Published online Jul 20, 2022. doi: 10.5662/wjm.v12.i4.274
Peer-review started: January 23, 2022
First decision: March 25, 2022
Revised: April 8, 2022
Accepted: June 3, 2022
Article in press: June 3, 2022
Published online: July 20, 2022
Processing time: 177 Days and 16.6 Hours
Performing ultrasound during the current pandemic time is quite challenging. To reduce the chances of cross-infection and keep healthcare workers safe, a robotic ultrasound system was developed, which can be controlled remotely. It will also pave way for broadening the reach of ultrasound in remote distant rural areas as well.
To assess the feasibility of a robotic system in performing abdominal ultrasound and compare it with the conventional ultrasound system.
A total of 21 healthy volunteers were recruited. Ultrasound was performed in two settings, using the robotic arm and conventional hand-held procedure. Images acquired were analyzed by separate radiologists.
Our study showed that the robotic arm model was feasible, and the results varied based on the organ imaged. The liver images showed no significant difference. For other organs, the need for repeat imaging was higher in the robotic arm, which could be attributed to the radiologist’s learning curve and ability to control the haptic device. The doctor and volunteer surveys also showed significant comfort with acceptance of the technology and they expressed their desire to use it in the future.
This study shows that robotic ultrasound is feasible and is the need of the hour during the pandemic.
Core Tip: Robotic ultrasound aims to provide remote ultrasound access through a robotic system. This system allows the radiologist to manipulate the ultrasound probe remotely from a safe distant location, in a separate enclosure, thus ensuring the safety of the sonologist and negating the need for a personal protective equipment kit each time, especially in the current coronavirus pandemic. System setup in an intensive care unit (ICU) could ensure that the sonologist can perform the ultrasound without needing to enter the ICU. Going forward, a distance transmission system may also be potentially developed so that patients can also access care at a convenient location without the need to travel long distances, further breaking the chain of transmission. This can be invaluable in a setting where healthcare is not widely available, such as in underserved rural areas.
- Citation: Chandrashekhara SH, Rangarajan K, Agrawal A, Thulkar S, Gamanagatti S, Raina D, Saha SK, Arora C. Robotic ultrasound: An initial feasibility study. World J Methodol 2022; 12(4): 274-284
- URL: https://www.wjgnet.com/2222-0682/full/v12/i4/274.htm
- DOI: https://dx.doi.org/10.5662/wjm.v12.i4.274
Severe acute respiratory syndrome coronavirus-2 has infected millions of people worldwide. As of May 2021, it has infected 157973438 people worldwide and the pandemic continues to rage with a tsunami of cases continuing to be reported in India, USA, and Brazil[1,2]. Healthcare workers (HCW) face an extremely high risk of infection for themselves, a risk that also gets transmitted to their families. Many healthcare workers have been infected and succumbed to the pandemic[3-6]. Although personal protective equipment (PPE) has been effective in protecting HCW, many countries grapple with shortages, and they have immensely added to plastic waste accumulation across the globe. Often, wearing PPE is not feasible or unavailable for HCW in non-coronavirus disease 2019 (COVID-19) designated areas, where the risk of transmission remains high in these times of the pandemic[7].
Telemedicine has evolved immensely in the last few years, though the adoption of these techniques was limited in the pre-pandemic era[8]. This was primarily due to the preference of many doctors and patients to personally see and converse traditionally[9]. The pandemic, however, has brought telemedicine and many of its applications to the forefront, proving that much of the care required can be guided from a distance. Adoption of this technology has received a boost with the pandemic as it provides the much-needed solution to address the challenge of protecting oneself while treating patients adequately.
Imaging plays a vital role in medicine at various stages in terms of diagnostic aid, aiding interventions, and procedures, and in the follow-up of patients. Ultrasonography is a non-invasive, non-ionizing, cost-effective, rapid, bedside, and easily available modality with immense use in point-of-care and follow-up examinations[10]. Often point-of-care ultrasound is the first modality with which a patient is assessed as he/she walks into the casualty. Ultrasound, however, requires an operator to be in close contact with a patient. Ultrasound rooms are often small and lack adequate ventilation, making the operator vulnerable to infection during the pandemic. In addition, ultrasound is often required in intensive care unit (ICU) settings. In the setting of COVID, they may be required for assessment of the chest or screening for thrombosis in veins. This often requires the operator to don and dough the PPE multiple times, despite needing to be present only for a limited amount of time.
Robotic ultrasound aims to provide remote ultrasound access through a robotic system. This system allows the radiologist to manipulate the ultrasound probe remotely from a safe distant location, in a separate enclosure, thus ensuring the safety of the sonologist and negating the need for a PPE kit each time. Similarly, such a system setup in an ICU could ensure that the sonologist can perform the ultrasound without needing to enter the ICU. Going forward, a distance transmission system may also be potentially developed so that patients can also access care at a convenient location without the need to travel long distances, further breaking the chain of transmission. This can be invaluable in a setting where healthcare is not widely available, such as in underserved rural areas.
In this study, we assessed one such system, where the robotic arm is mounted with the probe and is fixed next to the patient couch, and the sonologist operates it with a joystick, at some distance from the patient couch, with the two separated by a glass enclosure.
This prospective study was conducted in the Department of Radio-diagnosis, Dr. BRA Institute Rotary Cancer Hospital, All India Institute of Medical Sciences, New Delhi, India between February 2021 and May 2021. Ethical approval was obtained from the institute ethics committee. Informed consent was obtained from all the volunteers. A total of 21 healthy volunteers were recruited. The sample size was one of convenience as this was a feasibility study. On each volunteer, ultrasound was performed in two settings, using the mobile robotic arm and the conventional hand-held ultrasound by the same sonologist, a few hours apart. The ultrasound examination was performed by a radiologist having 15 years of experience. The ultrasound images obtained using the mobile robotic arm and the conventional hand-held ultrasound were analyzed separately by another blinded radiologist having 20 years of experience. This study was performed to assess the feasibility of the model and its safety. All the healthy volunteers consenting to take part in the study were included. Volunteers who were < 18 years of age or those who did not give consent were excluded from the study.
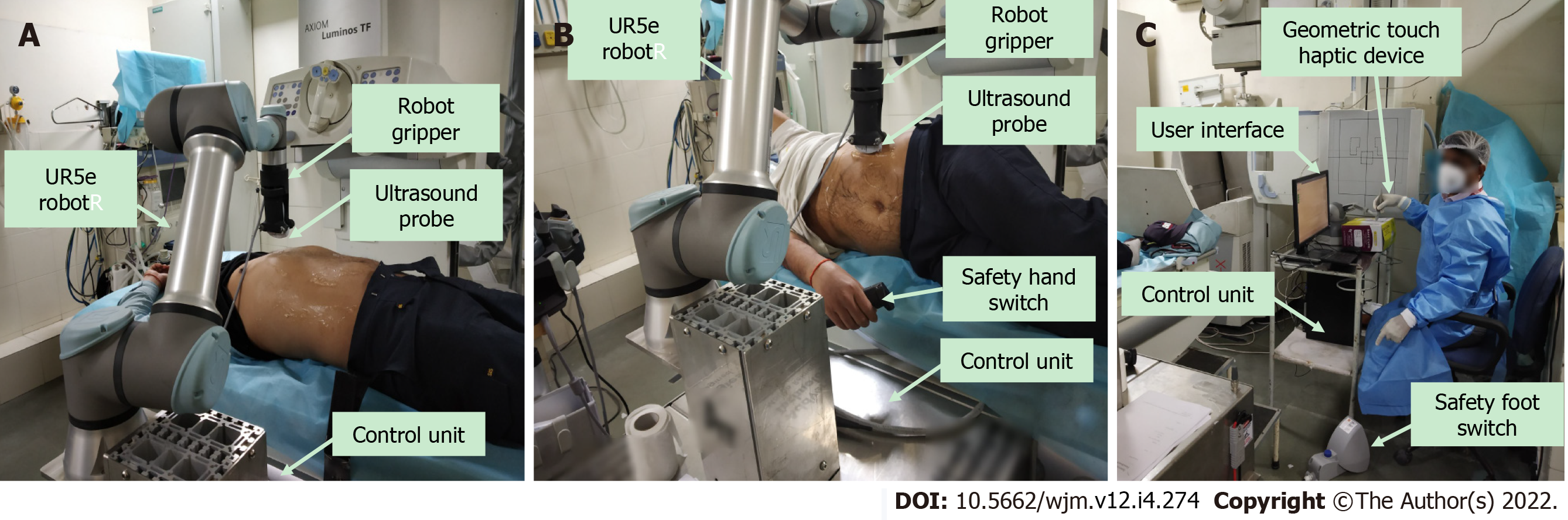
The robotic ultrasound system was co-developed by the Indian Institute of Technology, Delhi, and the All India Institute of Medical Sciences, New Delhi, in collaboration with Adverb Technologies. It consisted of a UR5e (by Universal Robots) robot arm at the patient site with the probe attached at its end using a custom-designed gripper. The doctor’s site consisted of a geomatic haptic touch device (by 3D systems) used to operate the robotic arm. In addition to this haptic device, a monitor with a simple graphic user interface (GUI) was set up at the doctor’s end to allow him or her to do basic control of the system. The sliding scale was provided on GUI to adjust the force exerted by the probe along with live camera feed to visualize the patient movements and responses. The systems were connected through a Wi-Fi router. Safety equipment was provided at both patient and doctor sites (Figure 1), such that the system would come to a complete standstill if pressed at either end.
The patient site includes the robotic arm with the gripper, a USG machine, and an auxiliary staff person. The patient is made to lie on the table with its height and dimensions adjusted according to the robotic arm. The auxiliary staff applies a coupling agent (ultrasound jelly) onto the patient and positions the patient as required. The required transducer is fixed on the gripper based on the exam being performed. The patient is made to hold a safety switch to control.
In the current system, the auxiliary staff performed the ultrasound settings like gain depth and image labeling at the patient end. However, the staff may maintain a safe distance from the patient as they are not required to move the machine or position it continuously during the exam.
The doctor site includes the geomatic haptic device with a stylus tip that is held by the doctor and simulates the probe movements. It also provides haptic (sense of touch) feedback allowing the doctor to perceive feedback sensations of contact between the US probe and the patient body. It also has a user interface with a screen showing the ultrasound images and the patient. Since this was only a feasibility study, the doctor site was created on one end of the same room. This allows only the purpose of safe distancing to be fulfilled. However, this can evolve into a more sophisticated system by using a camera at the patient end to provide video feedback and sufficient bandwidth to prevent communication delays.
The ultrasound machine used for the conventional and robotic ultrasound was the Sonosite M-TURBO model. Ultrasound images were acquired for each patient first using the robotic arm and subsequently by conventional hand-held ultrasound a few hours later. Time taken for each study was noted. After each study, the volunteer and the doctor were asked to fill out a satisfaction survey.
All the images were transferred from the ultrasound machine to a USB drive. A google form questionnaire was created to analyze the images. Images were not annotated, and the conventional and robotic arm images were arranged randomly, each followed by the options.
The images acquired in both settings were evaluated by a reviewer with more than 10 years of experience in a blinded manner. All images were classified subjectively into either of the two groups: Images adequate in resolution and for evaluation with some reservation, and those inadequate for evaluation needing repeat imaging. To compare the conventional hand-held ultrasound and robotic arm ultrasound image data, the Wilcoxon-signed rank test was used.
