Published online Jan 20, 2022. doi: 10.5662/wjm.v12.i1.1
Peer-review started: January 15, 2021
First decision: October 17, 2021
Revised: October 25, 2021
Accepted: December 11, 2021
Article in press: December 11, 2021
Published online: January 20, 2022
Processing time: 368 Days and 18.3 Hours
Al-Halabi is an intriguing ophthalmologist who invented numerous surgical instruments for treating various eye diseases. The illustrations of such instru
Core Tip: Medieval Islamic ophthalmological instruments are a rich, complex, and understudied subject. This topic is interesting and deserves more attention than it has had. The book of Al-Halabi is indeed one of the interesting books on ophthalmology written in Arabic. The ophthalmological instruments included in Al-Halabi’s table represent an untold story about the contributions of Muslim and Arab scholars in the field of ophthalmology. The aim of the present article is to fill in one of the gaps to some extent in biomedical engineering history. The ophthalmological instruments represent the biomechanics field.
- Citation: Saad MN. Ophthalmological instruments of Al-Halabi fill in a gap in the biomedical engineering history. World J Methodol 2022; 12(1): 1-19
- URL: https://www.wjgnet.com/2222-0682/full/v12/i1/1.htm
- DOI: https://dx.doi.org/10.5662/wjm.v12.i1.1
Studying the biomedical engineering history has greatly influenced the creative and inventive sense of biomedical engineering students[1]. Biomedical technologies have a very long history, among which are the ancient surgical instruments[2]. Bronze age epilation forceps were found in Ur, Iraq. The forceps, used in the treatment of trachoma, date back to ca. 2600 BC[3]. Other epilation forceps were discovered in tombs of the New Kingdom of Egypt (1570-1070 BC). Moreover, pots containing copper, zinc oxide, lead, and antimony sulphates were uncovered at the same tombs. These pigments were utilized for treating conjunctivitis[4]. It is argued that the first “book” on medicine in the world which is a medical papyrus (1553-1550 BC) was discovered in Luxor (Thebes), Egypt, in 1872 by the German archeologist Georg Ebers (1837-1898). In the eye treatment section, the only surgical procedure mentioned in the papyrus that has survived was applying to the eyelid onions, myrrh, gazelle excrement, and blood from lizards or bats after epilation through the use of feathers of a vulture[3].
Furthermore, in Egypt, several surgical needles could be seen carved in stone from the relief on the internal facade of the second wall in Kom Ombo Temple, constructed during the Ptolemaic dynasty (180-47 BC). Moreover, W.M. Flinders Petrie (1853-1942) (English Egyptologist) has discovered a series of ancient cooper needles with no hooks or apertures in King Khasekhemwy’s tomb (ca. 2690 BC) in the Royal Necropolis at Abydos, Upper Egypt, in 1900. These needles represent the earliest known ancient surgical instruments for dislodging the cataract away from the pupil[5]. These needles could be found in the National Museums in Liverpool, England[6].
Hippocrates (Greek physician d. 370 BC) recommended using wool rounded around a wooden rod soaked in a caustic solution for scraping the eyelids when treating trachoma. Celsus (Roman encyclopaedist d. 50 AD) included in the medical work of his encyclopedia the recommendation of using a hook, a threaded needle, and a scalpel in the treatment of pterygium. Galen (Greek physician d. 210 AD) utilized a cuttlefish bone for roughness in treating trachoma and as an agent to dissolve pterygium. Aëtius of Amida (Byzantine Greek physician, mid-5th century to mid-6th century) applied a blunt hook, a tiny hook, a horse-hair and linen thread through a needle, and a knife in the treatment of pterygium[7]. Numerous gaps exist in the biomedical engineering history, one of which the present article aims to fill in through providing an overview of Al-Halabi’s contributions.
Al-Halabi (middle of the 13th century)[8,9] - whose full name was Khalifah ibn Abi Al-Mahasin Al-Halabi[10] and who was known as Khalifa Ben Abi Al-Mahassin[11], Khalifa ibn Abi Al-Mahasen Al-Halabi[12], Halifa B Abi L-Mahasin[13], and Halifa[14] for short - was named after Aleppo (Arabic: Halab), a city in the northern part of Syria, known for its thriving trades and wealth in the middle ages before the Mongol onslaught (in 1260 AD)[11]. It was mostly where he was born and died[15,16]. He mentioned two incidents that happened to him in Aleppo in 1252 and 1254 AD (650 and 652 AH)[11,15]. Aleppo was, as it has been for centuries, an important city and the capital of a principality[17]. It appears that Al-Halabi must have had a wide spectrum of knowledge about medical sciences as can be derived from the list of references that he cited. He was considered the first ophthalmologist to use a magnet in order to remove metallic foreign body from the eye by Wafai and Kalaji as well as Hirschberg, as he extracted a couching needle that was broken in a patient’s eye during the surgery[14-16,18]. He realized that an instrument may be substituted by another because of unavailability[15].
The Sufficient Knowledge in Ophthalmology (Arabic: Kitab Al-Kafi fi Al-Kuhl), expected to be written within the period from 1256 to 1275 AD, is the only known book by Al-Halabi[11,13,14]. It is one of the masterpieces of Islamic ophthalmological medicine and surgery. The book’s scientific value is incomparable to European manuscripts till the beginning of the nineteenth century[14]. The book describes in a separate chapter the measurements, weights, and sizes used at that time by physicians. It quotes 73 authors and 41 books before its time[9,18]. He referenced famous Arabian or Muslim authors such as Al-Razi, Ibn Sina (Avicenna), Al-Tabari, Hunayn ibn Ishaq, Al-Ghafiqi, Ibn Zuhr (Avenzoar), and Al-Zahrawi; Greeks such as Galen, Hippocrates, and Oribasius; and Indians[15,16].
The two copies of the book are to be found in the Bibliotheque Nationale in Paris, France (under the number 1043d. Arabe), and the Süleymaniye Kütüphanesi in Istanbul, Turkey (under the number Yeni Jami 924). The Paris manuscript was written by the Christian copyist Abd Al-Aziz ibn Abi Saeed Al-Masihi Al-Mawsili Al-Mutatabbeb in 1277 AD, meaning that it is very close to the time of the author. The Istanbul manuscript was written by the Muslim copyist Ahmad Al-Wali in 1560 AD, meaning that the manuscript was written around 300 years after the death of the author[15].
The book was disappointingly ignored until the French medical historian Lucien Leclerc (1816-1893) had described it briefly for the first time in 1876 in his book “Histoire de la Médecine Arabe”[19]. In 1905, the German ophthalmologist and historian Julius Hirschberg (1843-1925) with the orientalists J. Lippert (1839-1909) and E. Mittwoch (1876-1942) wrote a book entitled “Arabian Ophthalmologists” in which they studied the book with great detail[15,16,20].
The present article depends basically on the reproduction of Al-Halabi’s book edited by M. Z. Wafai and M. R. Kalaji. They produced Al-Halabi’s book within the combined series “The Islamic Heritage in Ophthalmology” in which they unearthed the Islamic glorious heritage and its valuable knowledge that served humanity for over thirteen centuries. They compared the two copies of the book (in Paris and Istanbul) and put in the text the most accurate words. They explained in the footnotes some words that could contain more than one meaning. They gave the modern names of the diseases that Al-Halabi described. The book was published by the Islamic Educational, Scientific and Cultural Organization, Rabat, Morocco in 1990[15].
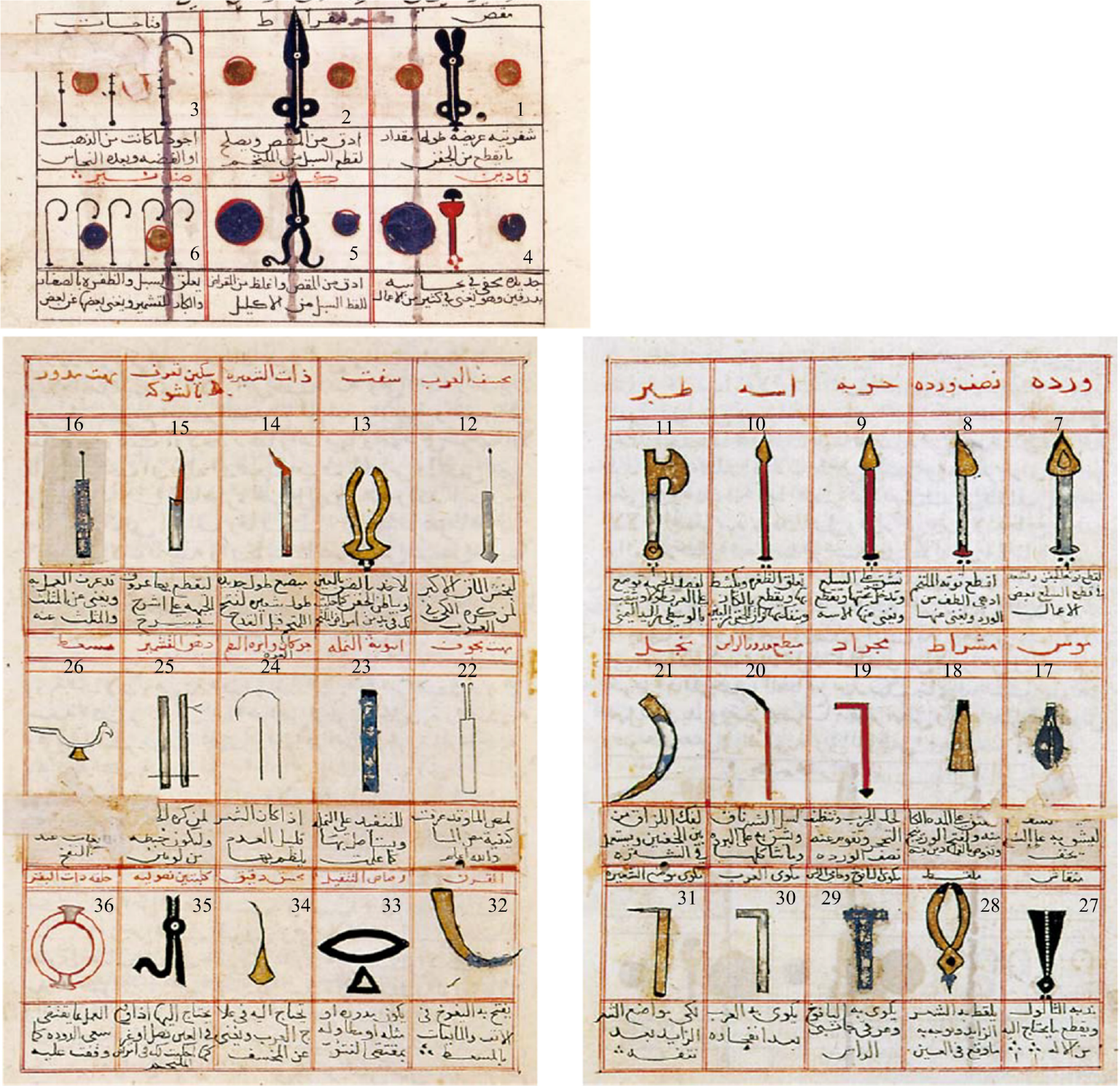
Al-Halabi’s book is the first book to place thirty-six surgical instruments in a very elegant table[9,21]. This table is considered to be well organized as each surgical instrument was placed in a special frame with the name of the instrument on the top and the way to use it underneath it, as shown in Figure 1[16,22]. This was the first time that an author put a table for the surgical instruments, unlike his predecessors who used to put the drawing of the instrument within the text[15].
Some of these instruments were known and used by earlier Arabic ophthalmologists, and a few authors also included illustrations of the instruments, but none was as comprehensively or as systematically as Al-Halabi[18]. For example, Al-Razi (d. 925 AD) recommended the rose leaf needle (No. 7 in Figure 1) for scraping off the chronic trachoma. Moreover, Al-Razi used hooks (No. 6 in Figure 1) to lift thick pannus, which was then excised with scissors[23]. Al-Zahrawi (d. 1013 AD) used spear (No. 9 in Figure 1) to treat symblepharon[24]. Al-Ghafiqi (d. 1165 AD) used drill (No. 12 in Figure 1) and small drill (No. 34 in Figure 1) in dacryocystorhinostomy[25]. Ammar ibn Ali Al-Mawsili (d. 1010 AD) invented a hollowed aspirating needle (No. 22 in Figure 1) for cataract surgery[26]. Ibn Al-Nafis (d. 1288 AD)[27] used the scalpel (No. 4 in Figure 1) or the rose leaf needle for scraping the eyelid in trachoma surgery. Besides, Ibn Al-Nafis used speculums (No. 3 in Figure 1), scissors (No. 2 in Figure 1), and hooks in the treatment of pannus. Furthermore, Ibn Al-Nafis applied the rounded couching needle (No. 16 in Figure 1) to penetrate pterygium and strip it away from the conjunctiva and cornea[28].
It is worth mentioning that Al-Halabi used the instruments with other diseases other than what he mentioned in the instruments table. So, for all the instruments discussed in the current article, the statements of use on the table itself were given first and then supplemented with other uses given elsewhere in his treatise (with page numbers given for those), as could be seen in Table 1. These instruments were as functional as the seventy-six instruments invented by the Austrian ophthalmic surgeon Wilhelm Czermak (1856-1906) as considered by Hirschberg[14].
| Instrument name | No. in Figure 1 | Uses in his table | Other uses in his book with page numbers in reference[15] given |
| Scissors | 1 | Distichiasis | |
| Scissors | 2 | Pannus | Concretions (p.121, p.276); Ectropion (p.278); Stye (p.279); Distichiasis (p.282); Hordeolum (p.287); Hemangioma at the eyelid (p.287); Wart (p.289); Lacrimal caruncle swelling (p.291); Pterygium (p.293); Hemangioma at the conjunctiva (p.297); Iris prolapse (p.299); Superficial temporal artery (p.300) |
| Speculums | 3 | Only description | Pannus (p.295) |
| Scissors | 5 | Pannus, pterygium (a note with the myrtle leaf needle) | Granuloma at the conjunctiva (p.297) |
| Hooks | 6 | Pannus, pterygium, distichiasis | Symblepharon (p.277); Ectropion (p.278); Distichiasis (p.281); Hemangioma at the eyelid (p.287); Sebaceous cyst (p.290); Lacrimal caruncle swelling (p.291); Hemangioma at the conjunctiva (p.297); Granuloma at the conjunctiva (p.297); Superficial temporal artery (p.300) |
| Rose leaf needle | 7 | Hemangioma at the eyelid, sebaceous cyst, hemangioma at the conjunctiva (a note with the half rose leaf needle) | Trachoma (p.275); Symblepharon (p.277); Lagophthalmos (p.123, p.278); Ectropion (p.278); Wart (p.289) |
| Half rose leaf needle | 8 | Hemangioma at the conjunctiva, (Trachoma, concretions) (a note with the scraper) | Adhesions between the two eyelids (p.277) |
| Spear | 9 | Sebaceous cyst | Symblepharon (p.277); Ectropion (p.278) |
| Myrtle leaf needle | 10 | Pterygium, symblepharon, sebaceous cyst (a note with the spear) | |
| Axe | 11 | Bloodletting the supraorbital vein | |
| Drill | 12 | Dacryocystitis | |
| Raven’s beak | 13 | Removing whatever sticks to the eye or the inner side of the eyelid | Conjunctival wound (p.213) |
| Lancet | 14 | Cataract | |
| Rounded couching needle | 16 | Could be substituted by the triangular needle | Pannus (p.295); Hemangioma at the conjunctiva (p.297); Cataract (p.305) |
| Scalpel | 18 | Hypopyon, chemosis | Adhesions between the two eyelids (p.277); Allergic dermatitis (p.288) |
| Scraper | 19 | Trachoma, concretions | |
| Lancet | 20 | Lipoma, chalazion | Concretions (p.276); Chemosis (p.285); Blepharitis (p.289); Hypopyon (p.298); Superficial temporal artery (p.300); Cataract (p.307) |
| Sickle | 21 | Adhesions between the two eyelids, ectropion | |
| Hollowed aspirating needle | 22 | Cataract | |
| Gooseneck speculum and tailor’s needle | 24 | Distichiasis | |
| Gatherer | 27 | Wart | ‘Foreign body’ fallen into the eye (p.215), Stye (p.279), Hordeolum (p.287), |
| Gatherer | 28 | Distichiasis, ‘foreign body’ fallen into the eye | |
| Cautery | 29 | Supraorbital vein, superficial temporal veins | Superficial temporal artery (pp.300-301) |
| Cautery | 30 | Dacryocystitis | |
| Cautery | 31 | Distichiasis | |
| Small drill | 34 | Dacryocystitis | |
| Awn-tongs | 35 | ‘Foreign body’ fallen into the eye |
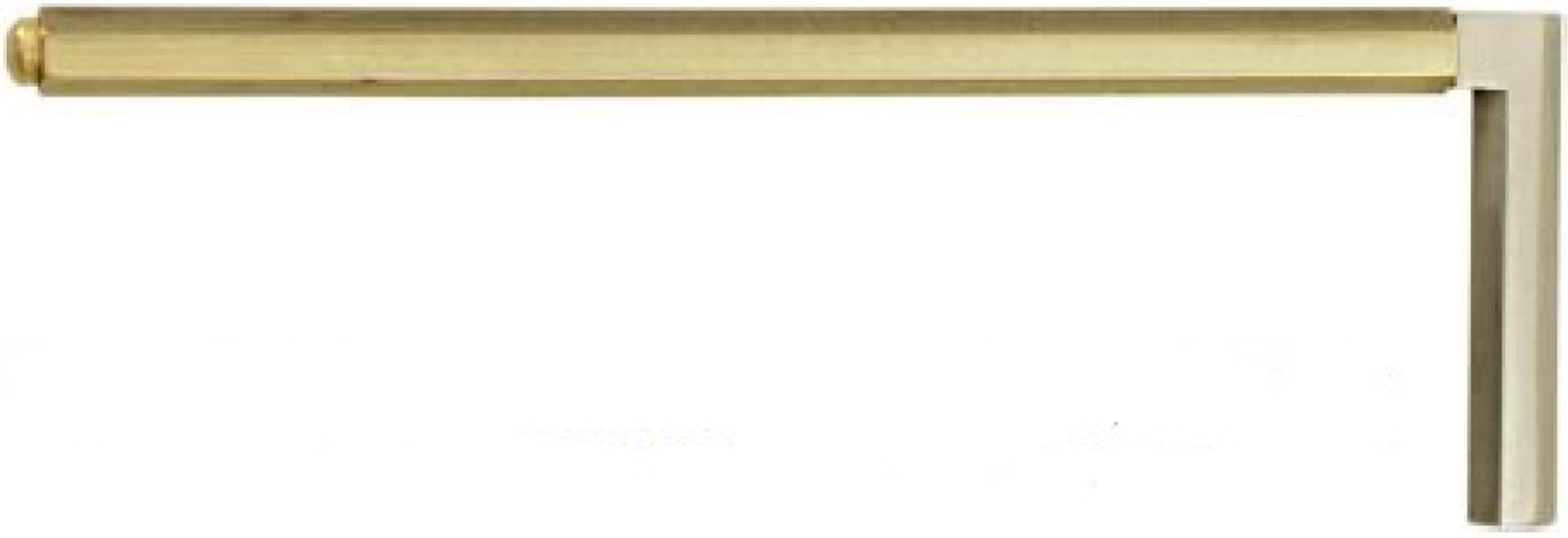
Al-Halabi utilized a needle in the treatment of trachoma (called granular conjunctivitis or Egyptian ophthalmia, which is a contagious, chronic inflammation of the mucous membranes of the eyes, caused by Chlamydia trachomatis; it is characterized by swelling of the eyelids, sensitivity to light, and eventual scarring of the conjunctivae and corneas of the eyes). The patient was lied down and Al-Halabi stayed beside the diseased eye. A nurse stayed beside Al-Halabi for handing him the required surgical instrument. The shape of the tip of the needle resembled the rose leaf with a small, short, pointed end, as illustrated in Figure 2[22]. He started stripping the scabies by the needle from the medial canthus to the lateral canthus. He noted that the ophthalmologist should preserve mildness and tranquility to prevent eye damage. As an alternative to the needle, a scraper can be used. It looks like a right-angled bolt extra
Moreover, Al-Halabi used the rose leaf needle when treating lagophthalmos (a condition in which a complete closure of the eyelids over the eyeball is difficult or impossible). If lagophthalmos was a result of a healed ulcer or a strained suture of a wound leading to eyelid attraction, the rose leaf needle was used to incise the place of the healed ulcer or the strained suture. Then, a piece of cotton was inserted at the place of the incision[15].
He used a lancet in order to remove chalazion (a cyst that appears on the eyelid because of a blocked meibomian gland)[8]. If medications did not heal chalazion, an incision should be applied to it. If the chalazion was at the upper eyelid, it should be extended downwards. If the chalazion was at the lower eyelid, it should be extended upwards. At this point, a horizontal incision was applied to the chalazion through the use of a lancet with a rounded tip (Figure 4) in order to cleave the chalazion[22]. If the chalazion was inclined to the outer side of the eyelid, the incision should be applied on the outer side of the eyelid, and vice versa. Finally, the chalazion should be removed using a spoon[15,29].
The lancet as well could be used in the treatment of chemosis (abnormal edematous swelling of the mucous membrane covering the eyeball and lining the eyelids) and lipoma (benign fatty tumor occurring at the inner side of the upper eyelid between its layers). In case of lipoma, Al-Halabi warned the ophthalmologists that they should be cautious of the penetration of the eyelid leading to the puncture of the tarsal cartilage of the eyelid, and a perforated cornea and iris. Furthermore, the lancet could be used in the incision of blepharitis (inflammation of the eye glands and eyelash follicles along the margin of the eyelids).
The same lancet was applied for removing the concretions (small, separated tumors at the inner side of the eyelid). A horizontal deep incision was conducted through the use of the lancet for digging out the stone formations. Besides, the scraper could be used as a substitution for the lancet. Al-Halabi mentioned that the ophthalmologist should be careful while using either the lancet or the scraper to prevent the pene
Al-Halabi used a tool that resembles to some extent an extremely small sickle (see Figure 6) in the treatment of the adhesions between the two eyelids[22]. If the two eyelids were closely adhered, a small incision should be performed using a fine scalpel (instrument number 18 in Figure 1) or a needle at the origins of the eyelashes to let the tip of the sickle be introduced between the two eyelids. The shape of the tip of the needle resembles half the rose leaf (instrument number 8 in Figure 1). He started opening the incision from the direction of the medial canthus towards the lateral canthus[15].
If the adhesions were between the eyelid and the conjunctiva or the cornea (symblepharon), two hooks were utilized for holding up the eyelid. If the adhesions were at the upper eyelid, it should be extended upwards. If the adhesions were at the lower eyelid, it should be extended downwards. Al-Halabi used the rose leaf needle to separate the adhesions. He stated that the ophthalmologist should use delicacy when the adhesions were between the eyelid and the conjunctiva. A tremendous delicacy should be applied when the adhesions were between the eyelid and the cornea in order to prevent making punctures in the corneal layers. These punctures could cause iris prolapse (protrusion of the iris or part of the iris through an injury in the cornea).
When the adhesions are closer to the bones of the eyebrow, it is harder to separate them, and a longer tool should be used like the needle or the spear. The shape of the tip of the needle resembles the myrtle leaf with a small, long pointed end appropriate for cleaving the adhesions, as presented in Figure 7[22]. The spear has a big long pointed end, as shown in Figure 8, and could replace the myrtle leaf needle[15,22].
Al-Halabi used hooks (instrument number 6 in Figure 1), the spear, and the scissors (Miqrad) in the treatment of ectropion (eversion or turning outward of the margin of the eyelid). If the ectropion was due to the growth of a superfluous fleshy tissue on the inner side of the eyelid, two or three hooks were inserted in the fleshy tissue for holding up the eyelid. Then, the tip of the spear was inserted under the fleshy tissue to warn it off the eyelid skin. Finally, the scissors were utilized for dissecting the fleshy tissue. Al-Halabi pointed out that the ophthalmologist should use tremendous delicacy in order to prevent the laceration of the eyelid skin and its dissection with the fleshy tissue[15].
He used the scissors (Miqrad) and a gatherer for treating stye (inflammation of the sebaceous gland of an eyelash) or wart (small, benign growth caused by a viral infection of the skin). The gatherer which has two broad heads (instrument number 27 in Figure 1) was utilized for holding stye or wart from its middle and extending it away from the eyelid. Then, the scissors were used for cutting it out of its roots. In the case of the wart, the scissors could be replaced by a horse-tail hair. In order to saw off the wart, the horse-tail hair was placed under the gatherer[16]. Actually, a recent study indicated that the horse-tail hair is about 0.2 mm thick, and it recommended using it in ophthalmic surgeries[30].
In addition, the scissors and gatherer were utilized for eradicating hordeolum (suppurative inflammation of a gland of the eyelid). Furthermore, the scissors were used for uprooting the hemangioma at the eyelid (benign tumor found on the eyelid, composed of dilated blood vessels, and often encapsulated within a fibrous shell) with the aid of a hook. The rose leaf needle could substitute the scissors.
The rose leaf needle was used in sebaceous cyst removal. The function of the needle was to make a horizontal incision at the liquefied tissue. Then, a hook and the rose leaf needle were utilized for removing the pus. The spear was applied for a deeper, T-shaped incision when the inflamed area was bigger and deeper. The myrtle leaf needle could substitute the spear. Al-Halabi elucidated that the liquefied tissue should be completely removed in order to avoid the reappearance of the sebaceous cyst[15].
Al-Halabi used annexation technique in the treatment of distichiasis (congenital, abnormal, accessory row of eyelashes, often causing severe discomfort from contact with the eye). If the eyelashes number was from one to five, a very thin tailor’s needle could be used. A thread was twisted through the needle hole and around itself to make a buttonhole. Another thread was entered in the buttonhole to make it ready for annexation. The needle was applied at the margin of the eyelid from its inner side to the center of the distichiasis. The abnormal eyelashes were entered in the buttonhole with the aid of a tip of a gooseneck speculum (instrument number 24 in Figure 1). Then, the needle was pulled slowly and carefully to tighten the buttonhole on the eyelashes. Finally, the needle was extended quickly away of the eyelid, and the eyelashes were epilated at the middle of the buttonhole[15].
Another technique for treating distichiasis was the use of glue. If the abnormal eyelashes were long enough and their number was from one to five, they were pasted to the nearest normal eyelashes. The components of the glue are listed in Table 2[31,32]. First, the glue was placed on a plate made of bronze. Second, the glue was melted on a soft flame. He noted that the flame should be near the ophthalmologist and ready to be used in order to prevent the glue from cooling down while being used. Third, an eye stick or a tip of a hook was utilized for applying the glue on the misdirected eyelashes. Finally, these eyelashes were extended to allow them to paste to the normal eyelashes for preventing the irritation of the eyeball. If the glue reached undesired normal eyelashes, it was removed by rubbing[15].
| Common name | Scientific name | Arabic name | Effects |
| Mastic | Pistacia lentiscus | Mustaqy | Antiseptic, anti-inflammatory, analgesic, sedative |
| Sarcocolla | Astragalus Sarcocolla L | Aanzarout | Anthelmintic, emollient |
| Aloe | Aloe vera | Sabr | Wound healing, antimicrobial |
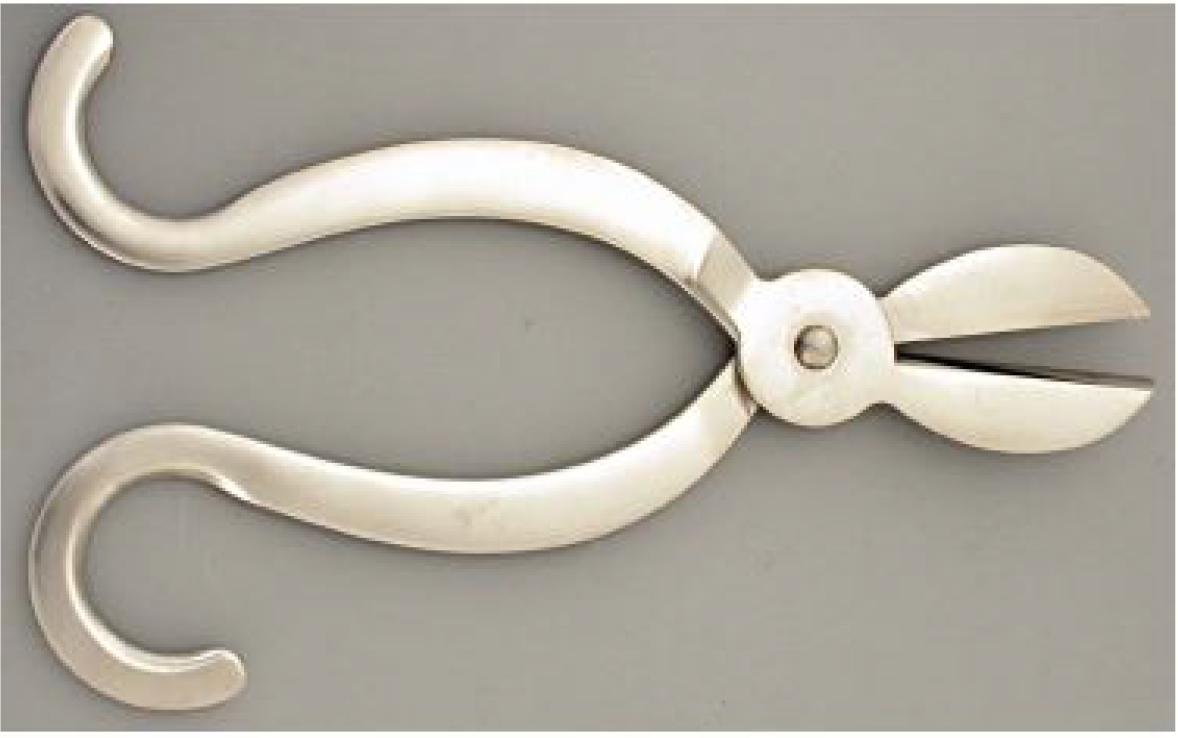
Moreover, distichiasis could be treated by cauterization. If the aberrant eyelashes number was from one to five despite being long or short, they should be plucked out first through the use of the gatherer. It could also be used in pulling out any “foreign body” that has fallen into the eye, as shown in Figure 9[22]. Then, a cautery was applied to the position of the pulled-out eyelashes. The cautery was pointed to be appropriate for the narrow places, as seen in Figure 10[22]. Al-Halabi preferred gold as a material of the cautery as the disease was cleared quickly and blisters did not appear at the cauterized position. When the eyelash was plucked out, the cautery was heated till its color turned red. Then, it was directed to the position of the pulled-out eyelashes. It should be slightly deeper to destroy the lash follicle[15].
In case of abnormal eyelashes number being more than five, their place on the eyelid should be cut using scissors. First, the eyelid was rolled up and incised at the location of the abnormal eyelashes from the medial canthus to the lateral canthus. A tailor’s needle and a thread were used to sew the incision. Then, Al-Halabi placed the amount of the eyelid’s skin between the two blades of the scissors. The scissors (Arabic: Miqass) (see Figure 11) should have two broad blades with their length equal to or more than the amount of the eyelid’s skin that should be removed[22]. He distinguished the Miqass scissors from the Miqrad scissors that the first type has thicker and longer blades than the second being appropriate for removing the amount of the eyelid’s skin in one cut[15].
Al-Halabi used a hook and scissors (Miqrad) in treating lacrimal caruncle swelling. The hook was utilized for hanging up the swelling. Then, the swelling was excised by the scissors. Finally, he warned the ophthalmologists that they should be cautious of the excision of a normal part of the lacrimal caruncle causing epiphora[15].
In case of dacryocystitis (congenital displacement of lacrimal tissue results in subconjunctival cysts), he placed a cautery that looks like a right-angled screwdriver, as shown in Figure 12[22]. Its shape is appropriate for the target with a smooth rounded tip contact. This cautery was used to cauterize the lacrimal gland fistula after its rupture until the vessels stop bleeding. He preferred gold as a material of the cautery. The cautery was heated till its color turns red. Then, it was directed to the position of the fistula till boiling. The cauterized position was wiped with a rag. Next, cauterization was repeated several times till the crust on the lacrimal bone was peeled. Finally, the cauterized position was cleaned from rot[15].
A drill was utilized in case the patient refused the cauterization solution. It consists of a handle and a long shaft with a small sharp pointed end, as seen in Figure 13[22]. It was used to clean the entire corner of the eye. In addition, a perforation was made at the tear-producing gland fistula in the nasal direction. A high strength should be applied until the blood flows from the nose and the mouth. Al-Halabi discussed that the perforation should not be directed upward as this would be the incorrect direction. Moreover, he noted that the ophthalmologist’s working hand should be inclined to the nose (not to the eye) in order to avoid damage to the eye layers. Through this, a smaller drill (instrument number 34 in Figure 1) was wrapped in cotton which should be dry or soaked in ox fat or in verdigris ointment (corrosive, anti-inflammatory effects). He pointed that the verdigris became less effective if used after a year of its manufacture date. This would then be exchanged every day until the cotton was extracted clean in order to reach the bone pureness. With some details, the opening of the wound should be widened through the use of the smaller drill, and the cotton should be exchanged as it is expected that the cotton would be extracted from the wound with small dirty fractures of the bone[15].
Al-Halabi used eye speculums, hooks, scissors (Miqrad), couching needle with a rounded tip, dove’s feather, and eye stick in the treatment of pannus (membrane of fine blood vessels and fibrous tissue that spreads down over the peripheral cornea in trachoma and other inflammatory corneal disorders causing loss of vision)[34]. The patient was lied down, and he stayed behind the patient. A sessile pillow was put under the patient’s head to make it slightly declined[15].
A tool, which looks somewhat like the eye speculum nowadays (instrument number 3 in Figure 1), was used to keep the patient’s diseased eye open. Al-Halabi expressed his preference of using two thumbs of a skilled nurse instead of two eye speculums. The disadvantage of using the eye speculums from Al-Halabi’s viewpoint was the obstruction of the eye speculums to the movement of the scissors (Miqrad) while cutting off the pannus. Three hooks were applied to hang up the pannus, one from the medial canthus, one from the center of the conjunctiva, and one from the lateral canthus. The hooks were applied near the upper eyelid[15].
A tip of the scissors (Miqrad) was utilized for cutting off a part of the membrane from the lateral canthus. Then, the couching needle was introduced to saw off the pannus. Al-Halabi recommended that the couching needle should be made of red bronze (instrument number 16 in Figure 1). A dove’s feather might substitute the couching needle. The Miqrad scissors were used again to pick out the membrane until reaching the medial canthus. At this part, the three hooks were applied near the lower eyelid, and the same procedure was repeated till the pannus was completely removed. He noted that the ophthalmologist should watch out the cornea while performing this procedure[15].
A tiny eye stick was wrapped in cotton which should be soaked in egg yolk and rose oil (calms painful sores and constricts and cools wounds). He recommended that the rose oil should not be used after two years of its manufacture date as it got expired. The eye stick should be applied at the middle of the eye and extended in the directions of the two eyelids in order to prevent any adhesions that might occur[15].
Al-Halabi described another way to get rid of the pannus. One hook was applied to hang up the pannus. The scissors (Arabic: Kaz) were used to make a cut in the mem
A third technique was elucidated by Al-Halabi for removing the pannus. Several hooks were used to hang up the pannus. The number of hooks ranged from six to twelve depending on the size of the eye. The insertion of the hooks started from the medial canthus near the upper eyelid and ended near the lower eyelid in a circular shape. A tip of the Miqrad scissors was used for cutting off a part of the membrane from the lateral canthus near the upper eyelid, and then near the lower eyelid. Then, the couching needle was introduced to saw off the pannus. At this point, the Kaz scissors were applied to make a circular incision in the membrane. The pannus would be extracted in a shape that looks like a signet ring[15].
Al-Halabi used a hook, a smooth dove’s feather, myrtle leaf needle, Miqrad scissors, and Kaz scissors in treating pterygium (a pink, fleshy tissue that grows on the conjunctiva)[33]. The hook was utilized for raising the pterygium from its center. If the pterygium loosely adhered to the conjunctiva, a smooth dove’s feather was inserted under the hook to saw off the pterygium. If the pterygium hardly adhered to the conjunctiva, two or three hooks could be added to the sides of the pterygium. Then, the myrtle leaf needle was used for sawing off the tissue. Finally, the Miqrad scissors or the Kaz scissors were used for cutting off the pterygium[15].
Al-Zahrawi used a horse-tail hair to saw off the pterygium. The dove’s feather and the horse-tail hair were utilized due to the inability of the technology of that era to manufacture a man-made instrument with the required thickness and sharpness[24]. Al-Halabi stated that the ophthalmologist should use extreme delicacy in order to avoid penetrating the cornea or the medial canthus. He asked the ophthalmologist to beware of the total removal of the pterygium to avoid its reappearance. Furthermore, he asked the ophthalmologist to take care of the adhesiveness of the pterygium with the conjunctiva. If the pterygium extremely adhered to the conjunctiva, the surgical instruments should not be applied at all in order to avoid eye damage[15].
Al-Halabi used a hook, a couching needle, the half of the rose leaf needle, and the Miqrad scissors in treating hemangioma at the conjunctiva. The hook was applied to raise up the hemangioma. He stated that the ophthalmologist should use tremendous delicacy while raising up the hemangioma because it has a spongy consistency, and the hook might turn up during the treatment. The couching needle was inserted under the blood vessels, and he started sawing off the hemangioma. The half of the rose leaf needle could replace the couching needle in sawing off the hemangioma. Finally, the scissors were utilized for uprooting the hemangioma[15].
Al-Halabi used a hook and the scissors (Kaz) in the treatment of granuloma at the conjunctiva (growth appearing like a nodule, consisting essentially of granulation tissue, and occurring as a result of localized inflammation). The hook was utilized for holding up the granuloma. If the size of the granuloma was large, two or three hooks should be applied. The Kaz scissors were applied to eradicate the granuloma[15].
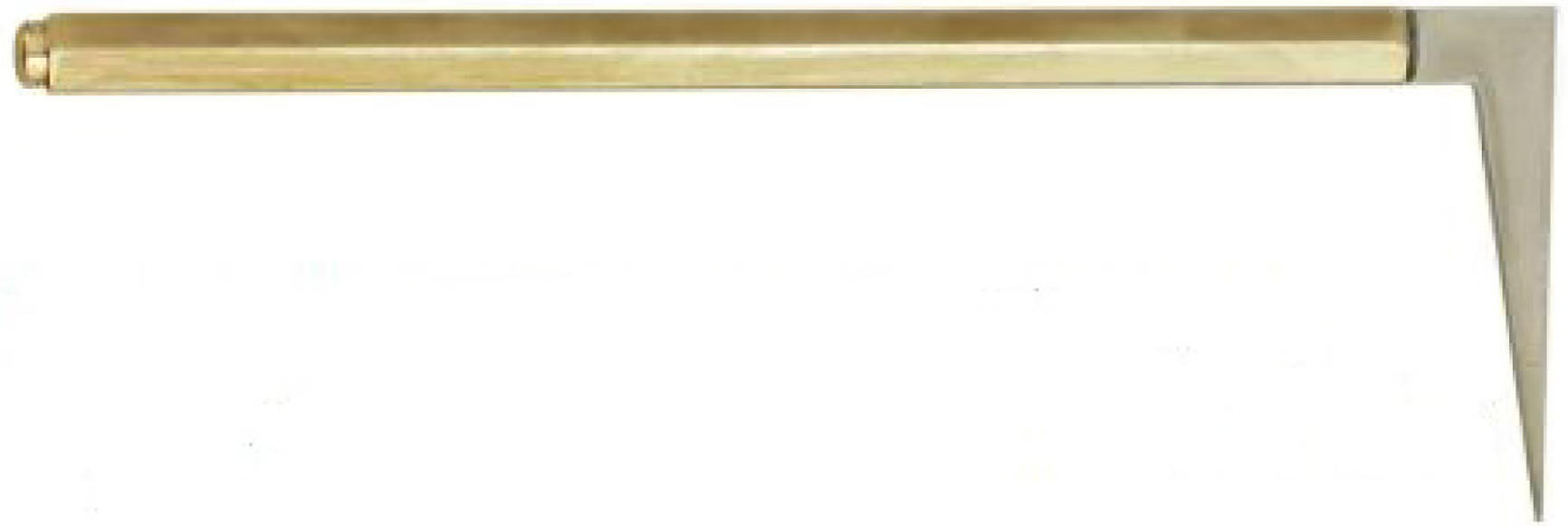
He used a Raven’s beak in the treatment of conjunctival wound (presence of wound or laceration of the conjunctiva with swelling and edema of the wound edges). The Raven’s beak is a slim gatherer with two heads, as displayed in Figure 15[22]. The Raven’s beak was used to extract an extremely small piece of wood that penetrated the eyeball and was fallen between the sclera and the eye bones. In addition, the Raven’s beak could be used for removing whatever sticks to the eye or the inner side of the eyelid. The awn-tongs (see Figure 16) were utilized when an awn (either a hair- or bristle-like appendage) or a similar object fell down into the eye[15,22].
Al-Halabi used a scalpel and a lancet in treating hypopyon (inflammatory cells in the anterior chamber of the eye). The scalpel was applied between the cornea and the conjunctiva to make an incision. He noted that the ophthalmologist should be cautious of the penetration of the iris. The lancet was applied at the position of the incision for the expulsion of the inflammatory cells. He used a needle, a thread, and scissors (Miqrad) in the treatment of the iris prolapse. A needle with a thread was inserted beneath the protrusion from the medial canthus and extracted from the lateral canthus. The two ends of the thread were drawn out of the eye. Then, the scissors were used to cleave the protrusion[15].
In case of pain in the temporal muscles, headache, and migraine due to eye diseases, Al-Halabi used scissors (Miqrad), a hook, a lancet, and a cautery in the bloodletting and cutting the superficial temporal arteries and the posterior auricular veins[13]. A cord was tightened around the patient’s throat with great mildness. Then, the patient was asked to throttle himself/herself with leniency. This procedure was conducted to make the arteries and the veins of the head visible and to target them. In case of the superficial temporal artery, he suggested shaving the temple, and spotting the artery with ink—this made the artery visible. After targeting the artery, the patient was asked to stop throttling himself/herself, and the cord was released to reduce the amount of the seepage blood while working[15].
Then, he attracted the skin over the artery using two fingers of his left hand. At this point, an incision was performed in the skin through the use of scissors (Miqrad). Consequently, the artery was extracted from its position and eradicated through the use of a hook’s tip. In case the artery was slim, a lancet was inserted under it to cut it off. Equally, the artery might be cut off using the scissors (Miqrad) instead of the lancet. In case the artery was thick, Al-Halabi used a needle and a thread made of silk or linen so that the artery would be tied in two places. Then, the lancet was utilized for opening an aperture between the two ligatures so that the desired amount of blood would flow out. After bloodletting, the artery was ligated and the blood flow was controlled[15].
Al-Halabi provided the cauterization by a flathead cautery instead of the eradication of the artery through the use of the lancet or the scissors. The same procedures were conducted for the posterior auricular vein except that the cautery was smaller than that for the superficial temporal artery. His usage of smaller cautery for the posterior auricular vein is in line with modern knowledge, as the thickness of the outer walls and the layers of muscle and elastic fibers of the veins is less than that of the arteries. As a disinfection procedure, he recommended the use of medical packs made of cotton after cauterization[15].
In case the previous procedures were unfruitful in treating migraine and headache, the supraorbital vein and the superficial temporal veins should be cauterized. First, the head was shaved from the middle of the scalp towards the forehead. Al-Halabi described how to know the position of the supraorbital vein in the forehead. The patient was asked to put the nail of his/her thumb of the right hand on the apex of the nose. Then, his/her forefinger was extended on the nasal septum towards the forehead. The maximum point the forefinger could reach was the position of the supraorbital vein. Next, this position was massaged using rough linen pack until it became red. At this point, a cautery was applied on the position longitudinally and horizontally in order to make a cross-shaped cauterization. The cautery looks like a fleshy olive and was made of iron, as shown in Figure 17[22]. The same procedures were performed on the superficial temporal veins. A knife that resembles to some extent an extremely small axe (see Figure 18) might replace the cautery for the supraorbital vein[22]. The knife was utilized for bloodletting the supraorbital vein. It was placed lengthwise on the vein, and the severing was conducted with the middle finger of the right hand[15].
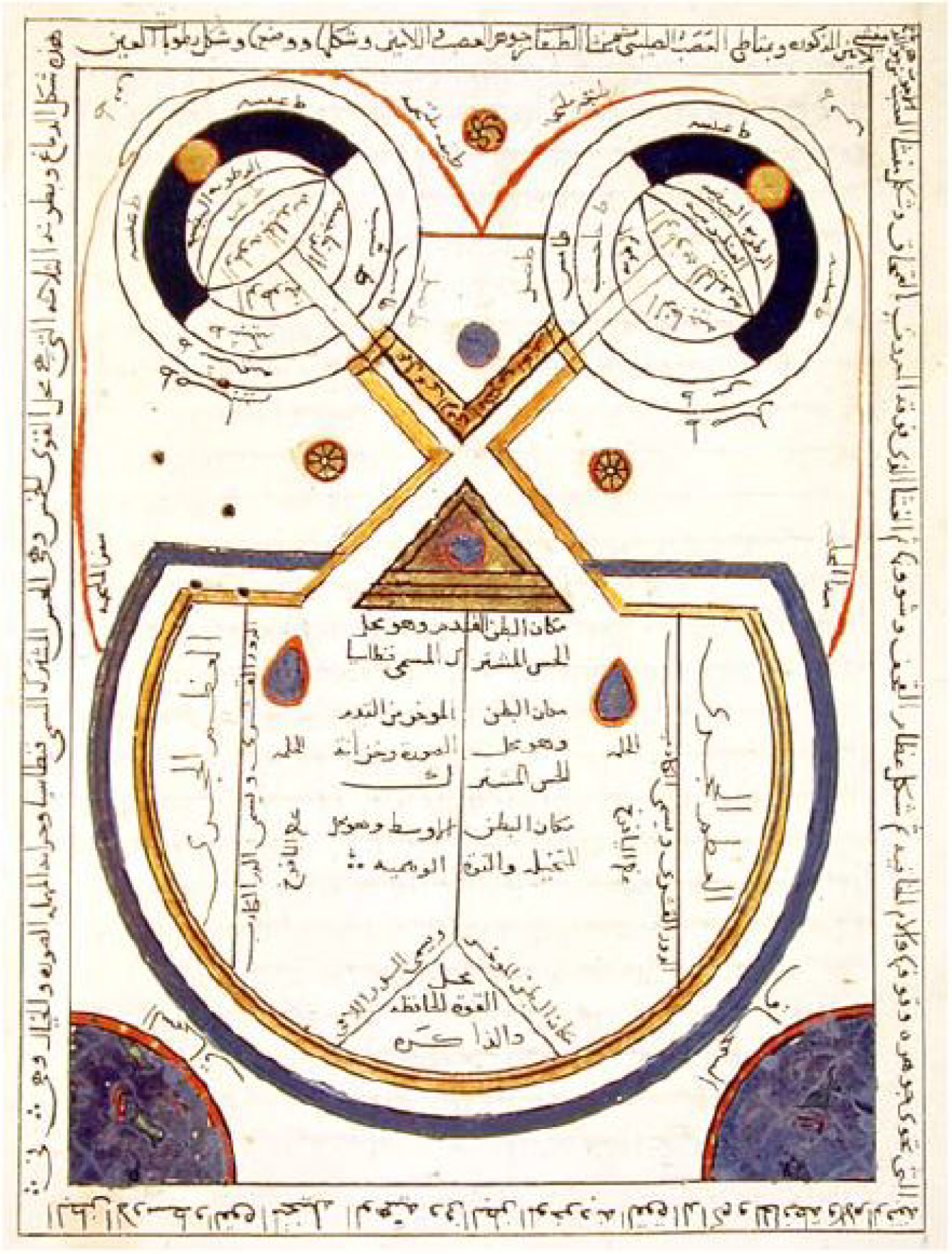
Al-Halabi’s book was the first book to give a remarkable illustration of the anatomy of the brain, the eyes, and the visual pathway among them, as displayed in Figure 19[9,22]. The illustration presented the eyes, the optic chiasm, the cerebral ventricles, the pericranium, the dura mater, the pia mater, the olfactory nerves, and the petrosal bone[34]. The illustration showed that the left eye is controlled by the right part of the brain, and vice versa. All the ocular coats (cornea, sclera, choroid, zonules, and the retina) and the three humidities (vitreous, crystalline lens, and aqueous) are clearly illustrated and labelled. In this drawing, the conjunctiva seemed to originate from the pericranium and the sclera from the dura mater[16].
He drew the optic nerves as hollow, parallel lines, stemming from the back of the sclera to meet the optic chiasm and continue their course posteriorly through the brain tissue until finally reaching the occipital lobe[35]. Two parallel lines extended from the back of the lens to the sclera and optic nerve, almost nearing the description of Cloquet’s canal. Although Al-Halabi drew a small circle in the middle of the triangle behind the chiasm, he did not mention or give the pituitary gland a name.
The American neuroanatomist and neurologist Stephen Lucian Polyak (1889-1955) considered all the European diagrams of the eye until the end of the 16th century, including those by Leonardo da Vinci (1452-1519)[36], to be dependent on Arabic models[37]. Al-Halabi’s drawing is more detailed and informative than Leonardo da Vinci’s one (Codex Atlanticus: Biblioteca Ambrosiana, Milan, vol. 3, fol. 628). Al-Halabi’s drawing remained a reference to all the books dealing with the anatomy of the eye until the German physician D. W. Soemmerring (1793-1871) drew a cross section of the eye in 1827. The American Academy of Ophthalmology used a modified version of Al-Halabi’s drawing as the emblem for the 1987 annual meeting without giving credit to him[11,15,16].
J. Hirschberg stated that “First of all one must appreciate that the Arab ophthalmologists since Hunain had made real efforts to exploit the anatomy, the physiology and the pathology of the brain for their patients. Therefore we do not wish to criticize them for having dragged the optic nerve crossing unnaturally to the front in this imaginary stylized representation of the brain in order to be able to illustrate it at all; we also do that in our diagrams” and “In any case we see in this venerable picture, which probably goes back to models at least from the time around 1000 A.D., a cautious attempt to represent what D. W. Soemmerring insightfully arranged in his classic illustration in 1827” commenting on Al-Halabi’s illustration[22].
Al-Halabi detailed cataract operation representing twelve sorts of cataract in a table[14]. He dedicated a chapter of his book to the surgeries for removing the cataract. He described cataract operations, the required instruments, and the steps to be taken after the operation. He included his own experience which was described in good detail. He is so confident in his own talents that he had the courage to operate the cataract surgery on a one-eyed man for forty days[11,13]. Moreover, he surprisingly reported that he performed a successful cataract surgery for a predatory bird that was owned by his servant. However, the bird’s head movement after the surgery allowed the reappearance of the cataract[15].
He preferred the use of the hollowed cataract needle for aspiration[33], on the solid three-edged couching needle or the rounded couching needle for its safety in the operation. First, a lancet with a rounded tip (instrument number 14 in Figure 1) was utilized for puncturing the outer coats. Then, the hollowed needle (instrument number 22 in Figure 1) was applied to the iris without perforating the cornea. Extracting the lens by suction, using the hollowed needle that resembles to some extent the aspirating syringe nowadays as what could be understood from Al-Halabi’s description has the benefit of excluding the possibility of the lens falling back into the eye[8,15].
Al-Halabi is an early biomedical engineer who invented various ophthalmological instruments. He is the first ophthalmologist to use a magnet for removing metallic foreign body from the eye. He utilized his instruments in the treatment of different eye diseases such as trachoma, lagophthalmos, chalazion, chemosis, symblepharon, ectropion, hordeolum, distichiasis, pannus, pterygium, and cataract. Al-Halabi’s book was the first to give a remarkable illustration of the anatomy of the brain, the eyes, and the visual pathway among them. Al-Halabi detailed cataract operation representing twelve sorts of cataract in a table.
The current research article could not come to light without the reproduction of Al-Halabi’s book edited by Wafai MZ (MD, FACS, FICS, and FRCOphth) and Kalaji MR (PhD). Dr. Wafai is a chief of Vitreo-Retina Division, King Khalid Eye Specialist Hospital, Riyadh, Saudi Arabia, and a former instructor in ophthalmology, Harvard Medical School, Boston, Massachusetts, United States. Dr. Kalaji is a professor of Islamic Studies, King Saud University, Riyadh, Saudi Arabia, and a former professor of Islamic Studies, Damascus University, Syria.
Finally, recognition must be given to the Frankfurt and Istanbul Museums for the History of Science and Technology in Islam. The Istanbul Museum has copies of the instruments that are in the Frankfurt Museum, and both museums are founded by the same person, Professor Dr. Fuat Sezgin. Institute for the History of Arab-Islamic Sciences, which runs the Frankfurt Museum, kindly and generously authorized the reproduction of the photos in this article.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medical laboratory technology
Country/Territory of origin: Egypt
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Au SCL S-Editor: Wang JJ L-Editor: A P-Editor: Wang JJ
| 1. | Gooday G, Lynch JM, Wilson KG, Barsky CK. Does science education need the history of science? Isis. 2008;99:322-330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Valentinuzzi ME. Why study the history of BME, science, and technology? IEEE Pulse. 2011;2:45-47. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Taylor HR. Trachoma is an ancient disease and a weapon of mass destruction. In: Taylor HR. Trachoma: A blinding scourge from the bronze age to the twenty-first century. Victoria, Australia: Centre for Eye Research Australia, 2008: 1-16. |
| 4. | Maccallan AF. THE BIRTH OF OPHTHALMOLOGY AND ITS DEVELOPMENT IN EARLY ARABIC LITERATURE. Br J Ophthalmol. 1927;11:63-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 5. | Griffith FLI. The inscriptions. In: Petrie WMF, Griffith FLI. The royal tombs of the first dynasty. London, UK: Cambridge University Press, 1900-1901: 48-55. |
| 6. | Ascaso FJ, Huerva V. The history of cataract surgery. In: Zaidi F. Cataract surgery. Rijeka, Croatia: IntechOpen, 2013: 75-90. [DOI] [Full Text] |
| 7. | Savage-Smith E. Hellenistic and Byzantine ophthalmology: Trachoma and sequelae. Dumbarton Oaks Papers. 1984;38:169-186. |
| 8. | FEIGENBAUM A. Early history of cataract and the ancient operation for cataract. Am J Ophthalmol. 1960;49:305-326. [PubMed] |
| 9. | Kaadan AN, Hamati S. The Ophthalmic Medicine in Aleppo in 100 Years 1850-1950 AD. The International Society for the History of Islamic Medicine. 2001. [cited 5 January 2021]. Available from: http://www.ishim.net/2009/The%20Ophthalmic%20Medicine%20in%20Aleppo%20in%20100%20Years.doc. |
| 10. | Abdalla M. The fate of Islamic science between the eleventh and sixteenth-centuries: a critical study of scholarship from Ibn Khaldun to the present. Griffith University. 2004. [DOI] [Full Text] |
| 11. | Zaimeche S. Aleppo. The Foundation for Science, Technology and Civilisation (FSTC). 2008. [cited 5 January 2021]. Available from: http://www.muslimheritage.com/uploads/Aleppo.pdf. |
| 12. | Kaadan AN, Alherek M. Subconjunctival hemorrhage in the most famous eye Islamic medical books. J Int Soc Hist Islam Med. 10-11:42-45. |
| 13. | POLLOCK WB. Arabian ophthalmology. Br J Ophthalmol. 1946;30:445-456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 14. | Hirschberg J. Arabian ophthalmology. J Am Med Assoc. 1905;XLV:1127-1131. [DOI] [Full Text] |
| 15. | Wafai MZ, Kalaji MR. Al-Kafi Fi Al-Kuhl by Khalifah ibn Abi Al-Mahasin Al-Halabi (died around 656AH = 1256AD). Rabat, Morocco: Islamic Educational, Scientific and Cultural Organization (ISESCO) Publications, 1990: 1-794. |
| 16. | Wafai MZ. Ophthalmologists of the Medieval Islamic world. The Foundation for Science, Technology and Civilisation (FSTC). 2016. [cited 5 January 2021]. Available from: http://www.muslimheritage.com/uploads/ophthalmologists_sy_v6_08_04.pdf. |
| 17. | Langermann YT. Ibn Kammūna at Aleppo. J R Asiat Soc. 2007;17:1-19. [DOI] [Full Text] |
| 18. | Savage-Smith E. Medicine in Medieval Islam. In: Lindberg DC, Shank, MH. The Cambridge history of science: Volume 2: Medieval science. Cambridge: Cambridge University Press, 2013: 139-167. [DOI] [Full Text] |
| 19. | Leclerc L. Histoire de la Medicine Arabe (History of the Arabian Medicine). Paris, France: Ernest Laroux, 1876: 157-213. |
| 20. | Hirschberg J, Lippert J, Mittwoch E. Ammar B. Ali Al-Mausili, Halifa Al-Halabi, Salah Ad-Din. In: Hirschberg J, Lippert J, Mittwoch E. Die Arabischen augenärzte (Arabian ophthalmologists). Leipzig, Germany: Verlag Von Veit & Comp, 1905: 150-153. |
| 21. | Haq I, Khatib HA. Light through the dark ages: The Arabist contribution to Western ophthalmology. Oman J Ophthalmol. 2012;5:75-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 22. | Sezgin F, Neubauer E. Volume IV: Catalogue of the collection of instruments of the institute for the history of Arabic and Islamic sciences. In: Sezgin F. Science and technology in Islam. Frankfurt am Main, Germany: Institute for the History of Arabic-Islamic Science, 2010: 1-94. |
| 23. | Alvarez-Millan C. Practice vs theory: tenth-century case histories from the Islamic Middle East. Soc Hist Med. 2000;13:293-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 24. | Saad MN. Could Al-Zahrawi Be Considered a Biomedical Engineer? IEEE Pulse. 2016;7:56-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 25. | Giasin O, Yeo DC, Aguirre A. Just how old is the modern dacrocystorhinostomy? Br J Ophthalmol. 2014;98:1134-1135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 26. | Laios K, Moschos MM, George A. Ammar ibn Ali al-Mawsili and His Innovating Suction Method for the Treatment of Cataract. Surg Innov. 2016;23:433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 27. | Masic I. On occasion of 800th anniversary of birth of Ibn al-Nafis--discoverer of cardiac and pulmonary circulation. Med Arh. 2010;64:309-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 28. | Savage-Smith E. Ibn al-Nafīs's Perfected book on ophthalmology and his treatment of trachoma and its sequelae. J Hist Arabic Sci. 1980;4:147-204. [PubMed] |
| 29. | Kaadan AN, Alherek M. Chalazion and its Treatment in Arabic and Islamic Medicine. The International Society for the History of Islamic Medicine. 2001. [cited 1 January 2021]. Available from: http://www.ishim.net/islam/baradah.htm#2. [DOI] [Full Text] |
| 30. | Yedke SR, Raut SY, Jangde CR. Experimental evaluation of horse hair as a nonabsorbable monofilament suture. J Ayurveda Integr Med. 2013;4:206-210. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 31. | Kaadan AN, Kakhshan, A. Ophthalmic drops in the book of Kitab Al-'Umdah Al-Kuhliyah fi Al-Amrad Al-Basariyah. J Int Soc Hist Islam Med. 14-15:31-34. |
| 32. | Alraghran A, khatib C. The new informations about aromatherapy and scents edited by Albucasis. J Int Soc Hist Islam Med. 14-15:64-83. |
| 33. | Savage-Smith E. The practice of surgery in Islamic lands: myth and reality. Soc Hist Med. 2000;13:307-321. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 29] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 34. | Savage-Smith E. Anatomical illustration in arabic manuscripts. In: Contadini, A. Arab painting: Text and image in illustrated Arabic manuscripts. Leiden, Netherlands: Brill, 2010: 145-159. |
| 35. | Tamraz JC, Comair YG. Optic pathway and striate cortex. In: Tamraz JC, Comair YG. Atlas of regional anatomy of the brain using MRI: With functional correlations. Berlin, Heidelberg, Germany: Springer Berlin Heidelberg, 2000: 257-298. [DOI] [Full Text] |
| 36. | Valentinuzzi ME, Pallotti G. Leonardo: the bioengineer. IEEE Pulse. 2013;4:58, 60, 62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 37. | Polyak SL. The retina: the anatomy and the histology of the retina in man, ape, and monkey, including the consideration of visual functions, the history of physiological optics, and the histological laboratory technique. Chicago: The University of Chicago Press, 1941:128. |