Published online Jan 20, 2022. doi: 10.5662/wjm.v12.i1.20
Peer-review started: February 23, 2021
First decision: June 17, 2021
Revised: July 1, 2021
Accepted: November 15, 2021
Article in press: November 15, 2021
Published online: January 20, 2022
Processing time: 327 Days and 17.5 Hours
The global spread of the novel severe acute respiratory syndrome coronavirus 2 has had serious consequences in terms of patient morbidity and mortality and overburdened health care systems as well as the socioeconomic implications. In the absence of effective therapies and vaccinations during the viral outbreak, the major and most concise means to control viral spread is spread prevention. Although information concerning the impact of severe acute respiratory syndrome coronavirus 2 on pediatric surgical patients has greatly expanded, relevant comprehensive studies are scarce. However, pandemic related morbidity has increased, while under normal circumstances mortality could have been minimized.
Core Tip: Severe acute respiratory syndrome coronavirus 2 pandemic related morbidity and mortality have been increased in children. Moreover, pandemic may manifest additional clinical problems. Pediatric surgeons must be aware of the different forms and symptoms in children affected by coronavirus disease 2019 infection.
- Citation: Vaos G, Zavras N. Severe acute respiratory syndrome coronavirus 2 pandemic related morbidity and mortality in patients with pediatric surgical diseases: A concerning challenge. World J Methodol 2022; 12(1): 20-31
- URL: https://www.wjgnet.com/2222-0682/full/v12/i1/20.htm
- DOI: https://dx.doi.org/10.5662/wjm.v12.i1.20
It has been approximately 1 year since the outbreak of novel pneumonia caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was first reported in the city of Wuhan in China. The disease was subsequently named coronavirus disease 2019 (COVID-19)[1]. The global spread of this new virus forced the World Health Organization to declare it a pandemic on March 11, 2020[2]. It is estimated that up to June 23, 2021, about 180079074 people worldwide have already been infected, and the number of confirmed deaths had reached 3900967[3].
In an attempt to restrict the accelerated transmission of the disease, governments and health organizations across the world adopted various measures[4]. The pediatric surgical community responded accordingly, both globally and locally. The American College of Surgeons and the American Pediatric Surgical Association proposed certain criteria for the management and prioritization of pediatric surgical procedures, taking into account elective procedures that could be postponed and balancing the risk between disease progression and viral vulnerability[5,6]. Similarly, the European Association of Urology issued a statement of recommendations for pediatric urological cases during the SARS-CoV-2 era[7]. In the same spirit, the Spanish Association of Pediatric Surgery published and announced elective surgery restrictions, with the exception of emergencies and oncological cases[8]. Several organizations in the United Kingdom also provided evidence-based guidelines for elective pediatric surgical services[9]. In addition to these measures, many hospitals at the local level established extensive protocols for the security, protection, and proper management of sick children and their parents[10].
Apart from the resultant drop in elective surgeries amid SARS-CoV-2 cases[11,12], many pediatric surgical centers also noted a decline in emergency cases[11]. Moreover, the pandemic has seen the emergence of a new clinical entity, defined as multisystem inflammatory syndrome in children (MIS-C), which is considered by many to be a complication of SARS-CoV-2[13].
This study aims to identify the influence of the SARS-CoV-2 pandemic on morbidity and mortality among children with surgical diseases.
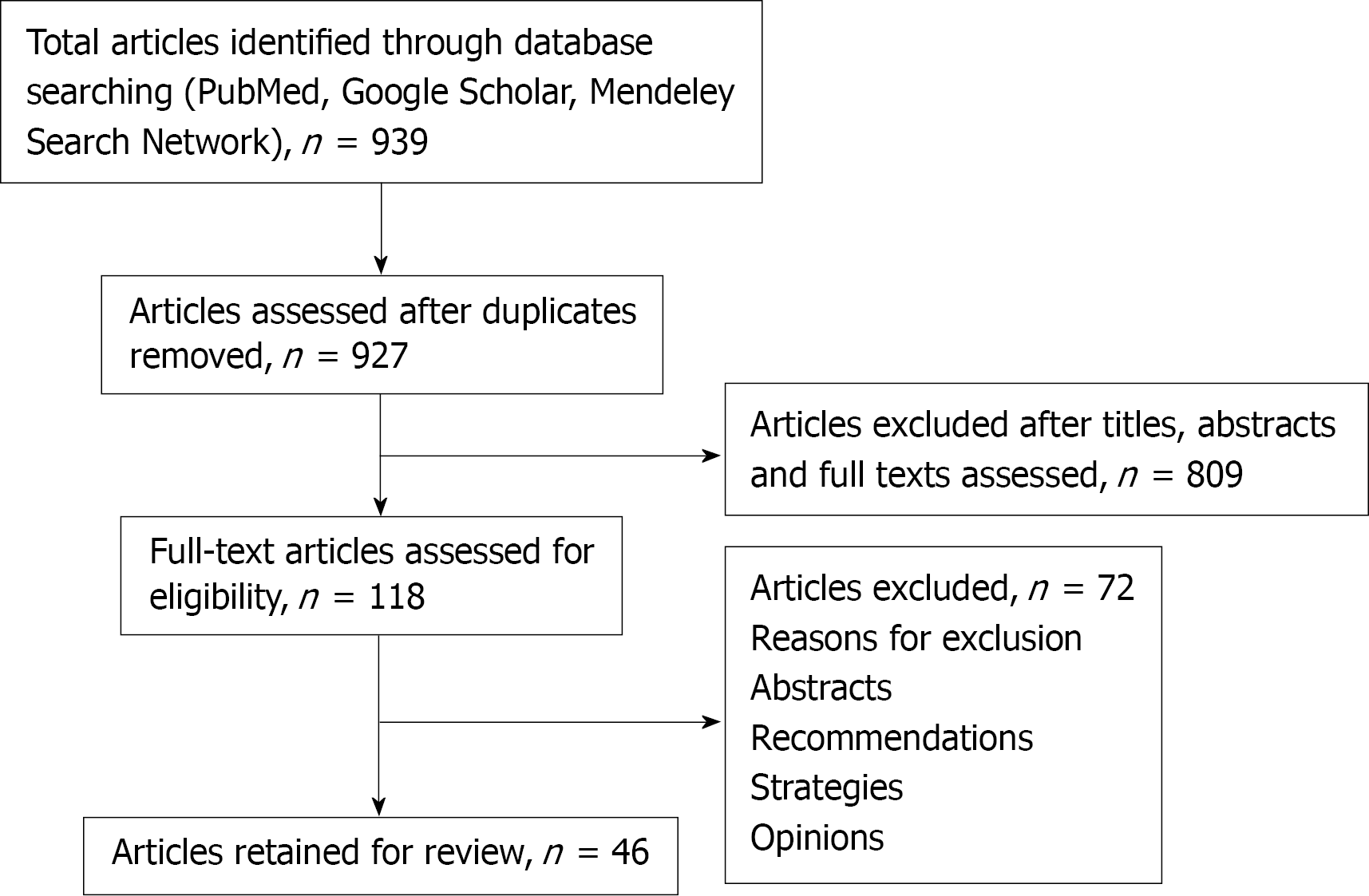
We selected all related articles regarding the morbidity and mortality of surgical pediatric patients during the SARS-CoV-2 pandemic by searching PubMed, Google Scholar, and Mendeley search network (www.mendeley.com) from January 1, 2020 to June 23, 2021. The search terms “COVID-19 and pediatric surgery” or “SARS-CoV-2 and pediatric surgery” or “COVID-19 and pediatric surgery and morbidity” or “SARS-CoV-2 and pediatric surgery and morbidity” or “COVID-19 and pediatric surgery and mortality” or “SARS-CoV-2 and pediatric surgery and mortality” were used. Articles in full texts including reviews, original articles, case reports, case series, and letters to the Editor were screened without language restrictions. Abstracts, recommendations, strategies, and opinions were excluded.
A data-based search retrieved 939 articles from the period January 1, 2020 to June 23, 2021. After subtracting duplicates, out of the 809 articles that emerged, we assessed 118 manuscripts in full text and finally reviewed 46 studies (Figure 1). The details of these studies are described below and summarized in Table 1.
| Ref. | Journal | Patient number | SARS-CoV-2 test | Disease | Treatment | Outcome | Study details |
| Place R et al[14] | JAMA Network Open 2020; 3: e2027948 | 90 | N/A | CAA: 35CAA + abscess: 8 | OT: 35; Abscess drainage with IA: 8 | Successful | Retrospective study. The authors noted increased number of CAA compared with the same period in 2019 |
| Kvasnovsky CL et al[15] | J Pediatr Surg 2020(Epub head of print) | 55 | Positive: 3 (without symptoms) | NOT: 25 (2 with CAA); OT: 30 (CAA: 13, Simple AA:17) | NOT: 25 pts (3 CAA); OT: 30 (13 CAA); 1 patient SARS-CoV-2+: OT; 2 patients SARS-CoV-2+: NOT | Successful | Retrospective study. 45.5% of all patients: NOT protocol to minimize operative resources; The majority of children (78.2%) did not meet previous criteria for non-admissions comparable to pre- SARS-CoV-2 era |
| Gerall CD et al[16] | J Pediatr Surg 2020 (Epub head of print) | 89 (41: pre SARS-CoV-2 era, 48: SARS-CoV-2) | Positive: 4 (excluded from the study) | UAA and CAA | NOT: Antibiotics 3 in the pre- SARS-CoV-2 era vs 7 during pandemic; OT: 33 in the pre- SARS-CoV-2 era vs 23 during pandemic | Successful | Retrospective study. It compares children’s’ symptoms and complications in pro- vs SARS-CoV-2 era. Patients in SARS-CoV-2 era: -Duration of symptoms: longer; -Increased number of imaging findings for perforation, increased LOS, increased time until resolution of symptoms. |
| Snapiri O et al[17] | Acta Pediatr 2020; 109: 1672-1676 | 7 | N/A | CAA (perforated, abscess) | OT: 4; NOT: 4 (abscess drainage) | Successful | Retrospective study. Delayed diagnosis: Insufficient initial evaluation, telemedicine: 3, parental concerns) |
| Fisher JC et al[18] | Ann Surg 2020 (Epub head of print) | 57 patients SARS-CoV-2 era vs control: 1292 | Positive: 11/28 | CAA in the SARS-CoV-2 era: 45% vs 27% in the control group | OT: UAA: 30; CAA: 20; NOT: 7 | Successful | Retrospective study. Comparison of clinical characteristics of children vs pre- SARS-CoV-2 era. Main findings: Higher duration of symptoms and perforation rates in the SARS-CoV-2 era. No differences between perforation rates and LOS among positive or negative SARS-CoV-2 children. |
| La Pergola F et al[19] | Front Pediatr 2020; 8: 600320 | 86 vs 309 in the pre- SARS-CoV-2 era | Positive: 3 | UAA: 59; CAA: 27 | N/A | Successful | Retrospective study. COVID-19 era vs previously (2017-2019); -No differences: in the prevalence of the AA, duration of symptoms and CAA |
| Raffaele A et al[20] | Br J Surg 2020; 107: e529-e530 | 14 | Positive: None | UCC: 7; CAA: 7l | OT: 13/14; NOT: 1 (abscess drainage) | Successful | Retrospective study. -Delayed presentation in the ED vs previous years, delayed admission to OT due to COVID-19 test preoperatively |
| Montalva L et al[21] | Pediatr Surg Int 2020; 36: 1397-1406 | 108 (69 during lockdown) | Positive: 3 | UAA: 24; CAA: 84 | OT: UAA and CAA with peritonitis:94; CAA with abscess: 14 (drainage or medical treated) | Successful | Retrospective cohort study. The authors found increased cases of AA during the period of lockdown compared to pre-lockdown era. LOS, complication rates, re-admissions and peritoneal abscesses similar |
| Bellini T et al[22] | Acta Pediatr 2021 (Epub head of print) | 27 in the SARS-CoV-2-era vs 75 control group | Positive: None | UAA: 14; CAA: 13 vs UAA: 50; CAA: 25 | N/A | Successful | Retrospective study. CAA cases significantly more when compared with previous 3 yr due to delayed admissions (P = 0.004) |
| Zampieri N et al[23] | Minerva Pediatr 2020; | N/A | N/A | N/A | N/A | N/A | Retrospective study. The authors found decreased number cases of AA during lockdown vs post-lockdown period (P < 0.05) possibly due to the less exposure to co-factors |
| Velayos M et al[24] | Ann Pediatr (Barc) 2020; 93: 118-122 | Pre- SARS-CoV-2-era: 41; Post- SARS-CoV-2: 25 | Positive: 1 | CAA: -pre- SARS-CoV-2: 3; -post- SARS-CoV-2: 8 | OT: All patients | Successful | Retrospective study. Increased number of CAA in SARS-CoV-2 era compared to pre- SARS-CoV-2 era due to delayed diagnosis (P = 0.019), LOS increased in the CAA SARS-CoV-2 group |
| Malhotra A et al[25] | Pediatr Inf Dis J 2021; 40: e49-e55 | 10 | Positive: 10 | CAA+MIS-C-: 5; UAA: 5 | OT: 8; NOT: 2 | Successful | Retrospective study. CAA associated with MIS-C |
| Cai et al[26] | Front Pediatr 2020;8: 1-9 | 5 | Positive: 5 | 1 patient: CAA + MIS-C | OT | Successful | Retrospective study. CAA associated with MIS-C |
| Schäfer FM et al[27] | Front Pediatr 2021; 9: 683607 | 514 | N/A | CAA | |||
| Zvizdic Z et al[28] | J Pediatr Surg 2021; 56: 196-200 | 6 | Positive: None | AA | OT | Successful | Letter to the Editor. Decreased admissions of AA compared to pre- SARS-CoV-2 era. Hypothesis: Correlation with decreased exposure to microbes due to lockdown |
| Lishman J et al[29] | J Pediatr Infect Dis 2020; 39: e472-e473 | 4 | Positive: 4 | UAA: 4; CAA: 2; MIS-C: 3 | OT: 3 | Successful | Case series. AA with MIS-C |
| Meyer JS et al[30] | J Pediatr Surg Case Rep 2021; 64: 101734 | 4 | Positive: All | UAA: 2; CAA: 2 | OT: 4 | Successful | Case series. Possible association of SARS-CoV-2 with AA |
| Lee-Archer P et al[31] | J Pediatr Child Health 2020; 56: 1313-1314 | 48 | N/A | UAA: 25; CAA: 23 | OT | Successful | Brief communication. Increased number of CAA compared to previous years (2014-2019), parental concerns |
| Wang H et al[32] | Chin J Pediatr Surg 2020; 41: 299-302 | 1 | Positive | UAA +; pneumonia | OT | Case report. UUA associated with pneumonia of the right lung | |
| Harwood R[33] | J Surg Case Rep 2020; 9: 1-3 | 2 | Positive: 1 | CAA + MIS-C | OT | Successful | Case report. CAA associated with MIS-C |
| Shahbaznejad L[34] | BMC Pediatrics 2020; 513 | 10 | Positive: 10 | 1 patient: UAA with MIS-C | OT | Successful | Case report. UAA associated with MIS-C |
| Alsuwallem AB et al[35] | Cureus 2020; 12: e8677 | 1 | Positive | CAA | OT | Successful | Case report. CAA associated with COVID-19 Infection |
| Mehl SC et al[36] | Pediatr Infect Dis J 2021 | 1 | Positive | NEC | NOT | Successful | Case report. Full term neonate with NEC secondary to SARS-CoV-2 infection |
| Rohani P et al[37] | J Pediatr Surg Case Rep 2021; 61: 101667 | 1 | Positive | NEC | NOT | Successful | Case report. Gastrointestinal SARS-CoV-2 manifestation |
| Moazzam Z et al[38] | J Pediatr Surg Case Reports 2020; 59:101533 | 1 | Positive | Intussusception | Pneumatic reduction | Successful | Case report. Gastrointestinal manifestation of SARS-CoV-2 |
| Rajalakshmi L et al[39] | Indian J Pract Pediatr 2020; 22:236 | 1 | Positive | Intussusception | Pneumatic reduction | Successful | Case report. Gastrointestinal manifestation of SARS-CoV-2 |
| Martinez-Castañoi[40] | Pediatr Emerg Care 2020;36: e368 | 1 | Positive | Intussusception | Hydrostatic reduction | Successful | Case report. Gastrointestinal manifestation of COVID-19 |
| Makrinioti H et al[41] | J Pediatric Infect Dis Soc 2020; 9: 504-506 | 2 | Positive: 2 | Intussusception; Intussusception + malrotation | Pneumatic reduction; Surgical reduction + ladd procedure | Death; Successful | Case reports. Fatal gastrointestinal manifestation of SARS-CoV-2; Gastrointestinal manifestation of SARS-CoV-2 |
| Bazuaye-Ekhuyasi EA et al[42] | Emerg Radiol 2020; 27: 761-764 | 1 | Positive | Intussusception | Hydrostatic reduction | Successful | Case report. Gastrointestinal manifestation of SARS-CoV-2 |
| Guerrón N et al[43] | Global Pediatr Health 2021; 8: 1-3 | 1 | Positive | Intussusception | Hydrostatic reduction | Successful | Case report. Gastrrointestinal manifestation of COVID-19 |
| Osorno JF et al[44] | Global Pediatr Health 2021; 8: 1-3 | 1 | Positive | Intussusception (delayed presentation) | Laparotomy | Successful | Case report. Gastrrointestinal manifestation of COVID-19 |
| Kawalec AM[45] | Burns 2020; 46: 1713-1714 | Increased admissions in ED compared to previous year | N/A | Increased TBSA burns, house fire burns and PICU admissions vs previous year | Outpatient care, hospitalization, PICU | N/A | Retrospective study. Need for a family plan during pandemic |
| Demicran M[46] | Burns 2020 (Epub ahead of print) | Increased admissions and hospitalizations compared to previous year | N/A | Increased TBSA burns, increased all kinds of burns | Outpatient care, hospitalization | N/A | Retrospective study. Burn care material must be ready |
| Sethuraman U[47] | Burns 2020 (Epub head of print) | Increased admissions in ED vs all visits | N/A | Increased TBSA | Outpatient care, hospitalization, PICU | 1 death | Retrospective study. Parents should keep children away from hot liquids and surfaces |
| Pelizzo G et al[48] | Healthcare 2021; 9: 551 | 84 (pandemic era: 52previous pre-pandemic period: 32) | Positive: 1 | TBSA < 10%: 32; 10%-15%: 11; > 15% >: 9 | 34/52: Discharge; 18/52: Burn Service Area; (10/18: Ward; 8/18: PICU) | Successful | Retrospective study. A higher number of admissions during pandemic was noticed compared to the same period in the previous year. An appropriate planned service and care ensure a safe and feasible hospitalization without risks of infections and major complications |
| Marino-Mateo L et al[49] | Actas UrolEsp 2020; 44: 659-654 | 45 | Positive: 0 | Pelviureteric junction obstruction, spina bifida, lithiasis, hypospadias | 49 interventions | Successful | Retrospective study. A stratification of the urological based on the different phases of pandemic and EAU was conducted |
| Cesaro S et al[50] | Pediatr Blood Cancer 2020; 67: e8466 | 247 | Positives: 10 | Solid tumors, leukemia | Ceased chemotherapy and radiation for 12-26 d | Successful | Retrospective study. Mild or asymptomatic patients with positive tests may continue therapy |
| Hrusak O et al[51] | Eur J Cancer 2020;132: 11-16 | 200 | Positives: 9 | Hepatoblastoma: 2; Wilms tumor: 1; Ewing’s sarcoma: 1; osteosarcoma: 1; cervical rhabdoid: 1; ALL: 1 | Antibiotics and/or hydroxychoroquine, lopinavir, ritonavir | Successful | Retrospective study. Children on anticancer therapy may have mild or asymptomatic course of infection with SARS-CoV-2. In this case anticancer treatment should not be delayed or postponed |
| Madhusiidhan PP et al[52] | Pediatr Blood Cancer 2020; e28843 | 578 | Positive: 98; No symptoms: 73 | Neuroblastoma: 5,Solid tumor: 16; Others: 77 | Mechanical; ventilation: 7; Supplemental oxygen: 25; SARS-CoV-2 direct treatment: 98 | Successful: 94; Death: 4 | Multi-institutional cohort study. Low morbidity and mortality among oncologic patients but higher than in general pediatrics. Significant impact of pandemic: Delay in therapy in 67% of positive patients; Overall delays: Chemotherapy 54%, surgery 46%, transplant 30% |
The literature search revealed 24 articles[14-35] concerning the influence of SARS-CoV-2 in children with acute appendicitis (AA). More specifically, we found 14 retrospective studies[14-27], one letter to the editor[28], two case series[29,30], one brief communication[31], and four case reports[32-35]. In many series[17,20,24], the diagnosis of AA was delayed for various reasons, such as fear of contact with SARS-CoV-2 patients, telemedicine, fear of traveling, and disruption of the local health system; this led to an increase in the number of cases with complicated AA (CAA). While an association between AA and SARS-CoV-2 has been speculated[26], other studies have also reported 13 children with CAA diagnosed in the context of MIS-C[29,33,34]. It is worth noting that one case reported the coexistence of AA and pneu
Two children aged 7 wk and 6 years respectively, both positive for SARS-CoV-2 infection, presented with clinical signs of acute abdomen. The clinical and diagnostic investigation showed necrotizing enterocolitis (NEC), which was successfully treated with antibiotics. The authors considered infection to be responsible for this emergency clinical manifestation[36,37].
Seven articles[38-44] referred to cases of ileocolic intussusception. Eight infants, aged 4-10 mo, presented with clinical symptoms related to intussusception (abdominal cramps, bilious vomiting, currant jelly stools) and were confirmed by ultrasound. On admission, seven infants were found to be positive for SARS-CoV-2, and one was found to be positive on the third postoperative day; four[38,40-42] had relatives with suspected or confirmed SARS-CoV-2 infection. Reduction (pneumatic or hydrostatic) was attempted in seven patients, six of whom had a successful outcome. Only two cases were treated surgically. Notably, in one case, at laparotomy, malrotation was found in addition to intussusception, and a Ladd’s procedure was performed[41]. In the other case, intestinal resection with consequent ileostomy and mucous fistula was performed due to intestinal ischemia and peritonitis[44]. Moreover, following successful pneumatic reduction of intussusception, one female infant with docu
A total of four articles was extracted for SARS-CoV-2 in children with burns[45-48]. All of them disclosed useful information. Specifically, they recorded an increase in admissions of children with moderate and severe fire-related burns in comparison to earlier years, while the greater difference in burned total body surface area was statistically significant[46-48].
One article from Spain was included[49] that reported clinical and surgical data, complications, and readmissions of all children who underwent procedures for various urological conditions. The authors developed an escalation program based on the different phases of the pandemic and the European Association of Urology recommendations. They concluded that this strategy allowed them to manage successfully urological diseases.
Three studies[50-52] that screened pediatric oncology/hematology patients for SARS-CoV-2 infection were evaluated. In the first study, 334 nasopharyngeal swabs were taken from 247 patients, only 10 (4%) of whom tested positive for SARS-CoV-2 infection (eight patients were asymptomatic and two had a mild fever). In nine patients, chemotherapy was postponed until they had tested negative (time period ranges from 12-26 d), while only one patient on chemotherapy and radiation was positive after 30 d[50]. In a multicenter survey performed in 25 countries involving 200 suspected patients, only nine tested positive for SARS-CoV-2 infection[51]. Notably, none required admission to pediatric intensive care or mechanical ventilation. Finally, a retrospective, multicenter study among 13 institutions including 578 patients examined test-positive SARS-CoV-2 patients aged ≤ 21 years receiving active anticancer treatment[52]. Among those 578 patients, 98 (16.95%) were positive, 78 (79.6%) of whom were symptomatic, and four died (4%). Delay of anticancer therapy occurred in 67% of these patients. Overall, these studies raised the question concerning the benefits of discontinuing or delaying chemotherapy in mild or asymptomatic SARS-CoV-2 positive patients.
This study provides descriptive data on pediatric surgical patients infected with the novel coronavirus SARS-CoV-2. The data show that the impact of SARS-CoV-2 seems to be multifactorial as it interferes directly with human health due to the vulnerability of the virus and indirectly with the resources to access care, thereby increasing morbidity and mortality[12].
SARS-CoV-2 infection can affect all ages of children with median age of infection of 6.7 years (1 d to 15 years)[53], with no gender predominance[54]. The angiotensin-converting enzyme 2 is the main host receptor of SARS-CoV-2 and is frequently expressed in ciliated epithelial cells in human lungs. The second most common site of angiotensin-converting enzyme 2 receptors is the gastrointestinal cells[53]. Notwithstanding, gastrointestinal symptoms attributed to SARS-CoV-2 infection are more prevalent in children, while respiratory involvement is more common in adults[55,56]. In line with this finding, Meyer et al[30] speculated a conceivable association of SARS-CoV-2 and AA based on the assumption of the predominant association of gastrointestinal infection and SARS-CoV-2. However, in the era of SARS-CoV-2, other factors such as the fear of contact with persons positive for SARS-CoV-2, difficulty in visiting health centers, and insufficient evaluation via telemedicine may constitute strong reasons for delayed diagnosis of CAA[17,20,24].
The predominant association of gastrointestinal infection and SARS-CoV-2 might also explain the cases of intussusception[38-44] and the two cases of NEC[36,37]. Intussusception is the most common cause of intestinal obstruction in infancy[57]. Although in most cases it is thought to be idiopathic, a preceding viral infection due to adenovirus and rotavirus has been reported in approximately 30% of cases[58]. Notably, all cases described here were positive for SARS-CoV-2 infection, while a previous history of upper respiratory tract infection was diagnosed in three cases[38-40]. In the two cases of NEC, the association of SARS-CoV-2 test positivity with coexistence of pneumatosis intestinalis and bloody stools suggests ischemic necrosis in both cases and hence NEC[36,37].
The increase in the number of children presenting with burns during the outbreak could be ascribed to the fact that the lockdown obliged children to stay home where they may have had less surveillance, since parents were constrained to work from home and were thus unable to keep a close watch on children. Educational programs are needed to increase parents’ knowledge concerning safety behaviors during a prolonged stay at home[45-48].
The impact of SARS-CoV-2 outbreak on children with urological problems is not known. An escalation program based on different phases of the pandemic has been proposed by Merino-Mateo et al[49] for the management of urological problems. However, the lengthy postponement of certain crucial surgical procedures, such as cryptorchidism, or obstructive uropathies including ureteropelvic junction obstruction, ureterovesical junction obstruction, or neurogenic bladder may lead to loss of a testicle function or loss of renal function. Three articles referred to testicular torsion[59-61]. The conclusions were contradictory, as increased rate of orchidectomies was noticed in the two articles due to delayed presentation[59,60], while in the remaining one article the authors found early presentation in testicular torsion and no differences in rates of orchidectomies between SARS-CoV-2 period and preceding era[61].
Children with cancer face significant health problems in view of the rapid changes in the health system and restrictions in accessing medical support. Compromised immunity due to malignancy and the unknown behavior of SARS-CoV-2 lead to further insecurity. Although the studies mentioned above[54-56] did not show significant consequences from the virus itself, it was clear that postponement of therapies owing to the heavily burdened health system could result in insufficient medical support.
In May 2020, the Centers for Disease Control in the United States expressed concern for a new entity termed MIS-C associated with SARS-CoV-2[34,62]. MIS-C is defined by clinically severe illness requiring hospitalization that presents with fever, elevated inflammatory markers, and multisystem organ dysfunction in the setting of recent proven or probable SARS-CoV-2 infection and the absence of a plausible alternative explanation[34]. However, there are no data available as to whether the mechanism that can lead to severe respiratory failure resembles that of MIS-C. Current data raise the suspicion for a distinct entity related to severe SARS-CoV-2 infection[62]. MIS-C-related AA was suspected in three studies[25,33,34] in which the coexistence of CAA and positive was tested.
This study is not without its limitations inasmuch as it is based on all types of articles, most of which included retrospective studies, letters to the Editor, case reports, and case series, all of which were written during the pandemic within a short period of time in an effort to share experiences and divulge information that could help the scientific community. Furthermore, in order to achieve a better understanding, a substantial number of studies compared their results with those to pre- SARS-CoV-2 era, which can lead to a significant bias. Another limitation is that most data were collected within 204 mo. Consequently, there is a lack of acceptable follow-up that would have helped us gain precise knowledge as concerns post
Pediatric surgical practice during the SARS-CoV-2 pandemic is challenging. Summarizing the information and results of studies, we conclude that SARS-CoV-2 infection could have a negative influence on virtually the entire pediatric surgical spectrum. Morbidity has increased for various reasons in children with burns, urological problems, and cancer including fear of contracting the virus in health centers, lockdown, telemedicine, postponement of medical consultation and elective surgeries, or unknown manifestations of SARS-CoV-2. Under normal circumstances, mortality could have been minimized. The delay in presentation and consequent management of AA has resulted in an increased number of CAA. The impact of SARS-CoV-2 on the gastrointestinal system has further exacerbated the manifestation of common pediatric surgical conditions such as AA, intussusception, and NEC. Further studies and research are needed to overcome the demands of this period.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Pediatrics
Country/Territory of origin: Greece
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Fei C, Morenikeji OB S-Editor: Wu YXJ L-Editor: Filipodia P-Editor: Wu YXJ
| 1. | Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, Liu L, Shan H, Lei CL, Hui DSC, Du B, Li LJ, Zeng G, Yuen KY, Chen RC, Tang CL, Wang T, Chen PY, Xiang J, Li SY, Wang JL, Liang ZJ, Peng YX, Wei L, Liu Y, Hu YH, Peng P, Wang JM, Liu JY, Chen Z, Li G, Zheng ZJ, Qiu SQ, Luo J, Ye CJ, Zhu SY, Zhong NS; China Medical Treatment Expert Group for Covid-19. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382:1708-1720. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19202] [Cited by in RCA: 18850] [Article Influence: 3770.0] [Reference Citation Analysis (7)] |
| 2. | Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020;91:157-160. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2616] [Reference Citation Analysis (0)] |
| 3. | COVID 19 coronovirus pandemic. Last updated: June 23, 2021; 10: 37 GMTwww.worldometers.info. |
| 4. | Han E, Tan MMJ, Turk E, Sridhar D, Leung GM, Shibuya K, Asgari N, Oh J, García-Basteiro AL, Hanefeld J, Cook AR, Hsu LY, Teo YY, Heymann D, Clark H, McKee M, Legido-Quigley H. Lessons learnt from easing COVID-19 restrictions: an analysis of countries and regions in Asia Pacific and Europe. Lancet. 2020;396:1525-1534. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 5. | Rusch VW, Wexner SD; American College of Surgeons COVID-19 Communications Committee, Board of Regents, and Officers. The American College of Surgeons Responds to COVID-19. J Am Coll Surg. 2020;231:490-496. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 6. | Turner AM, Albolino S, Morabito A. Paediatric surgery and COVID-19: urgent lessons to be learned. Int J Qual Health Care. 2021;33:mzaa149. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Quaedackers JSLT, Stein R, Bhatt N, Dogan HS, Hoen L, Nijman RJM, Radmayr C, Silay MS, Tekgul S, Bogaert G. Clinical and surgical consequences of the COVID-19 pandemic for patients with pediatric urological problems: Statement of the EAU guidelines panel for paediatric urology, March 30 2020. J Pediatr Urol. 2020;16:284-287. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 32] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 8. | de Agustín Asensio JC. Pediatric Surgery during the SARS-CoV-2 pandemic. Cir Pediatr. 2020;33:153. [PubMed] |
| 9. | Royal College of Paediatrics and Child Health. National guidance for the recovery of elective surgery in children. Online July 17, 2020. Available from: https://www.afpp.org.uk. |
| 10. | DeFazio JR, Kahan A, Fallon EM, Griggs C, Kabagambe S, Zitsman J, Middlesworth W, Stylianos S, Duron V. Development of pediatric surgical decision-making guidelines for COVID-19 in a New York City children's hospital. J Pediatr Surg. 2020;55:1427-1430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 11. | Wei Y, Yu C, Zhao TX, Lin T, Dawei HE, Wu SD, Wei GH. The impact of the COVID-19 pandemic on pediatric operations: a retrospective study of Chinese children. Ital J Pediatr. 2020;46:155. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 12. | Ogundele IO, Alakaloko FM, Nwokoro CC, Ameh EA. Early impact of COVID-19 pandemic on paediatric surgical practice in Nigeria: a national survey of paediatric surgeons. BMJ Paediatr Open. 2020;4:e000732. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 13. | Tullie L, Ford K, Bisharat M, Watson T, Thakkar H, Mullassery D, Giuliani S, Blackburn S, Cross K, De Coppi P, Curry J. Gastrointestinal features in children with COVID-19: an observation of varied presentation in eight children. Lancet Child Adolesc Health. 2020;4:e19-e20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 14. | Place R, Lee J, Howell J. Rate of Pediatric Appendiceal Perforation at a Children's Hospital During the COVID-19 Pandemic Compared With the Previous Year. JAMA Netw Open. 2020;3:e2027948. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 47] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 15. | Kvasnovsky CL, Shi Y, Rich BS, Glick RD, Soffer SZ, Lipskar AM, Dolgin S, Bagrodia N, Hong A, Prince JM, James DE, Sathya C. Limiting hospital resources for acute appendicitis in children: Lessons learned from the U.S. epicenter of the COVID-19 pandemic. J Pediatr Surg. 2021;56:900-904. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 16. | Gerall CD, DeFazio JR, Kahan AM, Fan W, Fallon EM, Middlesworth W, Stylianos S, Zitsman JL, Kadenhe-Chiweshe AV, Spigland NA, Griggs CL, Kabagambe SK, Apfel G, Fenster DB, Duron VP. Delayed presentation and sub-optimal outcomes of pediatric patients with acute appendicitis during the COVID-19 pandemic. J Pediatr Surg. 2021;56:905-910. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 17. | Snapiri O, Rosenberg Danziger C, Krause I, Kravarusic D, Yulevich A, Balla U, Bilavsky E. Delayed diagnosis of paediatric appendicitis during the COVID-19 pandemic. Acta Paediatr. 2020;109:1672-1676. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 103] [Cited by in RCA: 128] [Article Influence: 25.6] [Reference Citation Analysis (0)] |
| 18. | Fisher JC, Tomita SS, Ginsburg HB, Gordon A, Walker D, Kuenzler KA. Increase in Pediatric Perforated Appendicitis in the New York City Metropolitan Region at the Epicenter of the COVID-19 Outbreak. Ann Surg. 2021;273:410-415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 19. | La Pergola E, Sgrò A, Rebosio F, Vavassori D, Fava G, Codrich D, Montanaro B, Leva E, Schleef J, Cheli M, Pelizzo G, Gamba P, Alberti D, Betalli P. Appendicitis in Children in a Large Italian COVID-19 Pandemic Area. Front Pediatr. 2020;9 8:600320. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 32] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 20. | Raffaele A, Cervone A, Ruffoli M, Cereda E, Avolio L, Parigi GB, Riccipetitoni G. Critical factors conditioning the management of appendicitis in children during COVID-19 Pandemic: experience from the outbreak area of Lombardy, Italy. Br J Surg. 2020;107:e529-e530. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 21. | Montalva L, Haffreingue A, Ali L, Clariot S, Julien-Marsollier F, Ghoneimi AE, Peycelon M, Bonnard A. The role of a pediatric tertiary care center in avoiding collateral damage for children with acute appendicitis during the COVID-19 outbreak. Pediatr Surg Int. 2020;36:1397-1405. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 22. | Bellini T, Rotulo GA, Carlucci M, Fiorenza V, Piccotti E, Mattioli G. Complicated appendicitis due to diagnosis delay during lockdown period in Italy. Acta Paediatr. 2021;110:1959-1960. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 23. | Zampieri N, Cinquetti M, Murri V, Camoglio FS. Incidence of appendicitis during SARS-CoV-2 pandemic quarantine: report of a single area experience. Minerva Pediatr. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 24. | Velayos M, Muñoz-Serrano AJ, Estefanía-Fernández K, Sarmiento Caldas MC, Moratilla Lapeña L, López-Santamaría M, López-Gutiérrez JC. [Influence of the coronavirus 2 (SARS-Cov-2) pandemic on acute appendicitis]. Ann Pediatr (Engl Ed). 2020;93:118-122. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 36] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 25. | Malhotra A, Sturgill M, Whitley-Williams P, Lee YH, Esochaghi C, Rajasekhar H, Olson B, Gaur S. Pediatric COVID-19 and Appendicitis: A Gut Reaction to SARS-CoV-2? Pediatr Infect Dis J. 2021;40:e49-e55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 43] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 26. | Cai X, Ma Y, Li S, Chen Y, Rong Z, Li W. Clinical Characteristics of 5 COVID-19 Cases With Non-respiratory Symptoms as the First Manifestation in Children. Front Pediatr. 2020;8:258. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 68] [Cited by in RCA: 67] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 27. | Schäfer FM, Meyer J, Kellnar S, Warmbrunn J, Schuster T, Simon S, Meyer T, Platzer J, Hubertus J, Seitz ST, Knorr C, Stehr M. Increased Incidence of Perforated Appendicitis in Children During COVID-19 Pandemic in a Bavarian Multi-Center Study. Front Pediatr. 2021;9:683607. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 28. | Zvizdic Z, Vranic S. Decreased number of acute appendicitis cases in pediatric population during the COVID-19 pandemic: Any link? J Pediatr Surg. 2021;56: 199-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 29. | Lishman J, Kohler C, de Vos C, van der Zalm MM, Itana J, Redfern A, Smit L, Rabie H. Acute Appendicitis in Multisystem Inflammatory Syndrome in Children With COVID-19. Pediatr Infect Dis J. 2020;39:e472-e473. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 45] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 30. | Meyer JS, Robinson G, Moonah S, Levin D, McGahren E, Herring K, Poulter M, Waggoner-Fountain L, Shirley DA. Acute appendicitis in four children with SARS-CoV-2 infection. J Pediatr Surg Case Rep. 2021;64:101734. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 23] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 31. | Lee-Archer P, Blackall S, Campbell L, Boyd D, Patel B, McBride C. Increased incidence of complicated acute appendicitis during the COVID-19 pandemic. J Pediatr Child Health 2020; 56:1313-1314. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 43] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 32. | Wang H, Duan X, Yan X, Sun R, Liu X, Ji S. One case of novel coronavirus pneumonia complicated with acute appendicitis in children. Chin J Pediatr Surg. 2020;41: 299-302. [DOI] [Full Text] |
| 33. | Harwood R, Partridge R, Minford J, Almond S. Paediatric abdominal pain in the time of COVID-19: a new diagnostic dilemma. J Surg Case Rep. 2020;2020:rjaa337. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 34. | Shahbaznejad L, Navaeifar R, Abbakshanian A, Hosseinzadeh A, Rehimzadeh G, Rezai MS. Clinical characteristics of 10 children with a pediatric inflammatory multisystem syndrome associated with COVID-19 syndrome. BMC Pediatrics. 2020;20: 513. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 33] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 35. | Alsuwailem AB, Turkistani R, Alomari M. Complicated Appendicitis in a Pediatric Patient With COVID-19: A Case Report. Cureus. 2020;12:e8677. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 36. | Mehl SC, Whitlock RS, Marcano DC, Rialon KL, Arrington AS, Naik-Mathuria B. Necrotizing Enterocolitis-like Pneumatosis Intestinalis in an Infant With COVID-19. Pediatr Infect Dis J. 2021;40:e85-e86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 37. | Rohani P, Karimi A, Tabatabaie SR, Khalili M, Sayyari A. Protein losing enteropathy and pneumatosis intestinalis in a child with COVID 19 infection. J Pediatr Surg Case Rep. 2021;64:101667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 38. | Moazzam Z, Salim A, Ashraf A, Jehan F, Arshad M. Intussusception in an infant as a manifestation of COVID-19. J Pediatr Surg Case Rep. 2020;59:101533. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 39] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 39. | Rajalakshmi L, Satish S, Nandhini G, Ezhilarasi S. Unusual presentation of COVID-19 intussusception. J Pract Pediatr. 2020;22:236-238. |
| 40. | Martínez-Castaño I, Calabuig-Barbero E, Gonzálvez-Piñera J, López-Ayala JM. COVID-19 Infection Is a Diagnostic Challenge in Infants With Ileocecal Intussusception. Pediatr Emerg Care. 2020;36:e368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 41. | Makrinioti H, MacDonald A, Lu X, Wallace S, Jobson M, Zhang F, Shao J, Bretherton J, Mehmood T, Eyre E, Wong A, Pakkiri L, Saxena A, Wong G. Intussusception in 2 Children With Severe Acute Respiratory Syndrome Coronavirus-2 Infection. J Pediatric Infect Dis Soc. 2020;9:504-506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 42. | Bazuaye-Ekwuyasi EA, Camacho AC, Saenz Rios F, Torck A, Choi WJ, Aigbivbalu EE, Mehdi MQ, Shelton KJ, Radhakrishnan GL, Radhakrishnan RS, Swischuk LE. Intussusception in a child with COVID-19 in the USA. Emerg Radiol. 2020;27:761-764. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 43. | Guerrón N, Figueroa LM. Intussusception and COVID19, Successful Mechanic Reduction, Case Report. Glob Pediatr Health. 2021;8:2333794X211019693. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 44. | Osorno JF, Giraldo M, Marín AF, Figueroa LM. Novel Coronavirus Infection in an Infant with Intussusception. Glob Pediatr Health. 2021;8:2333794X211012978. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (1)] |
| 45. | Kawalec AM. The changes in the number of patients admissions due to burns in Paediatric Trauma Centre in Wroclaw (Poland) in March 2020. Burns. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 46. | Demircan M. Increased admissions and hospitalizations to pediatric burn center during COVID 19 pandemic. Burns. 2021;47:487-488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 22] [Reference Citation Analysis (0)] |
| 47. | Sethuraman U, Stankovic C, Singer A, Vitale L, Krouse CB, Cloutier D, Donoghue L, Klein J, Kannikeswaran N. Burn visits to a pediatric burn center during the COVID-19 pandemic and 'Stay at home' period. Burns. 2021;47:491-492. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 29] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 48. | Pelizzo G, Vestri E, Del Re G, Filisetti C, Osti M, Camporesi A, Rizzo D, De Angelis A, Zoia E, Tommasi P, Zuccotti G, Calcaterra V. Supporting the Regional Network for Children with Burn Injuries in a Pediatric Referral Hospital for COVID-19. Healthcare (Basel). 2021;9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 49. | Merino-Mateo L, Tordable Ojeda C, Cabezalí Barbancho D, Gómez Fraile A. Impact of the COVID-19 pandemic on the surgical activity of Pediatric Urology: analysis of postoperative complications according to the Clavien-Dindo classification. Actas Urol Esp (Engl Ed). 2020;44:659-664. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 50. | Cesaro S, Compagno F, Zama D, Meneghello L, Giurici N, Soncini E, Onofrillo D, Mercolini F, Mura R, Perruccio K, De Santis R, Colombini A, Barone A, Sainati L, Baretta V, Petris MG. Screening for SARS-CoV-2 infection in pediatric oncology patients during the epidemic peak in Italy. Pediatr Blood Cancer. 2020;67:e28466. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 51. | Hrusak O, Kalina T, Wolf J, Balduzzi A, Provenzi M, Rizzari C, Rives S, Del Pozo Carlavilla M, Alonso MEV, Domínguez-Pinilla N, Bourquin JP, Schmiegelow K, Attarbaschi A, Grillner P, Mellgren K, van der Werff Ten Bosch J, Pieters R, Brozou T, Borkhardt A, Escherich G, Lauten M, Stanulla M, Smith O, Yeoh AEJ, Elitzur S, Vora A, Li CK, Ariffin H, Kolenova A, Dallapozza L, Farah R, Lazic J, Manabe A, Styczynski J, Kovacs G, Ottoffy G, Felice MS, Buldini B, Conter V, Stary J, Schrappe M. Flash survey on severe acute respiratory syndrome coronavirus-2 infections in paediatric patients on anticancer treatment. Eur J Cancer. 2020;132:11-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 52. | Madhusoodhan PP, Pierro J, Musante J, Kothari P, Gampel B, Appel B, Levy A, Tal A, Hogan L, Sharma A, Feinberg S, Kahn A, Pinchinat A, Bhatla T, Glasser CL, Satwani P, Raetz EA, Onel K, Carroll WL. Characterization of COVID-19 disease in pediatric oncology patients: The New York-New Jersey regional experience. Pediatr Blood Cancer. 2021;68:e28843. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 81] [Article Influence: 20.3] [Reference Citation Analysis (0)] |
| 53. | Weston S, Frieman MB. COVID-19: Knowns, Unknowns, and Questions. mSphere. 2020;5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 104] [Cited by in RCA: 92] [Article Influence: 18.4] [Reference Citation Analysis (0)] |
| 54. | Lu X, Zhang L, Du H, Zhang J, Li YY, Qu J, Zhang W, Wang Y, Bao S, Li Y, Wu C, Liu H, Liu D, Shao J, Peng X, Yang Y, Liu Z, Xiang Y, Zhang F, Silva RM, Pinkerton KE, Shen K, Xiao H, Xu S, Wong GWK; Chinese Pediatric Novel Coronavirus Study Team. SARS-CoV-2 Infection in Children. N Engl J Med. 2020;382:1663-1665. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1629] [Cited by in RCA: 1703] [Article Influence: 340.6] [Reference Citation Analysis (0)] |
| 55. | Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, Schiergens TS, Herrler G, Wu NH, Nitsche A, Müller MA, Drosten C, Pöhlmann S. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell. 2020;181:271-280.e8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11946] [Cited by in RCA: 14234] [Article Influence: 2846.8] [Reference Citation Analysis (0)] |
| 56. | Bourgonje AR, Abdulle AE, Timens W, Hillebrands JL, Navis GJ, Gordinjn SJ, Bolling MC. Dijkstra G, Voors AA, Osterhaus AD, van der Voort PH, Mulder DJ, van Goor H. Angiotensin –converting enzyme 2 (ACES2), SARS-CoV-2 and the pathophysiology of coronavirus disease 2019 (COVID-19). J Pathol 2020; 251: 228-248. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 661] [Cited by in RCA: 736] [Article Influence: 147.2] [Reference Citation Analysis (0)] |
| 57. | Jiang J, Jiang B, Parashar U, Ngugen T, Bines J Patel MM. Childhood intussusception in children. PloS One 2013; 8: 1-14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 141] [Cited by in RCA: 187] [Article Influence: 15.6] [Reference Citation Analysis (1)] |
| 58. | Marsicovetere P, Ivatury SJ, White B, Holubar SD. Intestinal Intussusception: Etiology, Diagnosis, and Treatment. Clin Colon Rectal Surg. 2017;30:30-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 190] [Article Influence: 21.1] [Reference Citation Analysis (0)] |
| 59. | Pogorelić Z, Milanović K, Veršić AB, Pasini M, Divković D, Pavlović O, Lučev J, Žufić V. Is there an increased incidence of orchiectomy in pediatric patients with acute testicular torsion during COVID-19 pandemic? J Pediatr Urol. 2021;17:479.e1-479.e6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 35] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 60. | Holzman SA, Ahn JJ, Baker Z, Chuang KW, Copp HL, Davidson J, Davis-Dao CA, Ewing E, Ko J, Lee V, Macaraeg A, Nicassio L, Sadighian M, Stephany HA, Sturm R, Swords K, Wang P, Wehbi EJ, Khoury AE; Western Pediatric Urology Consortium (WPUC). A multicenter study of acute testicular torsion in the time of COVID-19. J Pediatr Urol. 2021;17:478.e1-478.e6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 61. | Littman AR, Janssen KM, Tong L, Wu H, Wang MD, Blum E, Kirsch AJ. Did COVID-19 Affect Time to Presentation in the Setting of Pediatric Testicular Torsion? Pediatr Emerg Care. 2021;37:123-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 62. | CDC. Multisystem inflammatory syndrome in children (MIS-C) associated with coronavirus disease 2019 (COVID- 19). [cited 25 August 2020]. Available from: https://emergency.cdc.gov/han/2020/han00432.asp. |