Published online Apr 12, 2015. doi: 10.5528/wjtm.v4.i1.38
Peer-review started: July 23, 2014
First decision: December 17, 2014
Revised: January 23, 2015
Accepted: March 4, 2015
Article in press: March 5, 2015
Published online: April 12, 2015
Processing time: 265 Days and 12.9 Hours
AIM: To investigate if music reduces anxiety and pain in the Veterans Affairs population undergoing flexible cystoscopy.
METHODS: This study was reviewed and approved by the University of California, San Diego Human Research Protections Program Institutional Review Board. Patients were prospectively randomized to undergo flexible cystoscopy with or without music. Thirty-eight patients were randomized into either the No Music group (n = 24) or the Music group (n = 14). We used the state-trait anxiety inventory and the visual analog pain scale, respectively. Statistics were generated and compared using an independent t-test and chi-squared tests. P values < 0.05 were considered statistically significant. Outpatient cystoscopy is a safe and useful procedure employed frequently in Urology for diagnosis and evaluation of genitourinary pathologies. However, cystoscopy-related distress cannot be ignored. Three components of outpatient cystoscopy have been evaluated to improve the cystoscopic experience: local anesthetic control, cystoscopic equipment redesign and environmental modification. We reviewed the literature pertaining to these modifications.
RESULTS: The mean age was 65.3 and 67.1 years for men in the No Music and Music groups, respectively. Although, the majority of patients in each group self-identified as Caucasians (66%), African American, Hispanic and other ethnicities represented 13%, 8% and 13% respectively. The majority of patients (68%) reported experiencing hematuria. Thirty-four percent had a history of bladder cancer, and eighteen percent had a history of prostate cancer. Ten patients (26%) admitted to taking antidepressants. Physiologic parameters that correlated to pain and anxiety (systolic blood pressure, diastolic blood pressure, and heart rate) were statistically similar in both groups prior to and after flexible cystoscopy. The median delta anxiety between the No Music and Music groups were not significantly different (0.78 vs -1.46), and the pain scores between the No Music and Music groups (1.5 vs 1.6) were not statistically different (P = 0.28 and P = 0.92, respectively).
CONCLUSION: Preliminary results demonstrate that music does not reduce anxiety or pain associated with flexible cystoscopy.
Core tip: Flexible cystoscopy is a very common in-office procedure performed in urology. There have been several technological advances made in the instrumentation of flexible cystoscopies, however, there have also been advances made in reducing patient pain and anxiety associated with this procedure such as viscous lidocaine jelly and music. We reviewed the literature on effects of modifiable factors on patient pain and anxiety associated with flexible cystoscopy, and also includes preliminary data on a Veterans Affairs randomized prospective trial evaluating the effect of classical music on pain and anxiety associated with flexible cystoscopy.
- Citation: Mirheydar HS, Raheem OA, Elkhoury FF, Jabaji R, Palazzi KL, Patel N, Du R, Maroney S, Sakamoto K. Modern advances in reducing anxiety and pain associated with cystoscopy: Systematic review. World J Transl Med 2015; 4(1): 38-43
- URL: https://www.wjgnet.com/2220-6132/full/v4/i1/38.htm
- DOI: https://dx.doi.org/10.5528/wjtm.v4.i1.38
Cystoscopy is a common urologic examination indicated for a wide variety of genitourinary conditions[1-4]. Cystoscopy was first conceptualized over two centuries ago[5] and underwent multiple advancements in technology to allow patients to undergo the procedure with relative comfort. Regardless of the reason for the inspection, however, cystoscopy is invasive and can be a distressing experience for patients.
Since patient distress negatively impacts adherence to cystoscopy guidelines, many studies have investigated techniques to reduce cystoscopy-associated anxiety and pain[1]. Three general methods to alleviate pain and anxiety are local anesthetic control, cystoscopic equipment redesign, and environmental modification. Lidocaine lubricants, inhaled nitrous oxide, and anxiolytic medication have been proposed to ameliorate flexible cystoscopy-associated distress, though none sufficiently relieves patient fear, pain, and anxiety[6-14]. The cystoscopic instrument has evolved from the rigid cystoscope to the flexible cystoscope, changing from analog visualization to digital and more recently digital high definition visualization.
For environmental modification, music is gaining increasing recognition as an effective tool to alleviate perceived pain and has been shown to be beneficial in a variety of clinical settings[15-23]. Herein, we report the result of a prospective randomized trial of the effect of music on pain and anxiety in the Veterans Affairs patient population during flexible cystoscopy. Furthermore, we reviewed the above-mentioned three factors (local pain control, equipment redesign and environmental modification) incorporated to lessen the anxiety and pain levels during cystoscopy.
This study was reviewed and approved by the University of California, San Diego Human Research Protections Program Institutional Review Board (IRB). Patient privacy and confidentiality are protected according to HIPAA guidelines. Following IRB approval, male patients at the Veterans Affairs San Diego Medical Center were prospectively randomized to undergo flexible cystoscopy with or without music. Thirty-eight patients were randomly assigned into one of two groups using an adaptive biased-coin randomization method: (1) the No Music group (patients did not hear music during preparation and draping of patient and anesthetization of urethra); or (2) the Music group (patients listened to the same excerpt of classical music). Inclusion criteria were age > 18 years old. There were no women in this study, although that was not an exclusion criterion. Exclusion criteria were current urinary tract infection, anatomic urethral abnormalities, and inability to complete the surveys. Patients’ past medical history, including history of bladder cancer, prostate cancer, hematuria, and current or past use of anti-depressants and anti-anxiety medication, was recorded. All patients with a prior history of bladder cancer were confirmed to have had prior cystoscopy and were currently undergoing cystoscopy for surveillance, while those without bladder cancer were undergoing cystoscopy for diagnostic purposes (e.g., microhematuria). Each patient was consented for the study on the day of the procedure.
Pre-operative and post-operative systolic and diastolic blood pressure, heart rate, and respiratory rate were measured for each patient. The pre-procedure vital signs, including blood pressure, heart rate, and respiratory rate, were all obtained prior to the cystoscopy and prior to playing music. Post-procedure vital signs were obtained after the cystoscopy was completed. During the 10-min dwell time of the 2% intraurethral lidocaine jelly, the patient either listened to classical music for 10 min or did not hear any music at all. A 15 French Olympus® digital flexible cystoscope was connected to a digital video monitor that was used for all procedures. The music was played prior to the cystoscopy.
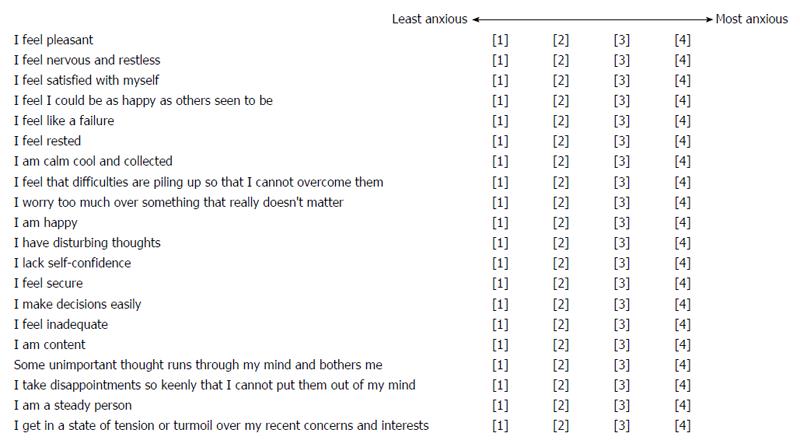
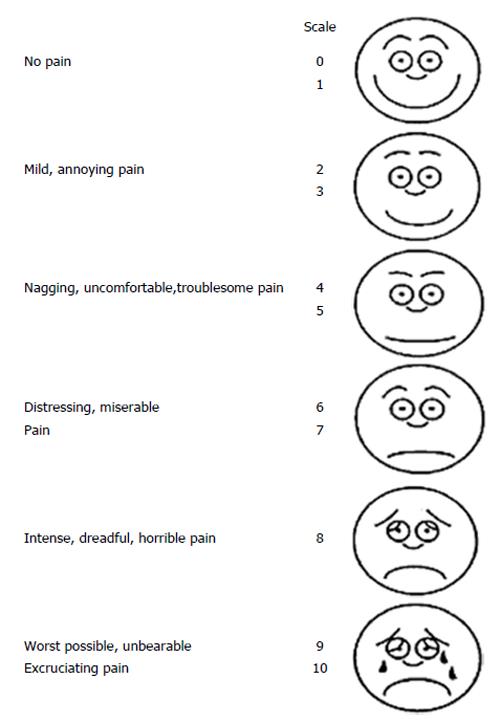
To measure anxiety level and pain level, we used the State-Trait Anxiety Inventory (STAI) and the Visual Analog Pain Scale, respectively (Figures 1 and 2)[24,25]. Both are validated surveys. The State-Trait Anxiety Inventory (range 20-80) measures the transitional emotional status evoked by a stressful situation, such as a medical procedure or surgery. The Visual Analog Pain Scale (range 0-10) quantifies pain level using verbal and visual descriptors. Higher scores indicate higher anxiety and pain for both tests. The patients were asked to complete two anxiety surveys, one pre-procedure and one post-procedure. Patients were also asked to complete a visual analog pain scale survey post-procedure.
Statistics were generated and compared using an independent t-test and chi-squared tests. P values < 0.05 were considered statistically significant. Delta anxiety score is defined as pre-cystoscopy anxiety score - post-cystoscopy anxiety score.
Thirty-eight patients were randomized into either the No Music group (n = 24) or the Music group (n = 14). The subjects were all male as noted above. Table 1 outlines the demographics and clinical characteristics of these subjects. The mean age was 65.3 and 67.1 years for men in the No Music and Music groups, respectively. The majority of patients in each group self-identified as Caucasians. A majority of patients (68%) reported experiencing hematuria. Thirty-four percent had a history of bladder cancer, and 26% admitted to taking antidepressants. Physiologic parameters that correlated to pain and anxiety (systolic blood pressure, diastolic blood pressure, and heart rate) were statistically similar in both groups pre- and post-flexible cystoscopy. Patients’ peri-procedural vital signs between the Music and No Music groups are summarized in Table 2. The median delta anxiety between the No Music and Music groups were not significantly different (0.78 vs -1.46), and the pain scores between the No Music and Music groups (1.5 vs 1.6) were not statistically different (P = 0.28 and P = 0.92, respectively).
| Variables | Groups | P value | |
| Music group | No music group | ||
| (n = 14) | (n = 24) | ||
| Age, mean + SD | 67.1 + 9.9 | 65.3 + 10.4 | 0.9541 |
| Race | 0.698 | ||
| Caucasian | 10 (71) | 15 (63) | |
| African American | 1 (7) | 4 (17) | |
| Hispanics | 1 (7) | 2 (8) | |
| Others | 2 (15) | 3 (12) | |
| History of bladder carcinoma | 10 (71) | 3 (1) | 0.1488 |
| History of prostate carcinoma | 2 (14) | 5 (21) | 0.3039 |
| History of hematuria | 12 (87) | 14 (58) | 0.2049 |
| Antidepressant or antianxiety medications | 4 (29) | 6 (25) | 0.7092 |
| Variables | Groups | P value | |
| Music group | No music group | ||
| (n = 14) | (n = 24) | ||
| Pre Cystoscopy | |||
| Systolic blood pressure (mmHg), mean + SD | 135.5 + 17.7 | 135.5 + 17.9 | 0.9834 |
| Diastolic blood pressure (mmHg), mean + SD | 79.4 + 12.9 | 80.0 + 11.5 | 0.7908 |
| Hear rate (beat/min), mean + SD | 73.5 + 13.3 | 75.3 + 14.3 | 0.4405 |
| Post Cystoscopy | |||
| Systolic blood pressure (mmHg), mean + SD | 139.1 + 22.8 | 137.2 + 17.3 | 0.5837 |
| Diastolic blood pressure (mmHg, mean + SD | 81.8 + 13.0 | 83.0 + 11.6 | 0.5717 |
| Hear rate (beat/min), mean + SD | 71.3 + 15.6 | 74.9 + 14.2 | 0.16 |
Outpatient cystoscopy is a safe and useful procedure employed frequently in Urology for diagnosis and evaluation of genitourinary pathologies. However, cystoscopy-related distress cannot be ignored[1]. Three components of outpatient cystoscopy have been evaluated to improve the cystoscopic experience: local anesthetic control, cystoscopic equipment redesign and environmental modification. We reviewed the literature pertaining to these modifications. In addition, since flexible cystoscopy is a more tolerable procedure more commonly utilized in the United States, we performed this study to investigate if music reduces anxiety and pain in American veterans undergoing flexible cystoscopy.
A recent study suggests that listening to classical music during rigid cystoscopy enhances patient comfort and decreases post-procedure pain and anxiety[23]. In addition to this report, prior studies have demonstrated music’s ameliorating effect on pain and anxiety in patients undergoing a variety of procedures, including rigid cystoscopy[16-18,20].
Contrary to these studies, our study did not show reduction of cystoscopy-related anxiety by listening to classical music during flexible cystoscopy, regardless of its indication. The lack of the effect of music in our group may be due to the small number of subjects. In addition, due to the patient demographics of the Veterans Affairs hospitals, the majority of our patients have been Caucasian males. Subsets of patients treated at the Veterans Affairs Hospitals respond to painful stimuli differently than their civilian counterparts, possibly due to the increased prevalence of PTSD and generalized anxiety disorder[24,25]. A subset of patients with history of bladder carcinoma that required repeated surveillance using office-based flexible cystoscopies were also included in this cohort. We observed that listening to music at time of respective cystoscopy did not influence their peri-procedural STAI anxiety scores when adjusting for other variables. We included blood pressure, heart rate, and respiratory rate as objective representations of the emotional state of the patient in addition to validated questionnaires. These parameters are directly influenced by sympathetic nervous system activation due to emotional distress or anxiety through the release of catecholamines, specifically norepinephrine and epinephrine[26,27]. Higher catecholamine levels from anxiety and fear result in elevated blood pressure, heart rate, and respiratory rate. Thus, the combination of these objective physiologic indicators with the subjective patient-provided information on anxiety and fear provided a more holistic assessment of the impact of music on how a patient experiences flexible cystoscopy.
Several randomized studies have shown the benefit of intraurethral lidocaine gel in reducing the pain associated with flexible cystoscopy and others have shown no improvement[6,8-13]. However, a recent meta-analysis[28] evaluating the effect of lidocaine gel on pain during flexible cystoscopy concluded that intraurethral instillation of lidocaine gel vs plain lubricating gel reduces the likelihood of moderate to severe pain during flexible cystoscopy. Although fiber optic technology is still utilized for many of the flexible cystoscopes in the country, digital technologies are available. In other endoscopic devices, visualization using digital technology has higher resolution, decreased distortion, improved color representation, and larger image size compared with the standard fiber optic visualization with a narrower field of view[29]. More recently, digital technology with distal sensor high definition images has been compared to standard digital visualization[30]. These reductions will likely result in improved patient comfort during outpatient flexible cystoscopy.
Modern advances in flexible cystoscopic instrumentation and peri-procedural instillation of intraurethral lidocaine have both decreased pain associated with flexible cystoscopy. Listening to music during rigid cystoscopy has been shown to reduce pain and discomfort. Our prospective, randomized study explored the effect of classical music on pain and anxiety associated with flexible cystoscopy, and preliminarily demonstrates that music does not reduce anxiety or pain associated with flexible cystoscopy in the Veterans Affairs population.
Flexible cystoscopy is a very common in-office procedure performed in Urology. Several technological advances have been made in flexible cystoscopy instrumentation, however, there have also been advances in reducing patient pain and anxiety associated with this procedure, such as viscous lidocaine jelly and music. The authors reviewed the literature on effects of modifiable factors on patient pain and anxiety associated with flexible cystoscopy, and also include preliminary data on a Veterans Affairs randomized prospective trial evaluating the effect of classical music on pain and anxiety associated with flexible cystoscopy. This study explored the effect of classical music on pain and anxiety associated with flexible cystoscopy, and preliminarily demonstrates that music does not reduce anxiety or pain associated with flexible cystoscopy in the Veterans Affairs population.
Flexible cystoscopy is a very common in-office procedure performed in Urology. Several technological advances have been made in flexible cystoscopy instrumentation, however, there have also been advances in reducing patient pain and anxiety associated with this procedure, such as the use of viscous lidocaine jelly and music.
In this systematic review, the authors attempted to evaluate whether listening to music at time of office-based flexible cystoscopy can alleviate pain and anxiety associated with this procedure. Previous studies have highlighted that listening to music during rigid cystoscopy reduces pain and discomfort. In contrast, they study did not show reduction of cystoscopy-related anxiety by listening to classical music during flexible cystoscopy, regardless of its indication. The lack of effect of music in their group may be due to the small number of subjects recruited in this study. Additionally, owing to the patient demographics of Veterans Affairs hospitals, the majority of our patients have been Caucasian males. Subsets of patients treated at Veterans Affairs hospitals respond to painful stimuli differently than their civilian counterparts, possibly due to the increased prevalence of PTSD and generalized anxiety disorder.
Although listening to music at time of office-based flexible cystoscopy may play a limited role in reducing pain and anxiety in the Veteran population, these findings cannot be generalized to the general patient population, particularly civilian, as responses to pain and/or anxiety associated with flexible cystoscopy can manifest differently among heterogeneous patient populations.
Well described medical and technological terminology commonly known to the general audience and the wider medical community was used. State-trait anxiety inventory; visual analog pain scale.
This study investigated cystoscopy-related distress, reviewing benefits of intraurethral lidocaine use as well as of digital cystoscopes for reducing procedural anxiety and pain. Indeed, the authors performed a study to investigate if listening to classical music reduces anxiety and pain in patients undergoing flexible cystoscopy who were treated at a Veterans Affairs hospital in the United States.
P- Reviewer: Nishio K, Orlacchio A S- Editor: Tian YL L- Editor: A E- Editor: Liu SQ
| 1. | Schrag D, Hsieh LJ, Rabbani F, Bach PB, Herr H, Begg CB. Adherence to surveillance among patients with superficial bladder cancer. J Natl Cancer Inst. 2003;95:588-597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 108] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 2. | Clark PE, Agarwal N, Biagioli MC, Eisenberger MA, Greenberg RE, Herr HW, Inman BA, Kuban DA, Kuzel TM, Lele SM. Bladder cancer. J Natl Compr Canc Netw. 2013;11:446-475. [PubMed] |
| 3. | Davis R, Jones JS, Barocas DA, Castle EP, Lang EK, Leveillee RJ, Messing EM, Miller SD, Peterson AC, Turk TM. Diagnosis, evaluation and follow-up of asymptomatic microhematuria (AMH) in adults: AUA guideline. J Urol. 2012;188:2473-2481. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 270] [Cited by in RCA: 271] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 4. | Hall MC, Chang SS, Dalbagni G, Pruthi RS, Seigne JD, Skinner EC, Wolf JS, Schellhammer PF. Guideline for the management of nonmuscle invasive bladder cancer (stages Ta, T1, and Tis): 2007 update. J Urol. 2007;178:2314-2330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 568] [Cited by in RCA: 577] [Article Influence: 33.9] [Reference Citation Analysis (0)] |
| 5. | Samplaski MK, Jones JS. Two centuries of cystoscopy: the development of imaging, instrumentation and synergistic technologies. BJU Int. 2009;103:154-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 6. | Birch BR, Ratan P, Morley R, Cumming J, Smart CJ, Jenkins JD. Flexible cystoscopy in men: is topical anaesthesia with lignocaine gel worthwhile? Br J Urol. 1994;73:155-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 49] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 7. | Calleary JG, Masood J, Van-Mallaerts R, Barua JM. Nitrous oxide inhalation to improve patient acceptance and reduce procedure related pain of flexible cystoscopy for men younger than 55 years. J Urol. 2007;178:184-18; discussion 188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 30] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 8. | Chen YT, Hsiao PJ, Wong WY, Wang CC, Yang SS, Hsieh CH. Randomized double-blind comparison of lidocaine gel and plain lubricating gel in relieving pain during flexible cystoscopy. J Endourol. 2005;19:163-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 46] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 9. | Herr HW, Schneider M. Outpatient flexible cystoscopy in men: a randomized study of patient tolerance. J Urol. 2001;165:1971-1972. [PubMed] |
| 10. | Holmes M, Stewart J, Rice M. Flexible cystoscopy: is the volume and content of the urethral gel critical? J Endourol. 2001;15:855-858. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | McFarlane N, Denstedt J, Ganapathy S, Razvi H. Randomized trial of 10 mL and 20 mL of 2% intraurethral lidocaine gel and placebo in men undergoing flexible cystoscopy. J Endourol. 2001;15:541-544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 53] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 12. | Palit V, Ashurst HN, Biyani CS, Elmasray Y, Puri R, Shah T. Is using lignocaine gel prior to flexible cystoscopy justified? A randomized prospective study. Urol Int. 2003;71:389-392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 13. | Rodríguez-Rubio F, Sanz G, Garrido S, Sánchez C, Estudillo F. Patient tolerance during outpatient flexible cystoscopy--a prospective, randomized, double-blind study comparing plain lubrication and lidocaine gel. Scand J Urol Nephrol. 2004;38:477-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 20] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Song YS, Song ES, Kim KJ, Park YH, Ku JH. Midazolam anesthesia during rigid and flexible cystoscopy. Urol Res. 2007;35:139-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 15. | Argstatter H, Haberbosch W, Bolay HV. Study of the effectiveness of musical stimulation during intracardiac catheterization. Clin Res Cardiol. 2006;95:514-522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 42] [Article Influence: 2.2] [Reference Citation Analysis (1)] |
| 16. | Chan YM, Lee PW, Ng TY, Ngan HY, Wong LC. The use of music to reduce anxiety for patients undergoing colposcopy: a randomized trial. Gynecol Oncol. 2003;91:213-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 94] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 17. | Ferguson SL, Voll KV. Burn pain and anxiety: the use of music relaxation during rehabilitation. J Burn Care Rehabil. 2004;25:8-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 44] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 18. | Krout RE. The effects of single-session music therapy interventions on the observed and self-reported levels of pain control, physical comfort, and relaxation of hospice patients. Am J Hosp Palliat Care. 2001;18:383-390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 78] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 19. | Lee DW, Chan KW, Poon CM, Ko CW, Chan KH, Sin KS, Sze TS, Chan AC. Relaxation music decreases the dose of patient-controlled sedation during colonoscopy: a prospective randomized controlled trial. Gastrointest Endosc. 2002;55:33-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 84] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 20. | Menegazzi JJ, Paris PM, Kersteen CH, Flynn B, Trautman DE. A randomized, controlled trial of the use of music during laceration repair. Ann Emerg Med. 1991;20:348-350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 21. | Ovayolu N, Ucan O, Pehlivan S, Pehlivan Y, Buyukhatipoglu H, Savas MC, Gulsen MT. Listening to Turkish classical music decreases patients’ anxiety, pain, dissatisfaction and the dose of sedative and analgesic drugs during colonoscopy: a prospective randomized controlled trial. World J Gastroenterol. 2006;12:7532-7536. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 68] [Cited by in RCA: 68] [Article Influence: 3.6] [Reference Citation Analysis (1)] |
| 22. | Tsivian M, Qi P, Kimura M, Chen VH, Chen SH, Gan TJ, Polascik TJ. The effect of noise-cancelling headphones or music on pain perception and anxiety in men undergoing transrectal prostate biopsy. Urology. 2012;79:32-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 53] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 23. | Yeo JK, Cho DY, Oh MM, Park SS, Park MG. Listening to music during cystoscopy decreases anxiety, pain, and dissatisfaction in patients: a pilot randomized controlled trial. J Endourol. 2013;27:459-462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 69] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 24. | Defrin R, Ginzburg K, Solomon Z, Polad E, Bloch M, Govezensky M, Schreiber S. Quantitative testing of pain perception in subjects with PTSD--implications for the mechanism of the coexistence between PTSD and chronic pain. Pain. 2008;138:450-459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 129] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 25. | Milanak ME, Gros DF, Magruder KM, Brawman-Mintzer O, Frueh BC. Prevalence and features of generalized anxiety disorder in Department of Veteran Affairs primary care settings. Psychiatry Res. 2013;209:173-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 41] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 26. | Khasar SG, McCarter G, Levine JD. Epinephrine produces a beta-adrenergic receptor-mediated mechanical hyperalgesia and in vitro sensitization of rat nociceptors. J Neurophysiol. 1999;81:1104-1112. [PubMed] |
| 27. | Sloviter RS, Dean E, Neubort S. Electron microscopic analysis of adrenalectomy-induced hippocampal granule cell degeneration in the rat: apoptosis in the adult central nervous system. J Comp Neurol. 1993;330:337-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 173] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 28. | Aaronson DS, Walsh TJ, Smith JF, Davies BJ, Hsieh MH, Konety BR. Meta-analysis: does lidocaine gel before flexible cystoscopy provide pain relief? BJU Int. 2009;104:506-509; discussion 509-510. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 72] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 29. | Zilberman DE, Lipkin ME, Ferrandino MN, Simmons WN, Mancini JG, Raymundo ME, Zhong P, Preminger GM. The digital flexible ureteroscope: in vitro assessment of optical characteristics. J Endourol. 2011;25:519-522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 30. | Lusch A, Liss MA, Greene P, Abdelshehid C, Menhadji A, Bucur P, Alipanah R, McDougall E, Landman J. Comparison of optics and performance of a distal sensor high definition cystoscope, a distal sensor standard definition cystoscope, and a fiberoptic cystoscope. Urology. 2013;82:1226-1230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |