Published online May 20, 2022. doi: 10.5662/wjm.v12.i3.113
Peer-review started: December 17, 2021
First decision: March 24, 2022
Revised: March 27, 2022
Accepted: May 7, 2022
Article in press: May 7, 2022
Published online: May 20, 2022
Processing time: 152 Days and 10 Hours
Nursing officers are an integral component of any medical team. They participate in taking care of basic airway management and assist in advanced airway management, specifically amidst the current coronavirus disease 2019 (COVID-19) pandemic.
To assess the efficacy of a standardized web-based training module for nurses in preparedness to fight against COVID-19.
The training was held in three sessions of 1 h each, consisting of live audio-visual lectures, case scenarios, and skill demonstrations. The sequence of airway equipment, drug preparation, airway examination, and plans of airway management was demonstrated through mannequin-based video-clips.
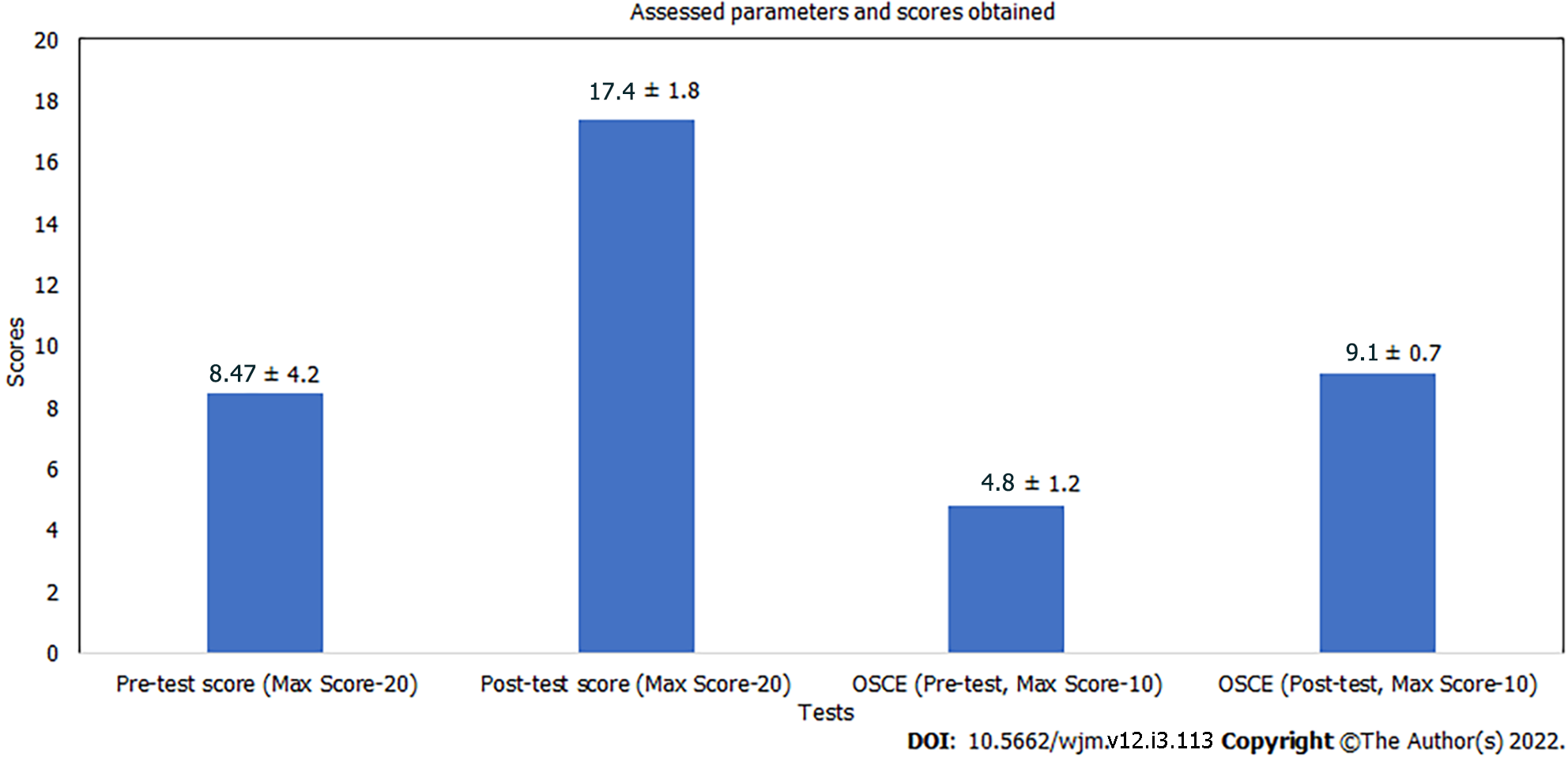
Pre- and post-test scores as well as objective structured clinical examination scores were analyzed using Student’s t-test and the Likert scale was used for feedback assessment. It was found that the mean score out of the total score of 20 was 8.47 ± 4.2 in the pre-test, while in the post-test it was 17.4 ± 1.8 (P value < 0.001). The participants also felt self-reliant in executing the roles of airway assistant (63.3%) and drug assistant (74.3%). Fear of self-infection with COVID-19 was also high, as 66% of participants feared working with the patient’s airway.
