Published online Jun 20, 2023. doi: 10.5662/wjm.v13.i3.98
Peer-review started: December 25, 2022
First decision: February 8, 2023
Revised: February 8, 2023
Accepted: March 15, 2023
Article in press: March 15, 2023
Published online: June 20, 2023
Processing time: 176 Days and 23.2 Hours
Female infertility with unknown causes (unexplained) remains one of the mysteries in the reproductive health field, where the diagnostic evidence is still weak and the proposed treatments still work with unknown methods. However, several studies have proposed some possible causes and risk factors for unexplained female infertility.
To characterize and identify factors associated with unexplained infertility in Sudanese women.
A matched (age and body mass index) case-control study was conducted from March 2021 to February 2022. The study samples were 210 women with unex
The results showed a higher proportion of women diagnosed with UI were residents of rural areas than controls (21.4% vs 11.1%, P < 0.05), and previous miscarriages and/or abortions were more common in fertile women compared with infertile women (13.16% vs 5.71%, P < 0.05). Additionally, infertile women had a significantly (P < 0.05) higher proportion of family history of infertility (explained and unexplained) compared with controls. Finally, after controlling for the effects of potentially confounding variables using multivariable logistic regression analysis, only marital status, family history of infertility, use of modern contraceptives, smoking, caffeine consumption, physical activity level, meals consumed, other vitamin-A-rich fruits and vegetables, and other vegetables were found to be significant (P < 0.05) factors associated with unexplained infertility among Sudanese women.
Married women with a family history of infertility who smoke and consume a high amount of caffeine, who live a sedentary lifestyle, and who consume more than two meals free of vitamin-A-rich fruits and/or vegetables and/or other vegetables per day are at the highest risk of developing unexplained infertility.
Core Tip: A matched (age and body mass index) case-control study was conducted to characterize and identify factors associated with unexplained infertility in Sudanese women. Four hundred women of reproductive age attending the maternity hospitals and fertility clinics in Khartoum, Sudan, were included in this study. The result showed that married women with a family history of infertility who smoke and consume a high amount of caffeine, who live a sedentary lifestyle, and who consume more than two meals free of vitamin-A-rich fruits and/or vegetables and/or other vegetables per day are at the highest risk of developing unexplained infertility.
- Citation: Abdullah AA, Ahmed M, Oladokun A. Characterization and risk factors for unexplained female infertility in Sudan: A case-control study. World J Methodol 2023; 13(3): 98-117
- URL: https://www.wjgnet.com/2222-0682/full/v13/i3/98.htm
- DOI: https://dx.doi.org/10.5662/wjm.v13.i3.98
Unexplained infertility (UI) refers to a diagnosis (or lack of diagnosis) made in infertile couples in whom all the standard approved infertility investigations, such as tests of ovulation, tubal patency, and semen analysis, are normal[1,2]. A "diagnosis of unexplained infertility" may be very frustrating for an infertile couple and is often interpreted as if there is no explanation for the cause of infertility, so there is no effective treatment"[3]. Importantly, the prognosis of UI is worse when the duration of infertility exceeds 3 years and the female partner is > 35 years of age[4].
Furthermore, the unexplained infertility estimates vary, and the likelihood that all such tests for an infertile couple are normal (i.e., that the couple has unexplained infertility) is approximately between 10% and 37% for all couples worldwide, and usually, female-related causes are responsible for 50% of it[4-9].
In Africa, the unexplained infertility prevalence is higher than that of other continents and ranges from 10%–37%[6,7]. In Sudan, a systematic review and meta-analysis found that the pooled prevalence of unexplained infertility in the Sudanese population is 17% with a confidence interval from 10% to 24%[6].
The high prevalence of unexplained infertility worldwide, especially in limited-resource countries like Sudan, implies that the current assessment of the human reproductive system is far from perfect. Nevertheless, significant improvements in diagnostic tools and assisted reproductive technologies have led to the finding of many causes of infertility that in the past had only been suspected, but, up until now, some causes of female infertility are still unknown. Subsequently, there is a need to search for more answers to the causes of female infertility to create better treatment options for patients.
Unexplained female infertility is considered one of the hot topics in reproductive medicine, and has been studied extensively; nevertheless, the studies in the area of diagnosis and treatment of unexplained female infertility didn't give concrete answers to the must-answer questions about the diagnosis and treatment of unexplained female infertility, whereby the diagnostic evidence is still weak and the proposed treatments still work with unknown methods. However, these studies have proposed some possible causes and risk factors for unexplained female infertility.
Studies conducted in low and low-middle-income countries showed that sociodemographic characteristics such as high body mass index (BMI), high waist-to-hip ratio (WHR), age older than 35 years, late marriage age, residence in rural and agricultural areas, low educational attainment, and unemployment were found to be significant risk factors for female infertility[8,10-16]. Furthermore, three systematic review and meta-analysis studies found a strong association between smoking and female infertility, whereby the pooled estimation showed that smoking women have a 1.8 times higher risk of developing infertility than women who do not smoke. Also, the same studies found a significant relationship between female infertility and alcohol consumption[10,17,18].
Additionally, other studies showed that high caffeine consumption was significantly associated with female infertility[12,19]. Meanwhile, several studies have found a negative significant association between increased physical activity level and unexplained female infertility[20], with sedentary women 3.61 times more likely to have unexplained infertility than moderately or very active women[19,21,22].
Furthermore, studies conducted in Iran and France found that women with a family history of infertility were 3.88 times more likely to develop unexplained infertility than women who did not have any close relatives who had experienced infertility previously[21,23]. This conclusion leads us to consider genetic factors as causes of unexplained infertility.
The previous history of abortion in women was one of the significant risk factors related to female infertility, whereby women with a previous history of abortion were more likely to have infertility in comparison to women without any previous history of abortion, with odds ratios of 9.33, 1.63, and 2.381, respectively, for Nigerian citizens[24], southeast Iranian citizens[23], and central Iranian citizens[25]. Some reports listed the use of contraceptives as a possible risk factor for female infertility[23,24]; in contrast, other reports found opposite results[13,26]. Therefore, there is still a need to find the association between the use of contraceptives and unexplained female infertility.
It is well known that nutritional status and the selection of food groups and supplements are crucial determinants of normal reproductive function. World Health Organization (WHO) and the Food and Agriculture Organization of the United Nations (FAO) described ten essential food groups for normal reproductive function in women of reproductive age[27,28]. Interestingly, in the available literature, there is no study about the effect of nutrition and diet diversity on unexplained female infertility, and the available evidence is only reported from cases of explained female infertility.
An 8-year prospective cohort study conducted by Chavarro et al[29], about the association between dietary diversity, eating habits, and the risk of female infertility, laid the basic foundation of what is now called a "fertility diet," which is a diet intended to increase the chances of women in the reproductive age of ovulation through changes in eating patterns and physical activity, whereby women with a high fertility diet score tend to have long menstrual cycles, normal reproductive hormone levels, and normal ovarian folliculogenesis. In addition, the findings of this study showed that the high fertility diet score was characterized by a lower intake of trans fat with a greater intake of monounsaturated fat; a lower intake of animal protein with a greater vegetable protein intake; a higher intake of high-fiber, low-glycemic carbohydrates; a greater preference for high-fat dairy products; a higher plant-based iron intake; and a higher frequency of multivitamin use[29]. Similarly, a nested case-control study in a Spanish cohort of 2154 female university graduates found that women with the highest adherence to the Mediterranean diet (characterized by high consumption of fruits and vegetables, fish, and poultry, low-fat products, and olive oil, which provides monounsaturated fat, and low consumption of red meat and sweets) are less likely to experience fertility difficulties[30].
Based on an extensive review of the existing literature about the risk factors of unexplained female infertility, the current study investigates sociodemographics, clinical history, dietary diversity, and consumption of different food groups as distinguishing factors associated with unexplained female infertility. More studies are needed to keep track of localized trends in infertility for better clinical management and research strategy as there is more variety and trends in unexplained infertility issues globally.
The present study highlights the characterization of unexplained infertility among Sudanese women and identifies factors associated with unexplained female infertility. The study outcome will contribute to the existing limited knowledge of unexplained female infertility and also have great significance for infertility program coordinators and policymakers as they design and implement effective strategies for preventing and managing female infertility.
The objectives of this study were achieved using a prospectively matched age and BMI case-control design. The study was carried out during the period from March 2021 to February 2022.
Prof. El-Sir Abo Elhassan Fertility Center, Omdurman Maternity Hospital, Nile Fertility Center, Khartoum Reproductive Health Care Center, Sudan Assisted Reproductive Clinic, University of Khartoum Fertility Center, Saad Abualila Teaching Hospital, Banoun Fertility Center, and Hawwa Center for Fertility were all used to collect study samples. Those centers were purposefully selected because they are the largest centers providing assisted conception and modern antenatal care in Sudan.
The current study targeted 420 Sudanese women between the ages of 18 and 44. The case group included 210 women with unexplained infertility; the women were chosen using a systematic random sampling technique from patients who had tried but were unable to conceive for at least a year (maintain regular unprotected vaginal sexual intercourse with their partner at least twice a week for a year); cases should also have regular menstruation, a normal ovarian reserve test result, open fallopian tubes, and a normal uterus cavity size according to the hysterosalpingography[1].
