Published online Sep 20, 2023. doi: 10.5662/wjm.v13.i4.359
Peer-review started: March 29, 2023
First decision: June 12, 2023
Revised: July 2, 2023
Accepted: July 25, 2023
Article in press: July 25, 2023
Published online: September 20, 2023
Processing time: 175 Days and 6.8 Hours
The anteromedial meniscofemoral ligament (AMMFL) is a very rare entity, com
We report the case of a 34-year-old ballerina with an AMMFL associated with a torn medial meniscus of both knees. Surgery was performed to treat the meniscal injury and two biopsies of each AMMFL were taken in different locations to define the histopathological composition. Histologic examination revealed fibro
Clinical, magnetic resonance imaging, arthroscopic, and histological features have been carefully described to better characterize the AMMFL.
Core Tip: The anteromedial meniscofemoral ligament (AMMFL) is a very rare entity, commonly unrecognized and underreported. Concerns have been raised on the relation between the presence of this structure and medial meniscus injury. Regarding histologic examination, some studies showed meniscus-like fibrocartilage, while others have identified it as ligament-like collagenous fibrous connective tissue. We report the case of a 34-year-old ballerina with an AMMFL associated with a torn medial meniscus of both knees. Surgery was performed to treat the meniscal injury and two biopsies of each AMMFL were taken in different locations to define the histopathological composition. Clinical, magnetic resonance imaging, arthroscopic, and histological features are carefully described to better characterize the AMMFL.
- Citation: Luco JB, Di Memmo D, Gomez Sicre V, Nicolino TI, Costa-Paz M, Astoul J, Garcia-Mansilla I. Clinical, imaging, arthroscopic, and histologic features of bilateral anteromedial meniscofemoral ligament: A case report. World J Methodol 2023; 13(4): 359-365
- URL: https://www.wjgnet.com/2222-0682/full/v13/i4/359.htm
- DOI: https://dx.doi.org/10.5662/wjm.v13.i4.359
Given the interest on meniscal preservation and transplantation, the insertion zones of the meniscus have been widely investigated. Recent anatomical studies have demonstrated several common patterns of attachment of the anterior horn of the medial meniscus (AHMM)[1-4]. According to Berlet and Fowler[3], there are four distinct insertion patterns based on bony landmarks. In type I (59%), the meniscus is inserted in the flat area between the articular surfaces (intercondylar region), providing a very firm attachment. In type II (24%), the meniscus is inserted medially, closer to the articular surface, also providing a strong tibial fixation. Type III insertions (15%) are very anterior and offer little resistance to anterior movement of the meniscus. Finally, type IV (3%) has no solid bony attachment and only the coronary fibers restrain the displacement of the anterior horn of the meniscus. Ohkoshi et al[2] subdivided type IV pattern based on the structure to which the AHMM is anchored: Transverse ligament (49%), anterior cruciate ligament (ACL) (38%), coronary ligament (11%), and infrapatellar synovial fold (2%). At last, Cha et al[5] subdivided the ACL type into ACL and intercondylar notch (ICN) type. McCormack and McGrath[6] named this ligamentous structure the anteromedial meniscofemoral ligament (AMMFL).
Several studies, mostly case reports, have documented the AMMFL with a wide variation in prevalence (1.2%-15%)[7,8] and several characteristics of this structure are still not well understood. Although the AMMFL was not proved to be a cause of anterior knee pain, concerns have been raised on the relation between the presence of this structure and medial meniscus injury secondary to its abnormal motion[2,6]. Regarding histologic examination of the AMMFL, some studies showed meniscus-like fibrocartilage, while others have identified it as ligament-like collagenous fibrous connective tissue[8,9].
Our knowledge of the AMMFL is based on very limited data. The aim of our work was therefore to describe the clinical, magnetic resonance imaging (MRI), and arthroscopic findings, as well as the histological composition of the AMMFL, through the case of a bilateral AMMFL in a 34-year-old ballerina.
A 34-year-old ballerina presented to our clinic referring bilateral knee pain of 10 mo long. This pain impaired her performance and provoked symptoms during her daily activities.
A partial meniscectomy in the patient’s right knee was performed 8 years ago in another hospital.
The patient denied any other medical history.
There was no personal and family history.