Amidst this COVID-19 emergency, when the health care systems are being persistently challenged, training of nursing staff in the safe conduct of airway management can ensure delivery of life-saving treatment.
Core Tip: The health care response systems are being persistently challenged by coronavirus disease 2019 (COVID-19). Nurses are actively involved in various tasks of airway management like preparation of airway equipment, drugs, and basic airway management. This study demonstrated a gross lack of knowledge regarding airway management despite receiving basic life support training. The participants felt more self-reliant and confident in executing the roles of airway assistant and drug assistant after the session. There is a need to train nursing staff from different subsets of practice in the safe conduct of airway management and simulation based online training program for health professionals can be employed for preparedness against COVID-19.
- Citation: Gupta B, Jain G, Pathak S, Mishra P, Kumar H, Rao S. Airway management training program for nurses via online course in COVID-19 preparedness. World J Methodol 2022; 12(3): 113-121
- URL: https://www.wjgnet.com/2222-0682/full/v12/i3/113.htm
- DOI: https://dx.doi.org/10.5662/wjm.v12.i3.113
Coronavirus infection is a public health emergency of international concern[1]. The frontline health care workers are at a heightened risk of catching the disease[2]. Nearly 15% of coronavirus disease 2019 (COVID-19) patients require hospitalization and oxygen support and 5% require definitive airway management. As it primarily involves the respiratory system, the caring medical team should acquire airway management skills[3]. Nursing officers are an integral component of such team, taking care of basic airway management and assisting in advanced airway management[4]. The World Health Organization (WHO)'s prescribed norm is one doctor and three nurses for 1000 people. A wide disparity, however, prevails in the health care professional to population ratio, with developing nations having poorer statistics. The nurse/population ratio is 2.1 in India, as per the latest available WHO’s global health workforce statistics[5]. This highlights our currently overloaded staff and also the necessity to keep our health care workers safe while dealing with COVID-19 patients as we cannot afford to lose the already worn-down workforce[6]. Acquiring adequate skills for airway management demands both technical proficiency and clinical knowledge. A lapse in judgment can contribute to increased morbidity and mortality in critically ill patients. Due to the threat of viral contamination during face-to-face training, online teaching is rising as the new norm of education. Thus, with the safety of health care workers as our chief priority, we designed an interactive online airway course to increase the ability of nursing officers in airway management of critically sick patients. The aim of the study was to assess the efficacy of a standardized web-based training module in preparedness to fight against COVID-19 and enhance Emergency Airway Response Team, knowledge, team dynamics, and personnel confidence.