In addition, their couples should have a normal spermiogram "with a concentration of at least 15 million sperm per milliliter, a motility value over 70 percent, and morphology of more than 4 percent with normal forms"[31]; the control group consisted of 210 fertile, nonpregnant women who had at least one healthy 2-year-old child (end of lactation).
Women were excluded from this study if they had any of the following illnesses: Hypertension, diabetes, endocrine disorders, autoimmune or immunocompromised conditions, a history of genetic disease, or sexually transmitted infections. In addition to that, women were also excluded if they were under the effect of anti-inflammatory medicines or if they were under the effect of hormonal contraception within the last 6 mo. Finally, any women who refused to sign the informed consent form or withdrew during the study were excluded.
To assess unexplained female infertility risk factors, a structured pre-tested questionnaire containing information on socio-demographic variables, anthropometrics, clinical diagnosis of infertility, behavioral factors, physical activity assessment, dietary diversity, and consumption of different food groups by study participants was used.
The questionnaire was prepared by reviewing several relevant published articles[19,32-34] and adopting standardized data collection tools[22,27]. Primarily, the questionnaire was prepared in the English language and translated into the country's main local language (Arabic). The consistency of the questionnaire was checked in different phases: First, by translating it back to English and reviewing it with a non-affiliated researcher with good knowledge of both languages; after that, the final form of the questionnaire was tested for consistency using internal consistency (Cronbach's alpha of 0.73); and then it was pretested by distributing it among 30 women not participating in the actual study but living in a similar setting.
After passing all quality check-ups, the questionnaire was filled out with the help of 10 research assistants who are experts in reproductive health (one in each previously mentioned healthcare facility) and who were trained on questionnaire administration skills relevant to this study by the primary investigator and charged with seeking signed informed consent from the study participants. The completeness of the data was checked each day at the end of data collection. Incomplete data was traced back and edited accordingly. The follow-up of study participants was done by tracking information (address, phone number of the participant as well as of relatives and close friends) and making periodic contact (reminders, updates) to minimize loss of follow-up, and the overall follow-up and data collection processes were coordinated and supervised by the research assistants' and principal investigator's.
Unexplained infertility was defined as a type of infertility that occurs when standard-approved infertility tests have not found a clear cause for the couple’s inability to achieve pregnancy[35].
BMI is defined as an estimation of human body fat based on height and weight. BMI is expressed in kg/m2, resulting from dividing body mass in kilograms by height in meters[36,37].
The WHR was defined as an estimation of fat stored around the waist and hips. The waist-hip ratio was calculated by dividing the waist measurement by the hip measurement.
Caffeine consumption: Caffeine is a central nervous system stimulant. It is used as a cognitive enhancer, increasing alertness and attentional performance. In this study, caffeine consumption was only from liquid sources of stimulants. It is used as a cognitive enhancer, increasing alertness and attentional performance. In this study, caffeine consumption was only from liquid sources. It is used as a cognitive enhancer, increasing alertness and attentional performance. In this study, caffeine consumption was only from liquid sources (tea, coffee, sodas, and energy drinks) and was estimated based on the number of drunk cups in 24 h, whereby no consumption was considered if the woman didn't "drink any cups of caffeine," low consumption if the woman "drank a cup or two a day," moderate consumption if the woman "drunk 3 or 4 cups in 24 h," and high consumption if the woman "drunk more than 4 cups in 24 h”.
Physical activity level is a way to express a person's daily physical activity as a number and is used to estimate a person's total energy expenditure. The physical activity level was estimated using a list of the physical activities a woman performs within a 24-h period and the amount of time spent on each activity. The following shows physical activity levels for several lifestyles: (Inactive = hospital patient with limited physical mobility; sedentary = office worker getting little or no exercise; moderately active = moderate physical activity at work or leisure; very active = considerable physical activity at work, e.g., agricultural worker (non-mechanized) or office workers who take at least moderate exercise for two or more hours per day; and extremely active = professional athlete or sports person, e.g., football player)[38]. Dietary diversity is a qualitative measure of food consumption that reflects women's access to a variety of foods, including grains, nuts, dairy products, meat, eggs, fruits, and vegetables. Dietary diversity was determined based on a 7-d recall method. For each group, no consumption was considered "no servings per week," low consumption "1 or 2 servings per week," moderate consumption "3 servings per week," and high consumption "more than 3 servings per week." Servings per week were defined considering the consumption considered adequate in the African and Arabic diets[27,39].
Data collected from this study were sorted and recorded in Microsoft Excel 2016, cleaned, and then transferred to STATA software, version 16.0 (Stata Corp LLC, 77845 Texas, United States), and Jeffrey’s Amazing Statistics Program, version 0.16.4.0 (JASP), for analysis. To characterize the study population, descriptive statistics, frequencies, and percentages for categorical data and summary statistics (mean standard deviation (SD) with a 95% confidence interval (CI) for continuous data normally distributed and median and interquartile range for continuous data not normally distributed) were used. In addition, tables and figures were used for data presentation. The normal distribution of the study variables (univariate, pairwise, and multivariate[40]) was performed using the Shapiro-Wilk test, and the data were considered normally distributed if the p-value was greater than 0.05.
The association between the categorical variables in the study population was checked using the chi-square test at the statistically significant level of P = 0.05. Meanwhile, this association was estimated using Cramer’s V statistic effect size test, according to which it was classified, according to Kim[41], 2017, into small, medium, and large effect sizes.
A binary logistic regression analysis (bi-variable and multivariable) was carried out to identify the independent predictors of unexplained infertility. All independent variables with a P value of less than 0.05 in the bivariable logistic regression model were considered candidate variables for the multivariable model. Finally, the relationship was presented using a crude odds ratio and an adjusted odds ratio (AOR) with their corresponding 95% confidence intervals, and a P value of 0.05 or less was considered to be statistically significant.
The overall response rate in the current study was 210 (100%) among cases and 190 (90.5%) among controls.
Finally, the study included 400 women (210 women with UI as case subjects and 190 fertile women as control subjects). The two study groups were matched by age and BMI. The mean age of cases was 28.59 years with a SD of 5.22 years and a CI: of 27.87–29.3 years, while it was 28.44 years for controls (SD 4.95 years and a CI: of 27.73–29.15 years). The mean BMI values were 24.67 (SD 4.08 and CI: 24.11–25.22) and 24.41 (SD 4.38 and CI: 23.78–25.03) for the cases and controls, respectively. Besides, the two groups had almost the same mean value of the WHR [0.844 (SD 0.108 and CI: 0.829–0.859) for the cases and 0.837 (SD 0.114 and CI: 0.821–0.854) for the controls].
In addition to the above-mentioned anthropometry parameters, other sociodemographic characteristics of study participants, such as place of residence, marital status, education status, religious affiliation, and occupation, were checked. The only place of residence and marital status showed a statistically significant difference between the two study groups (Table 1). Wherein more women diagnosed with UI lived in rural areas than in urban areas (21.4% vs 11.1%, P < 0.05). Furthermore, when compared to controls, the vast majority of cases (99.1% vs 89.5%, P < 0.05) were married.
| Variable | Categories | Cases (n = 210), N% | Control (n = 190), N% | Effect size Cramer’s V | P value |
| Age group (yr) | 18-24 | 49 (23.3) | 40(21.05) | 0.083 | 0.61 |
| 25-29 | 87 (41.4) | 91(47.9) | |||
| 30-34 | 44 (21) | 35(18.4) | |||
| 35-39 | 23 (11) | 21(11.05) | |||
| 40-44 | 7 (3.3) | 3(1.6) | |||
| mean ± SD | 28.59 ± 5.22 | 28.44 ± 4.95 | NA | NA | |
| BMI (kg/m2) | Underweight | 1 (0.5) | 4 (2.1) | 0.073 | 0.53 |
| Normal weight | 127 (60.5) | 111 (58.4) | |||
| Overweight | 59 (28.1) | 54 (28.4) | |||
| Obesity | 23 (10.9) | 21 (11.1) | |||
| mean ± SD | 24.67 ± 4.08 | 24.41 ± 4.38 | NA | NA | |
| WHR | Less than 0.75 | 46 (22) | 54 (28.4) | 0.113 | 0.08 |
| 075-0.84 | 53 (25.2) | 35 (18.4) | |||
| 0.85-0.90 | 45 (21.4) | 41 (21.6) | |||
| Greater than 90 | 66 (31.4) | 60 (31.6) | |||
| mean ± SD | 0.844 ± 0.108 | 0.837 ± 0.114 | NA | NA | |
| Residence | Rural | 45 (21.4) | 21 (11.1) | 0.143 | 0.005 |
| Urban | 165 (78.6) | 169 (88.9) | |||
| Marital status | Married | 208 (99.1) | 170 (89.5) | 0.214 | 0.001 |
| Divorced1 | 2 (0.9) | 13 (6.8) | |||
| Widow | 0 (0) | 7 (3.7) | |||
| Education status | Diploma or above | 89 (42.4) | 85 (44.7) | 0.053 | 0.85 |
| Secondary edu | 72 (34.3) | 65 (34.2) | |||
| Primary edu | 39 (18.6) | 34 (17.9) | |||
| No formal edu2 | 10 (4.8) | 6 (3.2) | |||
| Religious affiliation | Muslim | 198 (94.3) | 184 (96.8) | 0.063 | 0.22 |
| Christian | 12 (5.7) | 6 (3.2) | |||
| Occupation | Farmer | 9 (4.3) | 2 (1.1) | 0.164 | 0.06 |
| Governmental | 34 (16.2) | 29 (15.3) | |||
| Housewife | 132 (62.9) | 110 (57.9) | |||
| Private business | 28 (13.3) | 34 (17.9) | |||
| NGOs | 1 (0.5) | 6 (3.2) | |||
| Student | 6 (2.9) | 9 (4.7) |
Meanwhile, the estimation of the effect sizes (Cramer’s V) indicated a small association between female unexplained infertility (age, BMI, WHR, residence, education status, and religious affiliation) and a medium association between female unexplained infertility and (marital status and occupation).
Table 2 shows the detailed history and clinical characteristics of the study participants. In this study, the median duration of unexplained infertility in cases was 3 years, with a range of 1–15 years and an interquartile range of 3.75, compared to the controls, who had a median of 4 for marriage duration, with a range of 3–20 years and an interquartile range of 2. These results were not compared since they were dissimilar.
| Variables | Categories | Cases (n = 210), N% | Controls (n = 190), N% | Effect size Cramer’s V | P value |
| Duration of infertility/marriage duration (yr) | Median = 3; Range = 1-15; IQR (3.75) | Median = 4; Range = 3-20; IQR (2) | NC | NC | |
| Previous miscarriage or abortion | Yes | 12 (5.71) | 25 (13.16) | 0.133 | 0.02 |
| No | 198 (94.29) | 165 (86.84) | |||
| Number of miscarriages or abortions | Never | 198 (94.29) | 165 (86.84) | 0.164 | 0.08 |
| 1 | 6 (2.86) | 13 (6.84) | |||
| 2 | 4 (1.9) | 6 (3.16) | |||
| 3 | 1 (0.48) | 4 (2.1) | |||
| 4 | 0 (0) | 2 (1.05) | |||
| 5 | 1 (0.48) | 0 (0) | |||
| Family history of infertility | Yes | 59 (28.1) | 12 (6.3) | 0.293 | 0.001 |
| No | 151 (71.9) | 178 (93.7) | |||
| Family history of Unexplained infertility | Yes | 29 (13.8) | 3 (1.6) | 0.233 | 0.001 |
| No | 181 (86.2) | 187 (98.4) | |||
| Use of modern contraceptives/yr | Never | 136 (64.8) | 119 (62.6) | 0.093 | 0.28 |
| 0-3 yr | 53 (25.2) | 60 (31.6) | |||
| 4-6 yr | 16 (7.6) | 9 (4.7) | |||
| More than 6 yr | 5 (2.4) | 2 (1.1) | |||
| Not in use now | 0 (0) | 0 (0) | |||
| Alcohol consumption | Yes | 0 (0) | 0 (0) | NE | NE |
| Not at all | 210 (100) | 190 (100) | |||
| Stopped taking | 0 (0) | 0 (0) | |||
| Smoking1 | Not at all | 181 (86.2) | 174 (91.6) | 0.093 | 0.54 |
| < 1 yr | 1 (0.48) | 1 (0.53) | |||
| 1-2 yr | 6 (2.9) | 3 (1.6) | |||
| 2-3 yr | 9 (4.3) | 5 (2.6) | |||
| > 4 | 13 (6.2) | 7 (3.7) | |||
| Caffeine consumption (cup/d)2 | No consume | 8 (3.8) | 6 (3.2) | 0.063 | 0.72 |
| Low consume | 68 (32.4) | 69 (36.3) | |||
| Moderate consume | 66 (31.4) | 51 (26.8) | |||
| High consume | 68 (32.4) | 64 (33.7) | |||
| Physical activity level | Very active | 43 (22.6) | 38 (18.1) | 0.083 | 0.26 |
| Moderately active | 51 (26.9) | 71 (33.8) | |||
| Sedentary | 96 (50.5) | 101 (48.1) |
Interestingly, fertile women had more previous miscarriages or abortions than infertile women (13.16% vs 5.71%, P < 0.05).
Furthermore, the current study found that infertile women had a higher proportion of infertility in their families than fertile women (28.1% vs 6.3%, P < 0.05). Similarly, the proportion of unexplained infertility in infertile women's families was higher than in controls (13.8% vs 1.6%, P < 0.05).
However, other clinical history variables did not show any significant association (P > 0.05) with unexplained female infertility and were reported as follows: The majority of study participants did not use contraceptives (64.8% for cases vs 62.6% for controls), none of the study participants have ever consumed alcohol, and the majority of them do not smoke (86.2% for cases and 91.6% for controls). Furthermore, the caffeine consumption patterns were almost the same in the two groups, whereby no consumption was 3.8% for cases vs 3.2% for controls, low consumption was 32.4% for cases vs 36.3% for controls, moderate consumption was 31.4% for cases vs 26.8% for controls, and high consumption was 32.4% for cases vs 33.7% for controls.
Moreover, the three (sedentary, moderately active, and very active) physical activity levels were at the same levels in the two groups, and the majority of the study participants had a sedentary lifestyle (50.5% for cases vs 48.1% for controls).
Finally, as can be seen in table 3, the estimation of the effect sizes (Cramer’s V) indicated a small association between female unexplained infertility and (previous miscarriage or abortion, family history of infertility, family history of unexplained infertility, use of contraceptives, smoking, caffeine consumption, and physical activity levels) and a medium association between female unexplained infertility and the number of miscarriages or abortions.
This study examined the consumption patterns of the essential ten food groups described by the WHO and FAO for women of reproductive age and the number of daily meals based on a 7-d recall method. The results found that there was no significant association (P > 0.05) between unexplained infertility and the consumption patterns for each of the ten essential food groups and the number of daily meals consumed by the study participants.
Additionally, the estimation of the effect sizes (Cramer’s V) of these associations was small for all studied variables.
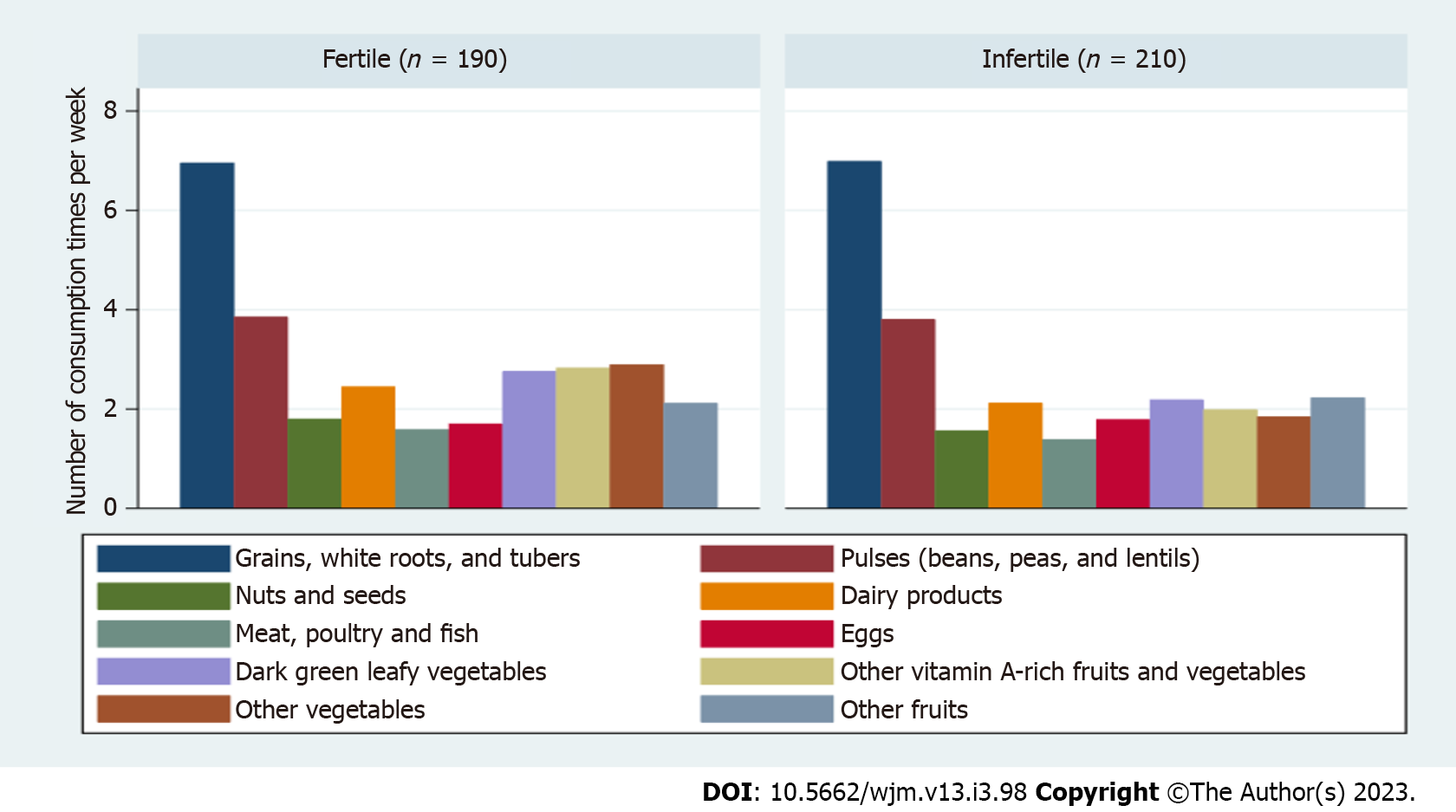
With an in-depth look at the general features of these findings, we can conclude that almost half of the Sudanese women used to consume 3 meals per day (42.4% for cases vs 45.3% for controls). Besides, regarding the consumption pattern of specific food groups, grains, and pulses were the most consumed food groups by study participants, whereas nuts, meat (including red meat, poultry, and fish), and eggs were the least consumed food groups by both study groups equally. The fully detailed consumption patterns of different food groups by the study participants are described in Table 3 and Figure 1.
