Published online Dec 20, 2023. doi: 10.5662/wjm.v13.i5.379
Peer-review started: September 25, 2023
First decision: November 14, 2023
Revised: November 18, 2023
Accepted: December 7, 2023
Article in press: December 7, 2023
Published online: December 20, 2023
Processing time: 85 Days and 18.4 Hours
When designing a study on dental movement acceleration or pain control during orthodontic treatment, it is crucial to consider effective parameters. The objective of this editorial is to compile the most effective parameters supported by evidence that should be considered in future studies to achieve complete parameter homogenization. The protocol currently recommended to homogenize the parameters and facilitate the development of further meta-analysis in terms of acceleration of movement and pain control in orthodontics is Wavelength: 810 nm, 2.2 J per surface, 0.1 W in continuous mode/0.1 W average power in a super-pulsed, sweeping movement, 1mm from the mucosa, 22 seconds along the vestibular surface and 22 seconds along the lingual surface, the recommended speed of movement is 2 mm/sec, 1 application during each orthodontic control, to achieve dental movement acceleration and repeat the dose at 24 h to ensure pain elimination. The energy density and power density will depend on the spot size used in the equipment and the distance from the mucosa. It will strengthen the evidence of photobiomodulation as the best therapy to accelerate tooth movement and at the same time control the pain produced by orthodontic treatments.
Core Tip: Several Systematic Reviews and Meta-Analyses have been published to evaluate the effectiveness of photobiomodulation (PBM) in accelerating dental movement and pain control during orthodontic treatment. These studies suggest that PBM is an effective method to achieve these objectives. However, all reports show a lack of standardization in the ideal parameters required.
- Citation: Dominguez A. Current protocol to achieve dental movement acceleration and pain control with Photo-biomodulation. World J Methodol 2023; 13(5): 379-383
- URL: https://www.wjgnet.com/2222-0682/full/v13/i5/379.htm
- DOI: https://dx.doi.org/10.5662/wjm.v13.i5.379
It is very common to find in randomized controlled clinical trials that evaluate the speed of tooth movement during orthodontic treatments or pain control, diverse protocols of photobiomodulation (PBM).
This means that at the time of developing a meta-analysis, or even a systematic review, the authors report that there needs to be a consensus in respect of guidance for clinical use, due to the lack of consistency of wavelengths and parameters applied.
The research question is no longer whether PBM controls pain and accelerates tooth movement when applied during orthodontic treatment. At the moment several systematic reviews and meta-analyses are in support of its efficacy[1-7].
The current question is how can we obtain the greatest effectiveness in PBM when we want to achieve those objectives.
To accomplish this goal, studies should focus on determining the necessary parameters such as wavelength, energy, power, application time, energy density, application points, and number of sessions.
This editorial aims to synthesize the parameters that are currently accepted to be effective in achieving these objectives during orthodontic treatment:
Pain control and dental movement acceleration.
Employing standardized parameters for accelerating movement and pain control will allow clinicians to be more effective in achieving these goals and will allow researchers to have adequate reproducibility in randomized controlled clinical trials that will later form part of systematic reviews and meta-analyses.
It is not enough to reproduce parameters such as energy, power, time, and energy density if we select a wavelength that is not the most effective to accelerate the movement.
Do we know what it is? The answer is: Yes.
In 2020, the first systematic review was conducted to establish an effective range of low-level laser therapy wavelengths for accelerating tooth movement in orthodontic treatment[8]. That review concluded that most randomized controlled trials related to accelerating tooth movement in orthodontic treatments are ideally between 780 and 830 nm wavelengths. The mean increase in speed of the dental movement calculated as a percentage of the control group was 24%.
Three years later, a systematic review and meta-analysis were performed with the same objective[9]. The authors concluded that ≤ 810 was determined as the wavelength associated with faster orthodontic tooth movement.
A range that fluctuates between 730 nm to 830 nm stimulates cell activity better[10,11]. It has been reported that wavelengths over 900 nm attract melanin and hemoglobin, resulting in a superficial energy uptake in soft tissue and insufficient energy in bone tissue. Shorter wavelengths have a greater ability to pass through soft tissue. Additionally, wavelengths within the range of 618 to 405 nm may not effectively stimulate orthodontic movement[12].
As for the effective wavelength to control pain during orthodontic treatments, the evidence has shown that pain reduction after 24 h is not significantly dependent on wavelength[13].
This indicates that if we are applying PBM to control pain and it disappears, we are not necessarily using the most effective wavelength to accelerate movement, as we considered in the years before these publications.
Until a few years ago, most studies were carried out to obtain the benefits of PBM in continuous mode. Most of the literature, before 2015, where we referred to Low-Level laser Therapy, provided studies with therapeutic equipment that emitted in continuous or pulsed mode. Currently, we have super-pulsed lasers available. However, the emission mode in laser-assisted orthodontics is not decisive. After selecting a device with the recommended wavelength, it can be continuous, pulsed, or super-pulsed. It is essential to take this into account when calculating the total energy delivered.
Several studies report 100 mW (0.1 W)[14-18], however, this varies greatly depending on the equipment used. Nowadays there is equipment that operates in pulsed or continuous mode, but its minimum power is 0.2 W, so it can be pulsed at 50% to obtain an adequate amount of total energy. We also have super-pulsed diodes in which it is advisable to select 0.2 W.
Since 2014 thanks to the first systematic review that evaluated these two objectives[19], we know that the most common and effective energy input is in the range of 0.2-2.2 J per point/2-8 J per tooth, to accelerate orthodontic tooth movement and control pain, the recommended energy per point ranged from 1-2 J when a single tooth was irradiated to 0.5-2.25 J per point when all teeth in the dental arch were irradiated.
Currently, 2-4 J per tooth is suggested to obtain both effects.
Energy density is the most important parameter in laser PBM, as it estimates the actual energy received by the target tissue. It is often referred to as fluence (J/cm2), meaning dose; however, some scholars also refer to energy in joules as dose[20].
The energy density is frequently mentioned in the dental literature, but the area of the spot in the tissue is often omitted. This error makes it impossible to verify their results or to see how they calculated the critical energy density information. Inconsistency in reporting these parameters is a major source of conflicting results in research and has contributed greatly to hindering acceptance of the effects of PBM[21].
The energy density is equal to the total energy if the tip or handpiece used in the equipment measures 1 cm 2, however, the dental equipment used for intraoral applications has round tips and in many cases, very small used without activation to allow the energy to reach the tissue and obtaining much higher energy densities, which are not always reported and make it difficult to standardize the parameters at the time of meta-analysis. This is why the ranges are extensive and energy density intervals range from 4.25 to 80 J/cm2; depending on the tip used to achieve movement acceleration and pain control.
Equipment tips are not interchangeable between manufacturers.
To adapt the protocol in the clinic, depending on the equipment that the practitioner has, he can adjust the energy density in 80 J/cm2 by applying the formula:
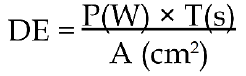
DE: Energy density;
T: Time in seconds;
A: Area in cm2 in cm2;
It is important to take into account that manufacturers report the diameter of the tip. To find the area in cm2, the following formula should be applied:
A = π × r2
Examples: For a 7 mm diameter tip the area is 0.38 cm2; For a 3 mm diameter tip the area is 0.07 cm2.
Ideally, spot size (The area that reaches the tissue) measurements would be preferred, but due to the complexity of clinical practice due to is an infrared laser, it is recommended to standardize applications based on tip area, which is the closest alternative.
Aside from energy density, a second important parameter in laser measurement is power density[22]. Few studies have reported on power density, thus it is not extensively covered in the literature: 20 mW/cm2[23] and 6.37 W/cm2[24].
The energy density is not adequately reported because the distance from the mucosa to which the laser is applied is not standardized and this parameter depends on this distance.
Currently, it is suggested at 1mm from the mucosa.
Future studies should report without exception the energy density to facilitate a later consensus on both energy density and power density (fluence and irradiance) when looking for either of the two therapeutic objectives during orthodontic treatment.
The average increase in speed movement calculated as a percentage of the control group found in 2020 was 24%. Many authors recommended punctual application and divided the root into thirds, for example, Limpanichkul et al[14] and Doshi-Mehta et al[16], and some up to 5 points per surface[25,26]. This type of application is highly recommended in research cases to calculate the energy density per point in a precise way. However, it is complicated to reproduce it in clinical practice and it is easier to make a scanning movement. The recommended speed of movement is 2 mm/sec[27]. During orthodontic treatment, this movement is performed along the buccal and lingual surface of each tooth which requires acceleration for 22 s to obtain 2.2 J per surface, at 100 mW (0.1 W)[28] obtaining an average 30% acceleration of the movement. These parameters are also used for pain control.
Studies differ greatly in the number of applications. There are reports of several acceleration appointments between orthodontic controls[29-31]. It is advisable to apply PBM in the orthodontic control appointment without additional sessions; repeated doses between control appointments do not increase the average acceleration.
The increase in the number of sessions does not exceed 30% acceleration of the movement which is the percentage by which the speed is increased if applied just in the controls. Therefore, it is not justifiable to increase the number of appointments between them.
To guarantee a pain-free orthodontic treatment, it is necessary to repeat the dose 24 hours after the orthodontic adjustment[32]. The suggested single monthly dose that allows acceleration of movement is insufficient to eliminate pain.
The protocol currently recommended to homogenize the parameters and facilitate the development of further meta-analysis in terms of acceleration of movement and pain control in orthodontics is Wavelength: 810 nm, 2.2 J per surface, 0.1 W in continuous mode/0.1 W average power in a super-pulsed, sweeping movement, 1mm from the mucosa, 22 seconds along the vestibular surface and 22 seconds along the lingual surface, the recommended speed of movement is 2 mm/sec, 1 application during each orthodontic control, to achieve dental movement acceleration and repeat the dose at 24 h to ensure pain elimination. The energy density and power density will depend on the spot size used in the equipment and the distance from the mucosa.
Thanks to Dr. Luciana Almeida-Lopes from whom I learned the physical principles of lasers and who recently helped me to clarify the inconsistencies in reporting energy density in dental applications.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Dentistry, oral surgery and medicine
Country/Territory of origin: Colombia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Cho SY, China; Qureshi W, India S-Editor: Liu JH L-Editor: A P-Editor: Yuan YY
| 1. | Ge MK, He WL, Chen J, Wen C, Yin X, Hu ZA, Liu ZP, Zou SJ. Efficacy of low-level laser therapy for accelerating tooth movement during orthodontic treatment: a systematic review and meta-analysis. Lasers Med Sci. 2015;30:1609-1618. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 80] [Article Influence: 7.3] [Reference Citation Analysis (21)] |
| 2. | AlShahrani I, Togoo RA, Hosmani J, Alhaizaey A. Photobiomodulation in acceleration of orthodontic tooth movement: A systematic review and meta analysis. Complement Ther Med. 2019;47:102220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 25] [Article Influence: 4.2] [Reference Citation Analysis (41)] |
| 3. | Long H, Zhou Y, Xue J, Liao L, Ye N, Jian F, Wang Y, Lai W. The effectiveness of low-level laser therapy in accelerating orthodontic tooth movement: a meta-analysis. Lasers Med Sci. 2015;30:1161-1170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 1.7] [Reference Citation Analysis (21)] |
| 4. | Yavagal CM, Matondkar SP, Yavagal PC. Efficacy of Laser Photobiomodulation in Accelerating Orthodontic Tooth Movement in Children: A Systematic Review with Meta-analysis. Int J Clin Pediatr Dent. 2021;14:S94-S100. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 12] [Article Influence: 4.0] [Reference Citation Analysis (42)] |
| 5. | Jedliński M, Romeo U, Del Vecchio A, Palaia G, Galluccio G. Comparison of the Effects of Photobiomodulation with Different Lasers on Orthodontic Movement and Reduction of the Treatment Time with Fixed Appliances in Novel Scientific Reports: A Systematic Review with Meta-Analysis. Photobiomodul Photomed Laser Surg. 2020;38:455-465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (16)] |
| 6. | Zhi C, Wang T, Guo Z, Liu D, Duan X, Yu X, Zhang C. The Optimal Energy Density of Photobiomodulation Therapy in Decreasing Orthodontic-Related Pain: A Systematic Review and Network Meta-Analysis. Photobiomodul Photomed Laser Surg. 2021;39:642-653. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (18)] |
| 7. | Zhi C, Guo Z, Wang T, Liu D, Duan X, Yu X, Zhang C. Viability of Photobiomodulaton Therapy in Decreasing Orthodontic-Related Pain: A Systematic Review and Meta-Analysis. Photobiomodul Photomed Laser Surg. 2021;39:504-517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (17)] |
| 8. | Domínguez Camacho A, Montoya Guzmán D, Velásquez Cujar SA. Effective Wavelength Range in Photobiomodulation for Tooth Movement Acceleration in Orthodontics: A Systematic Review. Photobiomodul Photomed Laser Surg. 2020;38:581-590. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (19)] |
| 9. | Grajales M, Ríos-Osorio N, Jimenez-Peña O, Mendez-Sanchez J, Sanchez-Fajardo K, García-Perdomo HA. Effectiveness of photobiomodulation with low-level lasers on the acceleration of orthodontic tooth movement: a systematic review and meta-analysis of split-mouth randomised clinical trials. Lasers Med Sci. 2023;38:200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 6.0] [Reference Citation Analysis (18)] |
| 10. | Ankri R, Lubart R, Taitelbaum H. Estimation of the optimal wavelengths for laser-induced wound healing. Lasers Surg Med. 2010;42:760-764. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 39] [Article Influence: 2.6] [Reference Citation Analysis (14)] |
| 11. | de Oliveira GJPL, Aroni MAT, Pinotti FE, Marcantonio E, Marcantonio RAC. Low-level laser therapy (LLLT) in sites grafted with osteoconductive bone substitutes improves osseointegration. Lasers Med Sci. 2020;35:1519-1529. |
| 12. | Baser Keklikci H, Yagci A, Yay AH, Goktepe O. Effects of 405-, 532-, 650-, and 940-nm wavelengths of low-level laser therapies on orthodontic tooth movement in rats. Prog Orthod. 2020;21:43. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 13. | Domínguez Camacho A, Bravo Reyes M, Velasquez Cujar SA. A systematic review of the effective laser wavelength range in delivering photobiomodulation for pain relief in active orthodontic treatment. Int Orthod. 2020;18:684-695. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 14. | Limpanichkul W, Godfrey K, Srisuk N, Rattanayatikul C. Effects of low-level laser therapy on the rate of orthodontic tooth movement. Orthod Craniofac Res. 2006;9:38-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 150] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 15. | Youssef M, Ashkar S, Hamade E, Gutknecht N, Lampert F, Mir M. The effect of low-level laser therapy during orthodontic movement: a preliminary study. Lasers Med Sci. 2008;23:27-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 170] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 16. | Doshi-Mehta G, Bhad-Patil WA. Efficacy of low-intensity laser therapy in reducing treatment time and orthodontic pain: a clinical investigation. Am J Orthod Dentofacial Orthop. 2012;141:289-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 176] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 17. | Camacho ÁD, Velasquez SA. Acceleration effect of orthodontic movement by application of low-intensity laser. J Oral Laser Appl. 2010;10:99-105. |
| 18. | Arumughan S, Somaiah S, Muddaiah S, Shetty B, Reddy G, Roopa S. A Comparison of the Rate of Retraction with Low-level Laser Therapy and Conventional Retraction Technique. Contemp Clin Dent. 2018;9:260-266. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 19. | Sousa MV, Pinzan A, Consolaro A, Henriques JF, de Freitas MR. Systematic literature review: influence of low-level laser on orthodontic movement and pain control in humans. Photomed Laser Surg. 2014;32:592-599. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 52] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 20. | Huang YY, Sharma SK, Carroll J, Hamblin MR. Biphasic dose response in low level light therapy - an update. Dose Response. 2011;9:602-618. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 524] [Cited by in RCA: 742] [Article Influence: 53.0] [Reference Citation Analysis (0)] |
| 21. | Zein R, Selting W, Hamblin MR. Review of light parameters and photobiomodulation efficacy: dive into complexity. J Biomed Opt. 2018;23:1-17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 201] [Cited by in RCA: 221] [Article Influence: 31.6] [Reference Citation Analysis (0)] |
| 22. | Star WM. Light dosimetry in vivo. Phys Med Biol. 1997;42:763-787. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 94] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 23. | Ekizer A, Türker G, Uysal T, Güray E, Taşdemir Z. Light emitting diode mediated photobiomodulation therapy improves orthodontic tooth movement and miniscrew stability: A randomized controlled clinical trial. Lasers Surg Med. 2016;48:936-943. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 45] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 24. | Domínguez A, Gómez C, Palma JC. Effects of low-level laser therapy on orthodontics: rate of tooth movement, pain, and release of RANKL and OPG in GCF. Lasers Med Sci. 2015;30:915-923. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 50] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 25. | Sousa MV, Scanavini MA, Sannomiya EK, Velasco LG, Angelieri F. Influence of low-level laser on the speed of orthodontic movement. Photomed Laser Surg. 2011;29:191-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 116] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 26. | Qamruddin I, Alam MK, Mahroof V, Fida M, Khamis MF, Husein A. Effects of low-level laser irradiation on the rate of orthodontic tooth movement and associated pain with self-ligating brackets. Am J Orthod Dentofacial Orthop. 2017;152:622-630. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 74] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 27. | Selting W. Laser Operating Parameters for Hard and Soft Tissue, Surgical and PBM Management. In: Coluzzi, D., Parker, S. (eds) Lasers in Dentistry—Current Concepts. Textbooks in Contemporary Dentistry. Springer, Cham 2017: 72. Available from: https://link.springer.com/chapter/10.1007/978-3-319-51944-9_4. |
| 28. | Dominguez A, Velasquez SA. Acceleration Effect of Orthodontic Movement by Application of Low-intensity Laser. J Oral Laser Appl. 2010;2:99-10. |
| 29. | Lalnunpuii H, Batra P, Sharma K, Srivastava A, Raghavan S. Comparison of rate of orthodontic tooth movement in adolescent patients undergoing treatment by first bicuspid extraction and en-mass retraction, associated with low level laser therapy in passive self-ligating and conventional brackets: A randomized controlled trial. Int Orthod. 2020;18:412-423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 30. | Zheng J, Yang K. Clinical research: low-level laser therapy in accelerating orthodontic tooth movement. BMC Oral Health. 2021;21:324. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 41] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 31. | Impellizzeri A, Horodynski M, Fusco R, Palaia G, Polimeni A, Romeo U, Barbato E, Galluccio G. Photobiomodulation Therapy on Orthodontic Movement: Analysis of Preliminary Studies with a New Protocol. Int J Environ Res Public Health. 2020;17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 32. | Domínguez A, Velásquez SA. Effect of low-level laser therapy on pain following activation of orthodontic final archwires: a randomized controlled clinical trial. Photomed Laser Surg. 2013;31:36-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 43] [Article Influence: 3.6] [Reference Citation Analysis (0)] |








