Copyright
©The Author(s) 2017.
World J Methodol. Dec 26, 2017; 7(4): 117-128
Published online Dec 26, 2017. doi: 10.5662/wjm.v7.i4.117
Published online Dec 26, 2017. doi: 10.5662/wjm.v7.i4.117
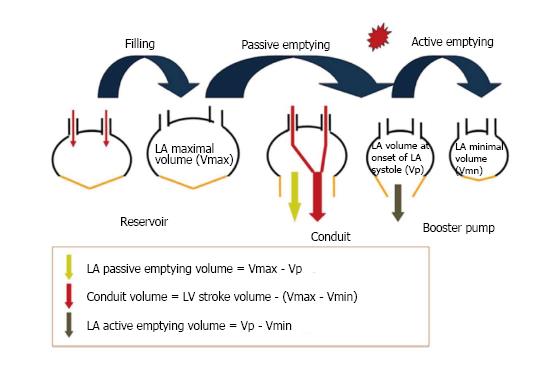
Figure 1 Phases of left atrial function.
Left atrial preload is determined by blood flowing from the pulmonary vein. In this initial filling phase the LA acts a reservoir storing blood during left ventricular systole against a closed mitral valve. During LV diastole, diastasis and as the mitral valve opens it acts as a conduit, passively using stored energy to empty into the LV. Finally, in LV end diastole the LA contracts and actively empties blood completing the LV filling cycle. Reprinted from Karayannis et al[21], with permission of the publisher (Copyright © 2007, Springer Science + Business Media. Authorization for this adaptation has been obtained both from the owner of the copyright in the original work and from the owner of copyright in the translation or adaptation). LA: Left atrial; LV: Left ventricle; Vp: Left atrial volume before atrial contraction; Vmax: Maximal volume (as defined at left ventricular end-systolic phase); Vmin: Left atrial minimal volume (as defined at left ventricular end-diastolic phase).
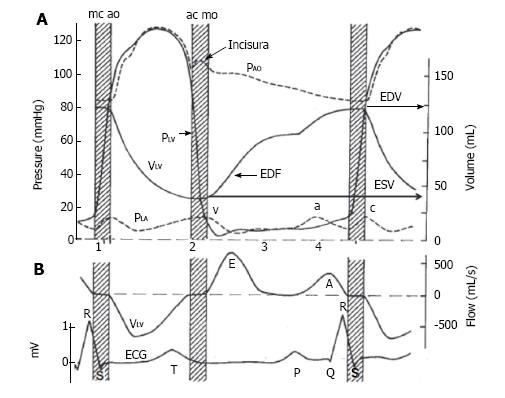
Figure 2 Describes the volume and flow relationships in the left atrium and left ventricle throughout one cardiac cycle, i.
e., systole and diastole. A: Pressure (P) and volume (V) are presented for the Aorta (Ao), left atrium (LA) and left ventricle (LV). Systole: During the early phase between mitral valve closure (mc) and aortic valve opening (ao) is the isovolumic contraction phase (stripped bar), where there is increase in PLV (solid line) without change in VLV (solid line). This is followed by ventricular contraction with a rise in PLV and PAO (upper dashed line), that peaks mid cycle, and a reduction in VLV. Diastole: At the end of LV contraction, and when the PLV is lower than the aorta the aortic valve closes (ac), followed by a period of isovolumic LV relaxation (stripped bar), where there is reduction in PLV without a change in VLV. The Incisura or dicrotic notch describes the small backflow of blood into the LV. Early diastolic point of early diastolic filling. In diastole PLA is generated early by the reservoir and conduit atrial function (v wave - lower dashed line) and corresponds with early diastolic filling (EDF) and a late atrial contraction or booster function (a wave) and contributes to late diastolic filling. Ventricular volumes are as end diastolic or end systolic (EDV or ESV; solid line). Cardiac sounds are shown as 1-4; B: Diagram showing relationship between electrical conduction and blood flow with an additional catheter in the LV. Systolic blood flow out of the ventricle (V LV), is followed by early diastolic blood flow into the LV (E wave), bate blood flow into the LV during LA contraction (A wave). A standard ECG lead II shows LA depolarization, LV depolarization, and LV repolarization (P wave, QRS complex, and T wave, respectively) (Published in Ref 28, figure provided courtesy of Dr. John V. Tyberg and Dr. Henk E. D. J. ter Keurs. Permission required). ECG: Electrocardiogram.
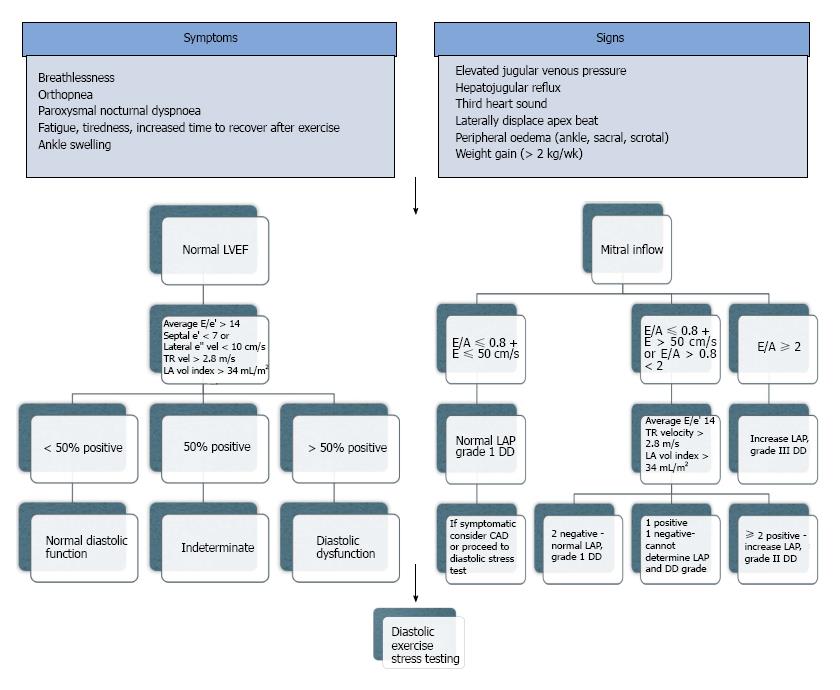
Figure 3 How to diagnose heart failure with preserved ejection fraction.
From the 2016 consensus statements of HF, the diagnosis of HF requires 4 important factors: (1) the presence of symptoms and/or signs of HF; (2) a “preserved” EF (defined as LVEF ≥ 50% or 40%-49% for HfmrEF; (3) elevated levels of natriuretic peptides (BNP > 35 pg/mL and/or NT-proBNP > 125 pg/mL); (4) objective evidence of other cardiac functional and structural alterations underlying HF; and (5) In case of uncertainty, a stress test or invasively measured elevated LV filling pressure may be needed to confirm the diagnosis. However in clinical practice many patients present predominately with a symptom such as SOB. The new guidelines are a positive step forward, and the authors for the first time acknowledged LA size, a surrogate for chronically elevated LVEDP and LA dysfunction. They fall short however as there are confounders for the abnormalities and none of the factors can be conclusively correlated to symptoms, where exercise testing could. A: Atrial filling velocity; BNP: Brain natriuretic peptides; E: Early filling velocity; e’: Early mitral annular tissue doppler velocity; EF: Ejection fraction; HfmrEF: Heart failure mid-range ejection fraction; LA: Left atrium; LAP: Left atrial pressure; LV: Left ventricle; LVEDP: Left ventricular end diastolic pressure; NT-proBNP: N Terminal Brain Natriuretic peptide; TR: Tricuspid regurgitation (adapted from References 1 and 3).
- Citation: Iyngkaran P, Anavekar NS, Neil C, Thomas L, Hare DL. Shortness of breath in clinical practice: A case for left atrial function and exercise stress testing for a comprehensive diastolic heart failure workup. World J Methodol 2017; 7(4): 117-128
- URL: https://www.wjgnet.com/2222-0682/full/v7/i4/117.htm
- DOI: https://dx.doi.org/10.5662/wjm.v7.i4.117