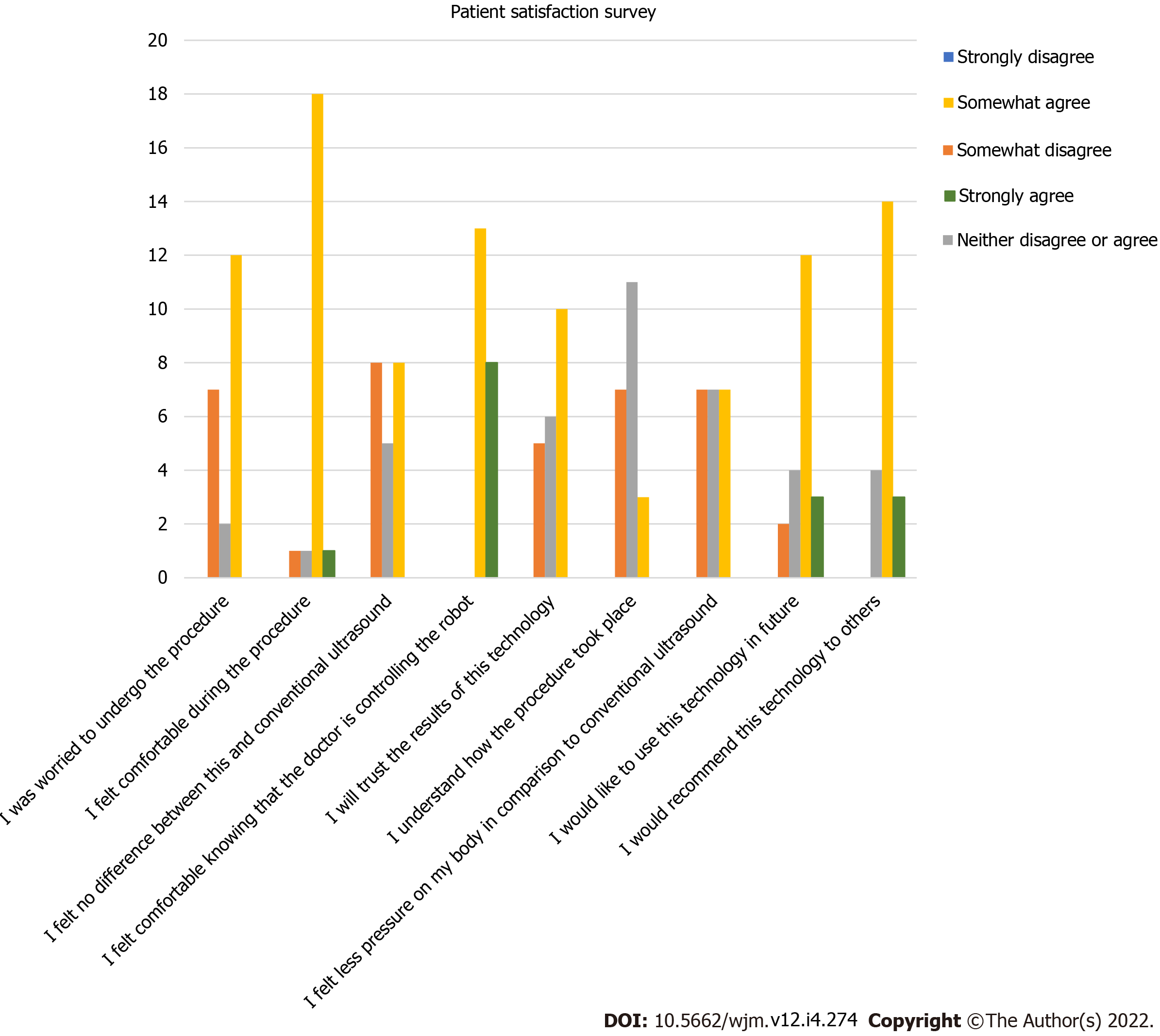
Feedback in the form of satisfaction surveys was taken from each volunteer and the radiologist after each ultrasound (Tables 1 and 2).
| Strongly disagree | Somewhat disagree | Neither disagree nor agree | Somewhat agree | Strongly agree | |
| I was worried to undergo this procedure | 0 (0) | 7 (33.4) | 2 (9.5) | 12 (57.1) | 0 (0) |
| I felt comfortable during the procedure | 0 (0) | 1 (4.8) | 1 (4.8) | 18 (85.6) | 1 (4.8) |
| I felt no difference between this and conventional ultrasound | 0 (0) | 8 (38.1) | 5 (23.8) | 8 (38.1) | 0 (0) |
| I felt comfortable knowing that doctor is controlling the robot | 0 (0) | 0 (0) | 0 (0) | 13 (61.9) | 8 (38.1) |
| I will trust the results of this technology | 0 (0) | 5 (23.8) | 6 (28.6) | 10 (47.6) | 0 (0) |
| I understand how the procedure took place | 0 (0) | 7 (33.4) | 11 (52.4) | 3 (14.3) | 0 (0) |
| I felt less pressure on my body in comparison to conventional ultrasound | 0 (0) | 7 (33.33) | 7 (33.33) | 7 (33.33) | 0 (0) |
| I would like to use this technology in future | 0 (0) | 2 (9.5) | 4 (19.1) | 12 (57.1) | 3 (14.3) |
| I would recommend this technology to others | 0 (0) | 0 (0) | 4 (19.1) | 14 (66.6) | 3 (14.3) |
| Overall rating | Average: 6.2 |
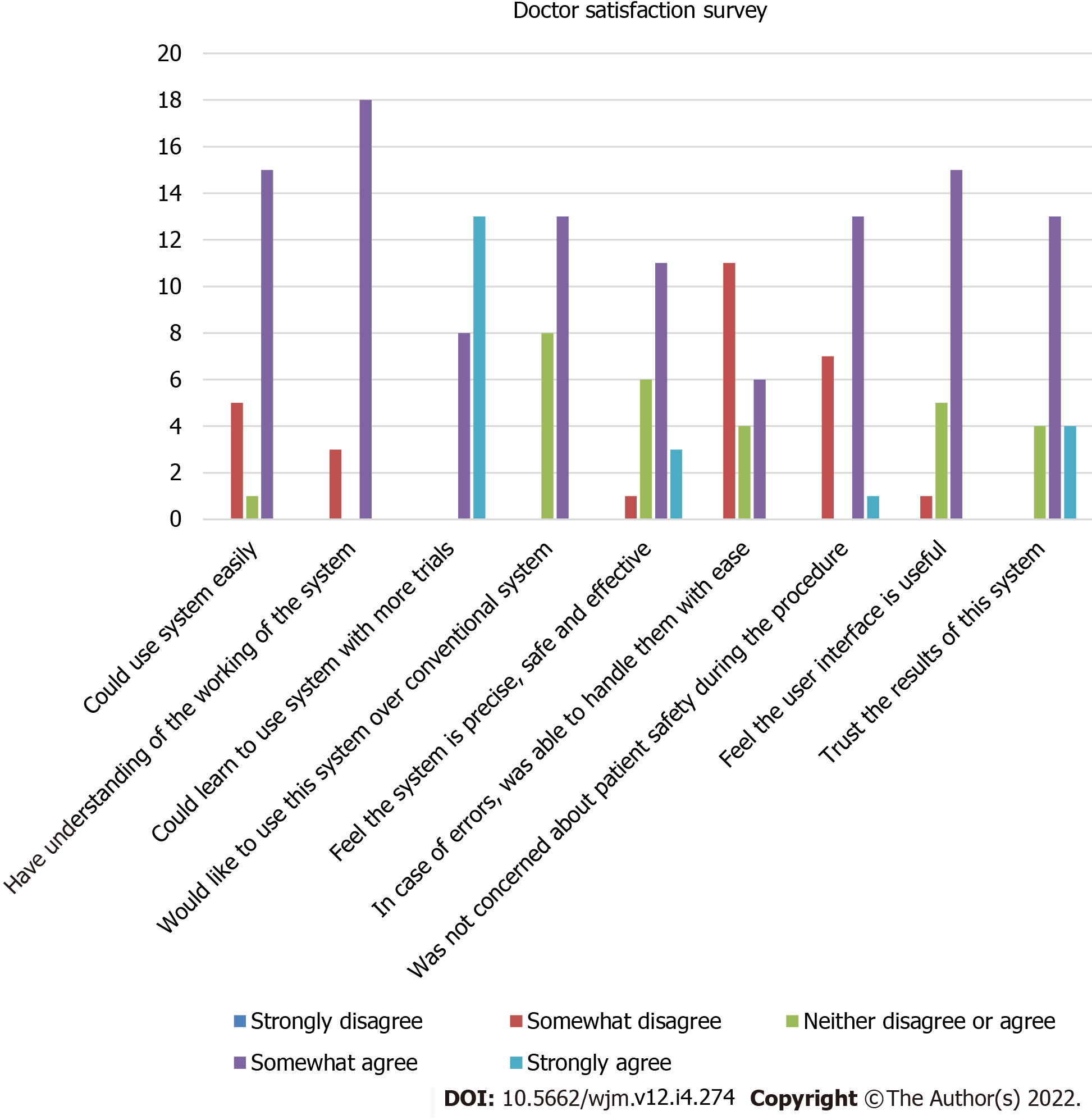
| Strongly disagree | Somewhat disagree | Neither disagree nor agree | Somewhat agree | Strongly agree | |
| I could use the system easily | 0 (0) | 5 (23.8) | 1 (4.8) | 15 (71.4) | 0 (0) |
| I have understanding of the working of the system | 0 (0) | 3 (14.3) | 0 (0) | 18 (85.7) | 0 (0) |
| I could learn to use the system with more trials | 0 (0) | 0 (0) | 0 (0) | 8 (38.1) | 13 (61.9) |
| I would like to use the system over conventional system | 0 (0) | 0 (0) | 8(38.1) | 13(61.9) | 0 (0) |
| I feel the system is precise, safe, and effective | 0 (0) | 1 (4.8) | 6 (28.6) | 11 (52.4) | 3 (14.2) |
| In case of errors, I was able to handle them with ease | 0 (0) | 11 (52.4) | 4 (19) | 6 (28.6) | 0 (0) |
| I was not concerned about the safety of the patient during the procedure | 0 (0) | 7 (33.3) | 0 (0) | 13 (61.9) | 1 (4.8) |
| I feel the user interface is useful | 0 (0) | 1 (4.8) | 5 (23.8) | 15 (71.4) | 0 (0) |
| I trust the results of the system | 0 (0) | 0 (0) | 4 (19.05) | 13 (61.9) | 4 (19.05) |
| Overall rating | Average: 6.38 |
All patients included in our study were males with a mean age of 37.09 ± 9.69 years. The average time taken to perform the conventional ultrasound was 4.05 min (range, 2-7 min), while that taken to perform an ultrasound using a robotic arm was 8.57 min (range, 4-17 min) (Table 3).
| Patient | Conventional hand-held (min) | Robotic arm (min) |
| 1 | 3 | 17 |
| 2 | 5 | 17 |
| 3 | 5 | 17 |
| 4 | 3 | 15 |
| 6 | 2 | 10 |
| 7 | 4 | 9 |
| 8 | 4 | 8 |
| 9 | 7 | 6 |
| 10 | 4 | 9 |
| 11 | 4 | 6 |
| 12 | 5 | 5 |
| 13 | 6 | 8 |
| 14 | 3 | 8 |
| 15 | 4 | 6 |
| 16 | 3 | 5 |
| 17 | 4 | 4 |
| 18 | 5 | 4 |
| 19 | 3 | 7 |
| 20 | 5 | 6 |
| 21 | 3 | 8 |
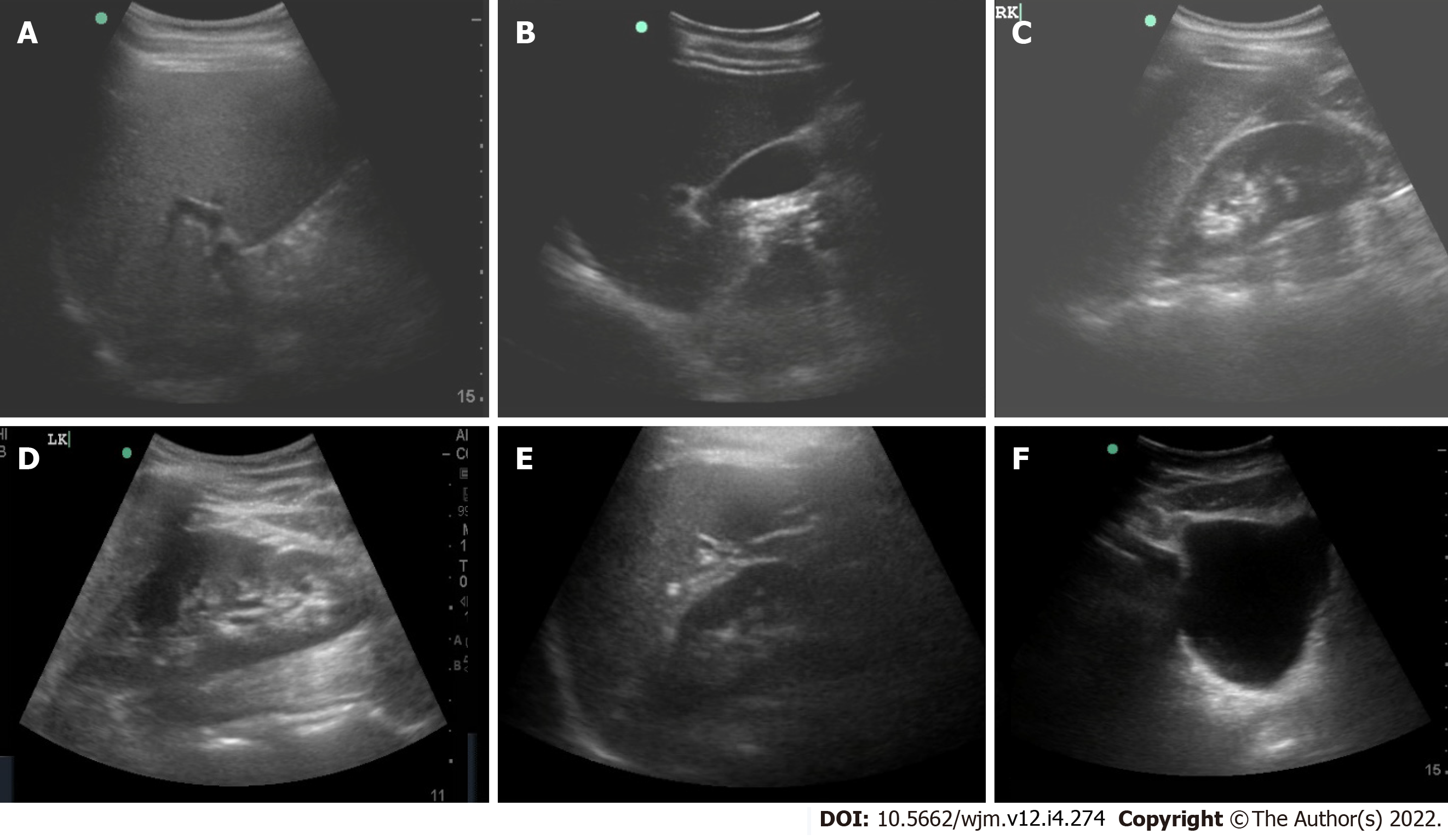
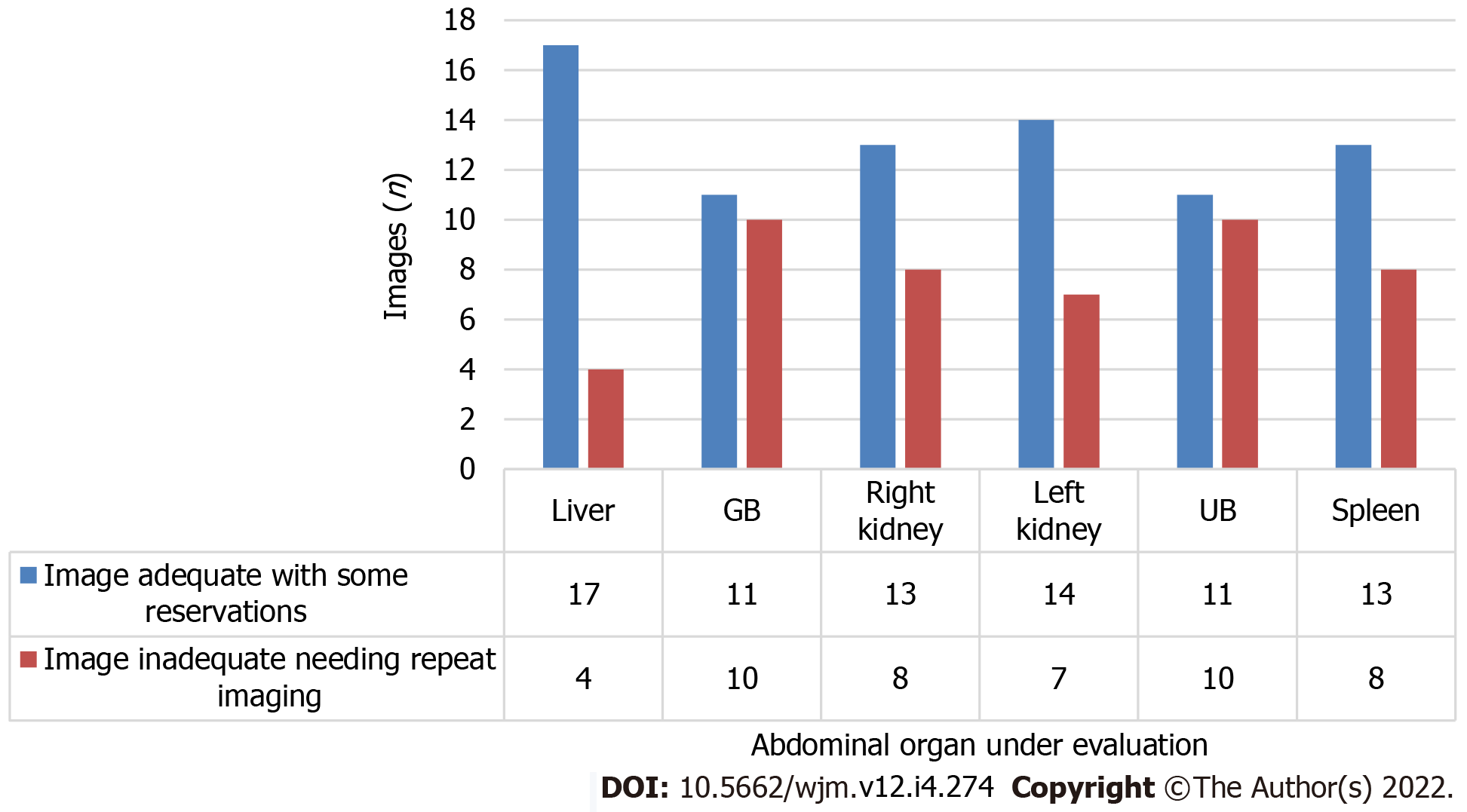
Images acquired using robotic arm ultrasound were divided into two groups (Figure 2). Image evaluation showed that 17/21 (80.9%) images of the liver were adequate with few reservations, while 4/21 (19%) required repeat imaging. Imaging of the gallbladder showed that 11/21 (52.4%) images were adequate, and 10/21 (47.6%) needed repeat imaging (Figure 3).
In the genito-urinary system, the right kidney (RK) image evaluation showed that 13/21 (61.9%) images were adequate with some reservations, and 8/21(38.1%) needed repeat imaging. For the left kidney (LK), 14/21 (66.67%) images were adequate with some reservations, and 7/21 (33.33%) needed repeat imaging. For the urinary bladder (UB), 11/21 (52.4%) images were adequate with some reservations, and 10/21 (47.6%) needed repeat imaging. Evaluation of the spleen ultrasound images showed that 13/21 (61.9%) images were adequate, and 8/21 (38.1%) needed repeat imaging.
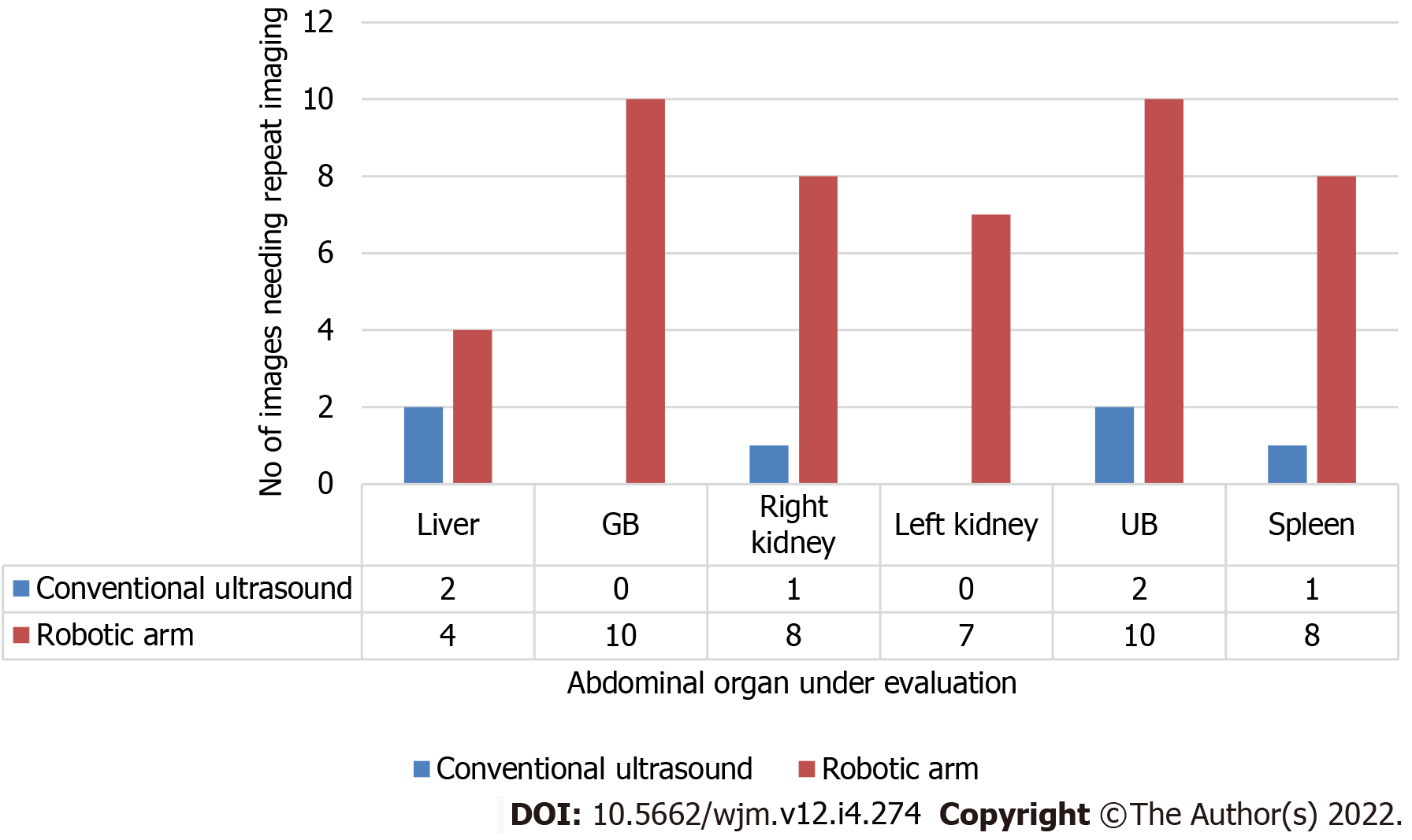
Ultrasound images of the hepato-biliary system showed no significant difference in the need for repeat imaging of the liver between the conventional (2/21) and robotic arm (4/21) groups. GB evaluation showed a significant difference in the need for repeat imaging between the conventional (0/21) and robotic arm (10/21) groups.
In the genito-urinary system, there was a significant difference in the need for repeat imaging between the conventional (RK = 1/21, LK = 0/21, and UB = 2/21) and robotic arm (RK = 8/21, LK = 7/21, and UB = 10/21) ultrasound. Evaluation of the spleen also showed a significant difference in the need for repeat imaging in the conventional (1/21) and robotic arm (8/21) groups (Figure 4).
The radiologists performing the ultrasound using a robotic arm were asked to fill a satisfaction survey after each ultrasound examination. The radiologists somewhat disagreed with being able to use the system with ease in the initial five scans, followed by some agreement in being able to use the system easily in 15 scans. The radiologists somewhat agreed to understand the system in 18 scans. On the survey of wanting to use the robotic arm over a conventional system, the radiologist somewhat agreed in 13 scans. The radiologists reported difficulty in case of being able to handle errors with ease (somewhat disagreed in 11 cases). The radiologists showed some concern about the safety of the patients in seven scans. They found the user interface to be useful and trusted the results of the system in the majority of the cases. The overall rating of the system was between 5 and 7, with an average of 6.38 (Figure 5).
Each volunteer was requested to fill out a satisfaction survey after the set of ultrasounds (both conventional and robotic arms).
The volunteers were somewhat worried to undergo this procedure (n = 12); however, most of them “somewhat agreed” to have felt comfortable during the procedure (n = 18). The volunteers “somewhat disagreed” to feeling no difference between robotic and conventional ultrasound. They somewhat agreed to be feeling more comfortable knowing that the doctor is controlling the robot. The volunteers were equivocal on trusting the results of the technology (n = 14 neither agreed nor disagreed, n = 4 somewhat agreed, and n = 1 somewhat disagreed). The volunteers somewhat agreed to understand how the procedure took place (n = 16). The volunteers did experience some pressure on their body with the robotic arm-loaded probe; however, they somewhat agreed (n = 19) that the pressure was equal to or less than conventional ultrasound and was not discomforting. The volunteers showed acceptance towards the technology (n = 12 somewhat agreed) and on their likelihood to use the technology in the future and recommended it to others (n = 14 somewhat agreed). The overall rating of the system was between 4 and 8, with an average of 6.2 (Figure 6). This can be attributed to the learning curve at the initial time.
There were only male volunteers in our study, which was coincidental and did not result from any deliberate selection or exclusion. The average time taken for ultrasound using a robotic arm in our study was almost double in comparison with that performed by hand-held ultrasound. Initial ultrasound exams in our study using the robotic arm took 17 min; however, as the operators became more accustomed to it, this was reduced to 4-7 min in the later ultrasound exams, which was comparable to that with handheld conventional ultrasound. This likely represents the learning curve associated with robotic ultrasound. This shows that with practice and as familiarity increases with the arm, imaging times would be very comparable to conventional ultrasound.
Image evaluation showed that most of the images acquired using the robotic arm were adequate with some reservations. In the evaluation of the liver, kidney, and spleen, the robotic arm performed well. However, evaluation of the gallbladder and UB showed that the robotic arm images needing repeat imaging were significantly more than conventional imaging. This could be attributed to fine probe angulations needed to focus on these organs.
In comparison with the conventional ultrasound images, evaluation of the liver using both modalities showed no significant difference. This could be attributed to the ability to image the liver in a supine manner without significant probe inclination. For the rest of the organs evaluated, there was a significant difference in the need for repeat imaging between conventional ultrasound and robotic arm ultrasound.
This can be attributed to the learning curve required for the radiologist to be able to control the haptic device and perform fine probe inclinations. With increasing experience later in the study, we observed that satisfactory scores for all images improved. The operators also subjectively reported better coordination and adaptation, which may help achieve better images using the robotic arm.
The radiologists performing the ultrasounds were able to use the system after an initial lag and understood the working of the system. The radiologists indicated their preference to use the system over the conventional ultrasound, which could be attributed partially to the current exposure of the healthcare workers during the pandemic. The radiologists experienced some difficulty in handling errors with the system, particularly at the beginning of the study, which needed the intervention of engineers. However, this was eventually addressed in the later part of the study, indicating again a need for dedicated training on the system before use. Regarding the safety of the patients, there was initial apprehension, both among radiologists and patients, concerning the landing of the robotic arm mounted with a probe on the patient’s abdomen and the pressure exerted during the examination. However, assurance was provided about adequate prior testing; in addition, the interface at the doctor’s end allowed force monitoring (through a slider on the computer screen) which may be used for dynamically increasing or decreasing the pressure whenever required. With controlled motions and increasing experience, the apprehension for patient safety was reduced. The radiologists found the user interface useful and were able to understand it with ease and trusted the results of the system. The radiologist performing the scan was more confident of the findings as he had scanned the entire organ compared to the single image provided for evaluation.
The volunteers were initially apprehensive to undergo the procedure as it was a first-time experience for them. Most of the volunteers were comfortable during the ultrasound. The volunteers felt that they were more comfortable with the conventional hand-held technique as it allowed more interaction with the radiologist. However, in some situations, they would be more comfortable using this technique. The awareness that the arm was being operated by a radiologist made them more comfortable and willing to use the technology in the future. The volunteers believed that the force exerted by the robotic arm-mounted probe was almost similar to that exerted by conventional ultrasound. The volunteers also indicated that they felt secure and comfortable with the technology and were willing to use the same in the future and recommend it to others.
The major limitation with the robotic arm is the increased setup and working cost. This cost is justified in the case of pandemic situations like the current one. However, it may take some time to become a routine method of performing ultrasound.
With the current robotic system, auxiliary staff is needed at the patient end for helping with patient positioning and rotation during the examination and for the application of the coupling agent. However, the staff is not needed to remain close to the patient during the entire study and may maintain a safe distance once the patient is positioned and a coupling agent was applied. With the use of a robotic arm for gel application, this time may be further reduced.
There is a learning curve required to be able to operate the haptic device; however, it was seen that with adequate training, the initial difficulty could be mitigated. Time for comfortable ultrasound was also organ based with imaging requiring more probe angulation and inclination requiring more time for the operator to be able to coordinate the haptic device and the robotic arm’s movements.
Our study had a small sample size, and recruiting more volunteers or patients would allow us to assess the system better.
Robotic ultrasound is the need of the hour, especially during this pandemic. The conventional hand-held ultrasound is the gold standard and is more cost-effective; however, in specific scenarios like the current pandemic, the robotic ultrasound is vital. Efficient use of this technology like other forms of telemedicine can help break the chain of transmission, reduce the amount of plastic waste, and provide adequate care while keeping the healthcare workers and patients safe. It will also play a role in broadening the reach of ultrasound in rural areas, thus improving the standards of health care.
Special circumstances like the current pandemic have led to the need to exploit the utility of robotics and telecommunication systems to perform remote diagnostic ultrasound. It requires robust engineering effort to achieve high precision, flexibility, and repeatability, which can replace the conventional handheld ultrasound examination. A robotic ultrasound system was developed in this study so that ultrasound examination can be performed without having patient contact with the radiologist.
In the coronavirus 2019 (COVID-19) pandemic, the chances of cross-infection significantly increase among health care workers while performing ultrasound examination. There is a need to negate the need for a PPE kit each time when ultrasound examination is done, especially in COVID wards. This has motivated us to develop the robotic ultrasound system and conduct a study to validate it.
To perform ultrasound remotely using a mobile robotic arm on healthy volunteers to assess the feasibility and effectiveness of the system; validate the system by comparing the accuracy of the images generated through remote manipulations of probe attached to robotic arm by the radiologist; and to assess the comfort of the patient and radiologist with the robotic technology.
This prospective study was conducted in the Department of Radio-diagnosis, All India Institute of Medical Sciences, New Delhi, India. Ethical approval was obtained from the institute ethics committee. Informed consent was taken from all the volunteers. A total of 21 healthy volunteers were recruited. On each volunteer, ultrasound was performed in two settings, using the mobile robotic arm and the conventional hand-held ultrasound by the same sonologist. The ultrasound images acquired using the mobile robotic arm and the conventional hand-held ultrasound were analyzed separately by another blinded radiologist.
Our study showed that the robotic arm model was safe and feasible, and the results varied based on the imaged abdominal organs. The liver images showed no significant difference. For other abdominal organs (such as the pancreas, spleen, kidneys, and urinary bladder), the need for repeat imaging was higher in case of robotic arm, which could be attributed to the learning curve and ability to control the haptic device. The doctor and volunteer surveys demonstrated significant comfort with acceptance of the technology and desire to use it in the future.
This study shows that robotic ultrasound is safe and feasible and has potential to perform ultrasound with reliability.
The scope of the developed tele-robotic ultrasound system can be expanded to perform ultrasound examinations remotely in distant rural places, emergency, trauma, and isolation wards.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medical laboratory technology
Country/Territory of origin: India
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ardengh JC, Brazil; Wahome R, United States A-Editor: Liu X, United States S-Editor: Wang LL L-Editor: Wang TQ P-Editor: Wang LL
| 1. | WHO. Coronavirus (COVID-19) Dashboard [Internet]. [RCA] [DOI] [Full Text] [Cited by in Crossref: 439] [Cited by in RCA: 293] [Article Influence: 58.6] [Reference Citation Analysis (0)] |
| 2. | COVID. Live Update: 159, 659,062 Cases and 3,319,284 Deaths from the Coronavirus - Worldometer [Internet]. [DOI] [Full Text] |
| 3. | Lancet T. COVID-19: protecting health-care workers. The Lancet. 2020;395:922. |
| 4. |
Mehta S, Machado F, Kwizera A, Papazian L, Moss M, Azoulay É, et al COVID-19: a heavy toll on health-care workers.
|
| 5. | Erdem H, Lucey DR. Healthcare worker infections and deaths due to COVID-19: A survey from 37 nations and a call for WHO to post national data on their website. Int J Infect Dis. 2021;102:239-241. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 108] [Cited by in RCA: 132] [Article Influence: 26.4] [Reference Citation Analysis (0)] |
| 6. | Nguyen LH, Drew DA, Graham MS, Joshi AD, Guo CG, Ma W, Mehta RS, Warner ET, Sikavi DR, Lo CH, Kwon S, Song M, Mucci LA, Stampfer MJ, Willett WC, Eliassen AH, Hart JE, Chavarro JE, Rich-Edwards JW, Davies R, Capdevila J, Lee KA, Lochlainn MN, Varsavsky T, Sudre CH, Cardoso MJ, Wolf J, Spector TD, Ourselin S, Steves CJ, Chan AT; COronavirus Pandemic Epidemiology Consortium. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health. 2020;5:e475-e483. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1446] [Cited by in RCA: 1380] [Article Influence: 276.0] [Reference Citation Analysis (0)] |
| 7. | Zhang DY, Liu H, Rizwan Younis M, Lei S, Yang C, Lin J, Qu J, Huang P. Corrigendum to "Ultrasmall platinum nanozymes as broad-spectrum antioxidants for theranostic application in acute kidney injury" [Chem. Eng. J. 409 (2020) 127371]. Chem Eng J. 2021;421:129963. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 8. | Mann DM, Chen J, Chunara R, Testa PA, Nov O. COVID-19 transform health care through telemedicine: Evidence from the field. J Am Med Inform Assoc. 2020;27:1132-1135. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 662] [Cited by in RCA: 886] [Article Influence: 177.2] [Reference Citation Analysis (0)] |
| 9. | Hjelm NM. Benefits and drawbacks of telemedicine. J Telemed Telecare. 2005;11:60-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 234] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 10. | Hussain A, Via G, Melniker L, Goffi A, Tavazzi G, Neri L, Villen T, Hoppmann R, Mojoli F, Noble V, Zieleskiewicz L, Blanco P, Ma IWY, Wahab MA, Alsaawi A, Al Salamah M, Balik M, Barca D, Bendjelid K, Bouhemad B, Bravo-Figueroa P, Breitkreutz R, Calderon J, Connolly J, Copetti R, Corradi F, Dean AJ, Denault A, Govil D, Graci C, Ha YR, Hurtado L, Kameda T, Lanspa M, Laursen CB, Lee F, Liu R, Meineri M, Montorfano M, Nazerian P, Nelson BP, Neskovic AN, Nogue R, Osman A, Pazeli J, Pereira-Junior E, Petrovic T, Pivetta E, Poelaert J, Price S, Prosen G, Rodriguez S, Rola P, Royse C, Chen YT, Wells M, Wong A, Xiaoting W, Zhen W, Arabi Y. Multi-organ point-of-care ultrasound for COVID-19 (PoCUS4COVID): international expert consensus. Crit Care. 2020;24:702. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 94] [Cited by in RCA: 86] [Article Influence: 17.2] [Reference Citation Analysis (0)] |