The patient appeared to be in good physical condition, with a height of 1.68 meters and a body mass index of 23. Examination revealed pain and tenderness over the medial joint line of both knees. The McMurray and Appley tests were positive on the medial side. No restriction in range of motion or laxity was detected.
No laboratory examinations were performed.
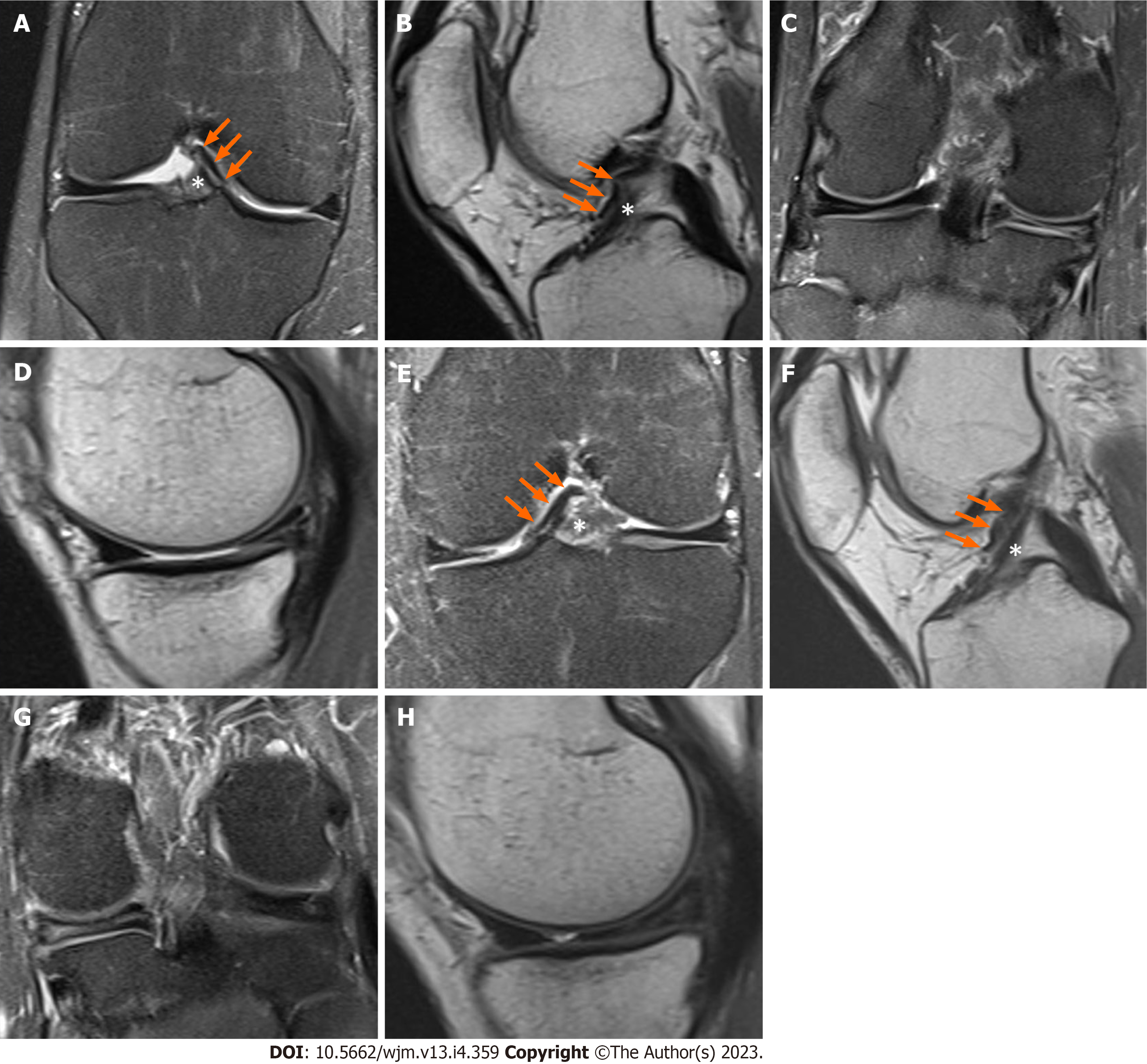
The MRI of both knees revealed a homogeneous low-signal linear structure on T1- and T2-weighted images, coursing anteriorly to the anterior aspect of the ACL and connecting the medial portion of the AHMM to the posterolateral ICN (Figure 1). This structure was best seen on sagittal view (Figures 1B and F). The MRI of the right knee also showed surgical traces of the previous partial medial meniscectomy together with a tear of the posterior horn of the medial meniscus (Figures 1C and D). The left knee showed a tear of the posterior horn of the medial meniscus (Figures 1G and H).
Plain knee and long-leg X-rays did not show bony abnormalities or coronal alignment deformity.
Bilateral AMMFL combined with a torn medial meniscus.
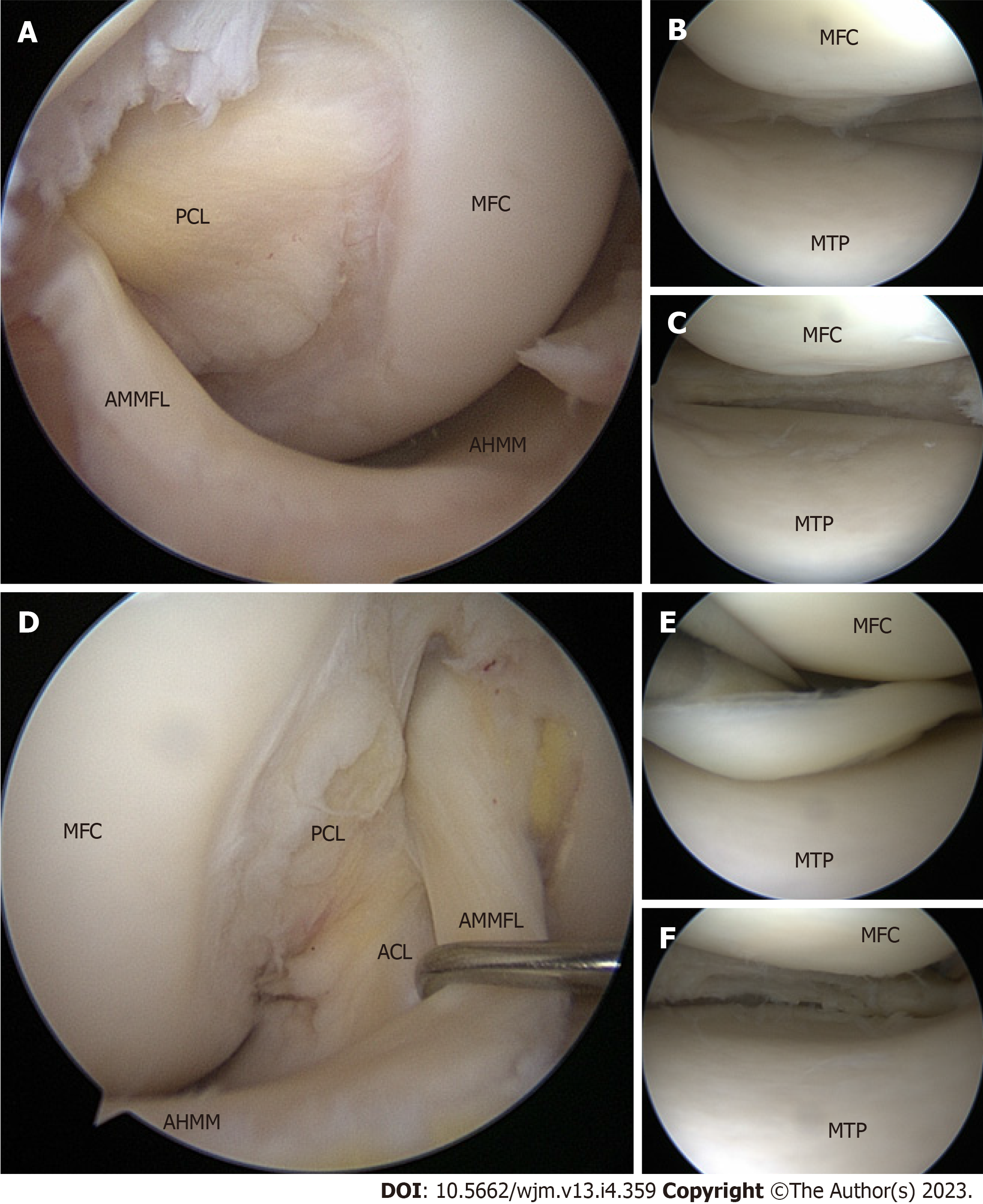
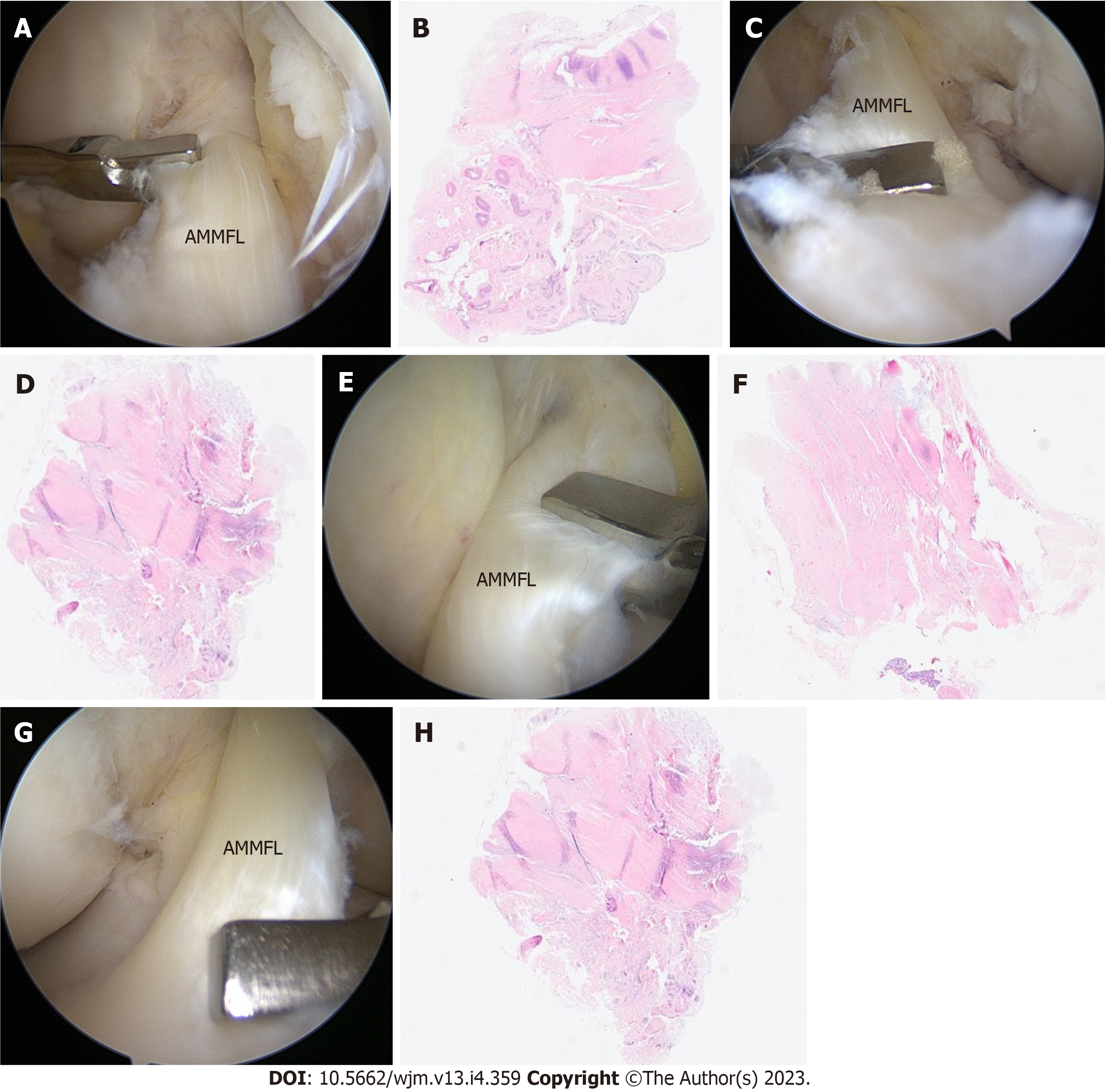
Diagnostic arthroscopy was performed together with a partial meniscectomy of both knees. Figure 2 shows the intraoperative findings of both knees. The AMMFL was visualized on both sides as an anomalous band-shaped structure covering the anterior portion of the ACL (Figures 2A and D). The band was originated at the AHMM and was attached to the posterolateral wall of the ICN. A fine band of synovial tissue engaged the AMMFL with the ACL. In both knees, the AHMM lacked a robust attachment to the tibia. Instead, it was connected to the tibia by meniscocapsular soft tissue. Therefore, the AHMM was noted to be abnormally mobile on palpation. No impingement of the AMMFL with the ICN was observed after mobilizing the knee through full range of motion. Therefore, we did not resect the AMMFL, preserving the structure. Two biopsies were taken from the AMMFL of each knee for histopathological examination, one proximal close to the ICN and one distal close to the AHMM (Figure 3). Histologic examination showed fibrocartilaginous tissue compatible with meniscus in all four biopsies (Figure 3). A complex tear of the body and posterior horn of the medial meniscus was corroborated arthroscopically, and a partial meniscectomy was performed in both knees (Figure 2).
The patient recovered favorably in the postoperative period. The use of crutches for 10 d and physiotherapy for 1 mo was indicated. After a period of strengthening, she returned to sports after 3 mo. Follow-up evaluation 1 year after surgery evidenced full remission of symptoms and the patient had resumed her athletic activities.
Variability of the AHMM patterns of insertion is relatively common according to cadaveric and arthroscopic studies[2,3,10]. However, abnormal insertion of the anterior horn into the ICN through the AMMFL is rare. The precise prevalence of this anatomical variation remains underestimated, as it may go undetected on preoperative MRI examination and is often only incidentally discovered during arthroscopy. One of the main issues in our knowledge of the AMMFL is a lack of high-level evidence studies. Our understanding on this topic is largely based on case reports[5,6,9,11-15] and there are only two case series available[7,8]. On the one hand, Kim and Joo[7] performed a retrospective review of 13 patients with an AMMFL with insertion at the ICN. In contrast to our report, all cases were diagnosed incidentally during arthroscopy. Although the AHMM had no bony attachment, they performed an MRI analysis and showed that there was no significant meniscal extrusion. On the other hand, Anderson et al[8] published a case series of 12 patients. Six patients were identified on a retrospective review of pictures taken during arthroscopies and the other six patients were identified prospectively. As in our case, all 12 patients had other abnormal conditions that were thought to be the cause of their symptoms.
Without prior awareness, the AMMFL may not be identified on preoperative MRI. Our review of the MRI findings revealed comparable features to those previously reported[1,5,16]. The AMMFL was identified as a linear structure of low signal intensity anterior to the ACL on sagittal and coronal views of T1- and T2-weighted images. Among the differential diagnoses, an ACL tear or an infrapatellar plica may be misdiagnosed on sagittal projections and a displaced bucket-handle tear on coronal views[16]. The anatomy of the distal insertion of the AMMFL, along with its morphology and position, can be used to differentiate it from these other structures.
It is still unclear whether the AMMFL may have biomechanical significance. It has been suggested that it functions as an anchor of the AHMM and probably plays an important role in load transmission[8]. This is in good agreement with the results of Kim and Joo[7], in which no significant extrusion of the medial meniscus was observed. However, the lack of normal bony attachment to the tibia causes the meniscus to be hypermobile, resulting in meniscal tears. According to Ohkoshi et al[2], during knee flexion, the AMMFL tightens and pulls the AHMM backwards, causing abnormal hoop tension on the entire medial meniscus and potentially inducing progressive degeneration or tears. This is consistent with our finding that the patient had a bilateral AMMFL associated with a torn medial meniscus. There was no impingement against the ICN, therefore, we did not resect the AMMFL and tried to preserve the structure.
Finally, there has been some disagreement regarding histopathological examination of this structure in different studies. Anderson et al[8] reported a ligamentous nature in one case, with dense fibrous tissue and collagen interspersed with parallel rows of fibroblasts. In contrast, Nakajima et al[9] described the histological features of a meniscal structure. Some authors argued that this difference could be related to the different biopsy sites. Therefore, we decided to take two biopsies in each AMMFL, one proximal and one distal to study the presence of possible transition zones and be able to define its histological nature. According to our findings, fibrocartilaginous tissue compatible with meniscus was found in all four biopsies.
The AMMFL is a very rare entity, commonly unrecognized and underreported. According to our case, as well as other previously published cases, the AMMFL shows several common features that can help reach an accurate diagnosis: (1) The AMMFL is observed as a low signal intensity band-like structure on MRI and is best seen on the sagittal view; (2) It is asymptomatic and often related to meniscal tears; (3) If discovered incidentally during arthroscopy, it should not be removed routinely; and (4) Its histopathological structure is predominantly meniscal tissue.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Argentina
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Chen Q, China; Nambi G, Saudi Arabia S-Editor: Wang JJ L-Editor: Wang TQ P-Editor: Wang JJ
| 1. | De Coninck T, Vanrietvelde F, Seynaeve P, Verdonk P, Verstraete K. MR imaging of the anatomy of the anterior horn of the medial meniscus. Acta Radiol. 2017;58:464-471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 2. | Ohkoshi Y, Takeuchi T, Inoue C, Hashimoto T, Shigenobu K, Yamane S. Arthroscopic studies of variants of the anterior horn of the medical meniscus. Arthroscopy. 1997;13:725-730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 41] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 3. | Berlet GC, Fowler PJ. The anterior horn of the medical meniscus. An anatomic study of its insertion. Am J Sports Med. 1998;26:540-543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 75] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 4. | Brown AA. The insertion of the anterior horn of the medial meniscus: an anatomic study. Muscles Ligaments Tendons J. 2013;3:210-212. [PubMed] |
| 5. | Cha JG, Min KD, Han JK, Hong HS, Park SJ, Park JS, Paik SH. Anomalous insertion of the medial meniscus into the anterior cruciate ligament: the MR appearance. Br J Radiol. 2008;81:20-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 24] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 6. | McCormack D, McGrath J. Antero-medial menisco-femoral ligament. Clin Anat. 1992;5:485-487. [RCA] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Kim YM, Joo YB. Anteromedial Meniscofemoral Ligament of the Anterior Horn of the Medial Meniscus: Clinical, Magnetic Resonance Imaging, and Arthroscopic Features. Arthroscopy. 2018;34:1590-1600. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 8. | Anderson AF, Awh MH, Anderson CN. The anterior meniscofemoral ligament of the medial meniscus: case series. Am J Sports Med. 2004;32:1035-1040. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Nakajima T, Nabeshima Y, Fujii H, Ozaki A, Muratsu H, Yoshiya S. Symptomatic anomalous insertion of the medial meniscus. Arthroscopy. 2005;21:629. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Kohn D, Moreno B. Meniscus insertion anatomy as a basis for meniscus replacement: a morphological cadaveric study. Arthroscopy. 1995;11:96-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 136] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 11. | Soejima T, Murakami H, Tanaka N, Nagata K. Anteromedial meniscofemoral ligament. Arthroscopy. 2003;19:90-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Hamada M, Miyama T, Nagayama Y, Shino K. Repair of a torn medial meniscus with an anteromedial meniscofemoral ligament in an anterior cruciate ligament-injured knee. Knee Surg Sports Traumatol Arthrosc. 2011;19:826-828. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Coulier B, Himmer O. Anteromedial meniscofemoral ligament of the knee: CT and MR features in 3 cases. JBR-BTR. 2008;91:240-244. [PubMed] |
| 14. | Shea KG, Westin C, West J. Anomalous insertion of the medial meniscus of the knee. A case report. J Bone Joint Surg Am. 1995;77:1894-1896. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 13] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 15. | Jung YB, Yum JK, Bae YJ, Song KS. Anomalous insertion of the medial menisci. Arthroscopy. 1998;14:505-507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 16. | Trinh JM, De Verbizier J, Lecocq Texeira S, Gillet R, Arab Abou W, Blum A, Teixeira P. Imaging appearance and prevalence of the anteromedial meniscofemoral ligament: A potential pitfall to anterior cruciate ligament analysis on MRI. Eur J Radiol. 2019;119:108645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |