Published online Mar 20, 2024. doi: 10.5662/wjm.v14.i1.88850
Peer-review started: October 13, 2023
First decision: December 7, 2023
Revised: December 20, 2023
Accepted: January 19, 2024
Article in press: January 19, 2024
Published online: March 20, 2024
Processing time: 145 Days and 16.8 Hours
The authors describe a technique for building an alternative jawbone phantom using dental gypsum and rice for research and dental radiology instruction.
To investigate the potential of an alternative phantom to simulate the trabecular bone aspect of the human maxilla in periapical radiographs.
Half-maxillary phantoms built from gypsum-ground rice were exposed to X-rays, and the resulting images (experimental group) were compared to standardized radiographic images produced from dry human maxillary bone (control group) (n = 7). The images were blindly assessed according to strict criteria by three exami
The differences in the trabecular aspects between groups were not statistically significant. In addition, interobserver agreement among observers was 0.43 and 0.51 for the control and experimental groups, respectively, whereas intraobserver agreement was 0.71 and 0.73, respectively.
The tested phantom seemed to demonstrate potential for trabecular bone image simulation on maxillary periapical radiographs.
Core Tip: The successful interpretation of radiographs is a complex process that relies on the clinician’s understanding of the radiographic image and ability to recognize the range of appearances of hard and soft tissues. To improve radiographic technique and image interpretation, the assimilation of normal appearances of hard tissues is fundamental in the research and teaching of dentomaxillofacial radiology. The authors describe a technique to build an alternative jawbone phantom using dental gypsum and rice for research and dental radiology instruction. The tested phantom seemed to have potential for trabecular bone image simulation on maxillary periapical radiographs.
- Citation: Munhoz EA, Xavier CRG, Salles RP, Capelozza ALA, Bodanezi AV. Convenient model of hard tissue simulation for dental radiographic research and instruction. World J Methodol 2024; 14(1): 88850
- URL: https://www.wjgnet.com/2222-0682/full/v14/i1/88850.htm
- DOI: https://dx.doi.org/10.5662/wjm.v14.i1.88850
Dental radiographs provide crucial and objective information that is unseen during clinical examination but that aids dentists in performing diagnosis, therapeutic planning, and treatment. Thus, an accurate analysis of a radiographic image depends on the quality of acquisition, a visual inspection, and an interpretation of the findings[1]. However, the successful interpretation of radiographs is a complex process relying on a combination of technical factors, anatomical and pathological knowledge, and clinician experience and expertise to understand the images and correlate them with perceived signs and symptoms[2]. By recognizing the difference between normal and varied radiographic tissue conditions, clinicians can identify changes caused by diseases that affect the teeth and jaws.
The process of learning, building, and improving radiographic diagnostic skills is a structured and rigorous undertaking that requires extensive human training. This should involve practicing radiologic technical skills, expanding scientific knowledge about diseases, and exposure to clinical environments[3].
Anthropomorphic devices, such as manufactured head phantoms, are proper alternatives commonly used to simulate the radiographic characteristics of maxillofacial tissues and to enable extensivelaboratory experimentation and practice. These simulators help to prevent unnecessary repetitions and patient X-ray overexposure in clinical settings[4], but they are also expensive, and the resulting bone trabeculae aspect is often insufficiently realistic. For this reason, cadaveric dried human skulls[5-11] or animal hard and soft tissue[12,13] are generally preferred for research and teaching, but they are extremely difficult to obtain. This is because ethical concerns involved in the fabrication and adjustment often needed for human or animal phantoms, such as cutting and grinding, demand considerable expertise and commonly produce irreversible changes that restrict their use in other applications[9-12].
Trabecular bone is highly visible, dominating images of the alveolar structure and adding complexity to human radiographic analysis[3,14]. Nevertheless, most in vitro studies on the reliability of the radiographic method are carried out only on uncovered extracted teeth[15-19], which may increase the differences related to clinical study results[3].
To date, no hard tissue simulation model can be manufactured in a simple and individualized way to mimic human bone for radiological training nor studies. As such, this study aimed to investigate the potential of an alternative phantom to simulate the trabecular appearance of the human maxilla in conventional periapical radiographs.
This study was approved by the local ethics committee, which is in compliance with the Declaration of Helsinki.
