Published online Jul 20, 2021. doi: 10.5662/wjm.v11.i4.208
Peer-review started: February 27, 2021
First decision: March 31, 2021
Revised: April 10, 2021
Accepted: June 1, 2021
Article in press: June 1, 2021
Published online: July 20, 2021
Processing time: 141 Days and 21.9 Hours
Despite its proven high utility, integration of pocked-sized portable ultrasound (US) into internal medicine residency training remains inconsistent. For 10 years, we have held a 1-d seminar biannually, consisting of lecture (half-day) and hands-on training (half-day) on pocket-sized US of the abdomen and lungs. The lecture consists of training on US physics and clinical applications of pocket-sized US, followed by a lecture covering the basic anatomy of the abdomen and lungs and introducing the systemic scanning method. Given the simple structure of pocket-sized US devices, understanding the basic physics is sufficient yet necessary to operate the pocket-sized US device. It is important to understand the selection of probes, adjustment of B mode gain, adjustment of color gain, and acoustic impedance. Basic comprehension may have a significant positive impact on the overall utilization of pocket-sized US devices. The easiest and most reliable way to observe the whole abdomen and lungs is a combination of transverse, sagittal, and oblique scanning, pursuing the main vascular system from the center to the periphery of the organ in the abdomen and systemic scanning of the pleura. There is usually a marked change in knowledge and attitudes among the program participants, although skill gaps remain among them. We discuss the limitations and problems to this education system as well.
Core Tip: Despite its high utility, there is no standardized method to integrate pocked-sized ultrasound (US) into daily clinical settings. We present here our 1-d seminar for residents that consists of lecture and hands-on training on pocket-sized US. The lecture consists of training on US physics and clinical applications of pocket-sized US, covering basic anatomy, and introducing the systemic scanning method. Understanding of some basic physics is necessary to operate the pocket-sized US device. Although the residents’ skill gaps remain, the seminar yields a marked change in knowledge and attitude towards pocket-sized US.
- Citation: Naganuma H, Ishida H. One-day seminar for residents for implementing abdominal pocket-sized ultrasound. World J Methodol 2021; 11(4): 208-221
- URL: https://www.wjgnet.com/2222-0682/full/v11/i4/208.htm
- DOI: https://dx.doi.org/10.5662/wjm.v11.i4.208
As the worldwide population rapidly ages, a concurrent rapid increase in the global financial healthcare burden has been observed[1]. The resources available for daily clinical practice are generally limited. Thus, simple, effective, and realistic systemic methods in patient care and medical education are urgently required. Actual clinical scenarios are varied, complex, and require a prompt response. Thus, the traditional medical approaches (inspection, palpation, auscultation, or other components of the physical examination and laboratory data analysis) cannot immediately answer the questions raised during clinical practice[2,3]. Addition of a “scientific eye” in the hand is expected to resolve such problems to a certain degree.
Recent advances in ultrasound (US) technology have made US instruments continuously smaller[4]. Among all of the medical imaging tools, the US device is the only instrument to be miniaturized. In the past, US examination was performed by radiologists using a bulky, expensive, and specialized machine with sophisticated functions in a specialized room[5]. US is currently utilized as an important adjunct to physical examination in a wide range of clinical situations due to the development of small-sized devices[6]. Portable US devices were first used in cardiology[7,8] then in emergent medicine[9,10]. A comparative study between fifth-year medical students using US and cardiologists not using US showed that the former achieved a correct diagnosis 75% of the time, while the latter achieved a correct diagnosis 49% of the time, indicating the importance of visual information in the diagnosis[8]. It also suggests that practitioners unexperienced with US can obtain adequate proficiency with minimal training.
The benefits of portable US are that it is widely available, and carries no risk of radiation exposure. However, an important disadvantage to using this tool is that its diagnostic accuracy is highly operator-dependent, and errors occur during image acquisition and image interpretation (like in traditional US examination)[4]. Furthermore, there is no standardized technique among examiners for observing the abdomen by portable US[11]. However, the benefits of portable US must be emphasized against such inconveniences, and US education is important to extend the benefit of portable US devices. Recent studies have reported favorable results of US education for medical students[12-14]. Though in our opinion, US education for new residents are more meaningful than for medical students. At the residency level, there is a deeper understanding of balancing portable US results and patient characteristics to establish clinical decision making. This background motivated us to begin a portable US education seminar intended for new internal medicine residents.
In this review, we present our US education 1-d seminar for new (post graduate year-1 or -2) internal medicine residents that focuses on the use of pocket-sized US on the abdomen and lungs. The goal of the seminar is for residents to have the confidence to integrate pocket-sized US results into their clinical decision making.
The use of portable US devices has recently been adopted more frequently in clinical settings, and the market is flourishing[15]. Portable US devices have passed through three generations: Laptop-associated devices (personal computer-sized machine coupled with multiple applications), hand-carried devices (book-sized machine carried by hand), and hand-held devices (portable and able to fit in the pocket of a clinician’s white coat, thus referred to as pocket-sized US). Each US company has different built-in applications, such as Doppler display, puncture guidance, and distance or volume measurement[16].
Pocket-sized US devices are usually used by unexperienced non-radiologist general clinicians under the name of “US stethoscope”[4] to complement clinical examination and provide immediate visual correlates of clinical findings. The concept of a US stethoscope is expanding worldwide, but like high-end US machines, pocket-sized US devices are effective in the hands of experienced examiners. Furthermore, comparative studies between pocket-sized US and high-end US have stressed some important points: the image quality of pocket-sized US is slightly inferior to high-end US but still satisfactory for clinical use[17,18]. US measurement by pocket-sized US devices is feasible, and acoustic power of the US machine strongly affects the penetration and resolution of the US image [mechanical index: 0.9-1.0 (pocket-sized US) vs 1.8 (high-end US)]. Pocket-sized US devices will not replace a high-end US machine and the need for detailed US examination by experienced radiologists will always be present, but there is value in the pocket-sized US examination.
Since 2010, we have biannually hosted a 1-d seminar consisting of lecture (half-day) and hands-on training (half-day) on portable US devices to increase the number of portable US operators and to develop the examination skills among new residents. For this hands-on training, we use pocket-sized US devices because of their portability and affordability (the most important characteristic of portable US devices when thinking of expected future applications). The aim of this seminar is to familiarize residents with pocket-sized US devices but not to immediately increase their US capability.
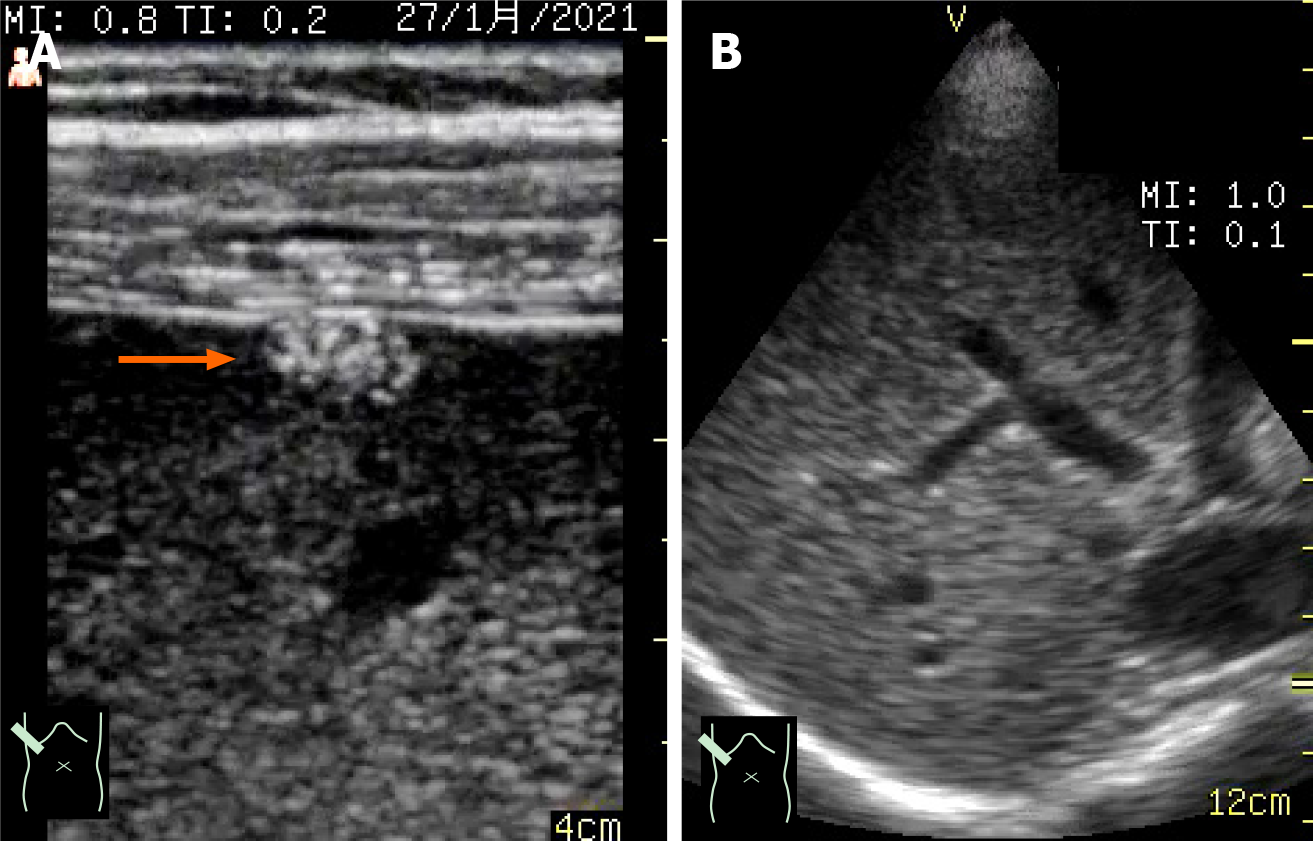
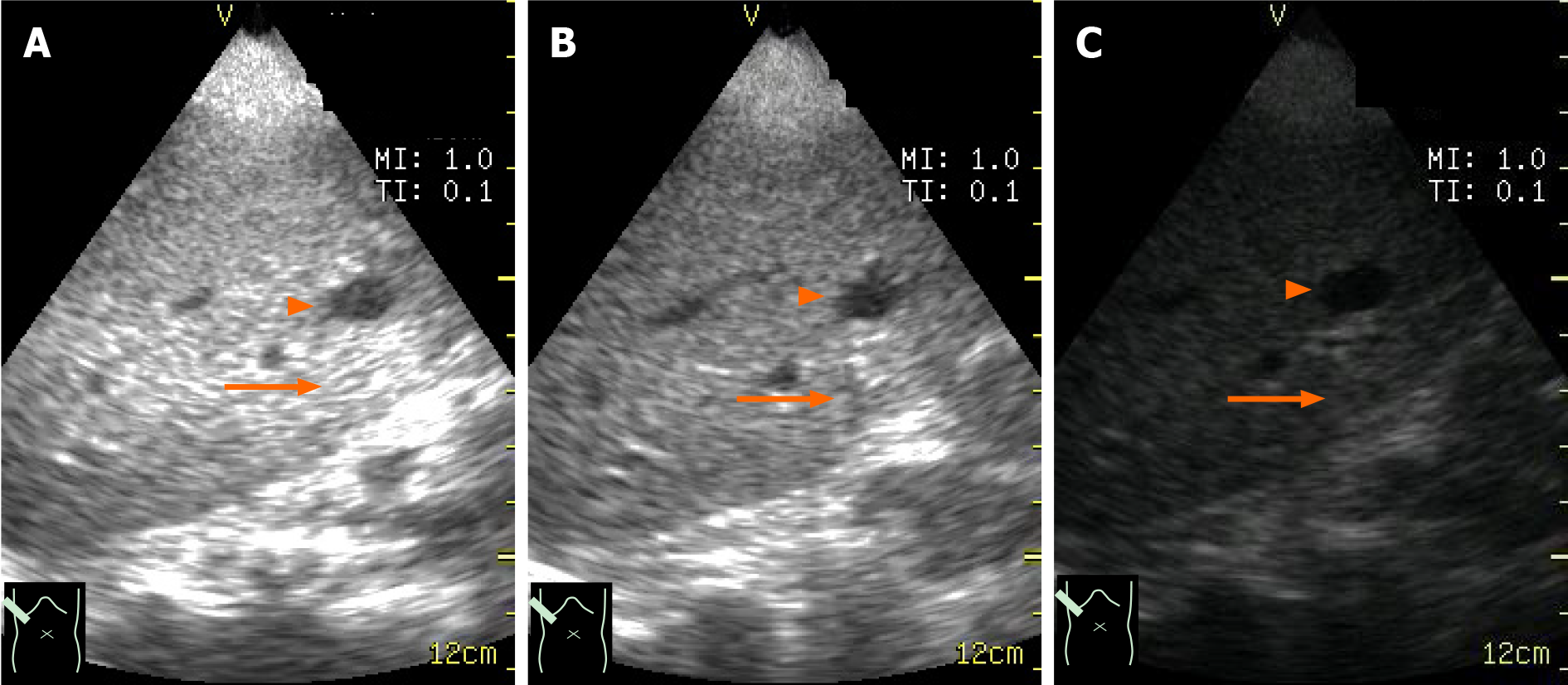
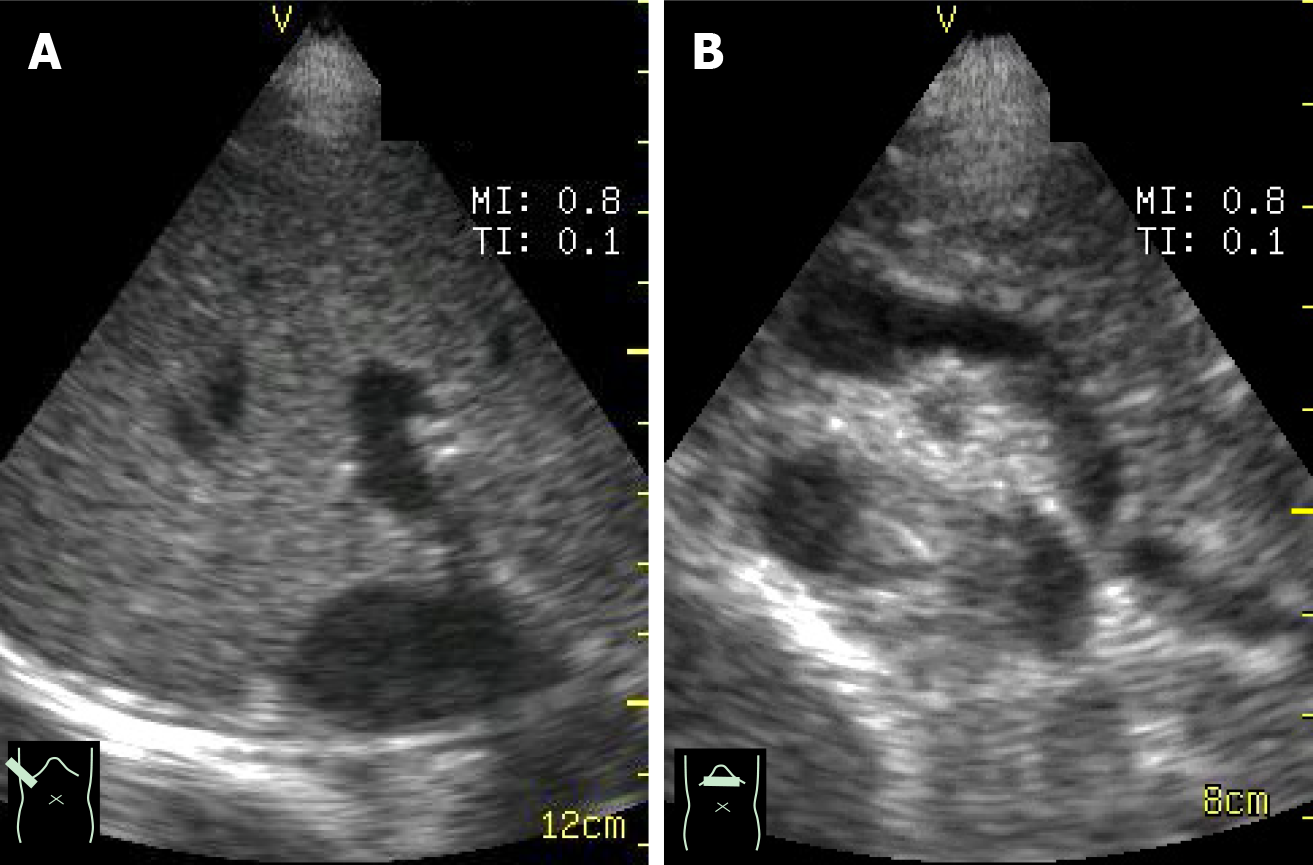
In the lecture, we begin with a simple lecture about fundamental US physics to optimize pocket-sized US application and to minimize errors in device manipulation and US image interpretation. The next lecture covers the basic anatomy of the abdomen and lungs as well as introducing systemic scanning procedures (Figure 1). In the lecture, we present both high-end US images and pocked-sized US images simultaneously in order to compare these images. This comparison is necessary to become familiar with the slightly inferior image quality of pocket-sized US (Figure 2). In the remaining time, we present a few model cases where pocked-sized US information helped create a patient care strategy followed briefly by a lecture on built-in applications including color Doppler US.
Compared with sophisticated and complex high-end applications, such as contrast-enhanced US and shear wave elastography, the pocket-sized US device has a simple structure. Understanding basic physics is sufficient but necessary to begin to operate the pocket-sized US device. During this lecture, we stress four basic points of US physics needed to prevent device manipulation errors[19]: Selection of probes (high-frequency linear probe for superficial areas, such as the gastrointestinal tract and pleura or conventional sector (convex) probe for deep areas, such as liver and abdominal vessels), adjustment of B mode gain, adjustment of color gain, and problems related with acoustic impedance/the reason why US detection of stones (biliary, renal, and others) and fluid collection (ascites, pleural effusion, and others) is highly sensitive. This basic comprehension has a significant positive impact on the utilization of pocket-sized US devices.
Probe selection: With the transducer, the US beams are steered at varying angles from one side to the other to produce a sector format. This format permits a large, deep field of view, but its near field focus is reduced. Therefore, this format is unsuitable for observing superficial areas. The linear probe activates a group of elements to generate perpendicular US beams, which provide a high resolution in the near field[20]. As a result, probe selection is dependent on the type of organ to be observed (Figure 3).
Adjustment of B mode gain: The echo signal amplitudes are usually compressed in order to be accommodated by the display. This accommodation serves to visualize a wide range of echo signals on the display but reduces the real differences in the echo signal amplitude. As a result, when B mode gain is too low or too high, we cannot recognize small differences in echogenicity (echo signal amplitude). Thus, B mode gain should be adjusted in order to not overlook the abnormality (Figure 4).
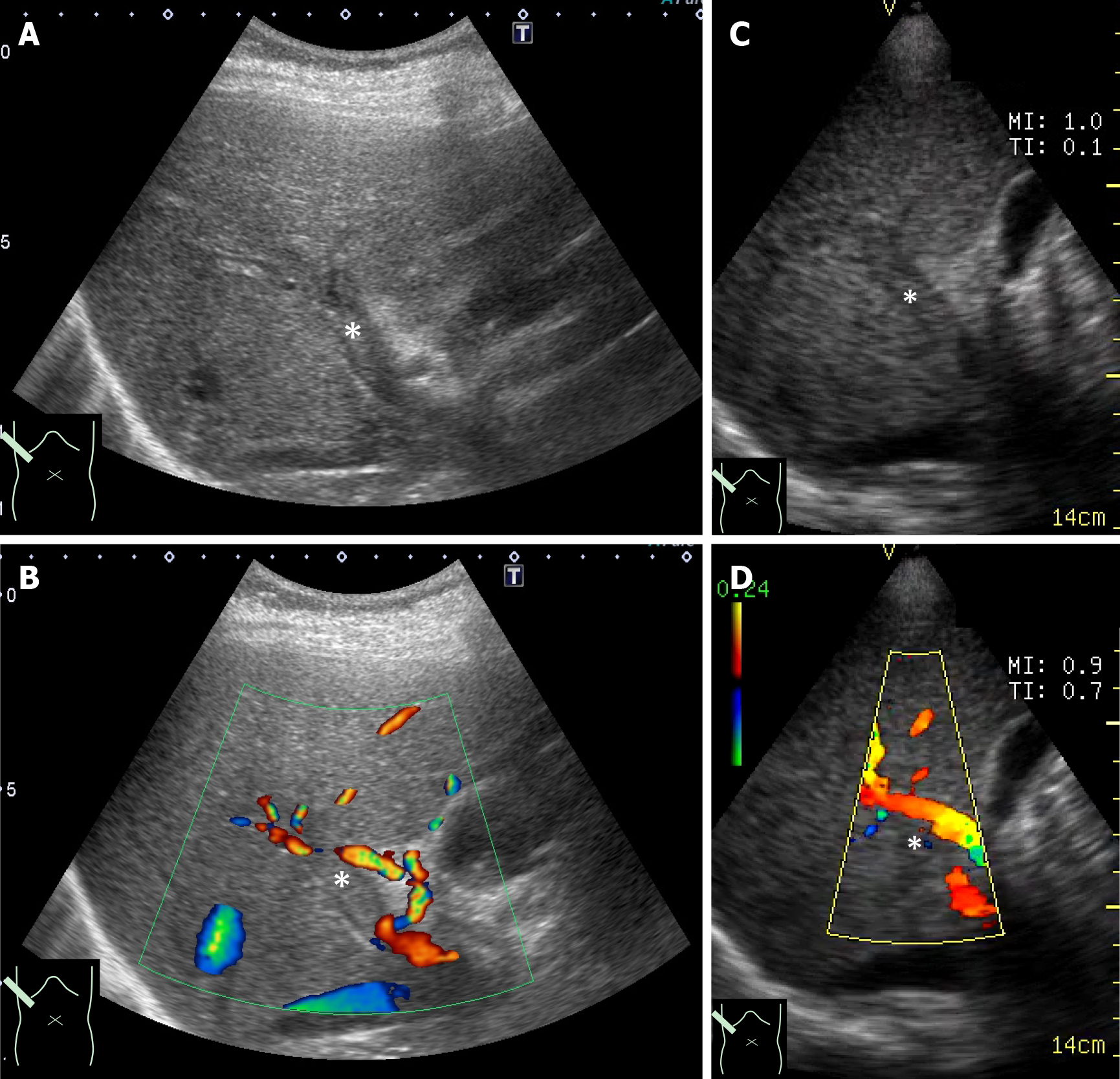
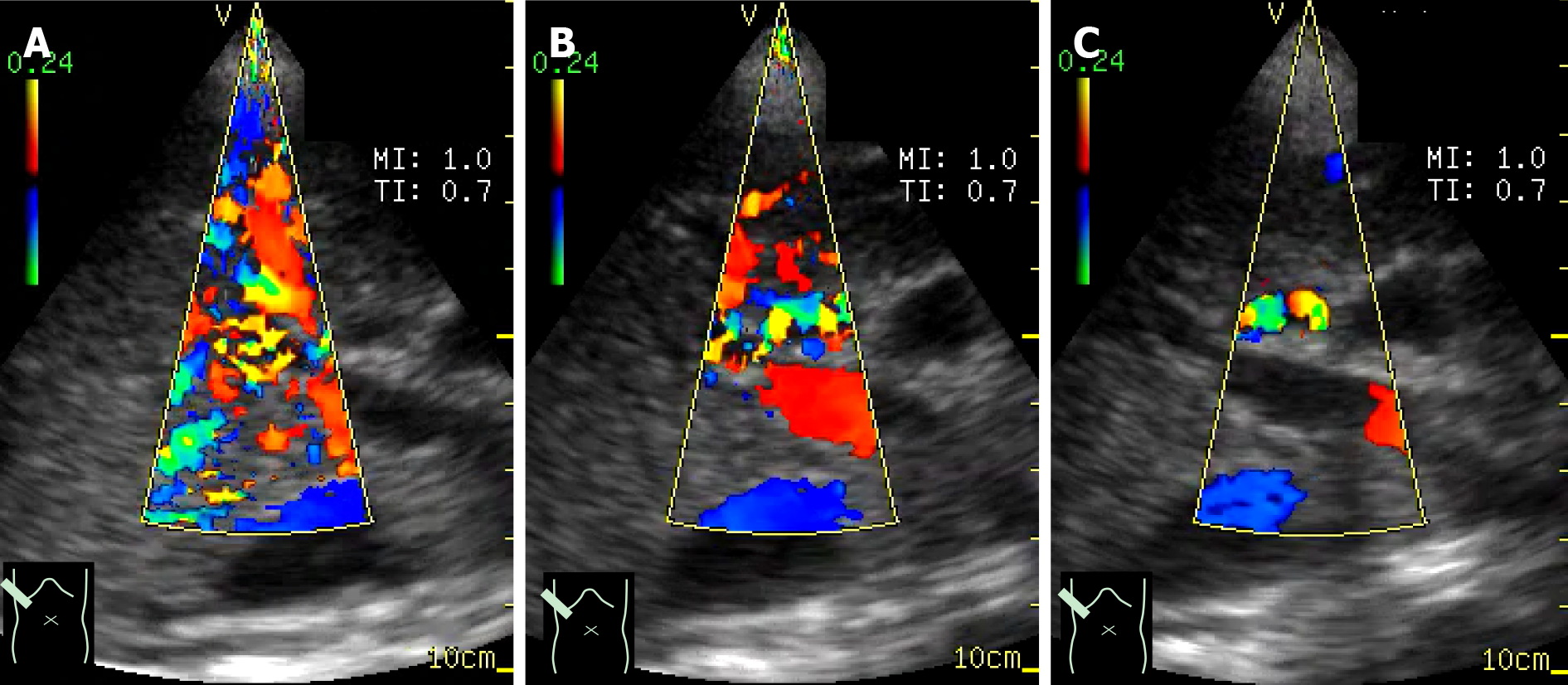
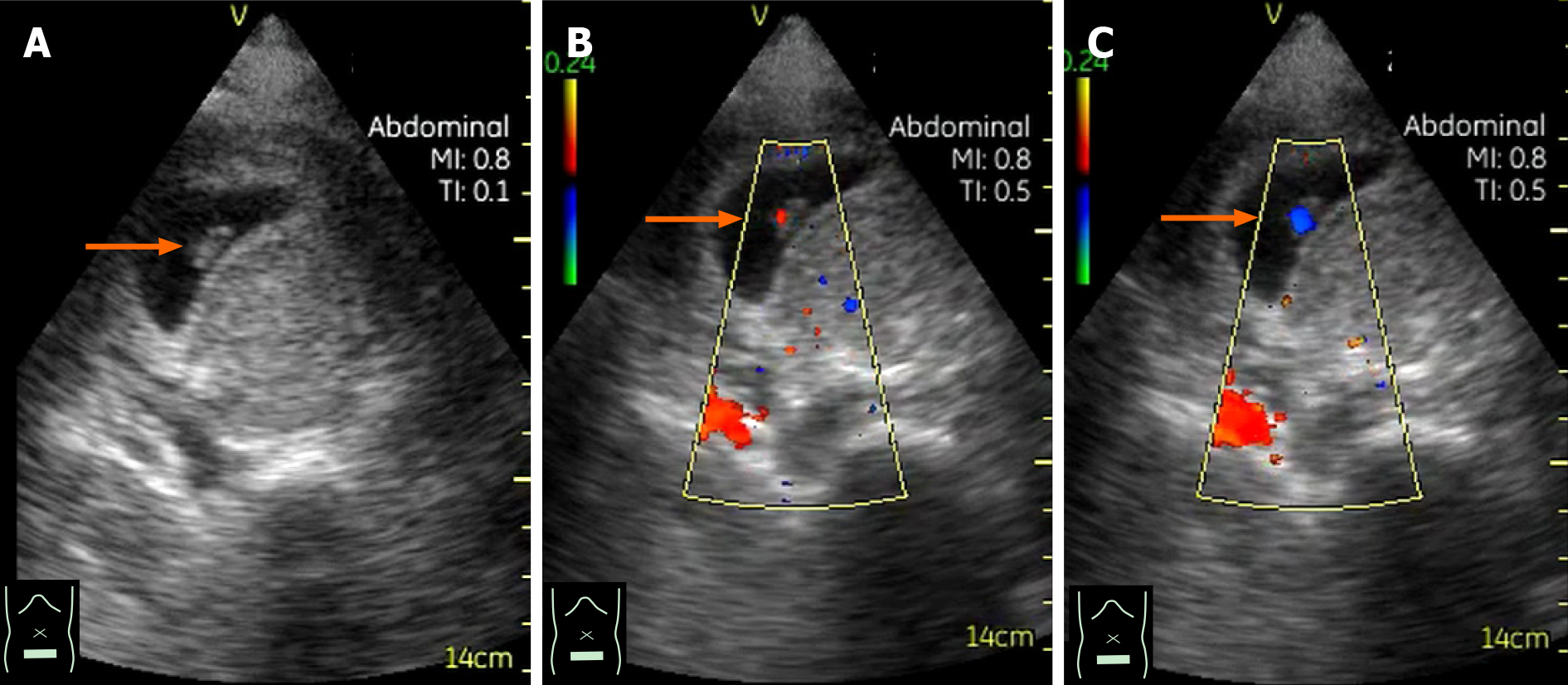
Adjustment of color gain: In color Doppler US, flow velocity in each point is indicated by color brightness: the higher the velocity, the brighter the color. Color Doppler gain is the receiver end amplification of the Doppler signal. The Doppler gain is usually increased to the maximum limit just before the background noise is seen. If color Doppler gain is too high, then the field of view is filled with noise. If it is too low, then useful Doppler data is not seen on the display. Thus, color Doppler gain must be properly adjusted to gain useful hemodynamic information (Figure 5).
US physics related to stones and fluid: Acoustic impedance is an important property of tissues. It is defined as the tissue density multiplied by its propagation velocity of sound[21]. Acoustic impedance changes according to the tissue (e.g., water: 1.48 × 106 kg/m2/s, liver: 1.65 × 106 kg/m2/s, bone: 7.80 × 106 kg/m2/s)[21]. When passing through two tissues of different acoustic impedance, some portion of the US is reflected. Its reflection degree depends on the difference in acoustic impedance between two tissues. The reflection of the US is larger between water (fluid collection) and soft tissue than between two soft tissues, leading to the fact that fluid collection is clearly margined and easily detected[22]. The reflection of the US is larger between soft tissue and stone. Almost all the US is reflected at the stone surface. Therefore, stones are easily and correctly detected by US[23] (Figure 6).
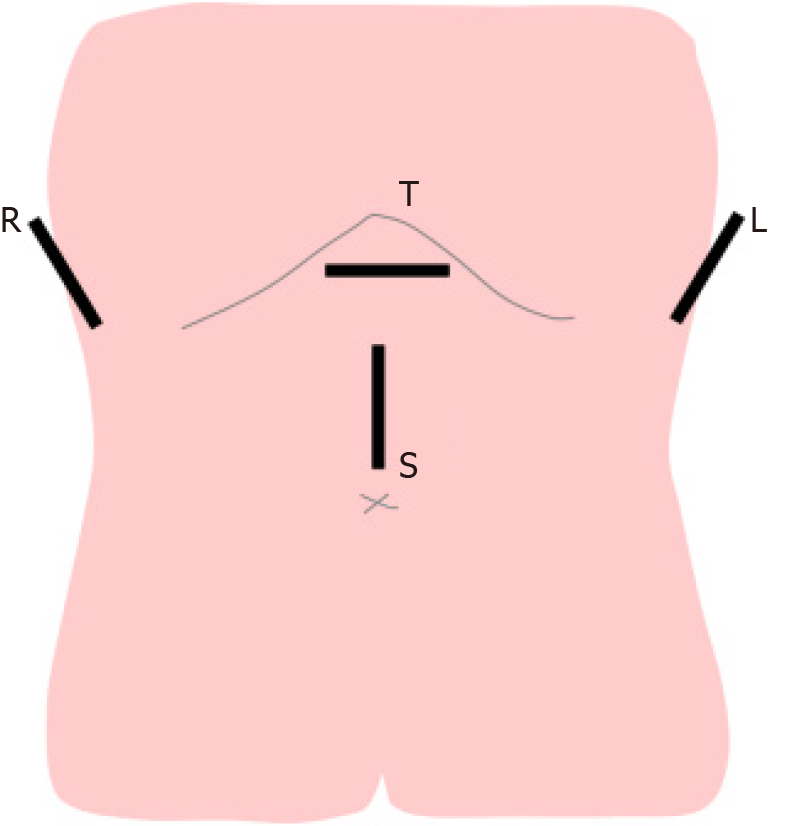
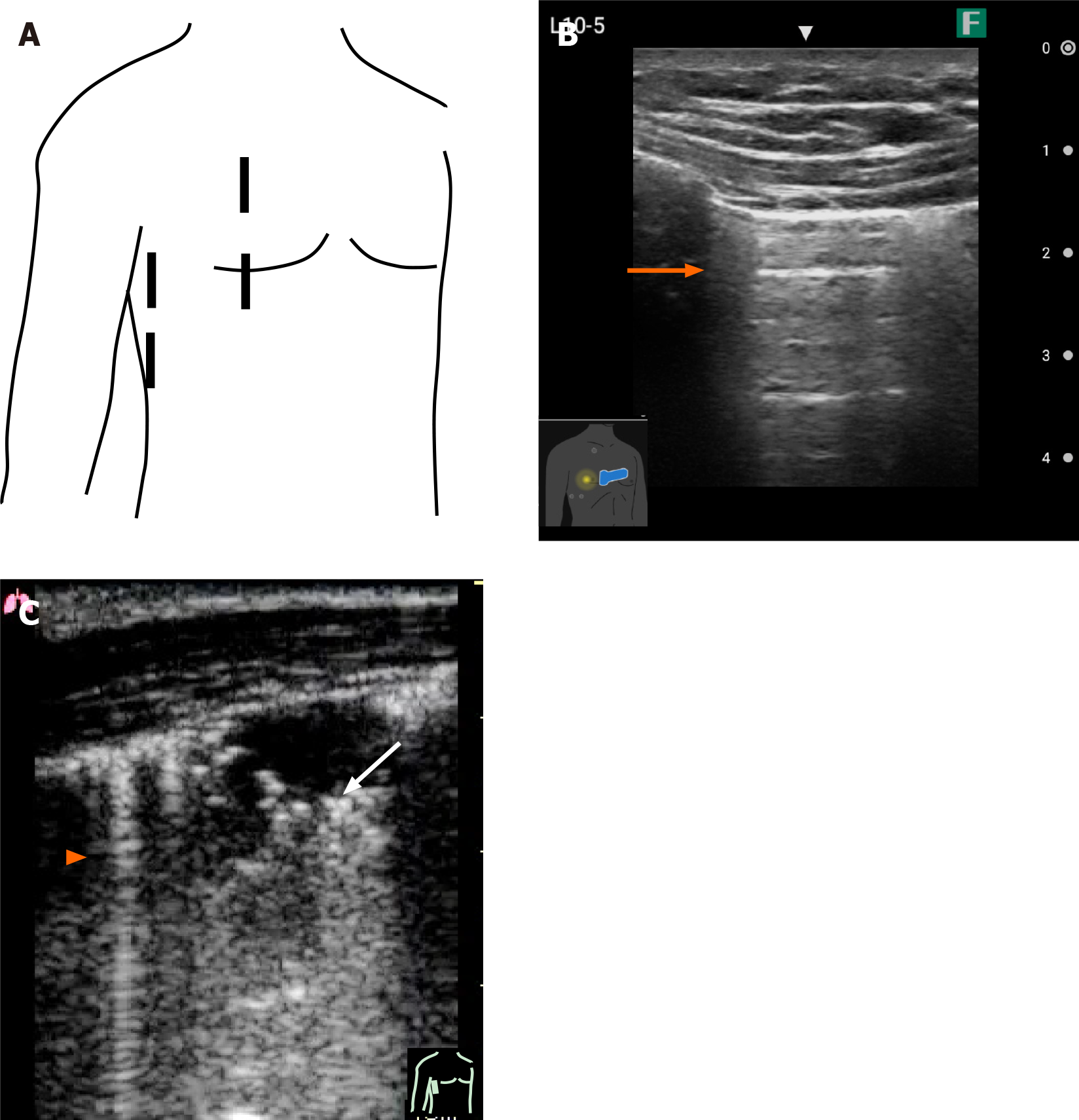
For detailed US diagnosis, the examiner is expected to make a differential diagnosis of a wide spectrum of diseases. Meticulous scanning techniques are required for this purpose. However, because most participants do not have sufficient prior knowledge of US examination, our initial effort is focused on understanding the global normal anatomy. The combination of transverse, sagittal, and oblique (intercostal) scanning (Figures 7 and 8) permits the efficient observation of the abdominal organs. The most reliable way to observe each organ (liver, pancreas, spleen, and kidneys) is to pursue the main vascular system (landmark) from the center to the periphery of the organ. After the training in each organ, the parenchymal echostructures around the vessel are presented. Recognition of these landscapes serves to detect abnormal lesions. Use of the high-frequency linear probe permits the observation of the pleura (Figure 9). The hands-on training following this short lecture reinforces the anatomical knowledge of the abdomen/Lungs and the technical skills (transducer handling, portable US device manipulation, and confidence in abdominal observation by pocket-sized US).
Then, we present several clinical cases where portable US was useful for confirming a wide spectrum of clinical applications.
Case 1: A 35-year-old female with known repetitive gastric ulcers presented with abdominal pain and nausea visited our outpatient clinic (Gastroenterology). Initially, the clinician may suspect a recurrence of the gastric ulcers. Though the patient denied the possibility of pregnancy, the use of a pocket-sized US device confirmed the pregnancy. The proper use of the pocket-sized US device led to reduced ionizing radiation exposure and allowed to the transfer of the patient to the gynecology section (Figure 10).
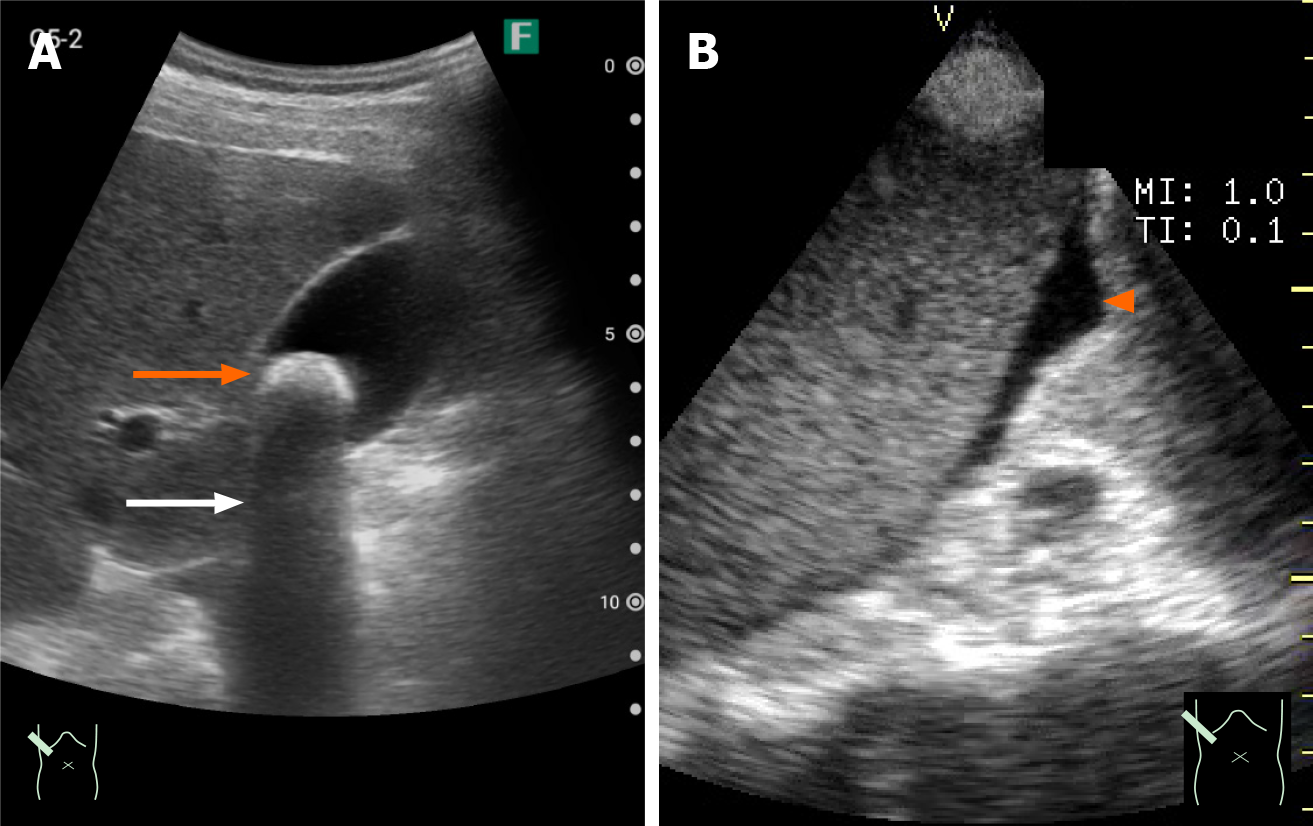
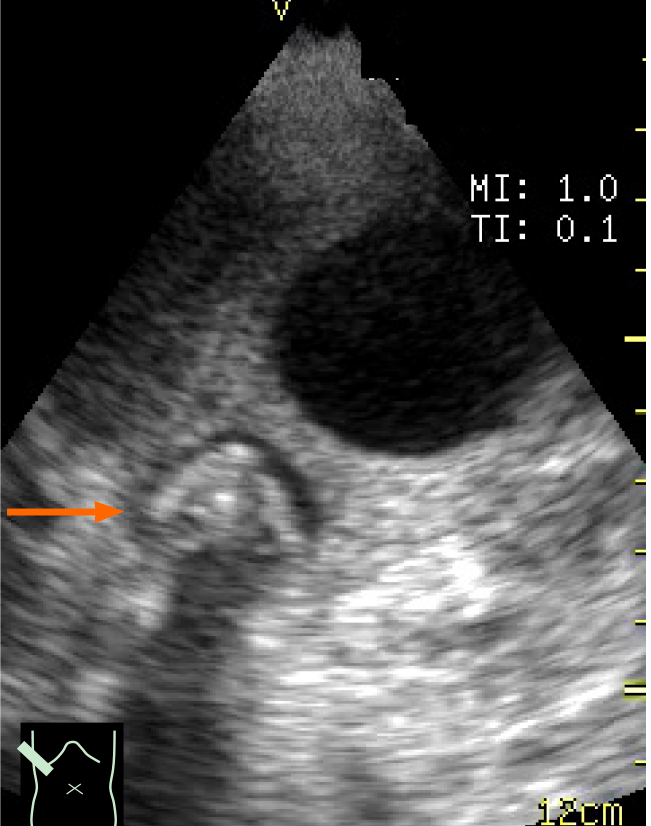
Case 2: A 72-year-old female with severe abdominal pain visited our emergency department. The pain was so severe that she could not move from the ambulance. A pocket-sized US device revealed an impacted gallbladder stone. The pain worsened upon probe compression of the gallbladder, which led to the diagnosis of acute stone-impact-induced cholecystitis. The patient was immediately treated. The pocket-sized US device significantly reduced the time to diagnosis (Figure 11).
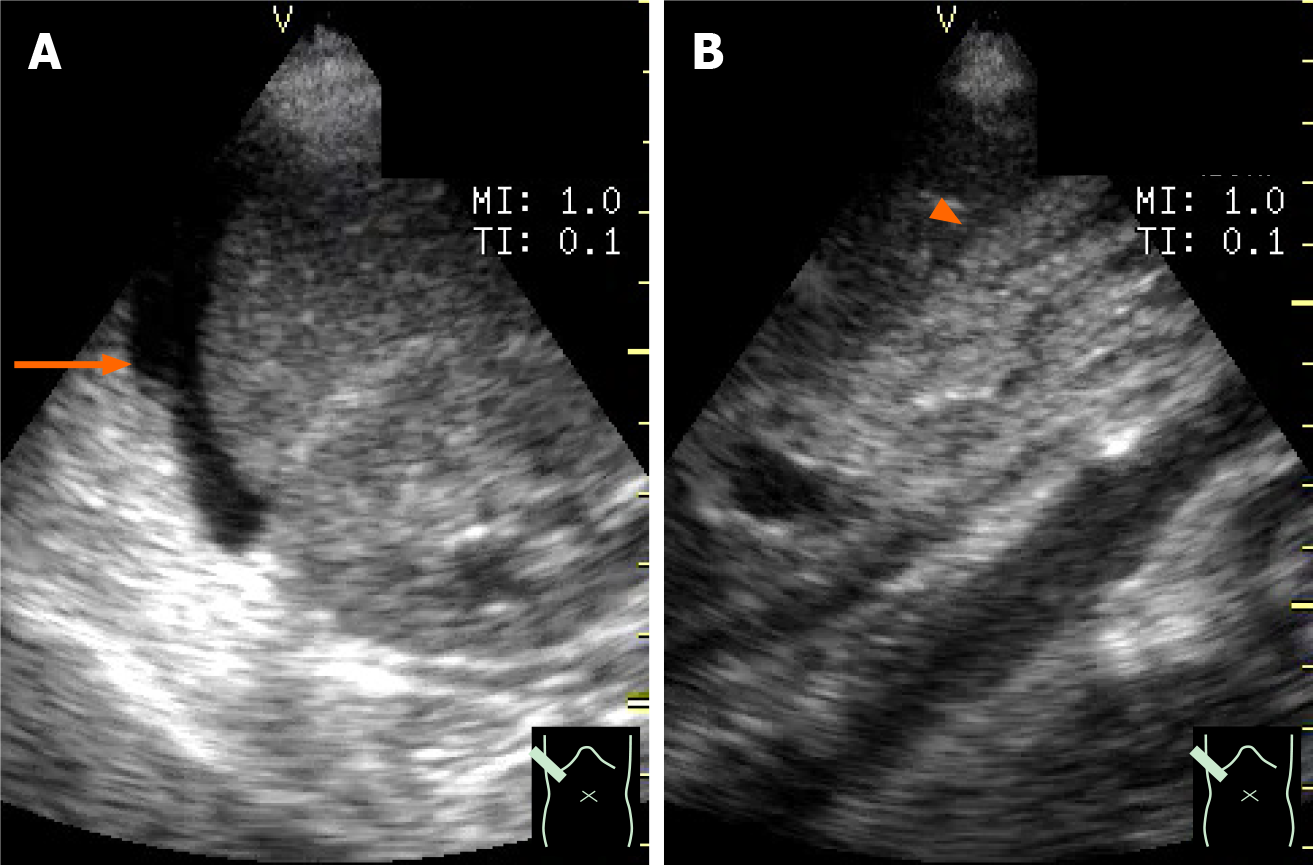
Case 3: A 41-year-old female was admitted to our hospital with a chief complaint of hepatic dysfunction. She was almost asymptomatic. A pocket-sized US device was used as part of the physical examination during rounds. The US revealed a small amount of ascites around the liver, and her gallbladder collapsed. Biochemical examination was immediately ordered and showed markedly elevated transaminases and coagulopathy. She was diagnosed with severe acute hepatitis, and energic treatment began immediately (Figure 12).
Although these US examinations were successfully performed by skillful pocket-sized US practitioners, the program participants can image how to utilize a pocket-sized US device in their own clinical setting[22-24].
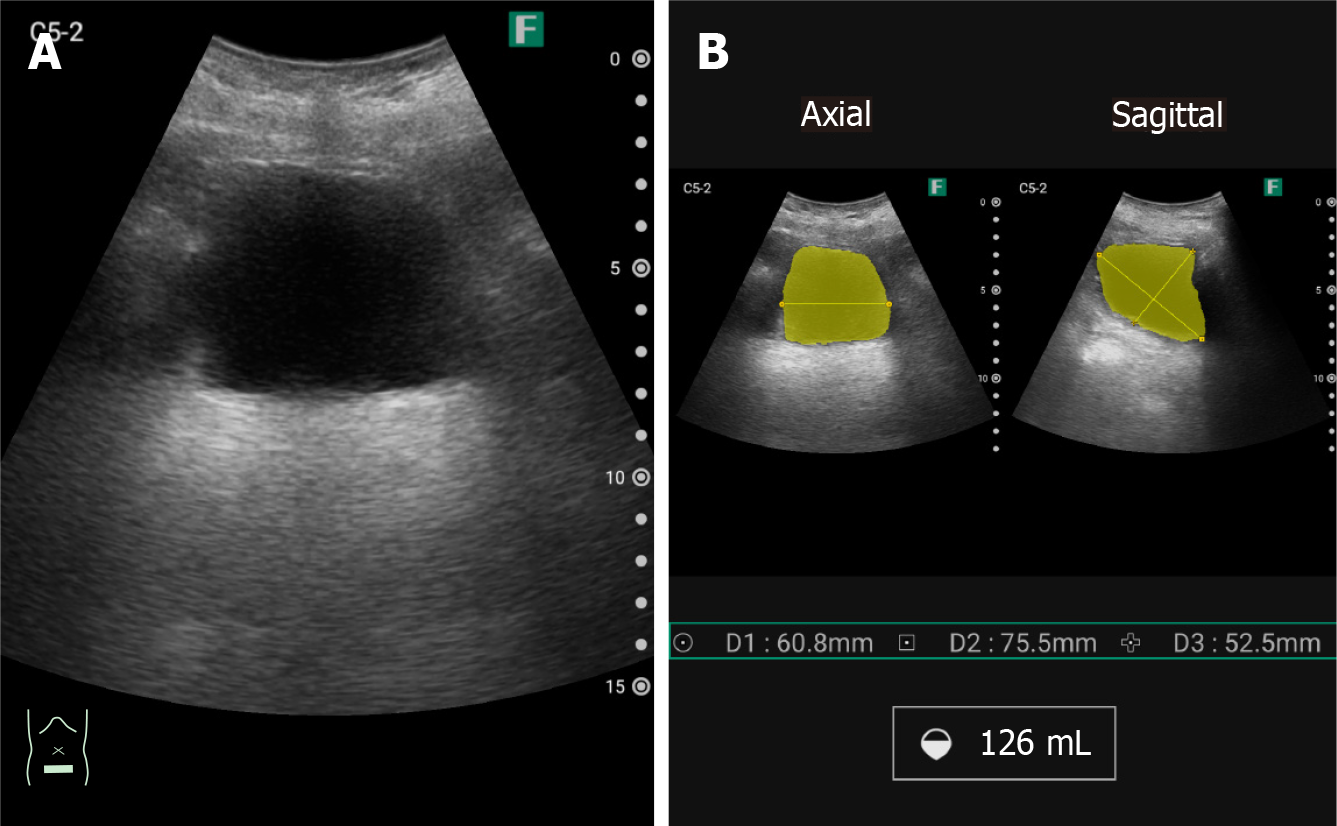
Each US company has different built-in applications, such as a Doppler display (Figures 2 and 5), embedded in almost all devices. Puncture guidance is embedded in about half of all devices[25], and distance or volume measurement function is em
Following the half-day lecture, the participants are divided into five or six groups (4-5 participants/group). Each participant receives hands-on training for 30 min under the supervision of experienced US physicians (5 min each for liver, biliary system, pancreas, vascular system, digestive tract, and lungs) with both a high-end machine and a pocked-sized US device for comparison. The abdomen is generally observed by a medium frequency transducer (Figure 8), and the pleura is observed by a high-frequency linear probe with a focus on pleura (Figure 9)[28-32]. All instructors are certified as registered Senior Medical Sonographers and fellowship-obtained highly diagnostic doctors of the Japan Society of Ultrasonics in Medicine. The participants are required to register in advance because the numbers of instructors and US machines are limited.
After the seminar, participants answer a questionnaire to determine whether: (1) The 1-d seminar was useful; (2) The lecture on basic US physics helped in under
There are a wide range of possible applications for pocket-sized US devices in offering advanced diagnostic capability to benefit patient care in the clinical setting. They include the following situations.
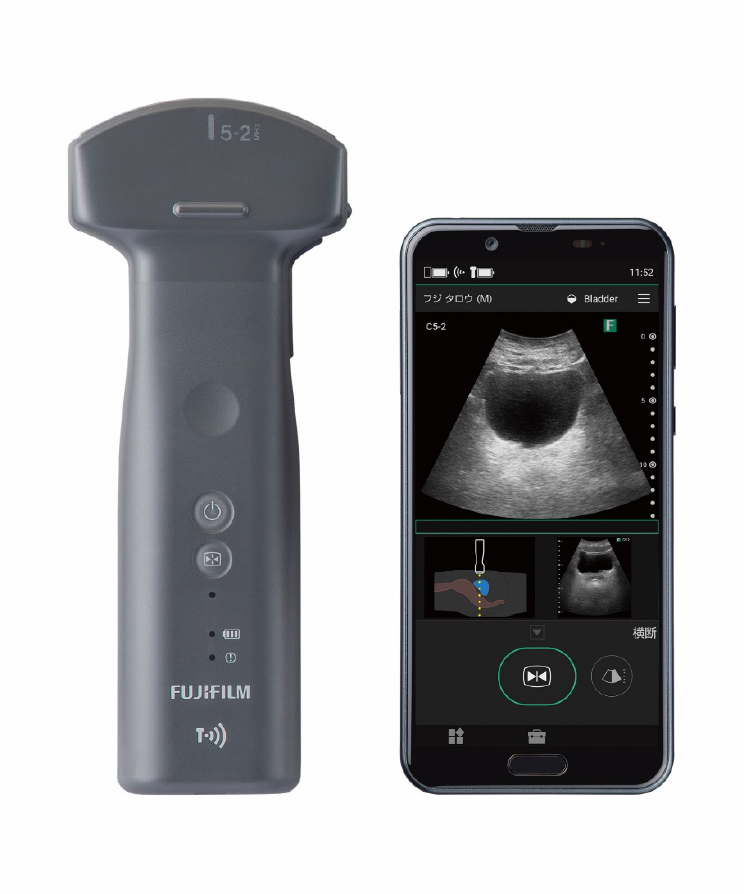
Due to recent advances in US technology and informatics, wireless probes are now a reality (Figure 14). Remote telesonography has the potential to improve the quality of patient care. Pocket-sized US devices are particularly important in situations where the time of examination is urgent (emergency room, intensive care) or the location favors the use of pocket-sized devices (remote locations)[33,34]. More advanced technologies will guarantee rapid transfer of US information to hospitals to provide the best medical care. Becoming wireless is a meaningful function[35]. Furthermore, remote telesonography will improve the quality of US applications in underserved communities[36]. Lesser trained examiners will be able to obtain and interpret US images that impact patient care immediately[37].
Clinicians at outpatient clinics see a range of abdominal problems. The differential diagnosis includes digestive tract, hepatobiliary and pancreatic diseases, and gynecological and urogenital diseases. Portable US provides clinically significant visual information that is not obtainable by physical examination and helps decrease the diagnosis time[38,39].
The biggest advantage of pocket-sized US devices is the time savings (booting time, transfer, bedside positioning). The most useful function of portable US is the global estimation of fluid volume (ascites, pleural effusion, pericardial effusion) under drug therapy[4]. Pocket-sized US may be repeated due to clinical need but is typically performed for monitoring physiologic or pathologic changes of admitted patients[40]. In addition, US-guided procedures provide safety to a wide variety of punctures (ascites, bile duct, abscess) (Figure 13).
Decontamination assessment must never be compromised. Some recent studies have shown that pocket-sized US performed efficiently as a tool for screening a variety of diseases[16,20,29,30,34,41]. The pocket-sized US devices were also used successfully by other healthcare providers, such as nurses and physical therapists. Additionally, pocket-sized US may be feasible for guiding aspiration needles for the drainage of abscesses, ascites aspiration, etc.
The compact size of the pocket-sized US device makes it possible to carry in a doctor bag when visiting patients[4,42,43]. The clinicians feel confident using the pocket-sized US when caring for patients in limited medical conditions[44]. Physicians proficient in its use can quickly answer specific questions at the bedside[45].
In this review, we have presented our 1-d method for implementation of pocket-sized US into the clinical setting. The biannual nature of the seminar is insufficient for completely integrating the pocket-sized US device into frequent clinical use. However, this method contributes to new residents gaining confidence in using the pocket-sized US despite the skill gap remaining. However, there are many limitations. There are a small number of US experts who can correctly and efficiently teach US physics and abdominal anatomy to new doctors and supervise their hands-on training. The ”teach-the-teacher” system is important for training new US practitioners[46,47]. Costs related to US equipment may present additional (and the most important) obstacles to develop and continue pocket-sized US training programs. We recommend that all the US leaders and experts find the means to integrate pocket- sized US into clinical setting through the training of new clinicians.
Manuscript source: Invited manuscript
Specialty type: Medical laboratory technology
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Deshwal H S-Editor: Fan JR L-Editor: A P-Editor: Wang LYT
| 1. | Nie P, Li Y, Zhang N, Sun X, Xin B, Wang Y. The change and correlates of healthy ageing among Chinese older adults: findings from the China health and retirement longitudinal study. BMC Geriatr. 2021;21:78. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 22] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 2. | Hagen-Ansert SL. Introduction to physical findings, physiology, and laboratory data. In: Hagen-Ansert SL. Textbook of diagnostic sonography. St. Louis: Elsevier-Mosby, 2006: 21-35. |
| 3. | Hagen-Ansert SL. Introduction to abdominal scanning: technique and protocols. In: Hagen-Ansert SL. Textbook of diagnostic sonography. St. Louis: Elsevier-Mosby, 2006: 132-164. |
| 4. | European Society of Radiology (ESR). ESR statement on portable ultrasound devices. Insights Imaging. 2019;10:89. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 45] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 5. | Weil FS. Examination methods and positioning. In: Weil FS. Ultrasound diagnosis of digestive diseases. Berlin: Springer-Cerlag, 1990: 37-42. |
| 6. | Stengel D, Rademacher G, Ekkernkamp A, Güthoff C, Mutze S. Emergency ultrasound-based algorithms for diagnosing blunt abdominal trauma. Cochrane Database Syst Rev. 2015;CD004446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 41] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 7. | Galusko V, Khanji MY, Bodger O, Weston C, Chambers J, Ionescu A. Hand-held Ultrasound Scanners in Medical Education: A Systematic Review. J Cardiovasc Ultrasound. 2017;25:75-83. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 37] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 8. | Kobal SL, Trento L, Baharami S, Tolstrup K, Naqvi TZ, Cercek B, Neuman Y, Mirocha J, Kar S, Forrester JS, Siegel RJ. Comparison of effectiveness of hand-carried ultrasound to bedside cardiovascular physical examination. Am J Cardiol. 2005;96:1002-1006. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 256] [Cited by in RCA: 258] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 9. | Paddock MT, Bailitz J, Horowitz R, Khishfe B, Cosby K, Sergel MJ. Disaster response team FAST skills training with a portable ultrasound simulator compared to traditional training: pilot study. West J Emerg Med. 2015;16:325-330. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 10. | Stengel D, Bauwens K, Rademacher G, Ekkernkamp A, Güthoff C. Emergency ultrasound-based algorithms for diagnosing blunt abdominal trauma. Cochrane Database Syst Rev. 2013;CD004446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 11. | Yamada M, Hasegawa Y, Yamashiro S, Sekine M, Asano Y, Fujinami H. Assessment of a Hands-On Seminar on Gastrointestinal Ultrasound. Healthcare (Basel). 2020;8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 12. | Kim EY, Park KH, Choi SJ, Chung WJ. Educational value of pocket-sized ultrasound devices to improve understanding of ultrasound examination principles and sonographic anatomy for medical student. PLoS One. 2017;12:e0185031. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Prosch H, Radzina M, Dietrich CF, Nielsen MB, Baumann S, Ewertsen C, Jenssen C, Kabaalioğlu A, Kosiak W, Kratzer W, Lim A, Popescu A, Mitkov V, Schiavone C, Wohlin M, Wüstner M, Cantisani V. Ultrasound Curricula of Student Education in Europe: Summary of the Experience. Ultrasound Int Open. 2020;6:E25-E33. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 45] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 14. | Celebi N, Griewatz J, Malek NP, Krieg S, Kuehnl T, Muller R, Pauluschke-Fröhlich J, Debove I, Riessen R, Zipfel S, Fröhlich E. Development and implementation of a comprehensive ultrasound curriculum for undergraduate medical students - a feasibility study. BMC Med Educ. 2019;19:170. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 34] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 15. | Baribeau Y, Sharkey A, Chaudhary O, Krumm S, Fatima H, Mahmood F, Matyal R. Handheld Point-of-Care Ultrasound Probes: The New Generation of POCUS. J Cardiothorac Vasc Anesth. 2020;34:3139-3145. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 139] [Article Influence: 27.8] [Reference Citation Analysis (0)] |
| 16. | Kimori K, Tamura Y. Feasibility of Using a Pocket-Sized Ultrasound Device to Measure the Inferior Vena Cava Diameter of Patients With Heart Failure in the Community Setting: A Pilot Study. J Prim Care Community Health. 2020;11:2150132720931345. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Rykkje A, Carlsen JF, Nielsen MB. Hand-Held Ultrasound Devices Compared with High-End Ultrasound Systems: A Systematic Review. Diagnostics (Basel). 2019;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 67] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 18. | Parsons C, Khan KA, Pink J, Verran A, Griffiths F, Hutchinson CE, Petrou S. Preferences for portable ultrasound devices: a discrete choice experiment among abdominal aortic aneurysm surveillance patients and general ultrasound patients in England. BMJ Open. 2018;8:e025428. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 19. | Prabhu SJ, Kanal K, Bhargava P, Vaidya S, Dighe MK. Ultrasound artifacts: classification, applied physics with illustrations, and imaging appearances. Ultrasound Q. 2014;30:145-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 20. | Smit MR, de Vos J, Pisani L, Hagens LA, Almondo C, Heijnen NFL, Schnabel RM, van der Horst ICC, Bergmans DCJJ, Schultz MJ, Bos LDJ; DARTS Consortium. Comparison of Linear and Sector Array Probe for Handheld Lung Ultrasound in Invasively Ventilated ICU Patients. Ultrasound Med Biol. 2020;46:3249-3256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 21. | Zagzebski JA. Physics of diagnostic ultrasound. In: Zagzenbski JA. Essentials of ultrasound physics. St. Louis, Missouri: Mosby-year book, 1996: 1-19. |
| 22. | Hagen-Ansert SL. The liver. In: Hagen-Ansert SL. The textbook of diagnostic ultrasonography. Saint-Louis: Elsevier, 2012: 205-266. |
| 23. | Hagen-Ansert SL. The gallbladder and the biliary system. In: Hagen-Ansert SL. The textbook of diagnostic ultrasonography. Saint-Louis: Elsevier, 2012: 267-299. |
| 24. | Levine D. Overview of obstetric imaging. In: Rumack CM, Levine D. Diagnostic ultrasound. Philadelphia: Elsevier, 2011: 1015-1033. |
| 25. | Merali HS, Tessaro MO, Ali KQ, Morris SK, Soofi SB, Ariff S. A novel training simulator for portable ultrasound identification of incorrect newborn endotracheal tube placement - observational diagnostic accuracy study protocol. BMC Pediatr. 2019;19:434. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 26. | Chen SC, Chen PY, Chen GC, Chuang SY, Tzeng IS, Lin SK. Portable Bladder Ultrasound Reduces Incidence of Urinary Tract Infection and Shortens Hospital Length of Stay in Patients With Acute Ischemic Stroke. J Cardiovasc Nurs. 2018;33:551-558. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 27. | Convissar D, Bittner EA, Chang MG. Biplane Imaging Using Portable Ultrasound Devices for Vascular Access. Cureus. 2021;13:e12561. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 28. | Tasci O, Hatipoglu ON, Cagli B, Ermis V. Sonography of the chest using linear-array vs sector transducers: Correlation with auscultation, chest radiography, and computed tomography. J Clin Ultrasound. 2016;44:383-389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 29. | Bennett D, De Vita E, Mezzasalma F, Lanzarone N, Cameli P, Bianchi F, Perillo F, Bargagli E, Mazzei MA, Volterrani L, Scolletta S, Valente S, Franchi F, Frediani B, Sestini P. Portable Pocket-Sized Ultrasound Scanner for the Evaluation of Lung Involvement in Coronavirus Disease 2019 Patients. Ultrasound Med Biol. 2021;47:19-24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 34] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 30. | Rajendram R, Hussain A, Mahmood N, Kharal M. Feasibility of using a handheld ultrasound device to detect and characterize shunt and deep vein thrombosis in patients with COVID-19: an observational study. Ultrasound J. 2020;12:49. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 31. | Bitar ZI, Shamsah M, Maadarani O, Bamasood OM, Bitar AZ, Alfoudri H. Lung Ultrasound and Sonographic Subpleural Consolidation in COVID-19 Pneumonia Correlate with Disease Severity. Crit Care Res Pract. 2021;2021:6695033. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 32. | Lieveld AWE, Kok B, Schuit FH, Azijli K, Heijmans J, van Laarhoven A, Assman NL, Kootte RS, Olgers TJ, Nanayakkara PWB, Bosch FH. Diagnosing COVID-19 pneumonia in a pandemic setting: Lung Ultrasound versus CT (LUVCT) - a multicentre, prospective, observational study. ERJ Open Res. 2020;6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 41] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 33. | Rominger AH, Gomez GAA, Elliott P. The implementation of a longitudinal POCUS curriculum for physicians working at rural outpatient clinics in Chiapas, Mexico. Crit Ultrasound J. 2018;10:19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 34. | Burleson SL, Swanson JF, Shufflebarger EF, Wallace DW, Heimann MA, Crosby JC, Pigott DC, Gullett JP, Thompson MA, Greene CJ. Evaluation of a novel handheld point-of-care ultrasound device in an African emergency department. Ultrasound J. 2020;12:53. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 35. | Marsh-Feiley G, Eadie L, Wilson P. Telesonography in emergency medicine: A systematic review. PLoS One. 2018;13:e0194840. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 31] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 36. | Constantinescu EC, Nicolau C, Săftoiu A. Recent Developments in Tele-Ultrasonography. Curr Health Sci J. 2018;44:101-106. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 37. | Karako K, Song P, Chen Y, Tang W. Realizing 5G- and AI-based doctor-to-doctor remote diagnosis: opportunities, challenges, and prospects. Biosci Trends. 2020;14:314-317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 38. | Adelman S, Fishman P. Use of portable ultrasound machine for outpatient orthopedic diagnosis: an implementation study. Perm J. 2013;17:18-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 39. | Van Der Wal S, Robson SJ, Choong S. Is bedside ultrasound now a routine part of specialist obstetrics and gynaecology outpatient consultation? Australas J Ultrasound Med. 2013;16:190-192. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 40. | Falgarone G, Pamoukdjian F, Cailhol J, Giocanti-Auregan A, Guis S, Bousquet G, Bouchaud O, Seror O. Lung ultrasound is a reliable diagnostic technique to predict abnormal CT chest scan and to detect oxygen requirements in COVID-19 pneumonia. Aging (Albany NY). 2020;12:19945-19953. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 41. | Özdemir U, Çimen M, Güney T, Gürsel G. Validity and reliability of pocket-sized ultrasound devices in measurement of optic nerve sheath diameter in ICU patients. J Clin Monit Comput. 2020;34:597-605. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 42. | Miceli L, Dal Mas F, Biancuzzi H, Bednarova R, Rizzardo A, Cobianchi L, Holmboe ES. Doctor@Home: Through a Telemedicine Co-production and Co-learning Journey. J Cancer Educ. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 43. | Peng S, Micks T, Braganza D, Sue K, Woo M, Rogers P, Freedman S, Lewis J, Hu S, Varner C, Patel N, Hameed S, Steinmetz P. Canadian national survey of family medicine residents on point-of-care ultrasound training. Can Fam Physician. 2019;65:e523-e530. [PubMed] |
| 44. | Pivetta E, Girard E, Locascio F, Lupia E, Martin JD, Stone M. Self-Performed Lung Ultrasound for Home Monitoring of a Patient Positive for Coronavirus Disease 2019. Chest. 2020;158:e93-e97. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 45. | Aminlari A, Quenzer F, Hayden S, Stone J, Murchison C, Campbell C. A Case of Covid-19 Diagnosed at Home With Portable Ultrasound and Confirmed With Home Serology Test. J Emerg Med. 2021;60:399-401. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 46. | Cantisani V, Dietrich CF, Badea R, Dudea S, Prosch H, Cerezo E, Nuernberg D, Serra AL, Sidhu PS, Radzina M, Piscaglia F, Bachmann Nielsen M, Ewertsen C, Săftoiu A, Calliada F, Gilja OH. EFSUMB Statement on Medical Student Education in Ultrasound [long version]. Ultrasound Int Open. 2016;2:E2-E7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 65] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 47. | Dietrich CF, Hoffmann B, Abramowicz J, Badea R, Braden B, Cantisani V, Chammas MC, Cui XW, Dong Y, Gilja OH, Hari R, Nisenbaum H, Nicholls D, Nolsøe CP, Nürnberg D, Prosch H, Radzina M, Recker F, Sachs A, Saftoiu A, Serra A, Sweet L, Vinayak S, Westerway S, Chou YH, Blaivas M. Medical Student Ultrasound Education: A WFUMB Position Paper, Part I. Ultrasound Med Biol. 2019;45:271-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 97] [Article Influence: 16.2] [Reference Citation Analysis (0)] |