| Variables | Categories | Cases (n = 210) | Controls (n = 190) | Effect size Cramer’s V | P value |
| Meals consumed per day | 2 | 50 (23.8) | 44 (23.2) | 0.041 | 0.97 |
| 3 | 89 (42.4) | 86 (45.3) | |||
| 4 | 42 (20) | 34 (17.9) | |||
| 5 | 24 (11.4) | 21 (11.1) | |||
| 6 | 5 (2.4) | 5 (2.6) | |||
| Grains, white roots, and tubers | No consume | 0 (0) | 0 (0) | NE | NE |
| Low consume | 0 (0) | 0 (0) | |||
| Moderate consume | 0 (0) | 0 (0) | |||
| High consume | 210 (100) | 190 (100) | |||
| Pulses (beans, peas, and lentils) | No consume | 7 (3.3) | 4 (2.1) | 0.091 | 0.36 |
| Low consume | 27 (12.9) | 36 (18.9) | |||
| Moderate consume | 51 (24.3) | 43 (22.6) | |||
| High consume | 125 (59.5) | 107 (56.3) | |||
| Nuts and seeds | No consume | 57 (27.1) | 69 (36.3) | 0.111 | 0.18 |
| Low consume | 88 (41.9) | 77 (40.5) | |||
| Moderate consume | 37 (17.6) | 25 (13.2) | |||
| High consume | 28 (13.3) | 19 (10) | |||
| Dairy products | No consume | 37 (17.6) | 38 (20) | 0.091 | 0.35 |
| Low consume | 89 (42.4) | 64 (33.7) | |||
| Moderate consume | 42 (20) | 42 (22.1) | |||
| High consume | 42 (20) | 46 (24.2) | |||
| Meat, poultry and fish | No consume | 74 (35.2) | 65 (34.2) | 0.091 | 0.32 |
| Low consume | 90 (42.9) | 69 (36.3) | |||
| Moderate consume | 37 (17.6) | 43 (22.6) | |||
| High consume | 9 (4.3) | 13 (6.8) | |||
| Eggs | No consume | 44 (20.9) | 49 (25.8) | 0.131 | 0.09 |
| Low consume | 90 (42.9) | 94 (49.8) | |||
| Moderate consume | 60 (28.6) | 36 (18.9) | |||
| High consume | 16 (7.6) | 11 (5.8) | |||
| Dark green leafy vegetables | No consume | 16 (7.6) | 13 (6.8) | 0.021 | 0.97 |
| Low consume | 101 (48.1) | 89 (46.8) | |||
| Moderate consume | 55 (26.2) | 53 (27.9) | |||
| High consume | 38 (18.1) | 35 (18.4) | |||
| Other vitamin A-rich fruits and vegetables | No consume | 25 (11.9) | 25 (13.2) | 0.081 | 0.47 |
| Low consume | 87 (41.4) | 75 (39.5) | |||
| Moderate consume | 63 (30) | 48 (25.3) | |||
| High consume | 35 (16.7) | 42 (22.1) | |||
| Other vegetables | No consume | 26 (12.4) | 33 (17.4) | 0.081 | 0.49 |
| Low consume | 83 (39.5) | 66 (34.7) | |||
| Moderate consume | 57 (27.1) | 49 (25.8) | |||
| High consume | 44 (20.9) | 42 (22.1) | |||
| Other fruits | No consume | 28 (13.3) | 30 (15.8) | 0.041 | 0.88 |
| Low consume | 94 (44.8) | 84 (44.2) | |||
| Moderate consume | 56 (26.7) | 46 (24.2) | |||
| High consume | 32 (15.2) | 30 (15.8) |
To identify the unexplained infertility predictor factors among Sudanese women, a binary logistic regression was used. The results found that from all the variables tested using the bi-variable binary logistic regression, only the place of residence, marital status, previous miscarriage or abortion, family history of infertility, family history of unexplained infertility, use of modern contraceptives, smoking, caffeine consumption, physical activity level, meals consumed, dairy, dark green leafy vegetables, other vitamin A-rich fruits and vegetables, and other vegetables were found to have significant associations with unexplained female infertility.
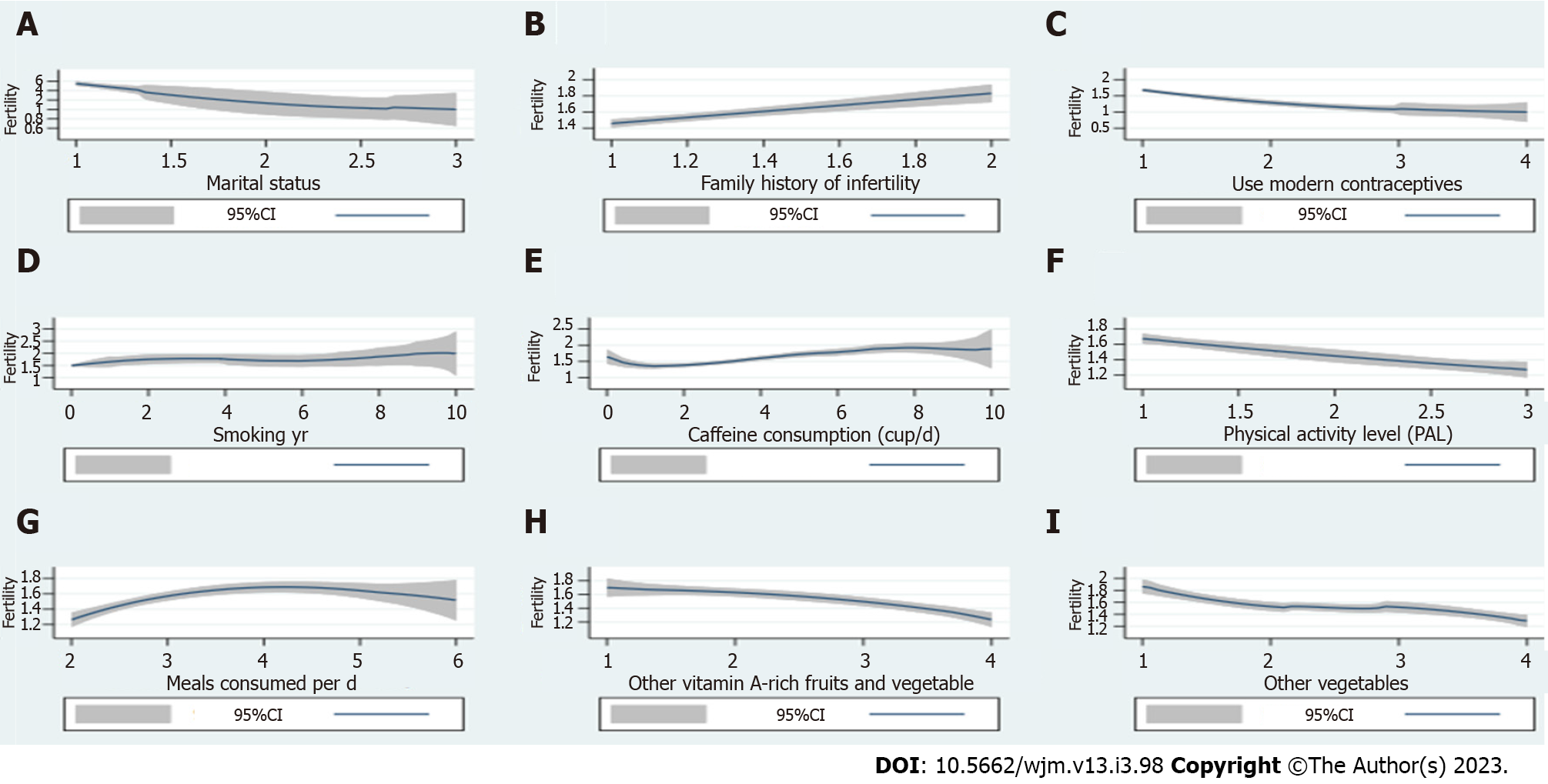
However, after controlling for the effects of potentially confounding variables using multivariable logistic regression analysis, only marital status, family history of infertility, use of modern contraceptives, smoking, caffeine consumption, physical activity level, meals consumed, other vitamin-A-rich fruits and vegetables, and other vegetables were found to be significant factors associated with unexplained infertility among Sudanese women. The variables eligible for the multivariable logistic regression model are described in Table 4 and Figure 2.
| Predictors | COR, 95%CI | AOR, 95%CI |
| Residence | ||
| Urban | Reference | Reference |
| Rural | 2.195 (0.225-1.347)a | 1.996 (-0.165-1.548) |
| Marital status | ||
| Married | Reference | Reference |
| Divorced | 0.126 (-3.576-0.571)a | 0.073 (-4.431-0.803)a |
| Widow | 0.419 (-0.922-0.386)a | |
| Previous miscarriage or abortion | ||
| No | Reference | Reference |
| Yes | 0.4 (-1.635 - 0.198)a | 0.426 (-1.874-0.165) |
| Family history of infertility | ||
| No | Reference | Reference |
| Yes | 5.796 (1.1 - 2.415)a | 3.257 (0.175-2.186)a |
| Family history of Unexplained infertility | ||
| No | Reference | Reference |
| Yes | 9.987 (1.095- 3.507)a | 3.580 (-0.594-3.145) |
| Use of modern contraceptives/yr | ||
| Never | Reference | Reference |
| 0-3 yr | 0.188 (-2.147-1.191)a | |
| 4-6 yr | 0.052 (-4.446-1.477)a | 0.475 (-0.987-0.502)a |
| More than 6 yr | 0.085 (-0.484-0.823) | |
| Smoking | ||
| Not at all | Reference | Reference |
| < 1 yr | 1.751 (-0.077-2.434)a | |
| 1-2 yr | 2.983 (-0.251-2.437)a | 1.276 (0.010-0.476)a |
| 2-3 yr | 4.102 (0.117-2.706)a | |
| > 4 | 3.356 (0.176-2.245)a | |
| Caffeine consumption (cup/d) | ||
| No consume | Reference | Reference |
| Low consume | 0.254 (-2.521-0.219)a | |
| Moderate consume | 0.648 (-1.586-0.718)a | 0.407 (0.168-0.514)a |
| High consume | 0.426 (-0.802-1.512)a | |
| Physical activity level (PAL) | ||
| Sedentary | Reference | Reference |
| Moderately active | 0.237 (-1.394- 0.464)a | 0.423 (-1.240-0.481)a |
| Very active | 0.292 (-2.291- 1.145)a | |
| Meals consumed per d | ||
| 2 | Reference | Reference |
| 3 | 4.172 (0.876-1.981)a | |
| 4 | 5.293 (1.006-2.326)a | 1.606 (0.169-0.778)a |
| 5 | 5.286 (0.899-2.432)a | |
| 6 | 2.917 (-0.253-2.394) | |
| Dairy | ||
| No consume | Reference | Reference |
| Low consume | 1.551 (-0.118-0.997)a | |
| Moderate consume | 0.974 (-0.649-0.596)a | 0.777 (-0.540-0.036) |
| High consume | 0.674 (-1.015-0.226)a | |
| Dark green leafy vegetables | ||
| No consume | Reference | Reference |
| Low consume | 1.014 (-0.780-0.807)a | |
| Moderate consume | 0.789 (-1.067-0.593)a | 0.730 (-0.651-0.021) |
| High consume | 0.346 (-1.948-0.176)a | |
| Other vitamin A-rich fruits and vegetables | ||
| No consume | Reference | Reference |
| Low consume | 0.673 (-1.078-0.287)a | |
| Moderate consume | 0.469 (-1.467-0.047)a | 0.540 (-0.948-0.283)a |
| High consume | 0.131 (-2.837-1.232)a | |
| Other vegetables | ||
| No consume | Reference | Reference |
| Low consume | 0.177 (-2.543-0.920)a | |
| Moderate consume | 0.169 (-2.614-0.940)a | 0.466 (-1.087-0.441)a |
| High consume | 0.064 (-3.623-1.866)a |
In the current study, married women were 0.073 times more likely to have unexplained female infertility in comparison to divorced and widowed women (AOR: 0.073, 95%CI: -4.431–0.803). Another vital factor significantly associated with unexplained female infertility was the family history of infertility, whereby any woman who has a history of infertility in her family was 3.257 times more likely to have unexplained female infertility compared with other women who don't have any family history of infertility (AOR 3.257, 95%CI: 0.175-2.186).
Meanwhile, the family history of unexplained infertility didn't show any significant associations with unexplained female infertility in the study participants. Women who did not use any contraceptives had significantly higher odds of developing unexplained female infertility compared with those who used them for any period of time (AOR 0.475, 95%CI: -0.987-0.502). In addition, smoking women had a significantly higher risk of developing unexplained female infertility than non-smoking women (AOR 1.276, 95%CI: 0.010–0.476).
This study also revealed that participants who had a sedentary lifestyle were more likely to have unexplained female infertility in comparison to participants with other lifestyles (AOR 0.423, 95%CI: 1.240–0.481). Furthermore, women who consumed more than two meals per day had a higher probability of developing unexplained infertility (AOR 1.606, 95%CI: -0.169-0.778). Additionally, women who didn't consume vitamin-A-rich fruits and vegetables and other vegetables had higher odds of having unexplained female infertility in comparison to those who consumed these two food groups in any amount. On the contrary, as caffeine consumption increases, the odds of having unexplained female infertility decrease (AOR 0.407, 95%CI: 0.168–0.514) (Table 4 and Figure 2).
The purpose of this thesis research was to identify factors associated with unexplained infertility in Sudanese women using the chi-square test to check the association and the logistic regression test to identify the unexplained infertility predictor factors. The results of the current study contribute to the limited knowledge of unexplained female infertility and have great significance for infertility program coordinators and policymakers as they design and implement effective strategies for preventing and managing female infertility. Also, the study data will be used as a baseline for other researchers who want to investigate further findings in this area.
The current study's finding reveals that, from all studied sociodemographic variables, only the place of residence and marital status showed a significant association with unexplained infertility in Sudanese women (Table 2). Specifically, infertility with unknown causes (unexplained) was significantly associated with married women and women residents in rural areas. This might be due to the fact that, in rural areas of Sudan, there are not enough healthcare facilities providing primary healthcare services and consulting in general and specifically for obstetrics and gynecology[42,43]. This can lead to neglecting the initial symptoms of infertility, which exacerbates the infertility conditions and makes it difficult to diagnose and treat them.
Furthermore, sociocultural practices such as believing infertility is a curse and that you should accept it and not seek help from anyone other than God are still prevalent in many rural communities in Sudan. In support of that, in a recent cross-sectional study of infertility management strategies among Sudanese participants, it was discovered that nearly one-half of the participants strongly believed that the best strategy for infertility management is to use Qur'an and Sunna treatments[44]. Such beliefs make it very difficult to diagnose and treat infertility cases in these communities.
All the above-mentioned factors can partially explain the high prevalence of unexplained female infertility among married women in rural areas of Sudan compared with other women in urban areas. This is in line with the findings of other female infertility studies conducted in Iran[13], Pakistan[16], Cameroon[15], the Central African Republic[15], and Chad[15]. These countries have economic settings and religion-oriented communities similar to Sudan; therefore, it is logical to draw similar conclusions.
In this study, 95.5% of the participants were Muslims, so the religious affiliation wasn't comparable, thereby showing no significant association with unexplained infertility in Sudanese women. Meanwhile, other sociodemographic variables, like occupation and education status, were comparable between the two groups; nevertheless, they didn't show any significant association with unexplained infertility in Sudanese women.
This result corroborates other findings reported in Nigeria[24], Iran[13], Pakistan[16], Cameroon[15], the Central African Republic[15], and Chad[15].
On the other hand, in contrast with the findings of the current study, a study conducted on women in Yazd, Iran[23], found a significant association between education status and female infertility, whereby the infertility risk increases with high educational attainment. Interestingly enough, this conclusion went against all the currently available literature.
The present study also investigated the clinical histories of the study participants (Table 3). Overall, the median duration of unexplained infertility among the case group was 3 years, ranging from 1 to 15 years. Furthermore, this study found a significant association between the family history of infertility (explained and unexplained) and unexplained infertility. This may indicate that there may be some genetic factors for unexplained female infertility, but due to the complexity of the reproduction process in females, this possible gene(s) is still unknown. Nevertheless, many studies found that most infertility causes and conditions, such as poor egg quality or low egg reserves and blocked or damaged fallopian tubes, can't be inherited and can happen to anyone, regardless of family history[45,46]. As a result, there is an urgent need for excessive research work to be done in the field of genetic infertility.
Although similar results to the findings of this study describing the association between family history of infertility and female infertility were reported in Iran[13,23,25], and Netherlands[47]. A case-control study conducted in Nigeria in 2020[24], with a smaller sample size, didn't find any significant association between female infertility and a family history of infertility.
It is important to note that, in the present study, the proportion of women with previous miscarriage and/or abortion was higher in fertile women compared with infertile women (13.16% vs 5.71%); however, the miscarriage proportion difference between the two groups is not significant.
This finding indicates that having a miscarriage and/or an abortion doesn’t affect a woman's ability to get pregnant in the future. A substantial number of studies reached similar conclusions[8,13,48,49]. Meanwhile, this result disagrees with the findings of studies from Nigeria[24], Iran[23], and Germany[50], which found a positive association between secondary infertility and abortion.
In this study, none of the study participants had ever consumed alcohol in any form or amount before. As a result, alcohol consumption among the study participants cannot be compared and is associated with unexplained infertility. The low prevalence of alcohol consumption in Sudanese women[51-53] could be responsible for the zero prevalence of alcohol consumption in our study cohort. These findings indicate that alcohol consumption cannot be considered a risk factor for unexplained female infertility in the Sudanese population.
Interestingly, despite the established significant association between female infertility and physical activity level in the previous studies, whereby an active lifestyle and moderate exercise reduce the risk of infertility (explained and unexplained) and abortions and increase the pregnancy success rates among women who undergo any of the assisted reproduction technologies[20,21,54,55], the current study did not find a significant association between unexplained female infertility and the physical activity level in Sudanese women.
This might be related mainly to the similarity of lifestyle choices and occupation affiliations mentioned before and the generally inactive lifestyle among females in Sudan[56].
The present study examined the consumption patterns of the ten essential food groups described by the WHO and FAO for women of reproductive age and the number of daily meals based on a 7-d recall method (Table 4). This study didn't find any significant association (P > 0.05) between unexplained infertility and the consumption patterns for each of the ten essential food groups among the study participants.
This indicates that despite the fact that female reproductive performance is definitely influenced by incorrect food consumption patterns, which lead to disturbances in nutritional status, alterations in ovarian function, and a subsequent decrease in fertility as shown in previous studies[29,30,57-60], however, in Sudanese women (fertile and infertile), in line with previous studies done in the Sudanese population[61-65], which found a similarity in food consumption patterns among women in Sudan, there was no difference in food consumption patterns between the two study groups.
This study used binary logistic regression to assess the unexplained infertility predictor factors among Sudanese women. According to the findings in Table 4 and Figure 2, only the place of residence, marital status, previous miscarriage or abortion, family history of infertility, family history of unexplained infertility, use of modern contraceptives, smoking, caffeine consumption, physical activity level, meals consumed, dairy, dark green leafy vegetables, other vitamin A-rich fruits, and vegetables. However, after controlling the effects of potentially confounding variables using multivariable logistic regression analysis, only marital status, family history of infertility, use of modern contraceptives, smoking, caffeine consumption, physical activity level, meals consumed, other vitamin-A-rich fruits and vegetables, and other vegetables were found to be significant factors associated with unexplained infertility among Sudanese women.
In the present study, married women were 0.073 times more likely to have unexplained infertility in comparison to divorced and widowed women. This can be explained by the fact that most Sudanese women seeking infertility services are married women (99.1%), so it makes sense that the odds of unexplained infertility are greater among them.
Also, women with a family history of infertility were 3.257 times more likely to have unexplained female infertility compared with other women who didn't have any family history of infertility. Similar findings were reported in studies from Iran and France, which found that women with a history of infertility in their family were 3.88 times more likely to develop unexplained infertility compared with women who didn't have any of their close relatives who had infertility before[21,23].
In light of this finding, it is essential to note that there is a strong argument that can be made about the effect of inherited "unknown genes" on female infertility. However, this argument needs more supporting evidence to make definitive conclusions.
Women who did not use any contraceptives (prior or current) had significantly higher odds of developing unexplained female infertility compared with those who used them for any period of time. Nevertheless, it can't be said with complete confidence that the use of contraceptives has contributed to the development of unexplained infertility cases in Sudanese women. Because contraceptives are used in women to prevent pregnancy from unprotected vaginal sex during fertile days, there is no need to use them in infertile women; thus, women who suffer from infertility usually do not use contraceptive methods[12,26]. This result corroborates all existing findings[13,17,23,25,35,66].
In this study, approximately 11% of Sudanese women of reproductive age smoke nicotine products, which is in line with the overall prevalence of smoking in the Sudanese population.
When compared to non-smokers, smoking women had 1.276 times the risk of developing unexplained female infertility.
This indicates that smoking has adverse effects on the normal female reproductive process, whereby the evidence specifically suggests that the smoking process produces some toxins that affect the folliculogenesis and steroidogenesis in the ovary and the FSH and LH secretion from the pituitary gland[67]. As a result, women are advised not to smoke to increase their fertility and their ability to get pregnant.
This result is consistent with a recent committee opinion report of the American Society for Reproductive Medicine[67], and other comprehensive studies about the negative effect of smoking on female fertility[14,18,68,69].
Women who had a sedentary lifestyle were more likely to have unexplained female infertility in comparison to participants with other lifestyles. This is consistent with recent findings that increasing physical activity level has a negative significant association with unexplained female infertility, with sedentary women 3.61 times more likely than moderately and very active women[21]. This finding may be explained by two main mechanisms. Sedentary physical activity in women may lead to an increase in leptin expression levels in the hypothalamus-pituitary-ovarian (HPO) axis, which has a negative effect on normal HPO axis function and may result in poor-quality eggs. Hence, an increase in physical activity leads to a decrease in leptin expression levels in the HPO axis and the resumption of ovulation by regulating HPO axis activity[70-73].
Additionally, high physical activity combined with the consumption of a healthy diet in women with infertility can decrease insulin and free androgen levels, leading to the restoration of the normal function of HPO by increasing the ovarian sensitivity to gonadotropins (LH and FSH) and resulting in recovery from infertility[20,74,75].
Women who consumed more than two meals per day had a 1.606 greater probability of developing unexplained infertility compared with other women who consumed three or more meals per day. In addition, women who didn't consume vitamin-A-rich fruits and vegetables and other vegetables had higher odds of having unexplained female infertility in comparison to those who consumed these food groups in any amount.
The current finding is corroborated by the findings of the American Society for Reproductive Medicine about the relationship between diet and female fertility[76].
The three food groups mentioned—vitamin A-rich fruits, vegetables, and other vegetables—are the main source of micronutrients (vitamin A, vitamin C, vitamin E, magnesium, zinc, phosphorus, and folic acid) in Sudanese women's diet; therefore, the lack of consumption of these food groups without compensation from an external source led to a deficiency in these micronutrients. Several studies have proven that vitamins A, C, and E, magnesium, zinc, phosphorus, and folic acid play an essential role in the normal female reproductive process; any deficiency in these substances leads to disturbances in the normal female reproductive process, resulting in infertility[60,76-79].
It is important to note that insufficient nutrient intake, in general, can contribute to female infertility. This may be due to the fact that unquestionably women of reproductive age are often nutritionally vulnerable because of the dynamic way in which their bodies work and the high physiological demands, especially during the menstrual cycle. Thus, they require a more nutrient-dense diet[28].
Finally, this study showed that as caffeine consumption increases, the odds of having unexplained female infertility decrease. Studies on the effect of caffeine consumption on female fertility are inconsistent, with several studies showing negative effects of caffeine on fertility, while other studies show no association or even a significant improvement in female fertility with caffeine consumption, as summarized in a systematic review done by Bu and his colleagues in 2020[80].
The findings of the current study can be explained in light of the fact that there may be some sort of unknown negative interaction between caffeine consumption (external causes) and the female reproductive system (internal causes), which increases the risk of infertility. Although this conclusion is not conclusive, we recommend that any woman who desires to have a baby consume caffeine wisely.
To recapitulate all the above, married women with a family history of infertility who smoke and consume a high amount of caffeine, who have a sedentary lifestyle, and who consume more than two meals free of vitamin-A-rich fruits and/or vegetables and/or other vegetables per day are at the highest risk of developing unexplained infertility. Therefore, any woman who intends to get pregnant and has one or more of these risk factors needs to get an immediate consultation from a certified fertility doctor to find out early if she has unexplained infertility or not and to know the best strategies to deal with it. Also, those women need to change their diet and lifestyle to decrease the likelihood of developing unexplained infertility.
This matched case-control study provided a useful characterization of unexplained female infertility in Sudan; this, along with the control of confounding factors and low loss to follow-up, contributes to the current study's strength.
Additionally, the study outcomes and arguments were based on relatively large sample size. Hence, its conclusion could be generalizable to other settings. We were constrained by the objectives of the significant study from which this study emanated. As such, some clinical details of the women with unexplained infertility were not captured. The data used for this study were obtained through patient-reported interviews, and some responses appear retrospective; thus, the participants’ responses could not be validated. However, efforts were made as much as possible to validate the information reported by participants through the patient records, especially for the participants who were not first-time visitors to the study recruitment clinics.
In conclusion, the median duration of unexplained infertility in this study was 3 years, with a range of 1–15 years. Furthermore, married women with a family history of infertility who smoke and consume a high amount of caffeine, who have a sedentary lifestyle, and who consume more than two meals free of vitamin-A-rich fruits and/or vegetables and/or other vegetables per day are at the highest risk of developing unexplained infertility.
Unexplained infertility remains one of the mysteries in the reproductive health field, where the diagnostic evidence is still weak and the proposed treatments still work with unknown methods.
Unexplained infertility remains one of the mysteries in the reproductive health field, where the diagnostic evidence is still weak and the proposed treatments still work with unknown methods.
The objective of this study was to characterize and identify factors associated with unexplained infertility in Sudanese women.
A matched (age and body mass index) case-control study was conducted from March 2021 to February 2022. The study samples were 210 women with unexplained infertility and 190 fertile women of reproductive age who were attending the maternity hospitals and fertility clinics in Khartoum, Sudan. The risk factors for unexplained infertility were identified using a structured, pre-tested questionnaire.
Infertile women had a significantly higher proportion of family history of infertility (explained and unexplained) compared with controls. Also, only marital status, family history of infertility, use of modern contraceptives, smoking, caffeine consumption, physical activity level, meals consumed, other vitamin-A-rich fruits and vegetables, and other vegetables were found to be significant (P < 0.05) factors associated with unexplained infertility among Sudanese women.
Married women with a family history of infertility who smoke and consume a high amount of caffeine, who live a sedentary lifestyle, and who consume more than two meals free of vitamin-A-rich fruits and/or vegetables and/or other vegetables per day are at the highest risk of developing unexplained infertility.
More interventional studies regarding the main factors, such as physical activity and dietary intake, for infertile women with unexplained causes, need to be done.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Obstetrics and gynecology
Country/Territory of origin: Sudan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Udo IA, Nigeria; Xu Y, China S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Practice Committee of the American Society for Reproductive Medicine. Practice Committee of the American Society for Reproductive Medicine. Fertility evaluation of infertile women: a committee opinion. Fertil Steril. 2021;116:1255-1265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 96] [Article Influence: 24.0] [Reference Citation Analysis (0)] |
| 2. | Wang R, Danhof NA, Tjon-Kon-Fat RI, Eijkemans MJ, Bossuyt PM, Mochtar MH, van der Veen F, Bhattacharya S, Mol BWJ, van Wely M. Interventions for unexplained infertility: a systematic review and network meta-analysis. Cochrane Database Syst Rev. 2019;9:CD012692. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 29] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 3. | Kiani Z, Simbar M, Hajian S, Zayeri F. The prevalence of depression symptoms among infertile women: a systematic review and meta-analysis. Fertil Res Pract. 2021;7:6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 73] [Cited by in RCA: 61] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 4. | Ray A, Shah A, Gudi A, Homburg R. Unexplained infertility: an update and review of practice. Reprod Biomed Online. 2012;24:591-602. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 113] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 5. | World Health Organization. Infertility. Geneva, Switzerland: World Health Organization; 2020 [updated 14 September 2020 cited 2022 24 November]. Available from: https://www.who.int/news-room/fact-sheets/detail/infertility. |
| 6. | Abdullah AA, Ahmed M, Oladokun A. Prevalence of infertility in Sudan: A systematic review and meta-analysis. Qatar Med J. 2021;2021:47. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (3)] |
| 7. | Abebe MS, Afework M, Abaynew Y. Primary and secondary infertility in Africa: systematic review with meta-analysis. Fertil Res Pract. 2020;6:20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 58] [Article Influence: 11.6] [Reference Citation Analysis (1)] |
| 8. | Sun H, Gong TT, Jiang YT, Zhang S, Zhao YH, Wu QJ. Global, regional, and national prevalence and disability-adjusted life-years for infertility in 195 countries and territories, 1990-2017: results from a global burden of disease study, 2017. Aging (Albany NY). 2019;11:10952-10991. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 235] [Cited by in RCA: 355] [Article Influence: 59.2] [Reference Citation Analysis (0)] |
| 9. | Eldib A, and Tashani O. Infertility in the Middle East and North Africa Region: A systematic review with meta-Analysis of prevalence surveys. Libyan J Med Sci. 2018;2:37-44. [DOI] [Full Text] |
| 10. | Nik Hazlina NH, Norhayati MN, Shaiful Bahari I, Nik Muhammad Arif NA. Worldwide prevalence, risk factors and psychological impact of infertility among women: a systematic review and meta-analysis. BMJ Open. 2022;12:e057132. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 81] [Article Influence: 27.0] [Reference Citation Analysis (0)] |
| 11. | Seth B, Arora S, Singh R. Association of obesity with hormonal imbalance in infertility: a cross-sectional study in north Indian women. Indian J Clin Biochem. 2013;28:342-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | Olooto WE, Amballi AA, and Banjo TA. A review of Female Infertility; important etiological factors and management. J Microbiol Biotechnol Res 2012; 2: 379-385. Available from: https://www.researchgate.net/publication/273322572_A_review_of_Female_Infertility_important_etiological_factors_and_management. |
| 13. | Moridi A, Roozbeh N, Yaghoobi H, Soltani S, Dashti S, Shahrahmani N, and Banaei M. Etiology and Risk Factors Associated With Infertility. IJWHR. 2019;7:346-353. [RCA] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 14. | Greenlee AR, Arbuckle TE, Chyou PH. Risk factors for female infertility in an agricultural region. Epidemiology. 2003;14:429-436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 73] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 15. | Larsen U. Infertility in central Africa. Trop Med Int Health. 2003;8:354-367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 17] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Hakim A. Factors affecting fertility in Pakistan. Pak Dev Rev. 1994;33:685-706. [PubMed] [DOI] [Full Text] |
| 17. | Deyhoul N, Mohamaddoost T, and Hosseini M. Infertility-Related Risk Factors: A Systematic Review. IJWHR. 2017;5:24-29. [RCA] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 18. | Augood C, Duckitt K, Templeton AA. Smoking and female infertility: a systematic review and meta-analysis. Hum Reprod. 1998;13:1532-1539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 290] [Cited by in RCA: 262] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 19. | Rossi BV, Abusief M, Missmer SA. Modifiable Risk Factors and Infertility: What are the Connections? Am J Lifestyle Med. 2014;10:220-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 51] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 20. | Xie F, You Y, Guan C, Gu Y, Yao F, Xu J. Association between physical activity and infertility: a comprehensive systematic review and meta-analysis. J Transl Med. 2022;20:237. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 26] [Reference Citation Analysis (0)] |
| 21. | Foucaut AM, Faure C, Julia C, Czernichow S, Levy R, Dupont C; ALIFERT collaborative group. Sedentary behavior, physical inactivity and body composition in relation to idiopathic infertility among men and women. PLoS One. 2019;14:e0210770. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 48] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 22. | World Health Organization. WHO guidelines on physical activity and sedentary behaviour: web annex: evidence profiles. Geneva, Switzerland patent 9240015116. 2020. |
| 23. | Mirzaei M, Namiranian N, Dehghani Firouzabadi R, Gholami S. The prevalence of infertility in 20-49 years women in Yazd, 2014-2015: A cross-sectional study. Int J Reprod Biomed. 2018;16:683-688. [PubMed] |
| 24. | Okafor IA, Saanu OO, Olayemi O, and Omigbodun AO. Characterization of primary female infertility in a Nigerian tertiary hospital: A case-control study. Afr J Reprod Health. 2022;26:66-82. [RCA] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 25. | Moini A, Malekzadeh F, Amirchaghmaghi E, Kashfi F, Akhoond MR, Saei M, Mirbolok MH. Risk factors associated with endometriosis among infertile Iranian women. Arch Med Sci. 2013;9:506-514. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 26] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 26. | Tworoger SS, Fairfield KM, Colditz GA, Rosner BA, Hankinson SE. Association of oral contraceptive use, other contraceptive methods, and infertility with ovarian cancer risk. Am J Epidemiol. 2007;166:894-901. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 106] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 27. | FAO. Food and Agriculture Organization of the United Nations, assignee. Minimum dietary diversity for women: a guide for measurement. Rome 2021. |
| 28. | United Nations. Minimum dietary diversity for women: An Updated Guide to Measurement-from Collection to Action. Rome: FOOD & AGRICULTURE ORG; 2021. |
| 29. | Chavarro JE, Rich-Edwards JW, Rosner BA, Willett WC. Diet and lifestyle in the prevention of ovulatory disorder infertility. Obstet Gynecol. 2007;110:1050-1058. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 193] [Cited by in RCA: 229] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 30. | Toledo E, Lopez-del Burgo C, Ruiz-Zambrana A, Donazar M, Navarro-Blasco I, Martínez-González MA, de Irala J. Dietary patterns and difficulty conceiving: a nested case-control study. Fertil Steril. 2011;96:1149-1153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 77] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 31. | World Health Organization. WHO laboratory manual for the examination and processing of human semen. 6 ed. World Health Organization H, editor. Geneva: World Health Organization; 2021 July 20, 2021. 276 p. |
| 32. | Collins GG, Rossi BV. The impact of lifestyle modifications, diet, and vitamin supplementation on natural fertility. Fertil Res Pract. 2015;1:11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 33. | Kamath MS, Bhattacharya S. Demographics of infertility and management of unexplained infertility. Best Pract Res Clin Obstet Gynaecol. 2012;26:729-738. [RCA] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 34. | Alam F, Tariq S, Syed F, and Rehman R. Impact Of Eating Habits And Physical Activity On The Fertility Of Females. Biosight. 2021;2:30-39. [DOI] [Full Text] |
| 35. | Gunn DD, Bates GW. Evidence-based approach to unexplained infertility: a systematic review. Fertil Steril. 2016;105:1566-1574.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 63] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 36. | Centers for Disease Control and Prevention (CDC). Defining Adult Overweight & Obesity: CDC; 2022. Available from: https://www.cdc.gov/obesity/basics/adult-defining.html. |
| 37. | World Health Organization. A healthy lifestyle - WHO recommendations: WHO 2010. Available from: https://www.who.int/europe/news-room/fact-sheets/item/a-healthy-lifestyle---who-recommendations. |
| 38. | World Health Organization. WHO guidelines on physical activity and sedentary behaviour: web annex: evidence profiles. Geneva: WHO; 2020. Available from: https://www.who.int/publications-detail-redirect/9789240015128. |
| 39. | Aboul-Enein BH, Bernstein J, Neary AC. Dietary transition and obesity in selected Arabicspeaking countries: a review of the current evidence. East Mediterr Health J. 2017;22:763-770. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 36] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 40. | Keselman HJ, Othman AR, and Wilcox RR. Preliminary Testing for Normality: Is This a Good Practice? J Mod App Stat Meth. 2013;12:2-19. [RCA] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 41. | Kim HY. Statistical notes for clinical researchers: Chi-squared test and Fisher's exact test. Restor Dent Endod. 2017;42:152-155. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 438] [Cited by in RCA: 763] [Article Influence: 95.4] [Reference Citation Analysis (0)] |
| 42. | Ebrahim EMA, Ghebrehiwot L, Abdalgfar T, and Juni MH. Health Care System in Sudan: Review and Analysis of Strength, Weakness, Opportunity, and Threats (SWOT Analysis). SJMS. 2017;12:133-150. [RCA] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 43. | Ismail M. Regional disparities in the distribution of Sudan's health resources. East Mediterr Health J. 2020;26:1105-1114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 44. | Babikir SA, Elhassan GO, Hamad-Alneil AI, Alfadl AA. Complementary medicine seeking behaviour among infertile women: A sudanese study. Complement Ther Clin Pract. 2021;42:101264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 45. | Yatsenko SA, Rajkovic A. Genetics of human female infertility†. Biol Reprod. 2019;101:549-566. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 128] [Article Influence: 21.3] [Reference Citation Analysis (0)] |
| 46. | Zorrilla M, Yatsenko AN. The Genetics of Infertility: Current Status of the Field. Curr Genet Med Rep. 2013;1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 112] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 47. | Brandes M, Hamilton CJ, van der Steen JO, de Bruin JP, Bots RS, Nelen WL, Kremer JA. Unexplained infertility: overall ongoing pregnancy rate and mode of conception. Hum Reprod. 2011;26:360-368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 59] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 48. | Johnson KM, Slauson-blevins KS, Greil AL, Shreffler KM, and Leyser-whalen O. The Infertility-Abortion Nexus: Does Having Had an Abortion Influence Distress and Help-Seeking for Infertility? Women's Reproductive Health. 2021;8:233-247. [DOI] [Full Text] |
| 49. | Männistö J, Mentula M, Bloigu A, Gissler M, Heikinheimo O, Niinimäki M. Induced abortion and future use of IVF treatment; A nationwide register study. PLoS One. 2019;14:e0225162. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 50. | Jacob L, Gerhard C, Kostev K, Kalder M. Association between induced abortion, spontaneous abortion, and infertility respectively and the risk of psychiatric disorders in 57,770 women followed in gynecological practices in Germany. J Affect Disord. 2019;251:107-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 51. | Popova S, Lange S, Probst C, Shield K, Kraicer-Melamed H, Ferreira-Borges C, Rehm J. Actual and predicted prevalence of alcohol consumption during pregnancy in the WHO African Region. Trop Med Int Health. 2016;21:1209-1239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 52. | El Mahi M. Substance use problem in Sudan: elephant in the room. BJPsych Int. 2018;15:89-91. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 53. | Probst C, Manthey J, Merey A, Rylett M, Rehm J. Unrecorded alcohol use: a global modelling study based on nominal group assessments and survey data. Addiction. 2018;113:1231-1241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 31] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 54. | Rich-Edwards JW, Spiegelman D, Garland M, Hertzmark E, Hunter DJ, Colditz GA, Willett WC, Wand H, Manson JE. Physical activity, body mass index, and ovulatory disorder infertility. Epidemiology. 2002;13:184-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 242] [Cited by in RCA: 244] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 55. | Ricci E, Viganò P, Cipriani S, Chiaffarino F, Bianchi S, Rebonato G, Parazzini F. Physical activity and endometriosis risk in women with infertility or pain: Systematic review and meta-analysis. Medicine (Baltimore). 2016;95:e4957. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 30] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 56. | Khalil S, Almobarak AO, Awadalla H, Elmadhoun WM, Noor SK, Sulaiman AA, Ahmed MH. Low levels of physical activity in Sudanese individuals with some features of metabolic syndrome: Population based study. Diabetes Metab Syndr. 2017;11 Suppl 2:S551-S554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 57. | Chavarro JE, Rich-Edwards JW, Rosner B, Willett WC. A prospective study of dairy foods intake and anovulatory infertility. Hum Reprod. 2007;22:1340-1347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 75] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 58. | Kim K, Wactawski-Wende J, Michels KA, Plowden TC, Chaljub EN, Sjaarda LA, Mumford SL. Dairy Food Intake Is Associated with Reproductive Hormones and Sporadic Anovulation among Healthy Premenopausal Women. J Nutr. 2017;147:218-226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 59. | Wise LA, Wesselink AK, Mikkelsen EM, Cueto H, Hahn KA, Rothman KJ, Tucker KL, Sørensen HT, Hatch EE. Dairy intake and fecundability in 2 preconception cohort studies. Am J Clin Nutr. 2017;105:100-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 60. | Gaskins AJ, Chavarro JE. Diet and fertility: a review. Am J Obstet Gynecol. 2018;218:379-389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 214] [Article Influence: 30.6] [Reference Citation Analysis (0)] |
| 61. | Elzaki R, Yunus Sisman M, and Al-mahish M. Rural Sudanese household food consumption patterns. Journal of the Saudi Society of Agricultural Sciences. 2021;20:58-65. [DOI] [Full Text] |
| 62. | Ibrahim A. Food Behavior and Consumption Pattern in Rural White Nile of Sudan. Int J Agric Sc Food Technol. 2018;4:007-14. [DOI] [Full Text] |
| 63. | Musaiger AO, Nabag FO, Al-Mannai M. Obesity, Dietary Habits, and Sedentary Behaviors Among Adolescents in Sudan: Alarming Risk Factors for Chronic Diseases in a Poor Country. Food Nutr Bull. 2016;37:65-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 64. | Elneim EAA. Dietary patterns of University students: A case study of the University of Sennar. IJSR 2013; 2: 396-400. Available from: https://www.ijsr.net/get_abstract.php?paper_id=02013510. |
| 65. | Elhassan MR, Gamal HE, and Mohammed G. Nutrition knowledge attitude and practices among students of Ahfad University for women. IJSR 2013; 4: 25-34. Available from:https://www.indianjournals.com/ijor.aspx?target=ijor:ijsr1&volume=4&issue=1&article=005. |
| 66. | Brosens I, Gordts S, Valkenburg M, Puttemans P, Campo R. Investigation of the infertile couple: when is the appropriate time to explore female infertility? Hum Reprod. 2004;19:1689-1692. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 28] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 67. | Practice Committee of the American Society for Reproductive Medicine. Practice Committee of the American Society for Reproductive Medicine. Smoking and infertility: a committee opinion. Fertil Steril. 2018;110:611-618. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 86] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 68. | de Angelis C, Nardone A, Garifalos F, Pivonello C, Sansone A, Conforti A, Di Dato C, Sirico F, Alviggi C, Isidori A, Colao A, Pivonello R. Smoke, alcohol and drug addiction and female fertility. Reprod Biol Endocrinol. 2020;18:21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 87] [Article Influence: 17.4] [Reference Citation Analysis (0)] |
| 69. | Ruder EH, Hartman TJ, Goldman MB. Impact of oxidative stress on female fertility. Curr Opin Obstet Gynecol. 2009;21:219-222. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 167] [Cited by in RCA: 143] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 70. | Kaneda C, Kanejima Y, Kitamura M, Izawa KP. Physical Activity and Body Mass Index in Relation to Infertility in Women. Rev Recent Clin Trials. 2020;15:199-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 71. | Hakimi O, Cameron LC. Effect of Exercise on Ovulation: A Systematic Review. Sports Med. 2017;47:1555-1567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 83] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 72. | Miyatake N, Murakami H, Kawakami R, Tabata I, Miyachi M; NEXIS Study Group. Circulating leptin levels are associated with physical activity or physical fitness in Japanese. Environ Health Prev Med. 2014;19:362-366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 73. | Bouassida A, Zalleg D, Bouassida S, Zaouali M, Feki Y, Zbidi A, Tabka Z. Leptin, its implication in physical exercise and training: a short review. J Sports Sci Med. 2006;5:172-181. [PubMed] |
| 74. | Randolph JF, Ginsburg KA, Leach RE, Blacker CM, Moghissi KS, Diamond MP, Reame NE. Elevated early follicular gonadotropin levels in women with unexplained infertility do not provide evidence for disordered gonadotropin-releasing hormone secretion as assessed by luteinizing hormone pulse characteristics. Fertil Steril. 2003;80:320-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 75. | Mena GP, Mielke GI, Brown WJ. Do physical activity, sitting time and body mass index affect fertility over a 15-year period in women? Hum Reprod. 2020;35:676-683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 76. | Chiu YH, Chavarro JE, Souter I. Diet and female fertility: doctor, what should I eat? Fertil Steril. 2018;110:560-569. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 57] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 77. | Chavarro JE, Schlaff WD. Introduction: Impact of nutrition on reproduction: an overview. Fertil Steril. 2018;110:557-559. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 78. | Skoracka K, Ratajczak AE, Rychter AM, Dobrowolska A, Krela-Kaźmierczak I. Female Fertility and the Nutritional Approach: The Most Essential Aspects. Adv Nutr. 2021;12:2372-2386. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 70] [Article Influence: 17.5] [Reference Citation Analysis (0)] |
| 79. | Panth N, Gavarkovs A, Tamez M, Mattei J. The Influence of Diet on Fertility and the Implications for Public Health Nutrition in the United States. Front Public Health. 2018;6:211. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 67] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 80. | Bu FL, Feng X, Yang XY, Ren J, Cao HJ. Relationship between caffeine intake and infertility: a systematic review of controlled clinical studies. BMC Womens Health. 2020;20:125. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 81. | Abdulslam Abdullah A, Ahmed M, Oladokun A, Ibrahim NA, Adam SN. Serum leptin level in Sudanese women with unexplained infertility and its relationship with some reproductive hormones. World J Biol Chem. 2022;5:83-94. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (1)] |