In total, 20 human teeth (13 to 18 and 23 to 28), extracted for therapeutic reasons and kept in 0.5% thymol solution, were scaled, polished with water/pumice, and dried with absorbent paper. After, the roots were covered with two layers of paraffin wax (Surgipath Medical Ind., Richmond, IL, United States) and heated to 56 °C in a water bath to simulate the periodontal ligament space on radiographs.
Right and left polyvinyl siloxane silicone negative molds (Elite Double 8, Zhermack, Badia Polesine, Italy) were obtained from the maxilla of a dental training manikin (Buyamag Inc., Carlsbad, CA, United States), which was previously split in half. The teeth were positioned upside down inside the right and left molds (n = 7), and the coronal part of each extracted tooth was inserted into its respective negative locus.
To make each gypsum-rice phantom piece, regular white rice was ground in a blender operating at medium speed (15000 revolutions per min) for 15 s, and the crushed grains were separated into four different fractions using 0.50-, 1.00-, and 2.00-mm mesh sieves. Smaller fragments were discarded, and the remaining larger fractions were mixed in equal-weight proportions. Thereafter, 40 g of a type V high-strength dental stone (Jade Stone, Whip Mix Co., Fort Collins, CO, United States) was mixed with water (0.19 L/P ratio) and homogenized in a bowl, together with 60 g of the processed hydrated rice. The resulting mixture was then poured into the silicone negative mold, and 24 h later, the set model was removed and kept in a controlled environment (25 °C and 75% relative humidity) until use. The filling process was repeated until seven phantoms were obtained.
The control group was composed of seven dry human skulls that were routinely used for educational training and radiographic research purposes, with at least four teeth in one of the maxillary sides (n = 7). No history or background on the skulls was available.
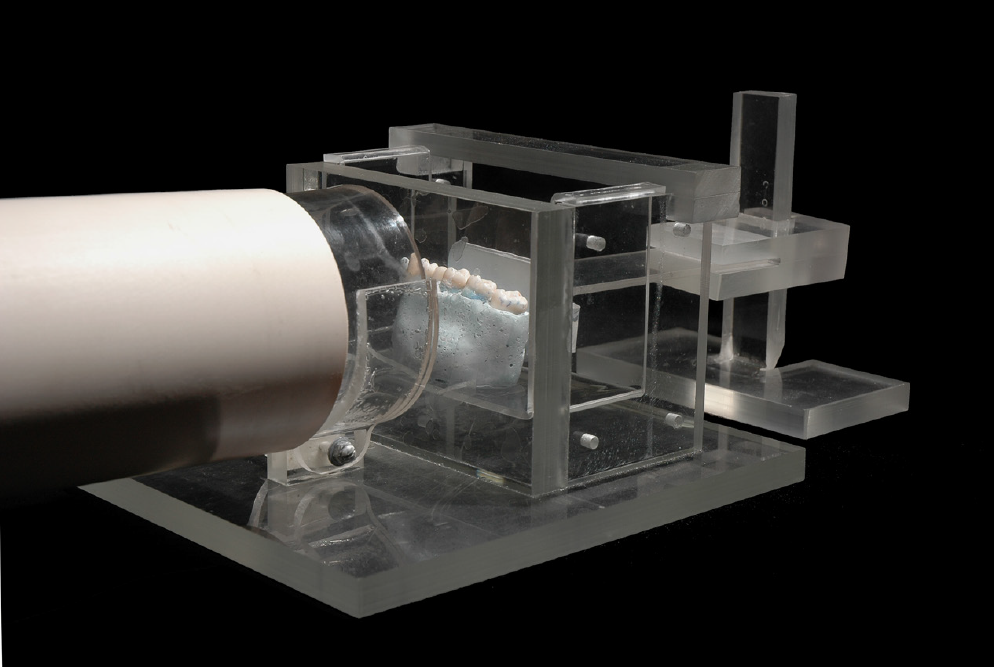
The experimental phantoms were fixed behind a 15-mm-thick vertical acrylic barrier intended to simulate the effect of soft tissues during X-ray exposure[11]. A periapical E film (Insight, Kodak Co., Rochester, NY, United States) was positioned behind each phantom using a specifically designed attaching device (Figure 1).
For the radiographic procedure involving the human skulls, a Rinn-XCP posterior horizontal holder (Dentsply Rinn, Elgin, IL, United States) was applied, and the film packet was placed in the palate next to the premolar and molar teeth. A cotton roll was positioned between the bite block and the occlusal surface of the teeth to keep the acrylic bite block away from the film exposure area. To simulate soft tissue, a 15-mm-thick vertical acrylic barrier was positioned at the front of the skulls[13].
Periapical radiographs of both the experimental and control groups were obtained in the buccolingual direction using the paralleling technique and a long spacer cone. The exposure time was 0.5 s, the focus-object distance was 50 cm, and the object-receptor distance was 2 cm. All radiographic images were obtained with a dental X-ray unit (X-707, Yoshida Dental MFC Co. Ltd, Tokyo, Japan) at 70 kVp and 8 mA.
The exposed films were immersed in developer solution for 3 min at 21 °C and rinsed with water for 10 s before being submerged in the fixer solution for 8 min. The developed films were subsequently washed with running water for 10 min and allowed to dry in a dust-free atmosphere.
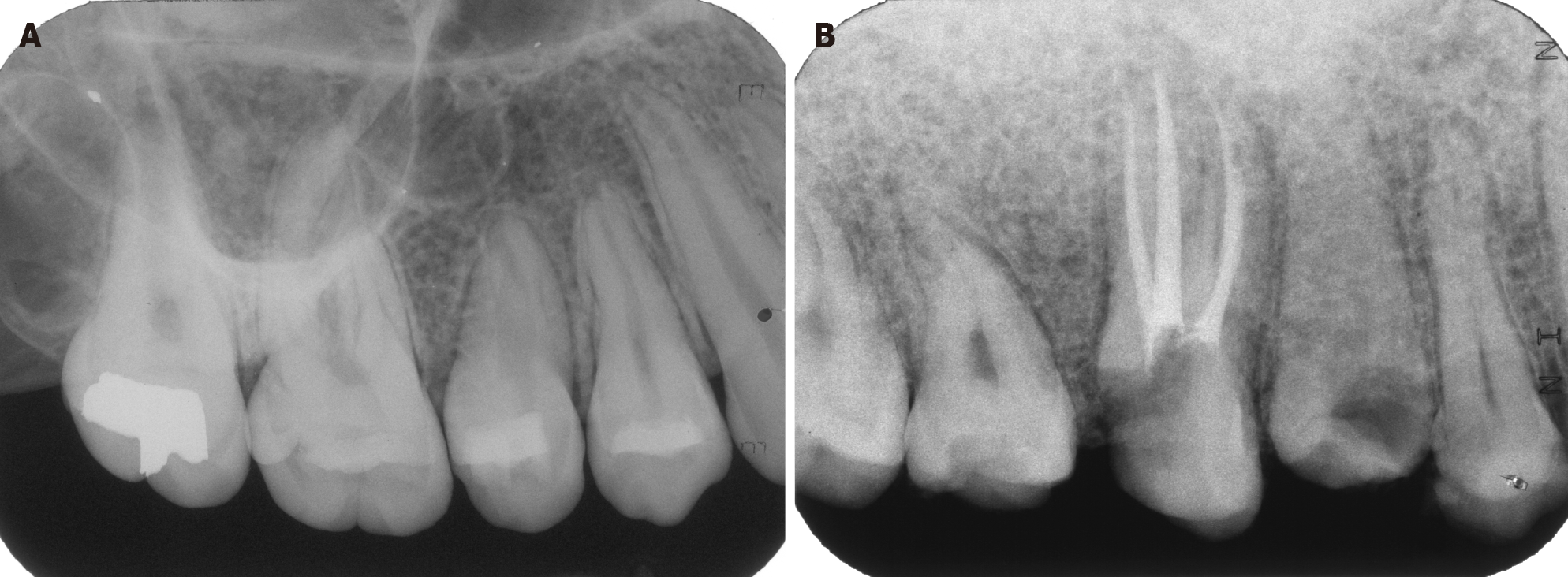
Three radiologists with at least five years of experience were asked to judge whether the images of bone trabeculae patterns in the 14 periapical radiographs, mounted in random order, resemble that experienced in daily clinical practice (Figure 2). Such features as intertrabecular distance, trabecular bone coarseness and striae, and mineral bone density were made available to the examiners as evaluation criteria. Then, before each evaluation, volunteers were instructed to disregard the presence of anatomical details, such as the maxillary sinus floor, the maxillary zygomatic process, and the lamina dura. Signs of previous dental interventions, such as root canal fillings, dental restorations, or absent teeth, were also ignored by the examiners.
All radiographic exams were performed with the aid of an ethyl-vinyl-acetate mask positioned over a fluorescent cold light box (Medalight LP-400, Hong Kong, China) in the same light-controlled room. Use of magnifying glasses was not allowed. The assessments were recorded in a proper form, and the viewing time was unlimited. A second evaluation was executed 4 wk after the first assessment. Then, the final assessment of each radiographic image was obtained from two or more similar assessments, as assigned by the examiners.
Differences between groups were compared using Fisher’s exact test, adjusted to the 5% significance level, whereas inter- and intraobserver agreements were determined by Cohen’s kappa statistic. Further, a statistical evaluation of all tests was performed using the SPSS database software (SPSS v. 18.0 for Windows, Chicago, IL, United States).
The number of images in the experimental group (3 of 7) from which examiners concluded that the maxillary trabecular pattern in the periapical radiograph resembled that experienced in daily clinical practice was not significantly different from that from the control group (6 of 7) (P = 0.559). In addition, the agreement between observers (interobserver reliability) was 0.43 (moderate) when experimental group images were analyzed and 0.51 (moderate) when control group radiographs were examined. Further, the stability of the responses from each examiner at different time points (intraobserver reliability) was 0.73 (substantial) for the experimental group images and 0.71 (substantial) for the control group radiographs, and the generated data are summarized in Table 1.
| Dry human maxillary bone | Rice maxillary phantom | |
| Trabecular pattern | ||
| Usual | 6 | 3 |
| Not usual | 1 | 4 |
| Total | 7 | 7 |
| Agreement test | ||
| Interobserver | 0.41 | 0.34 |
| Intraobserver | 0.73 | 0.71 |
Detailed knowledge of the appearances of normal radiographic bone and anatomical structures is mandatory for the identification of abnormal appearances, such as those due to infections or systemic diseases[6,14,20-23]. Thus, perceiving bone aspects in radiographs is complex because it requires the simultaneous assessment of diverse features, including the bone trabecular pattern, density, thickness, horizontal alignment, and space between trabeculae[2,10,11].
As well, the absence of significant differences between groups may have occurred because of the subjectivity involved in assessing each of these characteristics. Further, a wide variation in observer performance in the periapical radiological diagnoses has been widely recognized[24,25], and the previous experience of each observer may have influenced the interpretation of early periapical intraoral radiographs, as explained by Patel et al[22].
In this study, the interexaminer agreement for the bone aspect (0.43) was fair, even though the radiographs were viewed in the same light box and with the same radiographic mask, which are considered to improve interobserver agreement[22]. In addition, substantial variations in individuals’ interpretations of radiographic images were common
Moreover, the intentional lack of examiner calibration before the evaluations possibly contributed to this fair reliability. As such, prior clarification of the criteria by presenting human maxillary radiographic images to the examiners, including those from the control group, was expected to reduce the subjectivity of the analysis, as the control group’s radiograph evaluations would seem clearer to the examiners[27]. Another possible reason for the lack of significant differences between groups was likely due to the low number of intact human skulls available for comparison. Thus, most authors have adopted mandibular phantoms for their studies[10,11,13,14,28-31], as its flat anatomical nature facilitates the use of periapical films and positioning during radiographic imaging[2].
We presented an inanimate anthropomorphic phantom that was intended to simulate bone trabeculae in periapical radiographs of the maxilla. The superimposition of anatomical landmarks, such as the maxillary sinus floor and the maxillary zygomatic process, however, could not be reproduced in the radiographic images that were provided by this custom method. Thus, different results could be expected when applying this method to reproduce mandibular phantoms. In addition, in the maxilla, the trabeculae tend to be finer, more widely spaced, and homogenous, as observed in the experimental phantom, whereas in the mandible, the trabeculae tend to be relatively thick, closely packed, and often aligned horizontally[2].
In addition to simulating human anatomical structures, the tested phantoms are lightweight, easy to build, and low cost, and they have a reasonable size, features considered essential for a radiographic phantom[27]. In addition, the gypsum/rice mixture is poured into the mold, adapting to all root surfaces, including those of multi-rooted furcation teeth, thus eliminating alveoli cuts or grindings, as required for the use of dry human or animal mandible or maxilla[7,8,10-12]. In addition, the rice phantoms possess sufficient mechanical strength to withstand research or didactical handling, but due to the porous structure of the rice grains, the phantom can become fragile following careless repeated use.
According to the herein study results, it can be inferred that the narrow beam attenuation and scattering properties facilitated by the thickness of the tested gypsum-rice combination resemble those of human bone. These findings are thus non-definitive, as this is a preliminary report, and the composition of a larger sample whose radiographic appearance is analyzed by a system that produces quantifiable data may generate stronger evidence of the validity of gypsum-rice phantoms to mimic the radiographic appearance of human bone.
According to the preliminary results presented, the phantom constructed from dental gypsum and rice has the potential to simulate maxillary trabecular bone on laboratory periapical radiographs.
The process of learning, building, and improving radiographic diagnostic skills is a structured and rigorous undertaking that requires extensive human training. This should involve practicing radiologic technical skills, expanding scientific knowledge about diseases, and exposure to clinical environments.
Trabecular bone is highly visible, dominating images of the alveolar structure and adding complexity to human radiographic analysis. Nevertheless, most in vitro studies on the reliability of the radiographic method are carried out only on uncovered extracted teeth, which may increase the differences related to clinical study results. To date, no hard tissue simulation model can be manufactured in a simple and individualized way to mimic human bone for radiological training nor studies.
To investigate the potential of an alternative phantom to simulate the trabecular appearance of the human maxilla in conventional periapical radiographs.
Half-maxillary phantoms built from gypsum-ground rice were exposed to X-rays, and the resulting images (experimental group) were compared to standardized radiographic images produced from dry human maxillary bone (control group) (n = 7). The images were blindly assessed according to strict criteria by three examiners for the usual trabecular aspects of the surrounding bone, and significant differences between groups and in assessment reliability were compared using Fisher’s exact and kappa tests (α = 0.05).
The differences in the trabecular aspects between groups were not statistically significant. In addition, interobserver agreement among observers was 0.43 and 0.51 for the control and experimental groups, respectively, whereas intraobserver agreement was 0.71 and 0.73, respectively.
According to the preliminary results presented, the phantom constructed from dental gypsum and rice has the potential to simulate maxillary trabecular bone on laboratory periapical radiographs.
The perspectives are to improve the technique using rice as well as the creation of techniques using other accessible materials.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Dentistry, oral surgery and medicine
Country/Territory of origin: Brazil
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Mostafavinia A, Iran S-Editor: Chen YL L-Editor: A P-Editor: Yuan YY
| 1. | Krupinski EA. Current perspectives in medical image perception. Atten Percept Psychophys. 2010;72:1205-1217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 167] [Cited by in RCA: 171] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 2. | Whaites E, Drage N. Essentials of Dental Radiography and Radiology. 6ed. London: Elsevier, 2021. |
| 3. | Hegde S, Gao J, Vasa R, Cox S. Factors affecting interpretation of dental radiographs. Dentomaxillofac Radiol. 2023;52:20220279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Reference Citation Analysis (0)] |
| 4. | Hashimoto K, Arai Y, Iwai K, Araki M, Kawashima S, Terakado M. A comparison of a new limited cone beam computed tomography machine for dental use with a multidetector row helical CT machine. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95:371-377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 202] [Cited by in RCA: 188] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 5. | Barbat J. "In the eye of the beholder"--how radiographic image interpretation depends on who is looking and when. Aust Endod J. 1998;24:81-84. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 6. | Wallace JA, Nair MK, Colaco MF, Kapa SF. A comparative evaluation of the diagnostic efficacy of film and digital sensors for detection of simulated periapical lesions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92:93-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 32] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Hashimoto K, Kawashima S, Araki M, Iwai K, Sawada K, Akiyama Y. Comparison of image performance between cone-beam computed tomography for dental use and four-row multidetector helical CT. J Oral Sci. 2006;48:27-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 65] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 8. | Hashimoto K, Kawashima S, Kameoka S, Akiyama Y, Honjoya T, Ejima K, Sawada K. Comparison of image validity between cone beam computed tomography for dental use and multidetector row helical computed tomography. Dentomaxillofac Radiol. 2007;36:465-471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 69] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 9. | Mora MA, Mol A, Tyndall DA, Rivera EM. In vitro assessment of local computed tomography for the detection of longitudinal tooth fractures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:825-829. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 77] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 10. | Sîrbu VD, Perlea P, Nimigean VR, Bădiţă DG, Şerban A, Nimigean V. Morphological assessment of the mandibular canal trajectory in dentate subjects. Rom J Morphol Embryol. 2017;58:1401-1408. [PubMed] |
| 11. | Nimigean V, Sîrbu VD, Nimigean VR, Bădiţă DG, Poll A, Moraru SA, Păun DL. Morphological assessment of the mandibular canal trajectory in edentate subjects. Rom J Morphol Embryol. 2018;59:235-242. [PubMed] |
| 12. | Künzel A, Weimar S, Willers R, Becker J. Diagnostic of tooth fractures with the Vistascan system. Dent Traumatol. 2008;24:537-541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 13. | Caldas Mde P, Ramos-Perez FM, de Almeida SM, Haiter-Neto F. Comparative evaluation among different materials to replace soft tissue in oral radiology studies. J Appl Oral Sci. 2010;18:264-267. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 34] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 14. | Couture RA, Whiting BR, Hildebolt CF, Dixon DA. Visibility of trabecular structures in oral radiographs. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96:764-771. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Mileman PA, van den Hout WB. Comparing the accuracy of Dutch dentists and dental students in the radiographic diagnosis of dentinal caries. Dentomaxillofac Radiol. 2002;31:7-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 16. | Diniz MB, Rodrigues JA, Neuhaus KW, Cordeiro RC, Lussi A. Influence of examiner's clinical experience on the reproducibility and accuracy of radiographic examination in detecting occlusal caries. Clin Oral Investig. 2010;14:515-523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 17. | Lazarchik DA, Firestone AR, Heaven TJ, Filler SJ, Lussi A. Radiographic evaluation of occlusal caries: effect of training and experience. Caries Res. 1995;29:355-358. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Bussaneli DG, Boldieri T, Diniz MB, Rivera LM, Santos-Pinto L, Cordeiro Rde C. Influence of professional experience on detection and treatment decision of occlusal caries lesions in primary teeth. Int J Paediatr Dent. 2015;25:418-427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 19. | Vizzotto MB, Da Silveira PF, Liedke GS, Arus NA, Montagner F, Silveira HLD. Diagnostic reproducibility of the second mesiobuccal canal by CBCT: influence of potential factors. Oral Radiol. 2015;31:160-164. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 20. | White SC, Rudolph DJ. Alterations of the trabecular pattern of the jaws in patients with osteoporosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88:628-635. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 227] [Cited by in RCA: 318] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 21. | White SC, Cohen JM, Mourshed FA. Digital analysis of trabecular pattern in jaws of patients with sickle cell anemia. Dentomaxillofac Radiol. 2000;29:119-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 22. | Patel N, Rushton VE, Macfarlane TV, Horner K. The influence of viewing conditions on radiological diagnosis of periapical inflammation. Br Dent J. 2000;189:40-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 23. | Gaêta-Araujo H, Pinheiro MCR, Leite AF, Vasconcelos KF, Jacobs R, Oliveira-Santos C. Radiographic perception of anatomical structures and bony changes in oncologic patients under antiresorptive therapy. Support Care Cancer. 2023;31:149. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 24. | Goldman M, Pearson AH, Darzenta N. Reliability of radiographic interpretations. Oral Surg Oral Med Oral Pathol. 1974;38:287-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 163] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 25. | Kallio-Pulkkinen S, Haapea M, Liukkonen E, Huumonen S, Tervonen O, Nieminen MT. Comparison of consumer grade, tablet and 6MP-displays: observer performance in detection of anatomical and pathological structures in panoramic radiographs. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014;118:135-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 26. | Ulm C, Kneissel M, Schedle A, Solar P, Matejka M, Schneider B, Donath K. Characteristic features of trabecular bone in edentulous maxillae. Clin Oral Implants Res. 1999;10:459-467. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 74] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 27. | Guibelalde E, Vañó E. Design criteria for and evaluation of phantoms employed in conventional radiography. Rad Protect Dosimetry. 1993;49:39-46. [DOI] [Full Text] |
| 28. | Cavalcanti MG, Ruprecht A, Johnson WT, Southard TE, Jakobsen J. Radiologic interpretation of bone striae: an experimental study in vitro. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88:353-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 29. | Cavalcanti MG, Ruprecht A, Johnson WT, Southard TE, Jakobsen J. The contribution of trabecular bone to the visibility of the lamina dura: an in vitro radiographic study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93:118-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 30. | Colosi D, Potluri A, Islam S, Geha H, Lurie A. Brief communication: Bone trabeculae are visible on periapical images. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96:772-773. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 31. | Souza PH, da Costa NP, Veeck EB. Influence of soft tissues on mandibular gray scale levels. Braz Oral Res. 2004;18:40-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |