Published online Jul 20, 2021. doi: 10.5662/wjm.v11.i4.110
Peer-review started: October 22, 2020
First decision: November 25, 2020
Revised: December 20, 2020
Accepted: May 20, 2021
Article in press: May 20, 2021
Published online: July 20, 2021
Processing time: 270 Days and 1.2 Hours
As quality and cost effectiveness become essential in clinical practice, an evidence-based evaluation of the utility of imaging orders becomes an important consideration for radiology’s value in patient care. We report an institutional quality improvement project including a retrospective review of utility of sacrum mag
Core Tip: Sacrum magnetic resonance studies ordered for low back pain were suspected to lack clinical utility at our institution. A literature review demonstrated a lack of evidence based practice in ordering of this study for low back/tail bone pain. A quality project was then pursued to first assess the clinical usefulness of the study. Over four years these studies had no major impacts on management. An educational component of the quality project was then pursued with a rapid decrease in the number of studies ordered by referring providers.
- Citation: Castillo S, Joodi R, Williams LE, Pezeshk P, Chhabra A. Sacrum magnetic resonance imaging for low back and tail bone pain: A quality initiative to evaluate and improve imaging utility. World J Methodol 2021; 11(4): 110-115
- URL: https://www.wjgnet.com/2222-0682/full/v11/i4/110.htm
- DOI: https://dx.doi.org/10.5662/wjm.v11.i4.110
Magnetic resonance imaging (MRI) of the sacrum ordered for vague low back pain and tail bone pain was seen with some frequency at our institution over the last decade and with little evidence on its clinical value as subjectively reported by our radiologists. The American College of Radiology (ACR) Appropriateness Criteria does not include sacrum imaging in its reviews for low back pain indication[1]. The ACR Appropriateness Criteria does however recommend sacral MR imaging in patients with chronic low back pain, symptoms of inflammatory arthropathy, and negative or equivocal radiographs[2]. Recommendations from the American College of Physicians and the American Pain Society also state that imaging should not be obtained in uncomplicated back pain without neurologic symptoms unless history or physical examination suggest a specific underlying etiology[3]. In fact, increases in imaging in low back pain have been associated with increases in procedures for low back pain without improvement in outcomes—a finding highly suggestive of overutilization[4,5]. Coccydynia (or tail bone pain) has many similar underlying etiologies to low back pain, including muscular, post traumatic, and degenerative etiologies[6,7]. Treatment options also bear similarity to those available in patients with low back pain, including surgical and local therapeutic options based on the underlying pathology[6,8]. However, conservative treatments including physical therapies are effective treatments and often the most appropriate therapy in patients affected by these conditions[6,8,9].
While adherence to guidelines recommending physical therapy in low back pain can decrease long term health care costs and unnecessary procedures, it has also been postulated that up to 5% of low back pain suffers could have some degree of inflammatory arthropathy[9,10]. The clinicians ordering these exams might want to exclude a serious and clinically meaningful diagnosis.
It is thus clear that a specific systematic review of these orders in the setting of low back pain would be of use to determine the true value of this imaging order and examination in the clinical practice. Literature on the usefulness of these orders in the absence of known recent trauma, infection or neoplastic etiologies is currently lacking, resulting in an interest in determining if these orders contribute to a meaningful alteration of the patient care. This project was a quality improvement and practice management project, which entailed retrospective imaging and electronic patient chart reviews, focused provider education and post-intervention assessment to evaluate the impact of such procedures.
Sacrum MRI orders and examinations at our institution from 2013-2017 were retrospectively reviewed. Sacrum MR orders were identified through the PACS (picture archiving and communications system, Mckesson, Alpharetta, GA, United States), identifying 322 unique patients with sacrum MRI orders over this time period.
Orders for already known diagnosis of inflammatory arthritis, concern for infection (osteomyelitis), known or suspected tumor, recent trauma (< 4 wk) and concern for occult fracture were excluded from further review, leaving 98 studies performed over this time period. All studies had an indication of low back pain and/or tail bone pain as described by the ordering physician/provider without indicating specific suspected etiology of pain.
Imaging, radiology reports, and patient charts were reviewed by a radiology resident and/or musculoskeletal imaging fellow for included patients to evaluate for major, minor, and incidental findings, as well as major or minor impact on the patient diagnosis and care. Major findings were defined as those that may have been a cause of patient’s pain and could potentially be acted upon, particularly inflammatory spondyloarthropathy. Minor findings were findings felt to be unlikely the cause of patient’s symptoms, routine degenerative changes without evidence of inflammation, or seen on concurrent exam. Incidental findings were felt not to be related to patient’s symptoms and/or would be better evaluated by a different exam and/or modality of imaging. MRIs positive for major findings were reviewed by two expert subspecialty musculoskeletal radiologists with 4 and 10 years of post-fellowship attending ex
The current process map for patients who present to their clinicians with low back pain and/or tail bone pain was evaluated with electronic chart reviews. Ordering providers were from multiple different clinics in the hospital system. Imaging evaluation usually started with lumbar spine, sacral or sacroiliac (SI) joint or pelvic X-rays. The interpreting radiologist qualitatively described degenerative findings of the spine, SI joints or hip joints and/or chronic pelvic enthesophytes of trochanters and ischial tuberosities, all common findings. Sacrum MRIs were then ordered for further evaluation for many reasons including chronic but increasing low back/tail bone symptoms, partially obscured sacrum on radiographs due to bowel shadows, psychological factors, no response to initial conservative treatment, imaging prior to caudal blocks, and lack of defined appropriateness criteria for tail bone pain. It was determined that the strategy that would most likely impact the patient care would involve presentation of results of the above retrospective imaging and chart reviews with focused teaching of the referring clinicians who ordered most of these examinations.
The results were tabulated with frequencies of findings identified from the imaging and chart reviews, completed in June 2018. Impact on patient care was inferred from the electronic chart reviews, treatments patients received and their follow-up procedures. Powerpoint (Microsoft, Redwood, Seattle) presentations were generated on preliminary findings and presented at the department meeting of family medicine in April 2018. The presentations were also distributed to the clinicians at the care centers ordering most of these examinations as continuing education.
Finally, sacrum MRIs were again identified through the same methods over a 3-mo period after the distribution of the teaching materials, and the results were tabulated.
The frequencies were tabulated as percentages. No P values were generated due to clearly successful intervention.
There were 98 MRIs of the sacrum that met the inclusion criteria. The included patients were 65% female, with a mean 48.1 years of age. All included studies were non-contrast examinations. Majority of cases (85/98) had incidental findings including lumbar spine degeneration (often seen on concurrently performed lumbar spine MRIs, which were performed in 65 of the 98 studies) and incidental visceral findings in the pelvis such as incidental uterine fibroids and partially visualized renal lesions.
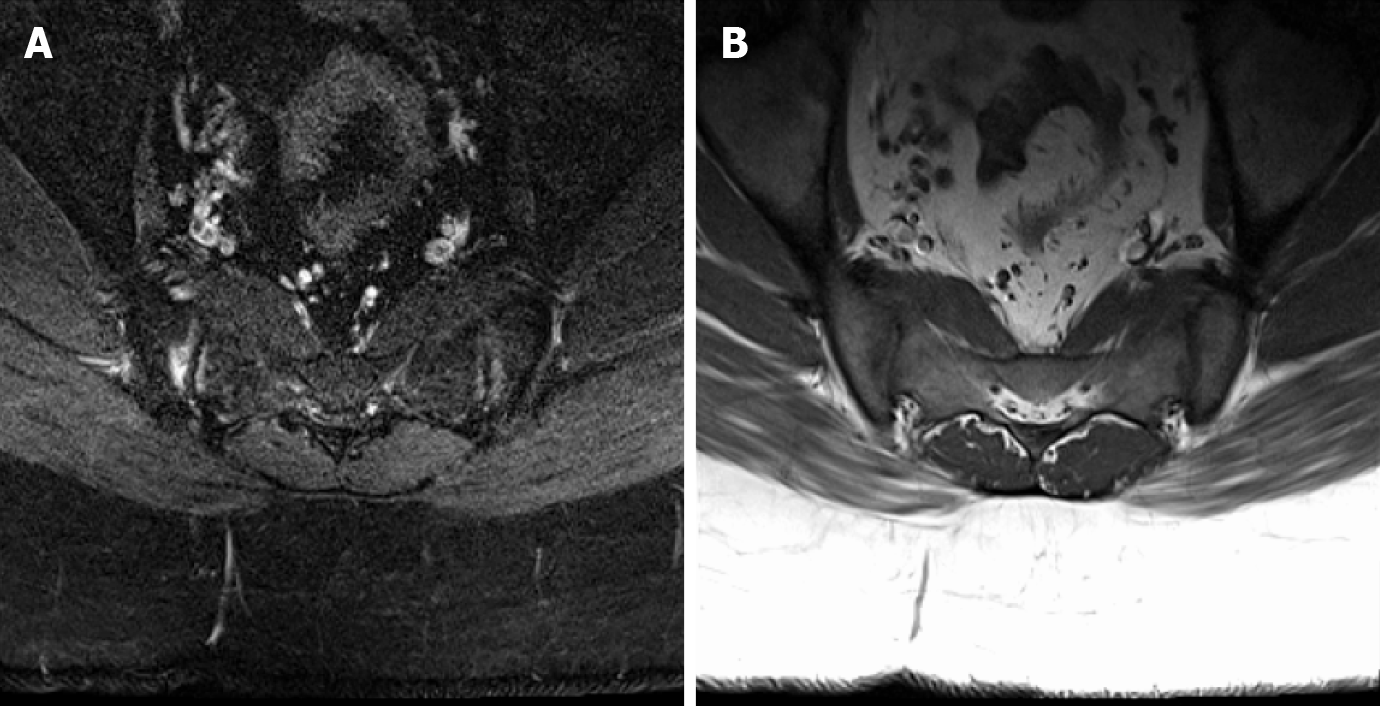
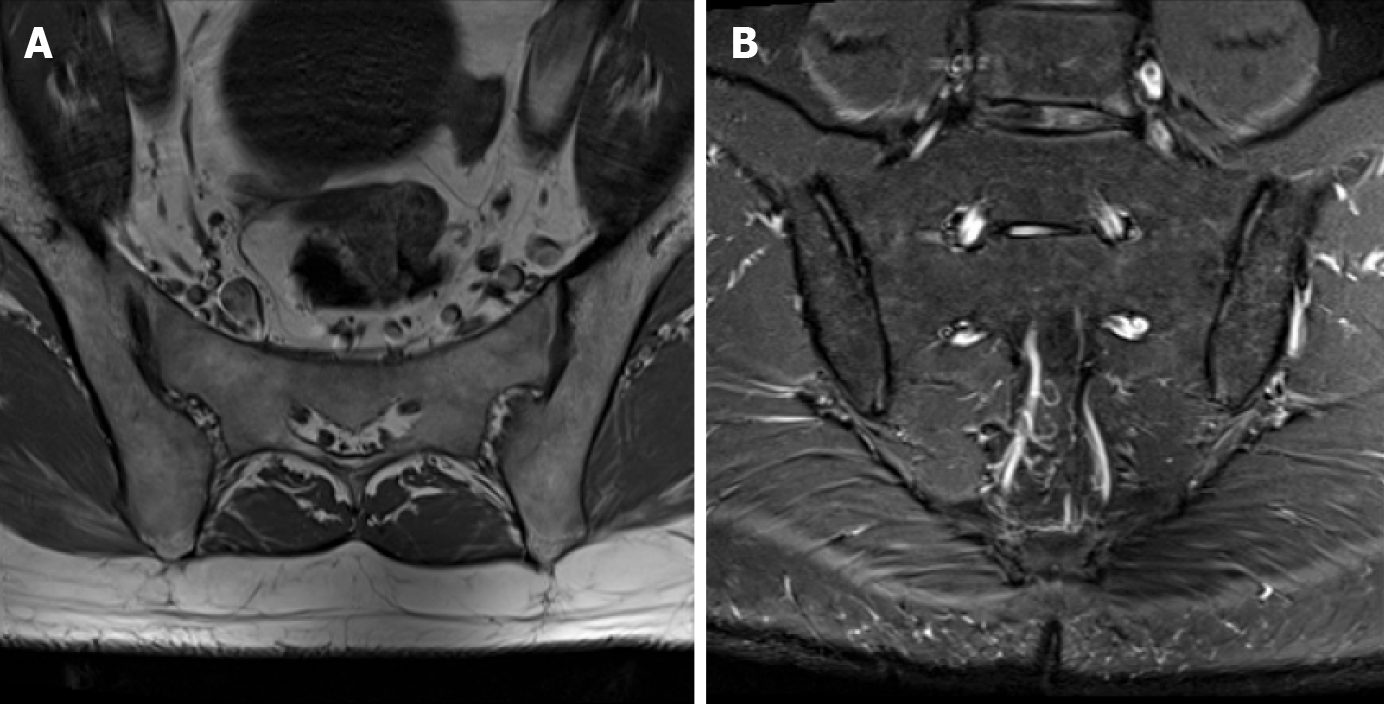
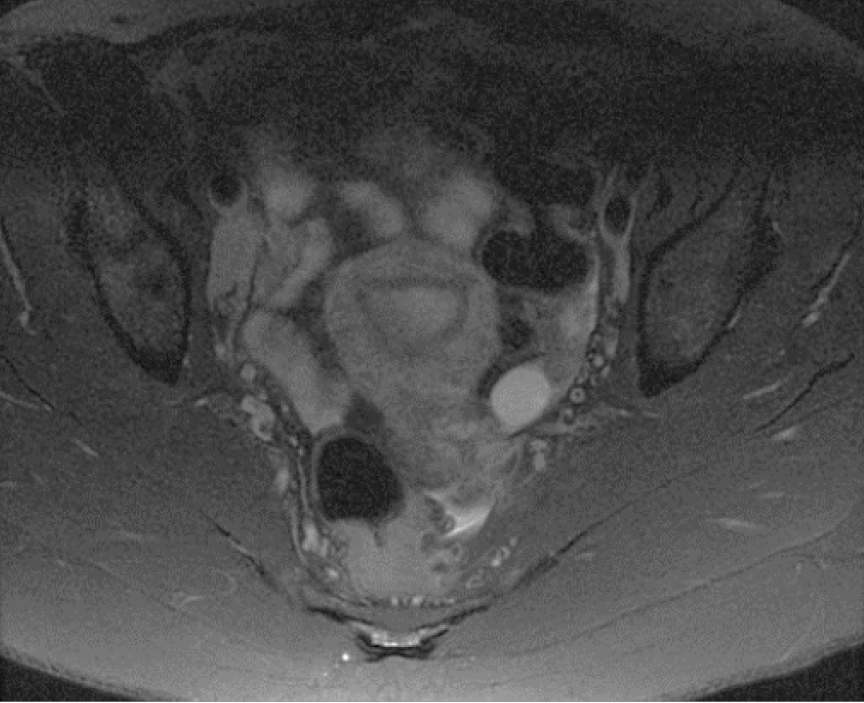
Two patients had a major change in diagnosis based on Sacral MR findings, one with acute SI inflammation and one with chronic inflammation. Forty-three patients had minor findings such as SI degenerative disease, Tarlov cysts, or old post-traumatic changes of the sacrum/coccyx. Of these patients with changes in diagnosis, 12 patients had minor changes in management, which included surgical referrals for degenerative disease and further imaging of incidental or minor findings. No major changes in management occurred as a result these examinations (Figure 1-3).
At the above rate, based on current charges for sacrum MRI examination at our institution ($4900 per MRI sacrum without contrast), patients were charged a total of $480200 for two major findings, no major changes in management, and only 12 minor changes in management. This doesn’t include costs of their travel times, parking, time away from work, increased clinic visits for management of minor or incidental findings, patient anxiety and discomfort from MRIs, etc.
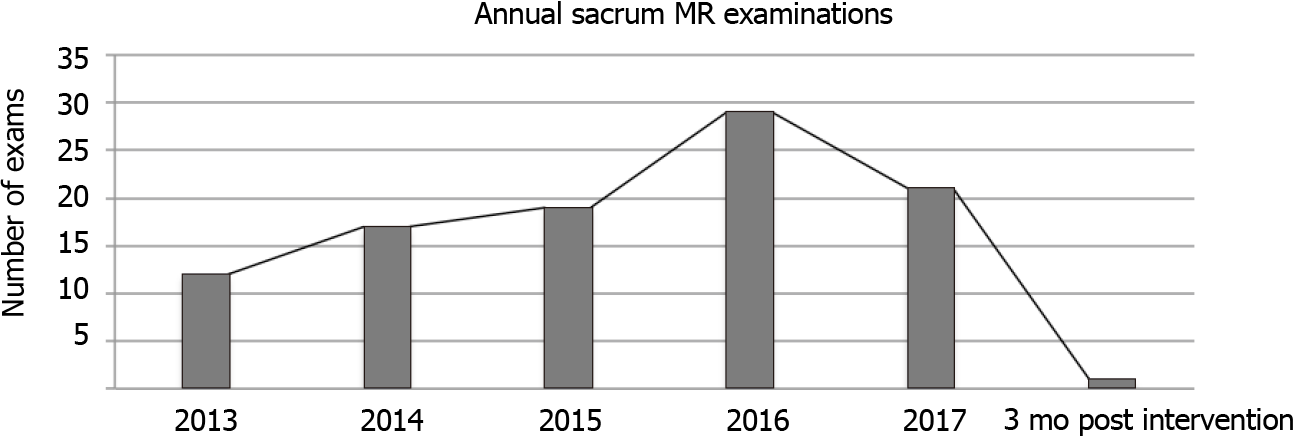
Post-intervention, during 3-mo follow-up, only 1 study meeting the inclusion criteria had been ordered and this was also negative for major or minor findings or any changes in management. This is less than the expected 2 exams per month average over the duration of the pre-intervention period, suggesting a positive impact on clinician ordering patterns. We hope to add this in the decision support software used by the ordering physicians at our institute with best practice alerts if there is no history of known tumor, recent trauma, infection, or spondyloarthritis (Figure 4).
Sacrum MRI at our institution was overall found to be an inefficient method of diagnosis of low back or tailbone pain, not lending itself to cost effectiveness or significant impact on patient care. This further strengthens the argument that advanced imaging should be avoided in favor of conservative therapies in patients with vague low back pain without neurologic symptoms or other clinical red flags (such as recent trauma or malignancy)[7,8]. Physician education led to at least a short-term decrease in frequency of these orders by approximately 83%, effectively saving $24500 over a 3-mo time period. In future, similar studies at other institutions may be helpful to confirm minimal, if any utility of sacral MR imaging in low back and/or tail bone pain.
Our findings add to the literature supporting clinician decision making when deciding to pursue conservative therapies in patients with low back or tail bone pain prior to imaging, as well as supporting literature which indicates this reduces health care cost. Additionally, our project supports the utility of clinician education and communi
Due to the nature of this retrospective review, we couldn’t evaluate the referring physician or patient factors driving the need for sacrum MRI examinations during their management, or the satisfaction they obtained from the positive or negative results. The negative predictive value of such examinations may also play a role in the alleviation of patient concerns of something unknown or significant that may be causing their symptoms. Eliminating redundant procedures and unnecessary diagnostic services, such as costly advanced imaging examinations is however in line with the strategy of best practice management while simultaneously decreasing health care costs and increasing patient care quality and medical efficiency.
Future research is needed to confirm similar lack of changes in clinical management based on sacral MRI in additional institutions. Furthermore, long term analysis of clinician response to education is needed as this may have a dampened effect over time.
Manuscript source: Invited manuscript
Specialty type: Medical laboratory technology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Leung PC S-Editor: Gao CC L-Editor: A P-Editor: Yuan YY
| 1. | Patel ND, Broderick DF, Burns J, Deshmukh TK, Fries IB, Harvey HB, Holly L, Hunt CH, Jagadeesan BD, Kennedy TA, O'Toole JE, Perlmutter JS, Policeni B, Rosenow JM, Schroeder JW, Whitehead MT, Cornelius RS, Corey AS. ACR Appropriateness Criteria Low Back Pain. J Am Coll Radiol. 2016;13:1069-1078. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 123] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 2. | Expert Panel on Musculoskeletal Imaging; Bernard SA; Kransdorf MJ, Beaman FD, Adler RS, Amini B, Appel M, Arnold E, Cassidy RC, Greenspan BS, Lee KS, Tuite MJ, Walker EA, Ward RJ, Wessell DE, Weissman BN. ACR Appropriateness Criteria® Chronic Back Pain Suspected Sacroiliitis-Spondyloarthropathy. J Am Coll Radiol. 2017;14:S62-S70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 3. | Chou R, Qaseem A, Snow V, Casey D, Cross JT Jr, Shekelle P, Owens DK; Clinical Efficacy Assessment Subcommittee of the American College of Physicians; American College of Physicians; American Pain Society Low Back Pain Guidelines Panel. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147:478-491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1876] [Cited by in RCA: 1678] [Article Influence: 93.2] [Reference Citation Analysis (0)] |
| 4. | Flynn TW, Smith B, Chou R. Appropriate use of diagnostic imaging in low back pain: a reminder that unnecessary imaging may do as much harm as good. J Orthop Sports Phys Ther. 2011;41:838-846. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 104] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 5. | Schroth WS, Schectman JM, Elinsky EG, Panagides JC. Utilization of medical services for the treatment of acute low back pain: conformance with clinical guidelines. J Gen Intern Med. 1992;7:486-491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 48] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 6. | Lirette LS, Chaiban G, Tolba R, Eissa H. Coccydynia: an overview of the anatomy, etiology, and treatment of coccyx pain. Ochsner J. 2014;14:84-87. [PubMed] |
| 7. | Skalski MR, Matcuk GR, Patel DB, Tomasian A, White EA, Gross JS. Imaging Coccygeal Trauma and Coccydynia. Radiographics. 2020;40:1090-1106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 8. | Hanney WJ, Masaracchio M, Liu X, Kolber MJ. The Influence of Physical Therapy Guideline Adherence on Healthcare Utilization and Costs among Patients with Low Back Pain: A Systematic Review of the Literature. PLoS One. 2016;11:e0156799. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 78] [Cited by in RCA: 68] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 9. | Scott KM, Fisher LW, Bernstein IH, Bradley MH. The Treatment of Chronic Coccydynia and Postcoccygectomy Pain With Pelvic Floor Physical Therapy. PM R. 2017;9:367-376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 10. | Underwood MR, Dawes P. Inflammatory back pain in primary care. Br J Rheumatol. 1995;34:1074-1077. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 130] [Article Influence: 4.3] [Reference Citation Analysis (0)] |