Peer-review started: July 23, 2020
First decision: October 21, 2020
Revised: October 26, 2020
Accepted: November 4, 2020
Article in press: November 4, 2020
Published online: November 29, 2020
Processing time: 125 Days and 7.8 Hours
Coronavirus disease 2019 has spread across the world and has been classified as a pandemic. It has overwhelmed the healthcare systems. Specifically, it has overstretched the intensive care units and renal replacement therapy services in many countries. In this paper, we discuss the reconfiguration of nephrology services in the State of Qatar during the current pandemic. We highlight the key strategies that have been implemented to ensure that renal replacement therapy capacity is not constrained in either the intensive care or ambulatory setting. Some innovative approaches for the safe delivery of ambulatory care to dialysis and kidney transplant patients are also discussed.
Core Tip: Although the impact of the pandemic and the healthcare models differ across countries, pandemic preparedness planning is vital to improve the effectiveness of a country’s response to the pandemic. Renal replacement therapy is a lifesaving treatment, and it is imperative that healthcare systems invest in technical infrastructure, staff, and supplies to provide efficient critical care nephrology services in the setting of a pandemic.
- Citation: Asim M, Alkadi M, Hamad A, Othman M, Abuhelaiqa E, Fituri O, El-Madhoun I, Al-Malki H. Restructuring nephrology services to combat COVID-19 pandemic: Report from a Middle Eastern country. World J Nephrol 2020; 9(2): 9-17
- URL: https://www.wjgnet.com/2220-6124/full/v9/i2/9.htm
- DOI: https://dx.doi.org/10.5527/wjn.v9.i2.9
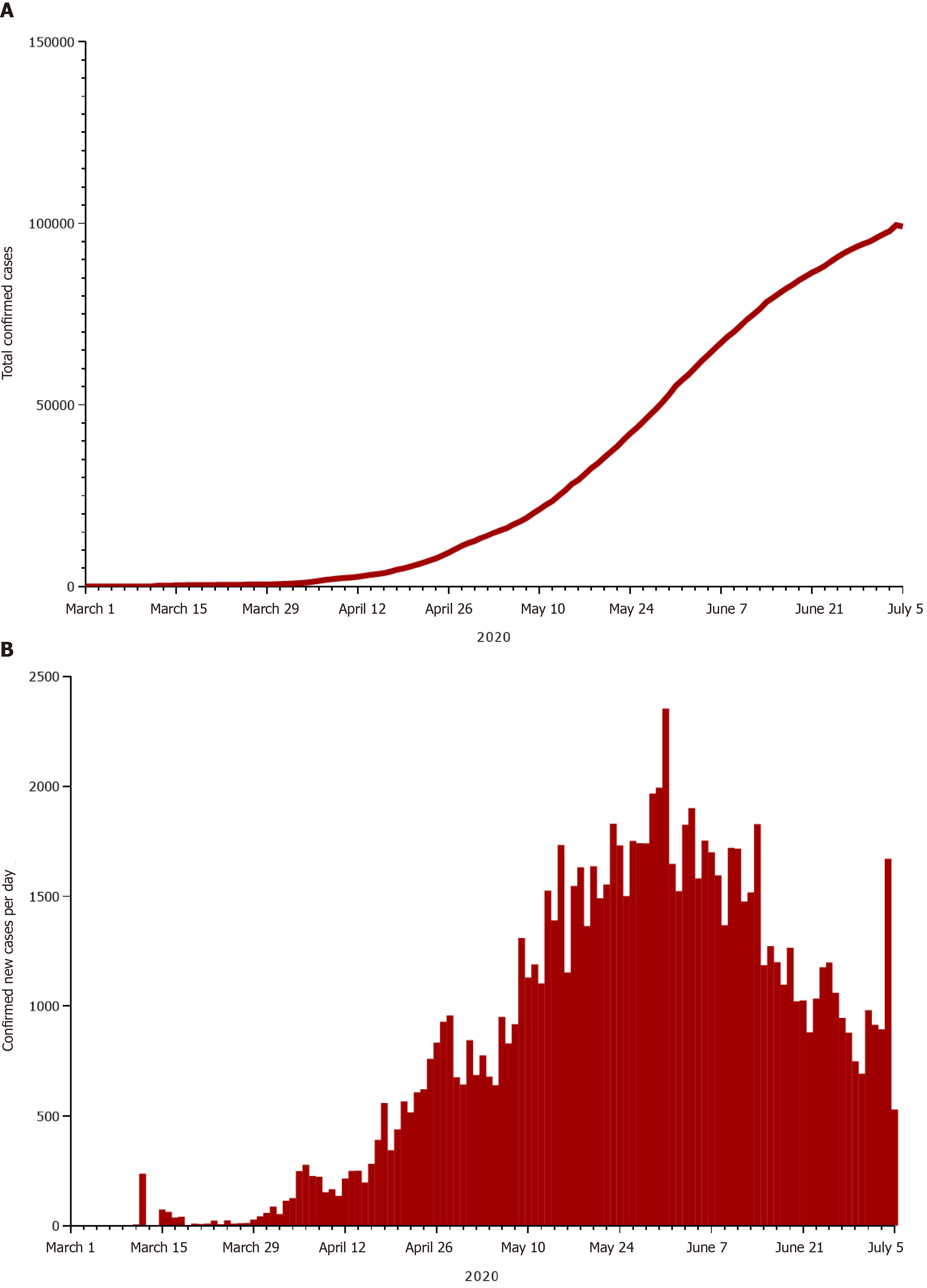
An epidemiological shift in public health priorities from communicable diseases to noncommunicable diseases has been observed in the last two decades. However, humankind continues to grapple with infectious diseases, including Ebola, dengue, middle east respiratory syndrome, and severe acute respiratory syndrome. The novel coronavirus disease (COVID-19) was first identified in the Chinese city of Wuhan in December 2019, and it has spread across the world, causing widespread increases in morbidity and mortality, economic collapses, and social fragmentation. It was classified as a pandemic on March 11, 2020. Qatar recorded its first confirmed case of COVID-19 on February 29, 2020. As of July 6, the total number of tests performed in Qatar stands at 135848 per million population, and there are 99799 confirmed cases (Figure 1A)[1]. Patients with kidney disease, especially those requiring renal replacement therapy (RRT), are at an increased risk for COVID-19 infection and have worse clinical outcomes owing to their underlying immunocompromised state and high frequency of comorbid risk factors such as cardiovascular disease, hypertension, diabetes mellitus, and pulmonary disease. This paper discusses the restructuring of nephrology services to combat COVID-19 in the State of Qatar, the country with the highest number of confirmed cases per million population in the world[1].
Occupying a peninsula on the western coast of the Arabian Gulf, Qatar is an independent state in the Middle East. It has a land area of approximately 11600 km2 and a population of 2.8 million. Qatar’s healthcare expenditure per capita is highest among all countries in the Middle East[2]. More than 85% of the population are noncitizens as a result of international migration of workers from developing countries. There is a high prevalence of risk factors for chronic kidney disease (CKD) such as obesity, diabetes mellitus, and hypertension among citizens and South Asian migrants, which has translated into an increased burden of CKD as well as end-stage renal disease (ESRD)[3,4].
Qatar’s noncitizen population is transient because of the contractual nature of their employment. Many expatriates choose to return to their home countries if a serious illness such as ESRD is diagnosed[5]. Conversely, some patients avail the subsidized RRT in Qatar as they cannot afford such therapy in their native countries. A study of Qatar’s annual data on RRT revealed that the unadjusted prevalence of RRT-treated ESRD was 666 per million population as of 31 December 2019. Forty-two percent of all patients on RRT had a functioning kidney transplant, 47.5% were receiving haemodialysis (HD) therapy, and 10.5% were being treated with peritoneal dialysis (PD).
General nephrology services and renal replacement therapies in Qatar are largely provided by the Ministry of Public Health (MoPH) government hospitals (Hamad Medical Corporation’s network of hospitals); there are no private dialysis/organ transplantation services. Each hospital in the network works as an independent unit with its own budget and staffing arrangements. During the pandemic, the organizational structure has been reformulated such that planning, coordination, and resource management have been centralized. For instance, the Chief of Nephrology Division at Hamad General Hospital, the principal hospital in the capital city of Doha, has been given the responsibility of reconfiguring and expanding nephrology services to meet needs.
A multidisciplinary nephrology operations committee for pandemic preparedness planning and response was formed in February 2020. The committee, which has representation from the nephrology division, administration, nursing staff, technicians, and infection control team, meets regularly to devise and refine action plans based on the evolving COVID-19 situation. It continuously reviews the dialysis treatment capacity of all healthcare facilities in the country and the distribution of the nephrology workforce. It also implements policies and protocols to limit cross infection and clinical care pathways to cope with patient volume during different phases of the pandemic.
In February, when COVID-19 had not yet peaked in most parts of the world, there was a paucity of epidemiological data regarding the impact of COVID-19 on the kidneys. Hence, it was difficult to accurately predict the effect of the pandemic on nephrology health services. Nevertheless, it was anticipated that despite the higher mortality rates associated with previous coronavirus infections, COVID-19 will place a heavier burden on critical care units and create a larger demand for RRT due to its contagiousness. Based on the local prediction models and data from China and the United States, it was estimated that approximately 30%-40% of hospitalized COVID-19 positive patients will require intensive care unit (ICU) admission, and 25% of ICU patients will require RRT[6,7].
Succession and workforce planning are critical because healthcare services often face periods of illness, self-isolation, or quarantine for healthcare professionals during pandemics. Hence, back-up strategies for each key personnel were made. In Qatar, all types of renal replacement therapies are carried out by dialysis nurses, including continuous renal replacement therapy (CRRT). There was a concern that increased demands for RRT during the pandemic will be compounded by the shortage of trained staff thus adversely affecting the staff-to-patient ratio. Hence, a training programme was developed to provide 225 ICU nurses with essential knowledge and skills for performing CRRT procedures.
Advance purchase agreements and stockpiling arrangements were made to acquire HD and CRRT machines as well as portable reverse osmosis units to boost the RRT capacity.
Steps were also taken to ensure that dialysis fluid and consumable dialysis supplies matched the requirements. Anticipating the increased risk of infection in kidney transplant and dialysis patients, policies were implemented to protect this vulnerable group of patients. Focus was placed on measures to mitigate the risk of cross-infection among patients and staff at dialysis centres. A key strategic decision was made by the MoPH to geographically separate and treat COVID-19 patients in designated facilities. Meanwhile, other facilities, including those that usually operate at near-surge capacity, have continued to provide uninterrupted acute health care to patients without COVID-19.
National lockdown and social distancing measures were imposed in March 2020 to curb the spread of the virus and ‘flatten the curve’ (a public health strategy to spread healthcare needs over time). Qatar approached the peak phase of the pandemic in late May 2020, when there were approximately 2300 cases per day (Figure 1B)[8]. Nephrology services were refigured to mitigate the risk of COVID-19 while providing optimized care not only to the vulnerable CKD population but also to the critically ill patients in ICUs, which hinges largely on the provision of RRT. The following are some of the critical changes that have been implemented.
To minimize the risk of viral transmission to healthcare professionals and patients in the outpatient department, in-person patient visits have been eliminated or severely curtailed since March 2020; telemedicine clinics have become a primary mechanism for routine outpatient care. Patients are notified about their upcoming telemedicine appointment via a phone call or text-message a couple of days prior to their appointment. On the day of appointment, the nephrologist calls each patient on the clinic list and addresses their medical needs. If deemed necessary, an in-person visit is arranged by the physician. The patients are screened for fever and symptoms of COVID-19 before entering the clinic area. Although this approach has its limitations, most patients find telemedicine visits more convenient than in-person visits. In our experience, no-show rates have been effectively reduced by telemedicine.
Frequent monitoring of renal function or drug levels is often required for many high-risk and vulnerable patients, such as patients on immunosuppression. Many patients refrained from attending the main hospital laboratory for their blood work in fear of COVID-19. Consequently, a special laboratory service has been created in an isolated area of the hospital, only accessible to kidney disease patients. This has minimized waiting time, given confidence to patients, and improved their compliance with laboratory tests. A home phlebotomy service has also been organized for the elderly or mobility-constrained high-risk individuals.
Since early April, hospital outpatient pharmacies have been closed, and a medication home delivery service has been provided to all patients through a collaborative project with Q-Post, the national postal service. Considering the high demand for this service, which requires up to 3 business days for delivery, a back-up pharmacy has been established in a convenient but secluded area of the hospital to cater only to transplant patients in need of an urgent supply of medication.
Although all acute care hospitals are equipped with ICU facilities to treat COVID-19 patients, the majority of such patients are treated in two of Hamad Medical Corporation’s COVID-19 designated acute care hospitals. The main buildings of these hospitals have been gradually transformed into mega intensive care units that offer advanced respiratory support in a modern ICU environment. A few critically ill COVID-19 patients have been managed in non-COVID-19 hospitals because they were too ill to be transferred; each COVID-19 patient is treated in a dedicated wing of the ICU by dedicated nursing staff to avoid transmission of infection within the facility.
Table 1 compares the baseline and current (6 July 2020) RRT capacities for critically ill patients with acute kidney injury in acute care hospitals. When the projected COVID-19 peak approached, 100 ICU nurses had completed their CRRT training and proved to be an important resource for managing CRRT. Several ICU physicians, nephrologists, and nurses from other hospitals have been redeployed to these facilities to strengthen the workforce. Staying ahead of the curve has been a key strategy, one involving close monitoring of the evolving situation, conducting forward-looking assessments of the adequacy and efficacy of the nephrology services, and expanding the system capacity, erring on the side of overestimation. As a result of these measures, ICUs have never reached maximum occupancy, and RRT capacity has never been constrained despite staff absences due to illness/quarantine.
| Resources | Baseline capacity (December 2019) | Current capacity (July 6, 2020) | Reserve capacity |
| ICU beds | 130 | 529 | 171 |
| Haemodialysis machines | 268 | 347 | - |
| CRRT machines | 8 | 30 | 14 |
| Portable reverse osmosis units | 50 | 95 | - |
| Trained ICU nurses for CRRT | 0 | 100 | 125 |
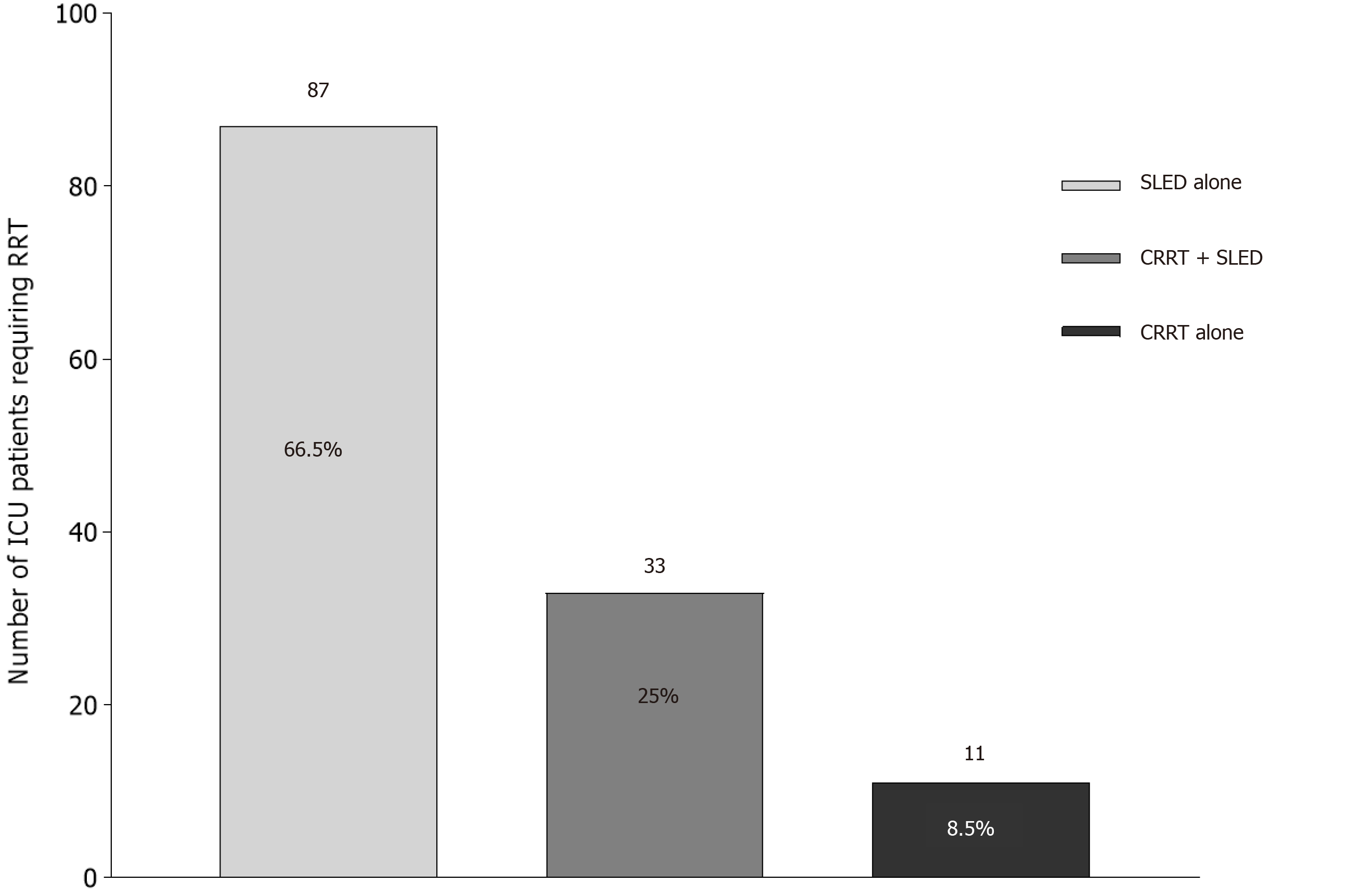
RRT is prescribed and supervised by nephrology physicians, although a collaborative goal-oriented approach agreed upon by nephrology and ICU teams is followed. This team-based approach is particularly helpful in COVID-19 positive patients with coexisting shock and acute respiratory distress syndrome to ensure alignment of critical care fluid interventions and RRT prescription. Sustained low-efficiency dialysis (also known as prolonged intermittent renal replacement therapy, if a CRRT machine is used) using the haemodialysis machine is the main modality of RRT for haemodynamically unstable ICU patients, although all forms of RRT are in use. An informal survey of the largest ICU at a COVID-19 designated facility revealed that sustained low-efficiency dialysis, either alone or in combination with CRRT, was prescribed in more than 90% of the cases of acute kidney injury related to COVID-19 from March 1 to July 3 (Figure 2). High-flow CRRT has not been used although some patients with cytokine storms have been treated with adsorptive membranes to remove inflammatory mediators as a part of a clinical trial. One ICU nurse was able to simultaneously manage two patients on CRRT in double/multiple-occupancy rooms, thereby decreasing organizational costs, conserving personnel protective equipment, and alleviating staffing shortage issues. Interdisciplinary collaboration continues so that experienced dialysis nurses are always around to serve as core-experts and provide guidance.
ICU patients on maintenance PD are managed by PD nurse specialists. To decrease staff exposure and fatigue due to frequent alarms, all patients on cycler-assisted PD are switched to manual PD using three exchanges per day unless the fluid status or biochemical parameters warrant a more intensified regimen. Fluid overload has been successfully managed with hypertonic solutions; to date, none of the patients have required a switch to HD. Used dialysate is disposed of in the dirty utility room and plastic waste in yellow biohazard bags.
Dialysis centres can become a source of viral transmission unless proper infection prevention and control practices are followed. The country’s largest dialysis facility in Doha accommodates 480 HD patients and provides outpatient facilities to 170 PD patients and 350 CKD stage 5 non-dialysis patients. It also has diabetes and podiatry clinics and a pharmacy unit. Preparing a dialysis facility as large as this and training the healthcare professionals to safely manage the patients has been a critical task.
A clinical protocol has been formulated in conjunction with the infection control team and Communicable Disease Centre, taking into consideration the recommendations of international societies and the World Health Organization to prevent, mitigate, and contain transmission to staff, patients, and visitors in the dialysis facilities[9,10]. Staff and patients are educated on hand and respiratory-related hygiene. Staff are fit-tested for N95 respirator masks, trained on proper donning and doffing of personnel protective equipment, and screened fortnightly using COVID-19 PCR. Dialysis centres have adequate signage, and hand sanitizer dispensers are installed at multiple places. All personnel entering the dialysis centre are required to have mandatory body temperature checks using infrared thermal devices. Patients are advised to call ahead if they have fever or symptoms of respiratory tract infection.
Another key strategy is to triage patients upon arrival at the dialysis facility using a questionnaire. Patients with no signs of infection are issued a screening ticket authorizing their entry to the treatment areas. Any patient suspected to be infected is dialyzed in a negative-pressure isolation room or a room with portable HEPA filter. A nasopharyngeal swab is taken and the MoPH notified. The dialysis machine is meticulously disinfected before and after each use.
Confirmed COVID-19 patients are dialyzed at the designated centres (and are red flagged on the Cerner electronic record system). The discharge criteria for patients have been updated by the MoPH during the pandemic.
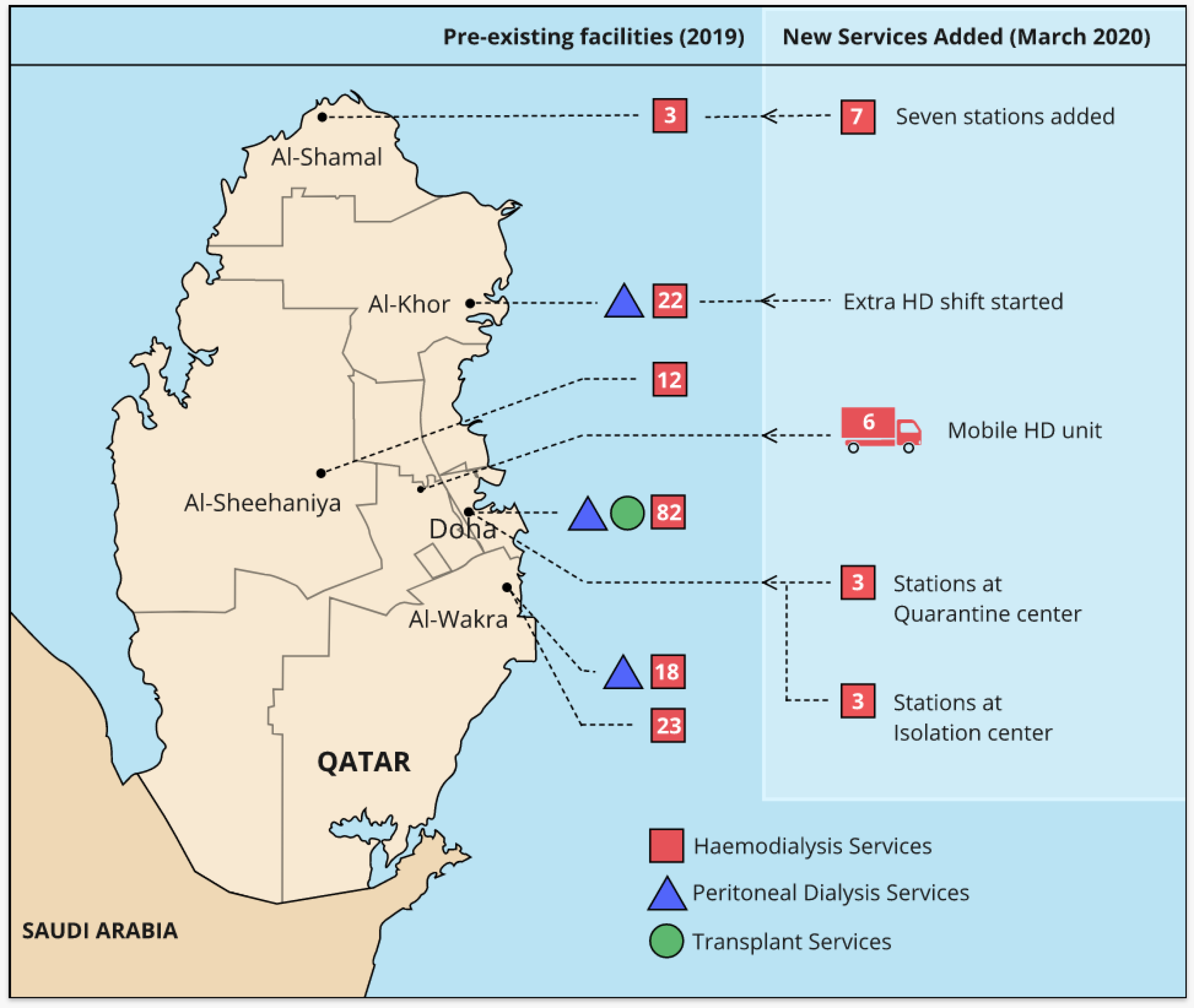
A six-bay mobile modern dialysis truck has been stationed next to one of the main COVID-19 designated acute care hospitals and is currently being used to dialyze stable COVID-19 patients on maintenance HD at field hospitals (Figure 3).
Special treatment rooms have also been set up to provide treatment to maintenance HD patients at quarantine centres (incoming travellers to Qatar and for locally exposed patients) and isolation centres (COVID-19 patients who are stable). Patients at these facilities are dialyzed using NxStage System haemodialysis machines and portable reverse osmosis units and supervised by the home-haemodialysis nephrology team.
An unusual increase in the prevalence of non-COVID-19 patients undergoing maintenance HD has been observed during the pandemic. Expatriates with newly diagnosed ESRD, many of whom would normally opt to return to their home-countries, as well as visitors on maintenance HD are stranded in Qatar due to the air travel disruptions and entry restrictions imposed by several countries. These factors, coupled with a marked decrease in transplant activity, have led to an increased demand for maintenance haemodialysis therapy. To accommodate these patients, extra stations have been added to an existing ambulatory dialysis facility, and an extra shift has been introduced at units that would normally run two shifts of patients per day (Figure 3). Available slots at inpatient HD units are also being utilized to accommodate these additional patients. All these measures have significantly enhanced the capacity to offer maintenance HD to additional patients without compromising the dialysis prescription of pre-existing HD patients.
The lack of public transport during the pandemic has been a significant barrier to commuting for many haemodialysis patients who do not have individual transport. Hamad Medical Corporation’s ambulance service has played a vital role in providing safe transportation to these patients to and from dialysis facilities while following safety guidelines provided by the Communicable Disease Centre. Some of the ambulances are assigned exclusively to transport confirmed or suspected COVID-19 patients between the health facilities. The staff wears the recommended personnel protective equipment, and the ambulance undergoes a deep-clean disinfection after each trip. The ambulance service has seen a 30% increase in the daily activity from COVID-19-related missions during the peak phase.
The COVID-19 pandemic has imposed new challenges and opened new learning opportunities for the Nephrology fellows in the training programme. The weekly fellows' seminar has been put on hold, and some of the fellowship rotations have been modified. The fellows have received brief training in critical care medicine and have been assigned to work in intensive care units under the supervision of intensivists and nephrologists. These changes in their rotation have broadened their learning experience. They have become more confident in managing critically ill patients and in prescribing different modalities of RRT in the ICU setting.
Although the COVID-19 surge appears to be abating in Qatar, the complete eradication of COVID-19 is unlikely to occur anytime soon. It is probable that we will continue to see critically ill COVID-19 patients who require acute nephrology care for the next several months. There is also the possibility of a second wave of the infection. Hence, it would be wise to retain the expanded ICU and RRT treatment capabilities.
Given the pitfalls in the COVID-19 PCR diagnostics, the potential for donor derived/hospital-acquired infection and concerns over the severity of illness in heavily immunosuppressed transplant recipients, organ procurement and transplantation activities have been unfavourably influenced by the COVID-19 pandemic. Methods for reinvigorating the transplant programme are now being considered. Transplant pathways and algorithms have been developed to guide donor and recipient screening and management. In the initial phase, transplantation will be restricted to highly sensitized patients and those with urgent clinical indications, if COVID-19-free pathways can be ensured.
Follow-ups for patients who had COVID-19-related kidney disease, the backlog of postponed living kidney donor and transplant recipient workup, and other nonurgent nephrology services will create a surge in outpatient activity once people overcome the fear of hospitals. Outpatient nephrology services will need to be enhanced to cope with the accumulated elective volumes.
Outbreaks of infectious diseases are likely to pose an ongoing threat to humankind. It is also expected that we will encounter recurrence of COVID-19 outbreaks in the future. Before effective vaccines and medical treatments become available, we need to remain vigilant to detect cases early, devise innovative approaches to protect the vulnerable, and implement infection control strategies to prevent major outbreaks that overwhelm the health services. RRT is a lifesaving treatment, and it is imperative that healthcare systems invest in technical infrastructure, staff, and supplies to provide efficient critical care nephrology services in the setting of a pandemic. We are struck by the reports of physicians working under tremendous pressure and making difficult decisions of ventilator/ICU bed rationing as well as the heroic efforts of nephrologists working with the RRT capacity that has been stretched to the breaking point in regions where the magnitude of the pandemic and healthcare capacity deficits could not have been foreseen[11,12].
We thank Dham T, Abdulla A, Joseph J, Joseph S, and all the Hamad Medical Corporation staff for their excellence in patient care in these extremely difficult times. We also thank Hamza Asim for his assistance with computer graphics.
Manuscript source: Unsolicited manuscript
Specialty type: Urology and nephrology
Country/Territory of origin: Qatar
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Abboud OI S-Editor: Gao CC L-Editor: Filipodia P-Editor: Wang LL
| 1. | Worldometer. Covid-19 coronavirus pandemic. [cited July 6, 2020]. Available from: https://www.worldometers.info/coronavirus/#countries. |
| 2. | Macrotrends. Qatar healthcare spending 2000-2020. [cited July 4, 2020]. Available from: https://www.macrotrends.net/countries/QAT/qatar/healthcare-spending. |
| 3. | World Health Organization. STEPwise approach to chronic disease risk factor surveillance. [cited July 4, 2020]. Available from: https://www.who.int/ncds/surveillance/steps/qatar/en/. |
| 4. | Ramachandran A, Snehalatha C, Shetty AS, Nanditha A. Trends in prevalence of diabetes in Asian countries. World J Diabetes. 2012;3:110-117. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 288] [Cited by in RCA: 306] [Article Influence: 23.5] [Reference Citation Analysis (0)] |
| 5. | Al-Malki H, Rashed AH, Asim M. Renal replacement therapy in Qatar—Past, present and future. Open J Nephrol. 2018;8:42-55. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, Wu Y, Zhang L, Yu Z, Fang M, Yu T, Wang Y, Pan S, Zou X, Yuan S, Shang Y. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8:475-481. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6231] [Cited by in RCA: 6660] [Article Influence: 1332.0] [Reference Citation Analysis (0)] |
| 7. | Lewnard JA, Liu VX, Jackson ML, Schmidt MA, Jewell BL, Flores JP, Jentz C, Northrup GR, Mahmud A, Reingold AL, Petersen M, Jewell NP, Young S, Bellows J. Incidence, clinical outcomes, and transmission dynamics of severe coronavirus disease 2019 in California and Washington: prospective cohort study. BMJ. 2020;369:m1923. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 137] [Cited by in RCA: 134] [Article Influence: 26.8] [Reference Citation Analysis (0)] |
| 8. | World Health Organization. Coronavirus disease (COVID-2019) situation reports. [cited July 6, 2020]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/. |
| 9. | Centers for Disease Control and Prevention. Interim additional guidance for infection prevention and control recommendations for patients with suspected or confirmed COVID-19 in outpatient hemodialysis facilities. [cited July 4, 2020]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/dialysis.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fhealthcare-facilities%2Fdialysis.html. |
| 10. | World Health Organization. Rational use of personal protective equipment for coronavirus disease (COVID-19): Interim guidance, 27 February 2020. [cited July 4, 2020]. Available from: https://apps.who.int/iris/bitstream/handle/10665/331215/WHO-2019-nCov-IPCPPE_use-2020.1-eng.pdf? Sequence=1&isAllowed=y. |
| 11. | Rosenbaum L. Facing Covid-19 in Italy - Ethics, Logistics, and Therapeutics on the Epidemic's Front Line. N Engl J Med. 2020;382:1873-1875. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 556] [Cited by in RCA: 563] [Article Influence: 112.6] [Reference Citation Analysis (0)] |
| 12. | Goldfarb DS, Benstein JA, Zhdanova O, Hammer E, Block CA, Caplin NJ, Thompson N, Charytan DM. Impending Shortages of Kidney Replacement Therapy for COVID-19 Patients. Clin J Am Soc Nephrol. 2020;15:880-882. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 96] [Article Influence: 19.2] [Reference Citation Analysis (0)] |