After institutional ethical approval (study registration No. AIIMS/IEC/20/283), we conducted a prospective, observational study over a period of 4 mo at the Advanced Center of Continuous Professional Development (CPD) Department through a dedicated online course conducted thrice weekly in our tertiary care institute. Our study was designed following the STROBE guidelines. A list of 30 participants (nursing officers) per session was prepared and we ensured a uniform representation from each department. Inability to attend the course due to prior commitment or network issues led to exclusion from that session and such participants were subsequently included in next scheduled course. Course content was diligently constructed to cover information regarding pandemic preparation, COVID-19 spread, risk alleviation, education about personnel protective equipment (PPE), protection required during airway procedures, signs of respiratory distress, indications of intubation, airway assessment, difficult airway predictors, airway management guidelines and sequence of plan, catalogue of airway equipment and COVID-19 intubation kit, drugs, procedure of rapid sequence induction, mask ventilation using vice grip, steps of video-laryngoscopy, intubation, supraglottic airway placement, and front of neck access (FONA).
Through the online portal of “Google meet”, the training was held in three sessions of 1 h each, consisting of live audio-visual relay of lectures, case scenarios, presentations, and skill station. The sequence of personal protection, airway equipment and drug preparation, designated COVID-19 isolation area for airway management, clinical airway examination with difficult airway assessment using MACHOCHA score, and plans of airway management (Plans A, B, C, and D) were demonstrated through simulator mannequin-based video-clips. The skill stations consisted of 1 h and included demonstration of preparation of appropriate equipment and drugs required for induction in a trolley, designation of negative pressure isolation room for intubation, team dynamics, plans of airway management, use of airway adjuncts, intubation using video-laryngoscope (Plan A), choosing appropriate size of supraglottic airway device and its insertion (Plan B), bag-mask ventilation using vice grip (Plan C), and equipment required (Plan D)-surgical scalpel cricothyroidotomy/FONA by the instructors via videos and skill stations. Participants could clarify their doubts by speaking through the microphone or writing it in the common chat window. To ensure an active participation, interaction of participants with instructors in the language that they were most comfortable with was encouraged. Each scenario was followed by a debriefing session, after which the participants were encouraged to enlist their achievements and shortcomings from the session.
The participants were provided with Google form links of “pre- and post-test questionnaire”. Both the questionnaire forms were identical and consisted of 20 multiple-choice questions (1 mark each), which included specific theoretical questions related to airway management. The participants also had to answer 10 objective structured clinical examinations (OSCE), each consisting of one mark each. Each participant’s performance during the skill stations was independently evaluated by two experienced instructors based on OSCE response. For a successful completion of training program, it was necessary for the participants to obtain 70% of marks in the post-test and more than 80% in OSCE assessment. A feedback form was filled at the end of the session, consisting of eight assertions on a 5-point rating Likert scale. The score of “5” indicated “strong agreement” with the statement while a score of “1” indicated that participants were in “strong disagreement” with it. Two faculty members, experts in airway management, validated the questionnaire and survey form at an independent level. An investigator who was blinded to the study protocols collected and then analyzed the outcome data. The basis for sample size estimates was convenience sampling.
The Statistical Package for the Social Sciences version 23.0 software (SPSS, IBM Corp. Armonk, NY, United States) was utilized to perform statistical analyses. A pre- and post-test questionnaire, specifically developed for this course, was analyzed as the primary outcome. The secondary outcome was evaluated as OSCE based assessment. The results are summarized as descriptive statistics and presented as the mean ± SD or mean ± SE. The Student’s t-test was employed to analyze the data for intra- and inter-group comparisons. To assess the survey form, a mean Likert score was averaged to the total number of items. A P value < 0.05 was considered statistically significant.
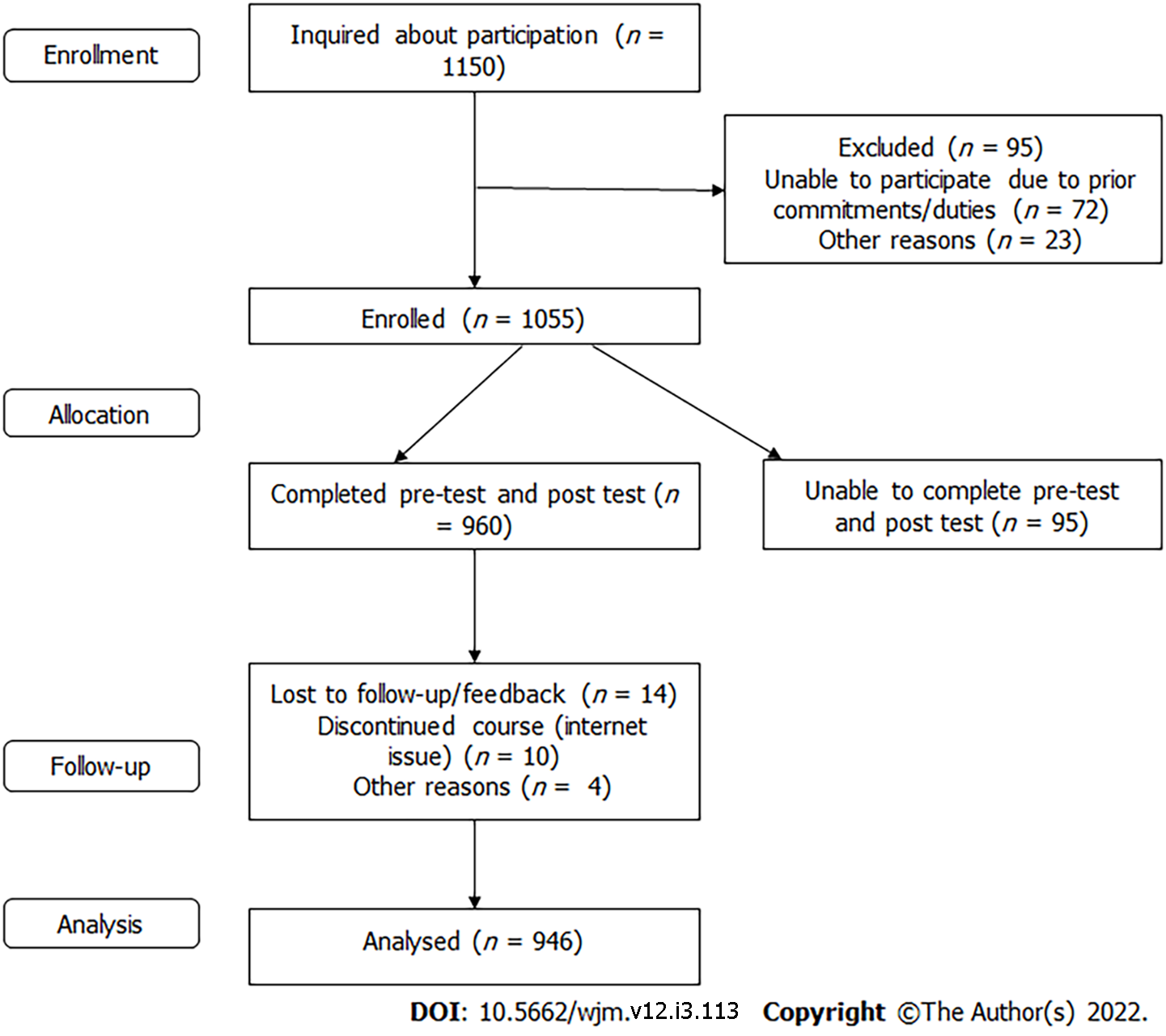
A total of 1055 nursing officers were trained during the program. One hundred and nine participants who could not complete either the pre- or post-test were excluded from the analysis. Nine hundred and forty-six nursing officers were able to complete the pre- and post-test and thus included in the final analysis (Figure 1). The mean years of work experience of the participants was 4.01 ± 3.16 (mean ± SD). On analyzing the questionnaire, it was found that the mean score out of the total score of 20 was 8.47 ± 4.2 in the pre-test, while in the post-test it was 17.4 ± 1.8 (Figure 2); the difference was statistically significant (P < 0.001). Although 68% of our participants were trained in basic life support (BLS), questions in the pre-test, based on the specific knowledge of airway and plans for airway management, were frequently missed. The concept of team dynamics and role allocation was also alien to the majority of nursing officers. The overall knowledge and cognizance regarding airway management of COVID-19 patients improved significantly following the session (P < 0.001). Approximately 92% of the participants accurately responded to specific questions related to airway management in the post-test. There was improvement in OSCE based assessment and all participants could score above 80% in OSCE.
