
Published online: March 20, 2024
Processing time: 80 Days and 15.9 Hours
Selecting the optimal size of components is crucial when performing a primary total hip arthroplasty. Implanting the accurate size of the acetabular component can occasionally be exacting, chiefly for surgeons with little experience, whilst the complications of imprecise acetabular sizing or over-reaming can be potentially devastating.
To assist clinicians intraoperatively with a simple and repeatable tip in elucidating the ambivalence when determining the proper acetabular component size is not straightforwardly achieved, specifically when surgeons are inexperienced or preoperative templating is unavailable.
This method was employed in 263 operations in our department from June 2021 to December 2022. All operations were performed by the same team of joint reconstruction surgeons, employing a typical posterior hip approach technique. The types of acetabular shells implanted were: The Dynasty® acetabular cup system (MicroPort Orthopedics, Shanghai, China) and the R3® acetabular system (Smith & Nephew, Watford, United Kingdom), which both feature cementless press-fit design.
The mean value of all cases was calculated and collated with each other. We distinguished as oversized an implanted acetabular shell when its size was > 2 mm larger than the size of the acetabular size indicator reamer (ASIR) or when the implanted shell was larger than 4 mm compared to the preoperative planned cup. The median size of the implanted acetabular shell was 52 (48–54) mm, while the median size of the preoperatively planned cup was 50 (48–56) mm, and the median size of the ASIR was 52 (50–54) mm. The correlation coefficient between ASIR size and implanted acetabular component size exhibited a high positive correlation with r = 0.719 (P < 0.001). Contrariwise, intraoperative ASIR measurements precisely predicted the implanted cups’ size or differed by only one size (2 mm) in 245 cases.
In our study, we demonstrated that the size of the first acetabular reamer not entering freely in the acetabular rim corroborates the final acetabular component size to implant. This was also corresponding in the majority of the cases with conventional preoperative templating. It can be featured as a valid tool for avoiding the potentially pernicious complications of acetabular cup over-reaming and over-sizing in primary total hip arthroplasty. It is a simple and reproducible technical note useful for confirming the predicted acetabular cup size preoperatively; thus, its application could be considered routinely, even in cases where preoperative templating is unavailable.
Core Tip: The technique mentioned can be featured as a valid tool for avoiding the potentially pernicious complications of acetabular cup over-reaming and over-sizing in primary total hip arthroplasty. It is a simple and reproducible technical note useful for confirming the predicted acetabular cup size preoperatively; thus, its application could be considered routinely, even in cases where preoperative templating is unavailable.
- Citation: Karampinas P, Vlamis J, Galanis A, Vavourakis M, Krexi A, Sakellariou E, Patilas C, Pneumaticos S. Technical note for intraoperative determination of proper acetabular cup size in primary total hip arthroplasty. World J Methodol 2024; 14(1): 90930
- URL: https://www.wjgnet.com/2222-0682/full/v14/i1/90930.htm
- DOI: https://dx.doi.org/10.5662/wjm.v14.i1.90930
Total hip arthroplasty (THA) is indubitably a successful and cost-effective surgical procedure. For obtaining reproducibly consummate results, apposite preoperative planning is a mandatory routine. This planning involves diligent physical examination and X-ray templating, aiding in appropriate component size selection. Intraoperatively, acetabular shell over-sizing, acetabular bony deficits arising from acetabular reaming and acetabular cup over-medialization are all conditions to avoid during a THA[1-3]. Consequently, precise reaming and acetabular cup sizing must be estimated and selected during the operation. Ben Lulu et al[1] propounded the intra-operative measurement of the femoral head as a tool for optimal acetabular size selection. Additionally, a single-center study by Muñoz-Mahamud et al[2] indicated that this simple tool might demonstrate analogous validity and accuracy as preoperative digital templating regarding determining the definitive implanted acetabular cup size in primary THA.
Perusing the existing literature, limited papers examine preoperative or intraoperative methods for measuring acetabulum size and the correlations with implanted acetabular cup size in primary THA. The current study’s objective is to scrutinize the association between the intraoperative features of the last acetabular reamer utilized for the acetabulum preparation and the final acetabular cup implanted contrasted to the preoperative acetabular cup templating in primary THA and to bolster orthopaedic surgeons’ intraoperative decision-making in terms of the selection of the final acetabular component by providing a simple and repeatable technical note.
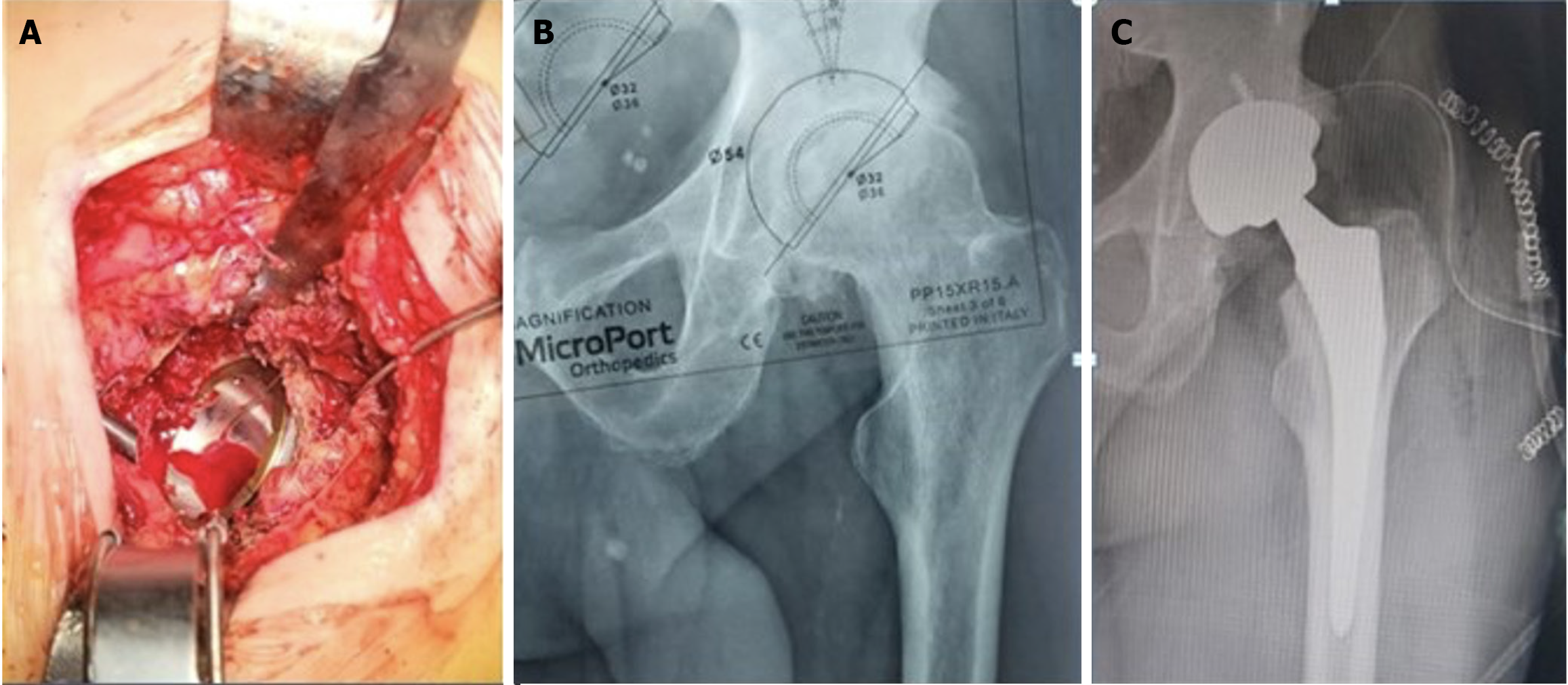
After acquiring approval from our Institution’s review board, a prospective observational single-center study was conducted in our department. From June 2021 to December 2022, all patients admitted to our hospital for elective primary THA were prospectively registered in a database and retrospectively reviewed. All operations were performed by the same team of joint reconstruction surgeons, employing a typical posterior hip approach technique. The types of acetabular shells implanted were: The Dynasty® acetabular cup system (MicroPort Orthopedics, Shanghai, China) and the R3® acetabular system (Smith & Nephew, Watford, UK), which both feature cementless press-fit design. Data were recorded regarding demographics, body mass index (BMI), comorbidities, indication for THA, hip approach, templated socket size, implanted cup outer diameter and acetabular cup type. Patients with a history of congenital/developmental hip deformity (Perthes’s disease, dysplasia), post-traumatic osteoarthritis, severe osteoarthritis with large acetabular osteophytes, and acetabular protrusion cases, were excluded from the study.
Our Institution’s picture archiving and communication system analyzed preoperative and postoperative radiographs. Regarding preoperative planning, acetabular size measurement was executed in traditional digital X-ray films (100% magnification) of anteroposterior pelvic and hip lateral views. To calibrate the image, we utilized known implanted femoral head component size. We then calculated the diameter of the contralateral native acetabulum size, assuming that patients’ femoral heads were generally symmetrical, apart from those with congenital/developmental hip deformities, which were excluded. To bolster the reliability of the measures, all X-ray films were examined by two of the authors. Each author performed three measurements. The three calculations were averaged to create the final value for that author. The average of the final values for each of the two authors was utilized as the final measurement for the analysis.
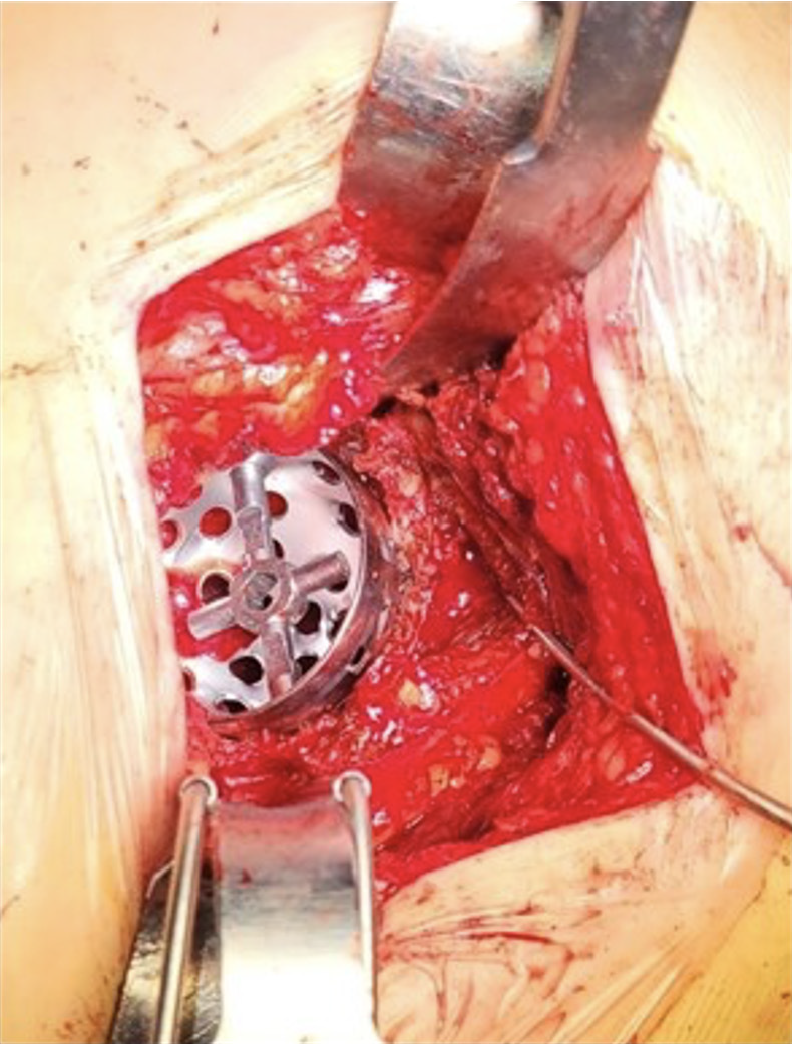
The last acetabular bone reamer used was defined as the acetabular size indicator reamer (ASIR), featuring a larger diameter than the acetabular rim, hence, not entering freely into it without cutting bone first (Figure 1). The Pearson correlation coefficient (r) was utilized to discover whether the reamer’s size correlated with the acetabular component size. The correlation size (Pearson correlation coefficient) was interpreted using the method delineated by Hinkle et al[4]. The level of statistical significance was set to P < 0.05, and all analyses were executed with the assistance of commercially available statistical software.
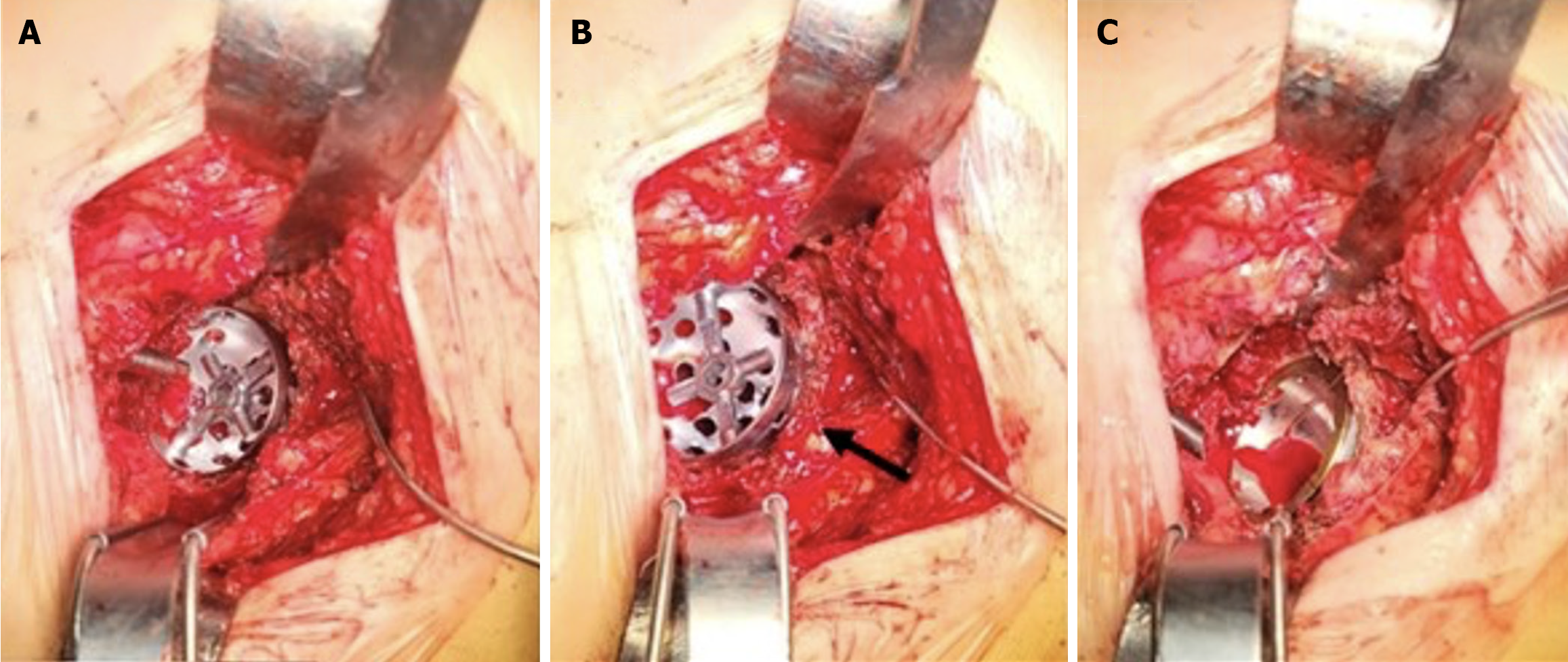
A conventional posterior approach was employed to expose the hip joint and acetabulum in all cases. After following the standardized steps of the operation, the acetabulum with bone reamers was prepared as described below: The first reamer utilized was the smaller one (43 mm), and then we continued by raising two numbers until the size of 47-48 mm. Until this point, all bone reamers enter the acetabulum cavity freely without resistance from the acetabular rim’s periphery. Reaming preparation starts from the acetabular fossa, while the reamers’ size is standardly rising symmetrically to the acetabulum until the subchondral bone is exposed. From the following sizes of acetabular reamers, 50 mm to 56 mm, the acetabulum periphery reaches a point where it is unattainable for the reamer to be inserted into the acetabulum cavity unobstructed because the maximum diameter of the reamer is bigger than that of the acetabular peripheral rim (Figure 2A). This exact reamer is the last used for the acetabular preparation after removing the acetabular bone periphery and small osteophytes. The size of the first reamer that is not feasible to be placed entirely into the acetabular cavity, gives us the size of the acetabular shell to implant (Figure 2B and C). This reamer has been defined as the ASIR. It is vitally important to underline that if the acetabular reaming process is carried on after that point, necessary bone from the acetabular periphery, acetabular rim, and the anterior and posterior walls is gradually removed, which could affect the implanted acetabular shell’s primary support.
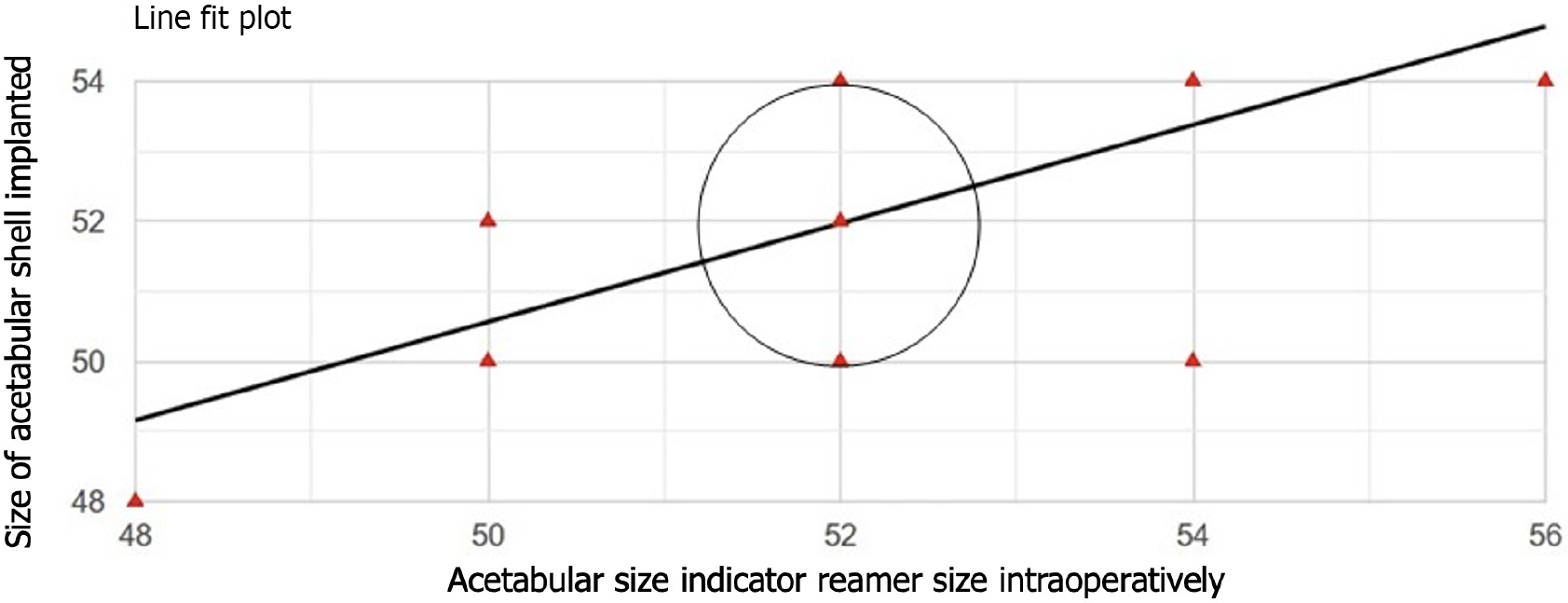
Out of 345 primary THAs performed, 263 cases were included in our study that met the inclusion criteria. The mean age of the patients was 68.1 years old (range 48-93). The majority (59%) of the patients were female, whilst mean BMI was 28.3 Kg/m2. Indications for surgery were osteoarthritis (241 cases), ischemic necrosis of the femoral head (9 cases) and femoral neck fracture (13 cases). We collected the data from the templating measurements for every single case. We juxtaposed them with the size of the final acetabular bone reamer (the ASIR) and the acetabular shell implanted. The mean value of all cases was calculated and collated with each other. We distinguished as oversized an implanted acetabular shell when its size was > 2 mm larger than the size of the ASIR or when the implanted shell was larger than 4 mm compared to the preoperative planned cup. The median size of the implanted acetabular shell was 52 (48–54) mm, while the median size of the preoperatively planned cup was 50 (48–56) mm, and the median size of the ASIR was 52 (50–54) mm (Table 1). The correlation coefficient between ASIR size and implanted acetabular component size exhibited a high positive correlation with r = 0.719 (P < 0.001) (Figure 3).
| Mean value templating | Mean value ‘fine reamer’ | Mean value cup implanted |
| 50 (48-56) mm | 52 (50-54) mm | 52 (48-56) mm |
Figure 4 depicts the correlation between the implanted acetabular shell and the preoperatively planned cup and intraoperative reaming measurement. The size of preoperatively planned cups precisely estimated the implanted shells’ size or differed by one size (2 mm) in 198 cases. Contrariwise, intraoperative ASIR measurements precisely estimated the implanted cups’ size or differed by one size (2 mm) in 245 cases (Table 2). The most frequently planned cup featured a 52 mm diameter in females, while 54 mm was the size most regularly implanted in males. Finally, it is paramount to accentuate that no alterations were discerned regarding the two types of acetabular implants employed in the study.
| Pre-operative templated cup size, % | Intra-operative reamer measurement, % | |
| Percentage of accurately prediction | 73.8 | 92.8 |
| Percentage of discrepancy > 1 size | 21.1 | 7.1 |
| Percentage of discrepancy > 2 size | 5.1 | 0.1 |
A few limitations apply to our technical note. First of all, our study group was limited to Caucasian patients living in Southern Europe. Furthermore, this technique may not be so accurate in patients with extremely severe osteoarthritis or in atypical cases such as congenital hip dysplasia. Finally, the technique was used by surgeons of the same institution/department and the postoperative follow-up was limited to 12 months.
Total hip arthroplasty aims for pertinent restoration of joint biomechanics. In terms of preoperative planning, precise and reliable evaluation of the appropriate acetabular component size is crucial. In general terms, the determination of the planned implant’s size can be carried out by specific overlays on standard plain X-rays, digital templating with or without the utilization of calibration to advanced imaging with EOS, computed tomography (CT), magnetic resonance imaging, and and customized guides for each patient[1-3]. Conventional planning is considered at least as robust as digital planning; however, contemporary literature is still contentious[5]. Anteroposterior pelvic radiographs are customarily used in preoperative THA templating. Information concerning the pelvis and contralateral hip anatomy enables the assessment of leg-length discrepancies[6]. The evaluation of bony morphology, arthritic wear pattern, and a proper implant design and size, is needed to restore joint’s biomechanics in present-day THA[3,7]. Sex, height and weight have all been indicated to be considerably associated with implant size[8].
Regarding existing literature on acetabular offset, the well-established biomedical theory of medialization appears as most prevalent for a better patient’s outcome. In this case, the acetabular preparation consists of reaming down to the true floor, thus medializing the hip’s rotation center and decreasing acetabular offset. This medialization dwindles the body weight’s lever arm during monopodial stance, diminishing the resultant force on the femoral head if every anatomic formation is intact[9]. Current literature focuses on reducing the acetabular offset in relation to the femoral offset, extensive criticism of this guideline has been observed[10-12]. Thorough preoperative planning may assist in avoiding excessive medialization of the acetabular cup, which is correlated to inferior outcomes following THA[10]. Orthopaedic surgeons should ream the medial cotyloid cavity to the floor until a suitable component size for implantation. This triggers medial and superior displacement of the hip’s rotational center to achieve a comparatively normal acetabular offset and rotation center[9]. Additionally, the exact preoperative planning reduces surgical time and number of complications[3,12]. Sharkey et al[10] reported that acetabular shell oversizing might be associated with enhanced rates of periprosthetic acetabular fractures, whilst undersizing might be connected to early implant loosening arising from insufficient press-fit. An oversized cup has been implicated in postoperative pain deriving from psoas impingement and anterior overhang[13-15].
Regarding preoperative templating, predicting the definite implant size ± one size is regarded as acceptable[12]. Templating accuracy has been proven to upgrade with the training level of the surgeon[16]. Previous experience augments preoperative templating performance, as clinicians accomplish proficiency in planning the acetabular cup size after 50-100 attempts when a succinct algorithm and immediate feedback are provided[3]. A direct correlation between radiographically measured native femoral head size and implanted acetabular shell size, has been conjugated in primary THA[5]. In accordance with the literature, preoperative planning of acetabular component size features a high level of accuracy, predicting the definite implant within ± one size in 80% to 100% of cases[11-12,17-19]. A retrospective study of 277 patients undergoing primary THA by Pfeufer et al[5] revealed a relation between the acetabular component’s size and radiographically measured contralateral native femoral head’s size, with a discrepancy of 7 mm. Moreover, digital radiographs’ templating accuracy in predicting the implant size has been gauged and found to be sufficiently good[8,9]. Nonetheless, digital templating demands special software provided by the companies. As these digital templates exhibit confined availability, many centers worldwide have halted templating prior to surgery. Therefore, surgeons incapable of procuring special digital templating software can resort to the typical acetate templates on digital radiographs[6]. Ben Lulu et al[1] computed the femoral head’s size intraoperatively, indicating a noteworthy association between the implanted shell’s diameter and the removed femoral head’s diameter calculated with calipers. Moreover, they recommended that measuring the femoral head’s diameter during surgery could be applied as a considerable intraoperative monitoring tool and, along with preoperative templating figures, may contribute to increased precision rates. Additionally, Muñoz-Mahamud et al[2] drew the inference that measuring the femoral head’s size intraoperatively is an uncomplicated and well-grounded method, availing surgeons selecting the optimal acetabular component size, being as reliable as preoperative templating regarding avoiding cup-oversizing in THA. Extreme caution is justified when the cup reamer is > 4 mm than the native head’s anteroposterior diameter.
Even though these methods are considered established and adequate, it is exceedingly salient to give prominence to the remaining space for refinement of the general guidelines concerning assisting surgeons in opting for the right decision when determining acetabular component size in primary THA. Moreover, inexperienced surgeons may pronouncedly find it helpful defining the acetabular shell’s size. Consequently, anybody involved in THA planning may reap the benefits from a simple tool aiding in predicting implant sizing in THA. The robust correlation we detected between the implanted acetabular shell’s size and the acetabular component’s size selected from the preparation of the acetabulum with our method, with a median difference of 2 mm, is of substantial clinical significance, as modern hip arthroplasty can benefit from the use of advanced technology by improving its accuracy and ensuring consistent and repeatable outcomes.
In our study, we demonstrated that the size of the first acetabular reamer not entering freely in the acetabular rim corroborates the final acetabular component size to implant. This was also corresponding in the majority of the cases with conventional preoperative templating. It can be featured as a valid tool for avoiding the potentially pernicious complications of acetabular cup over-reaming and over-sizing in primary THA. It is a simple and reproducible technical note useful for confirming the predicted acetabular cup size preoperatively; thus, its application could be considered routinely, even in cases where preoperative templating is unavailable.
Selecting the optimal size of components is crucial when performing a primary total hip arthroplasty. Implanting the accurate size of the acetabular component can occasionally be exacting, chiefly for surgeons with little experience, whilst the complications of imprecise acetabular sizing or over-reaming can be potentially devastating.
This paper aims to assist clinicians intraoperatively with a simple and repeatable tip in elucidating the ambivalence when determining the proper acetabular component size is not straightforwardly achieved, specifically when surgeons are inexperienced or preoperative templating is unavailable.
This paper aims to assist clinicians intraoperatively with a simple and repeatable tip in elucidating the ambivalence when determining the proper acetabular component size is not straightforwardly achieved, specifically when surgeons are inexperienced or preoperative templating is unavailable.
This method was employed in 263 operations in our department from June 2021 to December 2022. All operations were performed by the same team of joint reconstruction surgeons, employing a typical posterior hip approach technique. The types of acetabular shells implanted were: The Dynasty® acetabular cup system (MicroPort Orthopedics, Shanghai, China) and the R3® acetabular system (Smith & Nephew, Watford, United Kingdom), which both feature cementless press-fit design.
The mean value of all cases was calculated and collated with each other. We distinguished as oversized an implanted acetabular shell when its size was > 2 mm larger than the size of the acetabular size indicator reamer (ASIR) or when the implanted shell was larger than 4 mm compared to the preoperative planned cup. The median size of the implanted acetabular shell was 52 (48–54) mm, whereas the median size of the preoperatively planned cup was 50 (48–56) mm, and the median size of the ASIR was 52 (50–54) mm. The correlation coefficient between ASIR size and implanted acetabular component size exhibited a high positive correlation with r = 0.719 (P < 0.001). Contrariwise, intraoperative ASIR measurements precisely predicted the implanted cups’ size or differed by only one size (2 mm) in 245 cases.
In our study, we demonstrated that the size of the first acetabular reamer not entering freely in the acetabular rim corroborates the final acetabular component size to implant. This was also corresponding in the majority of the cases with conventional preoperative templating. It can be featured as a valid tool for avoiding the potentially pernicious complications of acetabular cup over-reaming and over-sizing in primary THA. It is a simple and reproducible technical note useful for confirming the predicted acetabular cup size preoperatively; thus, its application could be considered routinely, even in cases where preoperative templating is unavailable.
The robust correlation we detected between the implanted acetabular shell’s size and the acetabular component’s size selected from the preparation of the acetabulum with our method, with a median difference of 2 mm, is of substantial clinical significance, as it provides both the potential to enhance accuracy further and the ability to accomplish predictable and reproducible results in modern hip arthroplasty.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Greece
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Yang FC, China S-Editor: Liu JH L-Editor: A P-Editor: Zhang XD
| 1. | Ben Lulu O, Rubin G, Krasnyansky S, Elbaz A, Segal G, Rozen N. Measuring the Femoral Head Size--An Additional Real-Time Intraoperative Monitoring Tool for the Accuracy of the Preoperative Process and Implant Selection. J Arthroplasty. 2015;30:2201-2203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Muñoz-Mahamud E, Chimeno C, Tornero E, Alías A, Fernández-Valencia JÁ, Combalia A. Can the intra-operative measurement of the diameter of the femoral head help surgeons to choose the best size of the acetabular cup? Int Orthop. 2022;46:2793-2798. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Waldstein W, Bouché PA, Pottmann C, Faschingbauer M, Aldinger PR, Windhager R, Merle C. Quantitative and individualized assessment of the learning curve in preoperative planning of the acetabular cup size in primary total hip arthroplasty. Arch Orthop Trauma Surg. 2021;141:1601-1608. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Hinkle DE, Wiersma W, Jurs SG. Applied Statistics for the Behavioral Sciences. 5th ed. Houghton Mifflin Company, Boston, 2002: 756. [RCA] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 30] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Pfeufer D, Gililland J, Ajinkya R, Duensing I, Anderson MB, Peters CL, Pelt CE. Radiographic Native Femoral Head Size Correlates with Acetabular Cup Size in Primary Total Hip Arthroplasty. J Hip Surg. 2019;3:197-202. [DOI] [Full Text] |
| 6. | Krishnamoorthy VP, Perumal R, Daniel AJ, Poonnoose PM. Accuracy of templating the acetabular cup size in Total Hip Replacement using conventional acetate templates on digital radiographs. J Clin Orthop Trauma. 2015;6:215-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Kobayashi H, Cech A, Kase M, Pagenstart G, Carrillon Y, O'Loughlin PF, Bothorel H, Aït-Si-Selmi T, Bonnin MP. Pre-operative templating in THA. Part II: a CT-based strategy to correct architectural hip deformities. Arch Orthop Trauma Surg. 2020;140:551-562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 8. | Chen JB, Diane A, Lyman S, Chiu YF, Blevins JL, Westrich GH. Predicting Implant Size in Total Hip Arthroplasty. Arthroplast Today. 2022;15:210-214.e0. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 9. | Luca DiGiovanni P, Gasparutto X, Armand S, Hannouche D. The modern state of femoral, acetabular, and global offsets in total hip arthroplasty: a narrative review. EFORT Open Rev. 2023;8:117-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 18] [Reference Citation Analysis (0)] |
| 10. | Sharkey PF, Hozack WJ, Callaghan JJ, Kim YS, Berry DJ, Hanssen AD, LeWallen DG. Acetabular fracture associated with cementless acetabular component insertion: a report of 13 cases. J Arthroplasty. 1999;14:426-431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 88] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 11. | Knight JL, Atwater RD. Preoperative planning for total hip arthroplasty. Quantitating its utility and precision. J Arthroplasty. 1992;7 Suppl:403-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 118] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 12. | González Della Valle A, Comba F, Taveras N, Salvati EA. The utility and precision of analogue and digital preoperative planning for total hip arthroplasty. Int Orthop. 2008;32:289-294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 86] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 13. | Barrow JA, Divecha HM, Panchani S, Boden R, Porter ML; Board TN. Does oversizing an uncemented cup increase post-operative pain in primary total hip arthroplasty? Eur J Orthop Surg Traumatol. 2019;29:97-102. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 14. | Bricteux S, Beguin L, Fessy MH. [Iliopsoas impingement in 12 patients with a total hip arthroplasty]. Rev Chir Orthop Reparatrice Appar Mot. 2001;87:820-825. [PubMed] |
| 15. | Schoof B, Jakobs O, Schmidl S, Lausmann C, Fensky F, Beckmann J, Gehrke T, Gebauer M. Anterior iliopsoas impingement due to a malpositioned acetabular component - effective relief by surgical cup reorientation. Hip Int. 2017;27:128-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 16. | Hsu AR, Kim JD, Bhatia S, Levine BR. Effect of training level on accuracy of digital templating in primary total hip and knee arthroplasty. Orthopedics. 2012;35:e179-83. [RCA] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 38] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 17. | Shaarani SR, McHugh G, Collins DA. Accuracy of digital preoperative templating in 100 consecutive uncemented total hip arthroplasties: a single surgeon series. J Arthroplasty. 2013;28:331-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 66] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 18. | Suh KT, Cheon SJ, Kim DW. Comparison of preoperative templating with postoperative assessment in cementless total hip arthroplasty. Acta Orthop Scand. 2004;75:40-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 47] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 19. | Unnanuntana A, Wagner D, Goodman SB. The accuracy of preoperative templating in cementless total hip arthroplasty. J Arthroplasty. 2009;24:180-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 69] [Article Influence: 4.3] [Reference Citation Analysis (0)] |