Copyright
©The Author(s) 2024.
World J Methodol. Dec 20, 2024; 14(4): 93461
Published online Dec 20, 2024. doi: 10.5662/wjm.v14.i4.93461
Published online Dec 20, 2024. doi: 10.5662/wjm.v14.i4.93461
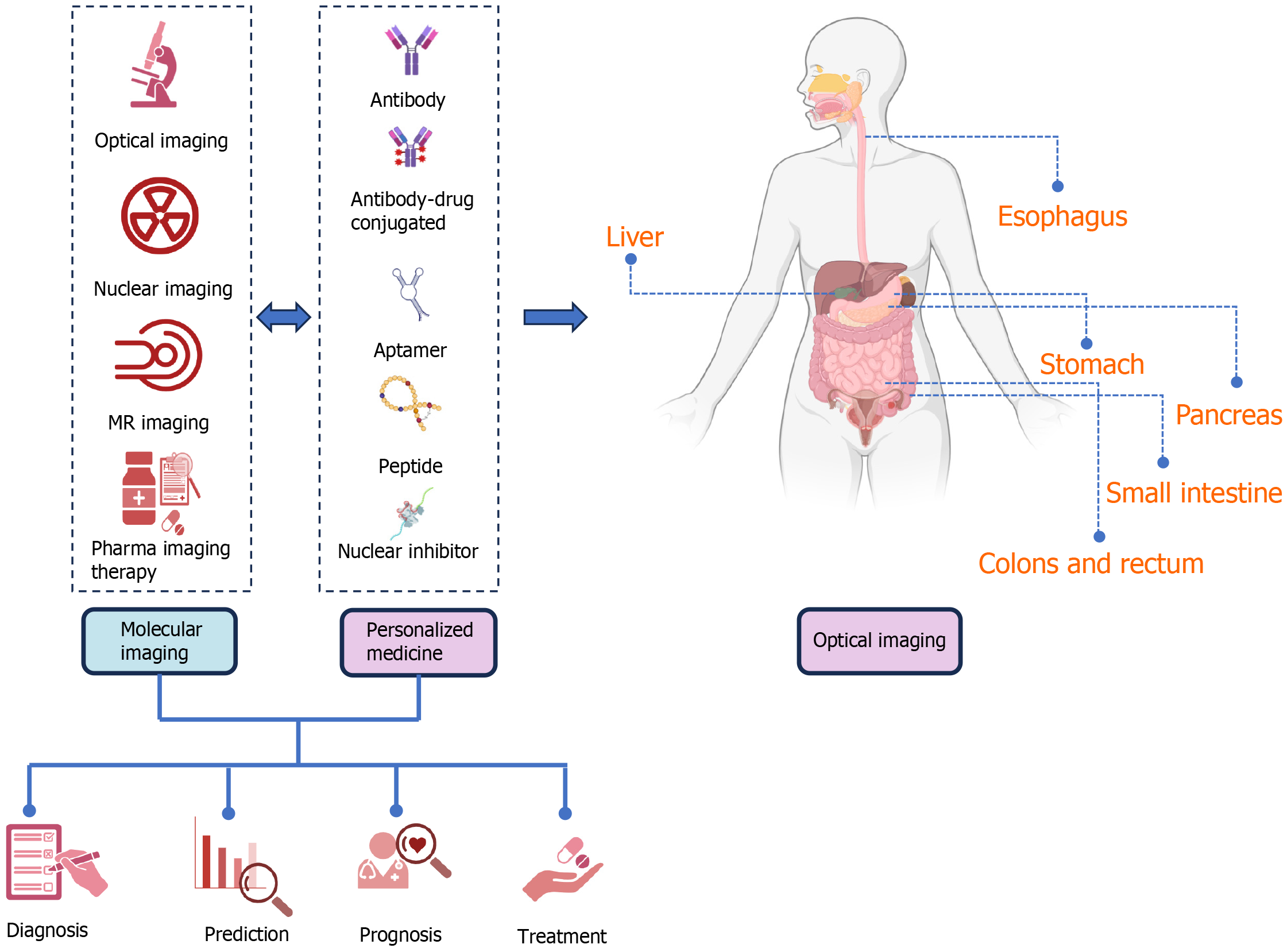
Figure 1 The function of molecular imaging along with personalized medicine in the diagnosis, screening, prognosis, treatment and also follow-up of gastrointestinal cancers, including the organs of the esophagus, stomach, intestines, colons, rectum, pancreas, and liver, is schematically shown.
With the use of molecular imaging and personalized medicine in recent years, the possibility of presenting the function and role of these two concepts in the form of priority and delay is generally not proposed and can be used in parallel or earlier and later according to each organ, and finally to benefit the patients. Molecular imaging including optical imaging (submodalities, including fluorescence, bioluminescence imaging, near infrared, surface-enhanced raman scattering and chemiluminescence), nuclear imaging [positron emission tomography (PET), PET/computerized tomography (CT), and single-photon emission CT], magnetic resonance imaging, imaging and pharma imaging Therapy can be used in the stage of screening, diagnosis, prognosis, treatment, and follow-up separately or in combination with personalized medicine (PM). PM can help patients and clinicians by intervening and taking into account the differences and considerations at the molecular level of various organs of digestive cancer, including aptamer, peptide, nuclear inhibitor, and antibodies. When necessary, PM aims to treat the appropriate patient. PM may be effective in molecular imaging since it helps in the identification of therapeutic targets and persons in need of therapy. It may assess drug transport, administration, and clearance in malignant or healthy cells to reduce side effects and prescribe medication dosage. By evaluating tumor drug activity, molecular imaging can analyze medication pharmacodynamics and uncover promising therapeutic responses and early malfunction. GI: Gastrointestinal.
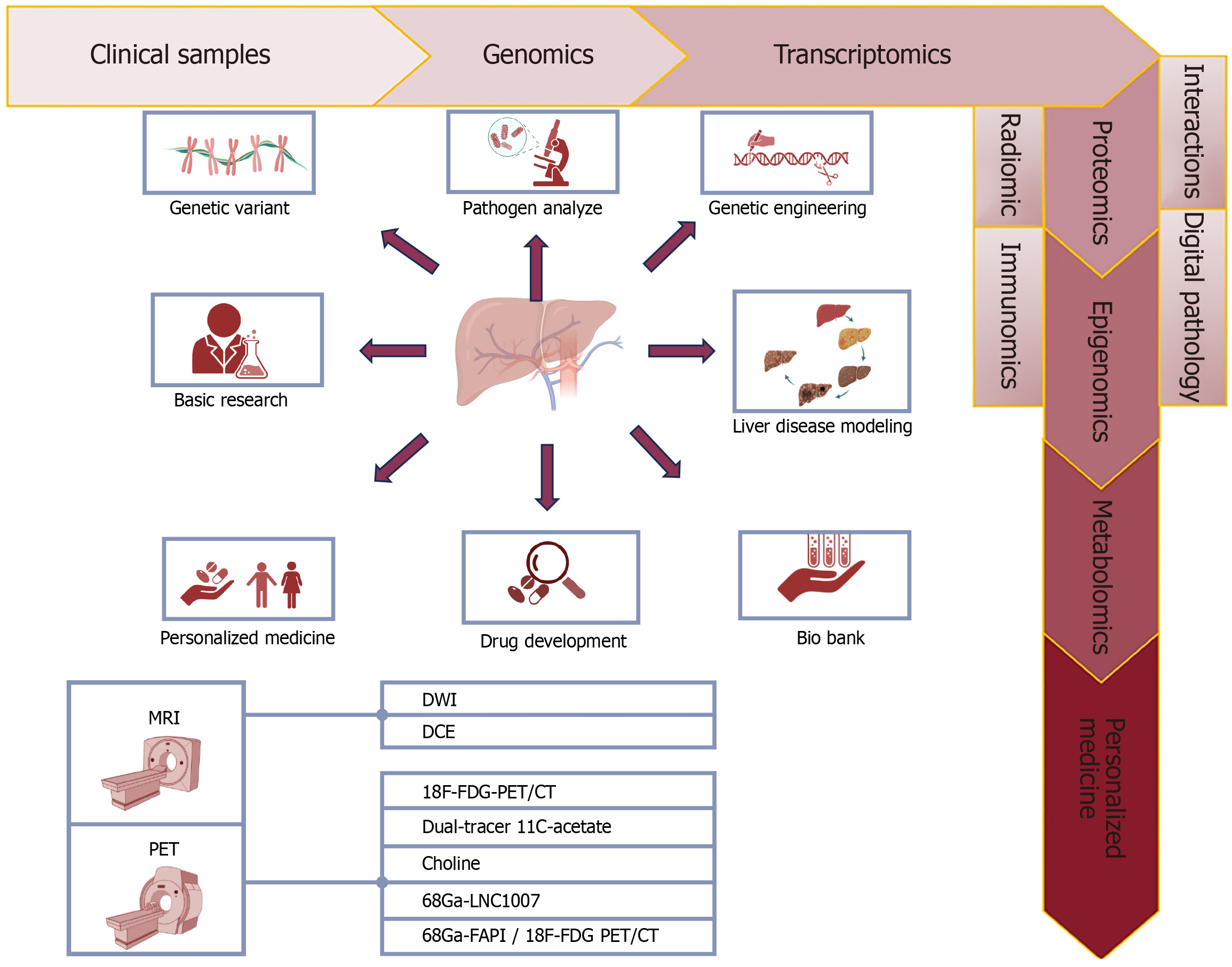
Figure 2 Role of personalized medicine and molecular imaging in liver cancers.
The main diagnostic and treatment modalities for liver cancer include positron emission tomography (PET) and magnetic resonance imaging, which are specific types of PET modalities including types bound with 18F-F-fluorodeoxyglucose, 11C-acetate, Choline, and types combined with Ga such as fibroblast activation protein inhibitor. The diagram with arrows shows the general progress and considerations made based on genetic, molecular, immunohistochemistry, microscopy, examination of pathogens at the cellular and molecular level, and background information of patients suffering from various types of liver cancer, which ultimately lead to adopting the best and most accurate and most appropriate and personalized solution available. In fact, in the pre-screening stage, collecting patient information, examining samples, and taking images to diagnose and adopt the most appropriate laboratory and imaging methods, as well as the most appropriate and personalized treatment method including medical treatment (drugs, dose, and type of drug), radiation therapy, non-intervention includes all types of surgeries on liver cancer patients according to different types of liver cancer including hepatocellular carcinoma, cholangiocarcinoma, and angiosarcoma. MRI: Magnetic resonance imaging; PET: Positron emission tomography; CT: Computed tomography; FDG: F-fluorodeoxyglucose; DCE: Dynamic contrast-enhanced imaging; DWI: Diffusion-weighted.
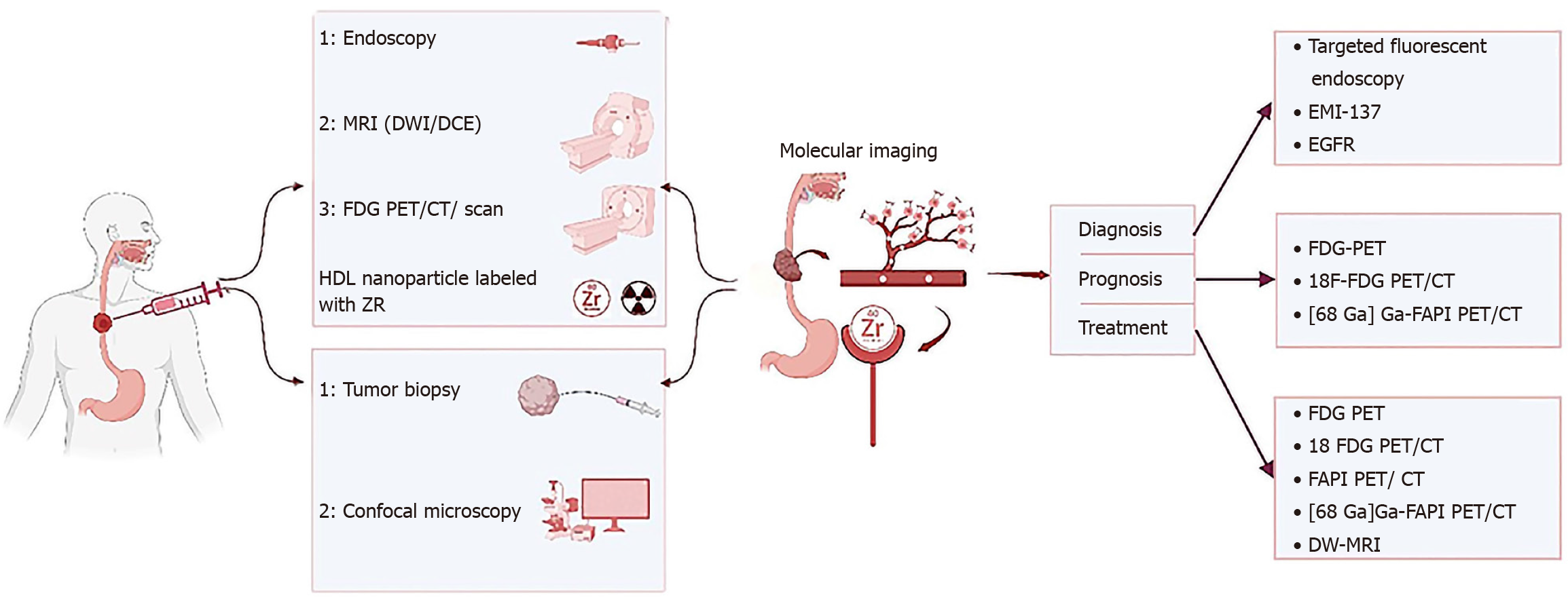
Figure 3 Role of personalized medicine and molecular imaging in esophagus cancers.
The function of molecular imaging and personalized medicine in esophageal cancers such as squamous cell carcinoma or adenocarcinoma including simultaneous or even initial and final examinations in the way of collecting temporal and personal information (specific to each person) in the diagnosis process including the collection of human samples, biopsy and blood samples and so on, all kinds of imaging modalities like endoscopy, magnetic resonance imaging (MRI) [diffusion-weighted (DWI)/dynamic contrast-enhanced imaging], [positron emission tomography (PET), PET computed tomograph (CT) and bound with F-fluorodeoxyglucose (FDG)] and also in the path of determining disease prognosis with PET types including FDG-PET, [68 Ga] Ga-FAPI PET/CT, and 18F-FDG PET/CT. Treatment with dedicated modalities FDG-PET, [68 Ga] Ga-FAPI PET/CT, 18F-FDG PET/CT, and DWI-MRI and it is tried in each stage of the currency, from the beginning of data collection to diagnosis, determining prognosis, treatment, response to treatment, assessment of relapse and follow-up, is the most appropriate and accurate and personalized solution possible based on personalized medicine in determining the dose of the substances used in the modalities imaging, choosing the most suitable imaging modality and binding element, the amount of medical treatment (drugs, amount and type of drug), and even all kinds of combined solutions with surgery and radiation therapy should be used. MRI: Magnetic resonance imaging; DW: Diffusion-weighted; PET: Positron emission tomography; CT: Computed tomography; FDG: F-fluorodeoxyglucose; EGFR: Epidermal growth factor receptor.
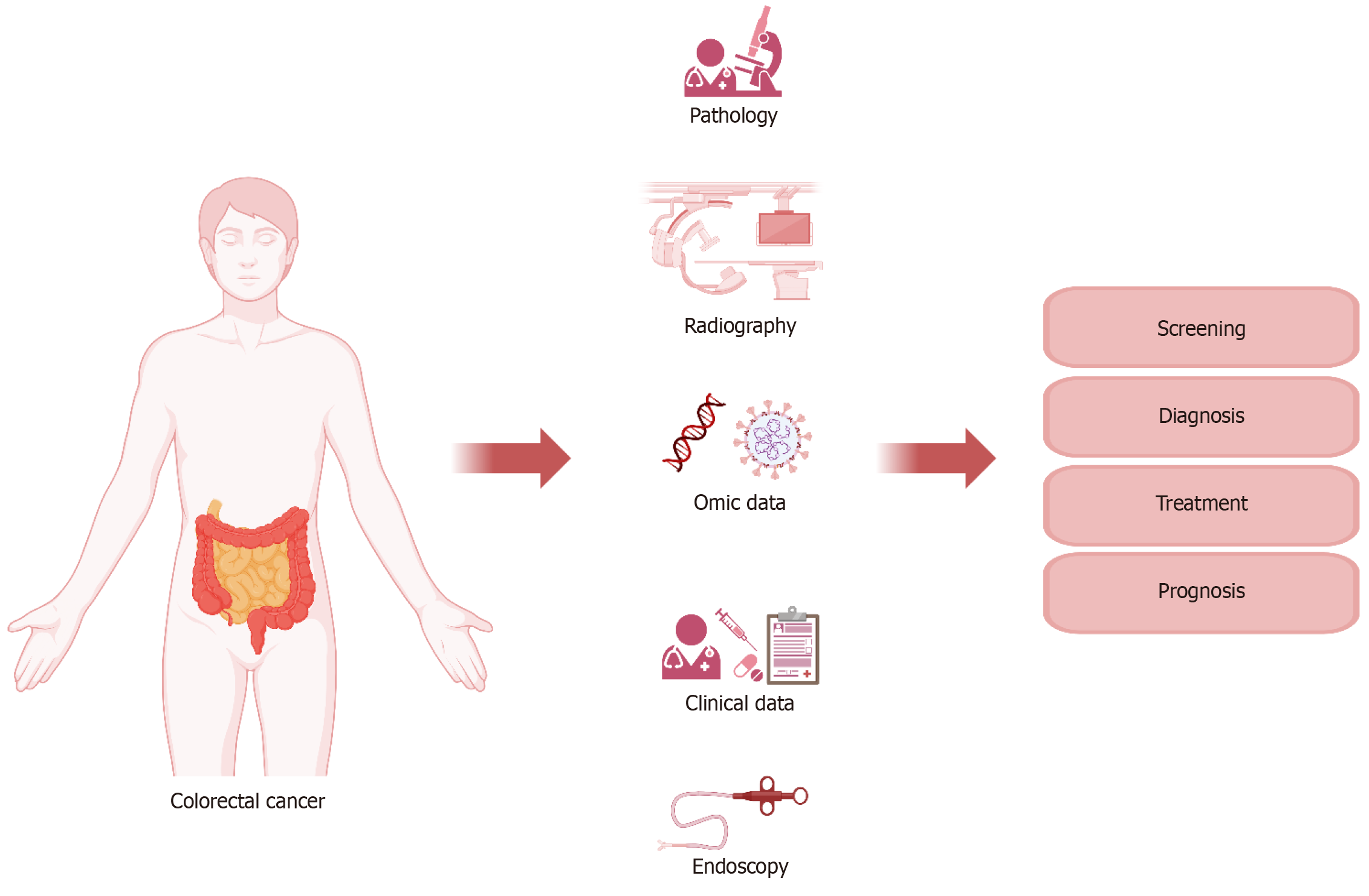
Figure 4 Role of personalized medicine and molecular imaging in colorectal cancers.
The function and role of molecular imaging and personalized medicine in charge of management of colorectal cancers is shown schematically in the picture, and the possibility of playing the role of these two concepts does not have any special priority or delay and can be simultaneous and parallel. The role of these two concepts is to adopt the most accurate, appropriate, and personalized mode for patients with colorectal cancers, including the basic steps of collecting individual demographic information of patients, collecting human samples, including blood, urine, and biopsy samples etc, and examination and analysis, screening, in the diagnostic path using common and novel imaging and anatomical laboratory methods and even at the cellular and molecular level, determining the most suitable and targeted treatment method including various medical methods (drugs, type and amount), and types of surgical methods, radiation therapy or combined methods, determining the rate of response to treatment, recurrence, prognosis and follow-up of patients according to the characteristics of each patient. Imaging modalities including positron emission tomography (PET), 18F-fluorodeoxyglucose (FDG) PET, FDG-PETPET, 68[Ga]Ga-DOTA-fibroblast activation protein inhibitor (FAPI)-04 PET/computed tomography (CT), 68Ga-FAPI PET/CT, magnetic resonance imaging (MRI), including dynamic contrast-enhanced imaging (DCE) MRI and CT perfusion imaging in determining the course diagnosis, prognosis and FDG-PET/CT, 18F-FDG PET/CT, 68Ga-FAPI PET/CT, and DCE-MRI in treatment.
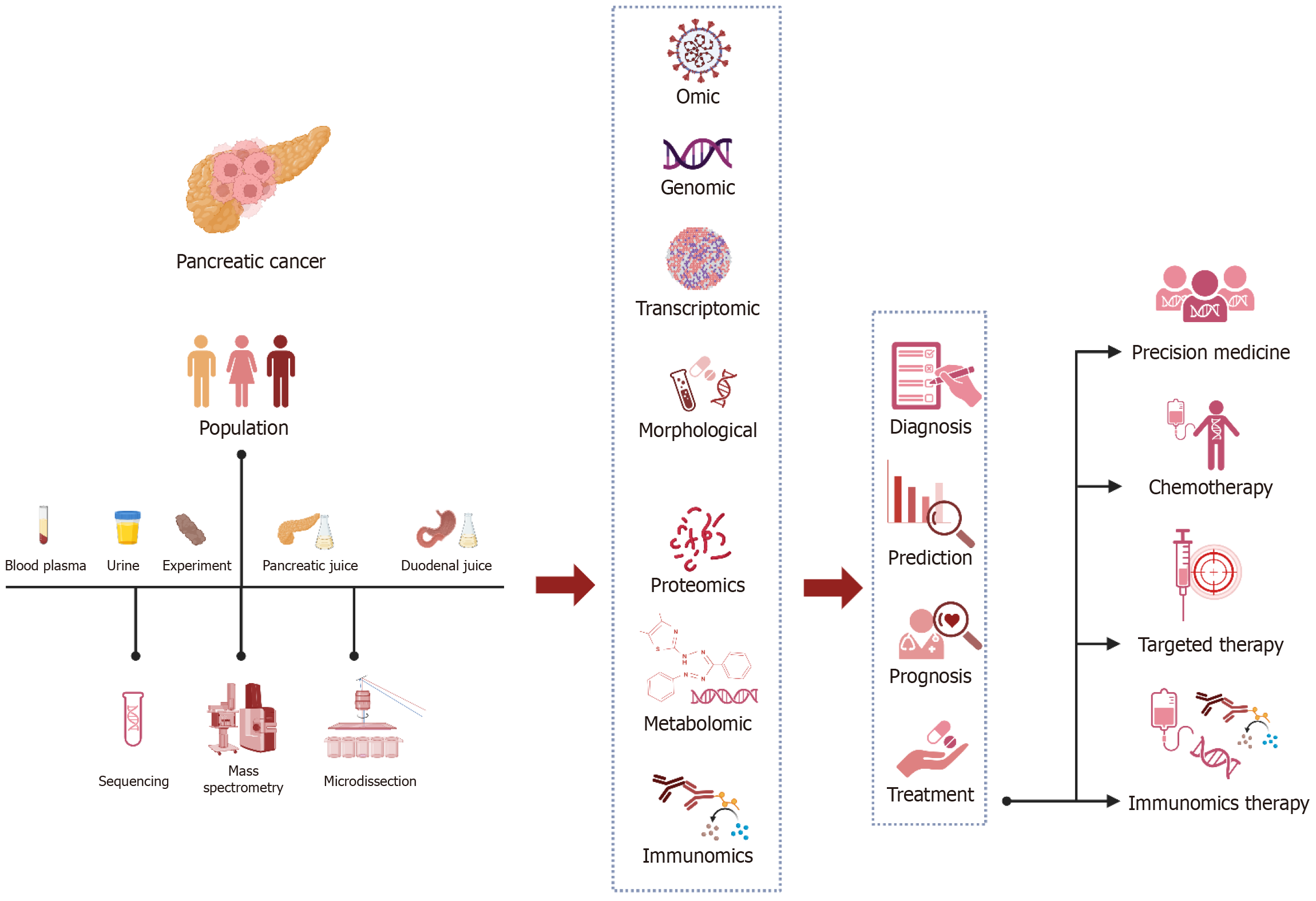
Figure 5 Role of personalized medicine and molecular imaging in pancreatic cancers.
The function and role of molecular imaging and personal medicine in the management of pancreas is shown in a semantic way, and the possibility of playing the role of these two concepts does not have any special priority or delay, and it can be both concurrent and concurrent, and it is changing day by day. The role of these two concepts is to adopt the most accurate, appropriate and personalized mode possible for pancreatic cancer patients from the initial stages of collecting individual demographic information of patients, collecting human samples including blood, urine and biopsy samples, etc. and checking and their analysis, in the path of individualization using the common methods of novel imaging and anatomical laboratory and even at the cellular and molecular level to determine the most appropriate and targeted treatment including various medical methods (drugs, type and amount) and various surgical methods, radiation Treatment or combined methods is to determine the rate of response to treatment, recurrence, prognosis and follow-up of patients according to the conditions and characteristics of each patient. Imaging modality in determining the course of diagnosis and determining prognosis includes endoscopy, computed tomography (CT), positron emission tomography (PET) and their combination with chemical agents such as 68Ga- fibroblast activation protein inhibitor (FAPI) PET/CT, 18F-fluorodeoxyglucose (FDG) PET/CT and even FAPI PET/CT alone, and Gd-enhanced magnetic resonance imaging (MRI) with diffusion-weighted along contrast-enhanced CT and adopting a treatment plan based on CT, PET, PET/CT, 18F-FDG PET/CT, FDG-PET/contrast-enhanced CT, FDG-PET/non-contrast-enhanced CT, FAPI PET/CT, single-photon emission CT/CT and dynamic contrast-enhanced-MRI are utilized to select chemotherapy, endohistochemical therapy or medical treatment based on personalized medicine.
- Citation: Fathi M, Taher HJ, Al-Rubiae SJ, Yaghoobpoor S, Bahrami A, Eshraghi R, Sadri H, Asadi Anar M, Gholamrezanezhad A. Role of molecular imaging in prognosis, diagnosis, and treatment of gastrointestinal cancers: An update on new therapeutic methods. World J Methodol 2024; 14(4): 93461
- URL: https://www.wjgnet.com/2222-0682/full/v14/i4/93461.htm
- DOI: https://dx.doi.org/10.5662/wjm.v14.i4.93461