Participants were asked to provide feedback at the end of session. Amongst the various questions asked in feedback, one was pertaining to the part of training which they found most helpful. The video demonstration of airway procedures, preparation of airway trolley, and medications was the most cherished by the nursing officers. After attending the program, 79% of participants felt that they were familiar with airway management techniques and protocols for COVID-19 patients. The participants also felt self-reliant in executing the roles of airway assistant (63.3%) and drug assistant (74.3%). An increase in level of self-confidence was reflected in other parameters like performing laryngoscopy, supraglottic airway device (SGA) insertion, and arrangement of necessary equipment as well (Table 1). Fear of self-infection with COVID-19 was also high, as 66% of participants feared working with the patient’s airway (Table 2). This short online training module for airway management in COVID-19 patients was liked by majority of our participants and they strongly believed that it helped in improving their clinical acumen and skills.
| S. No. | Role/procedure | Percentage of participants with a score ≥ 4 | Percentage of participants with a score of 3 | Percentage of participants with a score ≤ 2 |
| A Pre-training assessment | ||||
| 1 | Airway assistant | 35 | 31 | 34 |
| 2 | Drug assistant | 41 | 45 | 14 |
| 3 | Laryngoscopy | 9 | 15 | 76 |
| 4 | SGA insertion | 14 | 28 | 58 |
| 5 | Familiarity with airway management plan | 29 | 24 | 47 |
| B Post-training assessment | ||||
| 1 | Airway assistant | 63.3 | 21.6 | 15.1 |
| 2 | Drug assistant | 74.3 | 23 | 2.7 |
| 3 | Laryngoscopy | 58 | 13 | 29 |
| 4 | SGA insertion | 78 | 19 | 3 |
| 5 | Familiarity with airway management plan | 79 | 14 | 7 |
| S. No. | Reason for fear | Percentage of participants |
| 1 | Breach in PPE | 49 |
| 2 | High aerosol generation | 34 |
| 3 | Lack of airway experience | 38 |
| 4 | Cross-infection | 57 |
| 5 | Difficult airway situation | 23 |
| 6 | No fear | 18 |
The role of nursing staff in any health care service is indispensable. They form a pivotal part in the patient care in wards, emergency area, outpatient department (OPD), operation theatres, high dependency units, and intensive care units (ICU). They are actively involved in various tasks of airway management like preparation of airway equipment and drugs, checking for adequate resources like oxygen, airway suctioning, and basic airway management[7]. There is a high probability that the first responder to any patient with respiratory urgency is a nurse who might have to manage airway till a physician help arrives[8]. In such a scenario, the lack of knowledge and experience in airway management can not only jeopardize patient care but also result in a heightened risk of infection transmission[9]. The goals for the airway rescuer in COVID-19 patients is to rapidly secure an airway, preferably in first attempt, with clear backup contingencies, while reducing the aerosol generation and preventing redundant contamination[10-12]. European Society guidelines for management of airway in COVID-19 patients, recommend endotracheal intubation using rapid sequence intubation (RSI) for Plan A; in the advent of failure of plan A, SGA placement as Plan B; face mask ventilation as Plan C; and finally FONA as Plan D[13]. Our prime expectation from this training module was to equip the nursing officers with adequate information, clearing their queries and fears related to COVID-19 patient care such that they could efficiently work in a high performing airway rescue team without compromising personal safety. Although the pretest score was as low as 8.47 ± 2.4, by the end of our session, the respondents were clear with these features and achieved a high score of 17.4 ± 1.8. It was evidenced by their poor performance in the pre-test questionnaire regarding airway assessment and difficult airway predictors like modified Mallampati grade and MACOCHA score. The reason for this could be accredited to the mixed population from different practice areas (general wards, OPDs, operation theatres, emergency, and ICU) and the years of experience. We succeeded in educating them about airway assessment sufficiently enough to perform significantly better in the post-session analysis with the same set of questions.
Although the regular curriculum of nursing does impart education about basic airway support, it is not emphasized enough. The proportion of respondents (58%) who were already trained in BLS had a better understanding of basic airway care as compared to those who had not completed BLS course. This was evident by their fair knowledge about identification of respiratory distress, indications for intubation, and basic equipment in airway management. The majority of participants (71%), however, showed gross deficit in information with respect to the plans for airway management, drugs required for RSI, advanced airway equipment like video laryngoscope and procedure of intubation, supraglottic airway device insertion, and FONA. This revealed the necessity to train them in both basic and advanced airway care so that in the crisis, they can play the role of competent assistants in airway management.
Continuing medical education programs, workshops, and seminars comprise an efficient approach to achieve proficient teaching and learning[14,15]. Conforming to the principle of social distancing amidst this highly infectious health emergency, simulation-based medical education has an important role in learning. Various international recommendations include airway training simulation as a part, which has shown to be beneficial with respect to behavior changing process, acquisition of skills, and trainee satisfaction[16].
A wide range of airway complications and increased viral transmission may occur if nurses who are involved in such teams have no experience in emergency airway management[17,18]. Cook et al[19] documented that permanent harm or death due to airway related complications was mainly due to inadequate access to properly skilled staff or equipment, inability to identify at-risk patients, poor planning, and lack of structured strategies for tackling predictable airway complications.
It is noteworthy that registered nurses, even those working in ICU, may spend a larger fraction of working hours in patient care, without the requirement to manage respiratory emergencies on an everyday basis[20]. This in itself reveals the state of experience of nurses working in non-ICU environment with respect to airway care. Kelleher et al[21] conducted a study to investigate the endotracheal care practices amongst critical care nurses and found a wide variety in their techniques, with non-adherence to best practice recommendations and resultant lower-quality care. Another descriptive analytic study showed that the knowledge and performance of intensive care nurses regarding endotracheal suctioning and care was good (71.6 ± 10.91) and medium (41.22 ± 7.91), respectively[22].
The key to effective airway management is proper assessment and anticipation of any associated difficulties[23]. The foundation of any high performing team is a strong understanding of team dynamics. Ranging from deploying of the scarce available resources or employing the latest evidence-based guidelines to building a firm groundwork of healthy teamwork with good and clear communication can provide a strategic lead in tackling this pandemic. Our aim was to emphasize on the clear role allocation, closed loop communication, and cross monitoring (checking for cross- contamination) while working in the airway rescue team. There was a statistically significant improvement in terms of knowledge and confidence in competent role execution as airway team members in the post survey analysis as compared to their pre-test evaluation.
The feedback submitted by the participants highlighted the truth that this global crisis has fostered fear among all healthcare workers. The majority of the participants admitted that the fear was mainly based on risk of breach in PPE, aerosol spread, lack of proper training in airway prior to actual patient handling, and fear of contracting infection and carrying the infection back home amongst others. These responses go in line with a study done in healthcare workers working with COVID-19 patients that revealed higher anxiety, depression, and apprehension due to similar factors among 71.5%, 44.6%, and 50.4% of the respondents, respectively[24,25].
This training module highlighted the need to put more emphasis on airway training of the nursing staff and contributed to fill up the lacunae in the realm of airway care while giving due weightage to occupational safety and health. We believe that by using simulation based online training program for nurses, we successfully educated them and simultaneously strengthened our workforce in airway management, if and when the need arises.
Our study adds to the theoretical development of efficacy of online simulation-based training of health care professionals in inevitable situations like the COVID-19 pandemic. To the best of our knowledge, this is a novel study to train nurses for airway management of COVID-19 patients through an online platform and gives evidence of statistically significant improvement in knowledge, attitude, and confidence regarding the same. We took extra care to reach up to individual level participation and trained them in the language that they understood well. Free will to attend the training program as many times needed was the additional advantage of our course.
We completely acknowledge that the chief and inevitable limitation in our study was an inability to conduct the skill station training in person. The heterogeneous study population with diverse levels of exposure to airway care was another limitation. Although the majority of participants passed the post session evaluation, 140 of them had to repeat this course once due to sub-par scoring. The infrequent issues with internet connectivity, first time online course learning, difficulty to comprehend, and language disturbance were responsible for inefficiency in understanding, leading to poor response in post-test analysis and hence the need for repetition of course.
Amidst this COVID-19 public health emergency, when the health care response systems are being persistently challenged, training of nursing staff from different subsets of practice in the safe practice of airway management can play a substantial role in ensuring access of life-saving treatment to COVID-19 patients, without compromising the safety of health care professionals. Our study in its unique aspect has the potential to pave way for further large-scale research while confirming to incorporate similar training regimes aimed at improving the preparedness and skill of various health professionals to tackle this crisis efficiently.
The nursing officers are an integral part of medical team. They contribute in basic airway management and as an assistant in advanced airway management, which holds great significance in the coronavirus disease 2019 (COVID-19) pandemic.
The pandemic has resulted in over-burdened medical staff with lack of adequate skills for airway management to handle this respiratory disease pandemic.
The primary research objective was to create an interactive online airway course to increase the ability of nursing officers in airway management of critically sick patients.
The training was conducted through live audio-visual lectures, case scenarios, and skill demonstrations through mannequin-based videos. The demonstrations for airway equipment, preparation of drugs, airway examination, and plans of airway management were done.
The mean score out of the total score of 20 was 8.47 ± 4.2 in the pre-test, while it was 17.4 ± 1.8 in the post-test (P < 0.001). After attending the program, 79% of participants felt that they were familiar with airway management techniques and protocols for COVID-19 patients. An increase in level of self-confidence was reflected in other parameters like performing laryngoscopy, Supraglottic airway insertion, and arrangement of necessary equipment as well.
The training of nursing staff from different subsets of practice in the safe practice of airway management can play a substantial role in ensuring access of life-saving treatment to COVID-19 patients, without compromising the safety of health care professionals.
This research has the potential to pave way for further large-scale research while confirming to incorporate similar training regimes aimed at improving the preparedness and skill of various health professionals to tackle this crisis efficiently.
We would like to acknowledge the contribution of all the coordinators, instructors, and participants of this training program and Department of Advanced Centre of Continuous Professional Development and Department of Anesthesiology, All India Institute of Medical Sciences, Rishikesh, India.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Anesthesiology
Country/Territory of origin: India
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Alberca RW, Brazil; Ng DTK, China S-Editor: Ma YJ L-Editor: Wang TQ P-Editor: Ma YJ
| 1. | Stephenson J. Coronavirus Outbreak—an Evolving Global Health Emergency. JAMA Heal Forum. 2020;1:200114. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 2. | Sim MR. The COVID-19 pandemic: major risks to healthcare and other workers on the front line. Occup Environ Med. 2020;77:281-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 173] [Article Influence: 34.6] [Reference Citation Analysis (0)] |
| 3. | Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497-506. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35178] [Cited by in RCA: 30049] [Article Influence: 6009.8] [Reference Citation Analysis (3)] |
| 4. | Sullivan EH, Gibson LE, Berra L, Chang MG, Bittner EA. In-hospital airway management of COVID-19 patients. Crit Care. 2020;24:292. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 5. | Kumar R, Pal R. India achieves WHO recommended doctor population ratio: A call for paradigm shift in public health discourse! J Family Med Prim Care. 2018;7:841-844. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 61] [Reference Citation Analysis (0)] |
| 6. | Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, Wu Y, Zhang L, Yu Z, Fang M, Yu T, Wang Y, Pan S, Zou X, Yuan S, Shang Y. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8:475-481. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6231] [Cited by in RCA: 6654] [Article Influence: 1330.8] [Reference Citation Analysis (0)] |
| 7. | St John RE. Airway management. Crit Care Nurse. 2004;24:93-96. [PubMed] |
| 8. | Jones D, Baldwin I, McIntyre T, Story D, Mercer I, Miglic A, Goldsmith D, Bellomo R. Nurses' attitudes to a medical emergency team service in a teaching hospital. Qual Saf Health Care. 2006;15:427-432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 110] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 9. | Jain G, Gupta B, Gupta P, Rao S. Online training for sensitisation on airway and ventilatory management as preparedness to combat COVID situation. Indian J Anaesth. 2020;64:919-920. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. | Mwakanyanga ET, Masika GM, Tarimo EAM. Intensive care nurses' knowledge and practice on endotracheal suctioning of the intubated patient: A quantitative cross-sectional observational study. PLoS One. 2018;13:e0201743. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 11. | Wax RS, Christian MD. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Can J Anaesth. 2020;67:568-576. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 658] [Cited by in RCA: 608] [Article Influence: 121.6] [Reference Citation Analysis (0)] |
| 12. | Orser BA. Recommendations for Endotracheal Intubation of COVID-19 Patients. Anesth Analg. 2020;130:1109-1110. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 113] [Cited by in RCA: 130] [Article Influence: 26.0] [Reference Citation Analysis (0)] |
| 13. | Sorbello M, El-Boghdadly K, Di Giacinto I, Cataldo R, Esposito C, Falcetta S, Merli G, Cortese G, Corso RM, Bressan F, Pintaudi S, Greif R, Donati A, Petrini F; Società Italiana di Anestesia Analgesia Rianimazione e Terapia Intensiva (SIAARTI) Airway Research Group, and The European Airway Management Society. The Italian coronavirus disease 2019 outbreak: recommendations from clinical practice. Anaesthesia. 2020;75:724-732. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 221] [Cited by in RCA: 232] [Article Influence: 46.4] [Reference Citation Analysis (0)] |
| 14. | Gesme DH, Towle EL, Wiseman M. Essentials of staff development and why you should care. J Oncol Pract. 2010;6:104-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 15. | Cook DA, Hatala R, Brydges R, Zendejas B, Szostek JH, Wang AT, Erwin PJ, Hamstra SJ. Technology-enhanced simulation for health professions education: a systematic review and meta-analysis. JAMA. 2011;306:978-988. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1226] [Cited by in RCA: 1011] [Article Influence: 72.2] [Reference Citation Analysis (0)] |
| 16. | Hodzovic I, Latto I, Pradhan P, Gururaj P, Wilkes A, Gataure P, Popat M. Effect Of The Provision Of An Airway Training Module On The Acquisition Of Complex Airway Skills. Inter J Anesthesiol. 2006;15:1-6. |
| 17. | Dörges V, Wenzel V, Neubert E, Schmucker P. Emergency airway management by intensive care unit nurses with the intubating laryngeal mask airway and the laryngeal tube. Crit Care. 2000;4:369-376. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 18. | Cook TM, MacDougall-Davis SR. Complications and failure of airway management. Br J Anaesth. 2012;109 Suppl 1:i68-i85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 251] [Cited by in RCA: 269] [Article Influence: 20.7] [Reference Citation Analysis (0)] |
| 19. | Cook TM. Strategies for the prevention of airway complications - a narrative review. Anaesthesia. 2018;73:93-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 93] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 20. | Westbrook JI, Duffield C, Li L, Creswick NJ. How much time do nurses have for patients? BMC Health Serv Res. 2011;11:319. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 199] [Cited by in RCA: 221] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 21. | Kelleher S, Andrews T. An observational study on the open-system endotracheal suctioning practices of critical care nurses. J Clin Nurs. 2008;17:360-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 28] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 22. | Higginson R, Parry A, Williams M. Airway management in the hospital environment. Br J Nurs. 2016;25:94-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 23. | Cook TM, El-Boghdadly K, McGuire B, McNarry AF, Patel A, Higgs A. Consensus guidelines for managing the airway in patients with COVID-19: Guidelines from the Difficult Airway Society, the Association of Anaesthetists the Intensive Care Society, the Faculty of Intensive Care Medicine and the Royal College of Anaesthetists. Anaesthesia. 2020;75:785-799. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 619] [Cited by in RCA: 614] [Article Influence: 122.8] [Reference Citation Analysis (0)] |
| 24. | Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, Wu J, Du H, Chen T, Li R, Tan H, Kang L, Yao L, Huang M, Wang H, Wang G, Liu Z, Hu S. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw Open. 2020;3:e203976. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5313] [Cited by in RCA: 4366] [Article Influence: 873.2] [Reference Citation Analysis (0)] |
| 25. | Gupta B, Bajwa SJS, Malhotra N, Mehdiratta L, Kakkar K. Tough times and Miles to go before we sleep- Corona warriors. Indian J Anaesth. 2020;64:S120-S124. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |