Peer-review started: December 14, 2018
First decision: December 21, 2018
Revised: February 26, 2019
Accepted: March 27, 2019
Article in press: March 27, 2019
Published online: June 28, 2019
Processing time: 196 Days and 12.1 Hours
Hemodialysis machine-generated circuit pressures and clearance profiles are potential predictors of quality assurances. In our practice, we previously we observed that elevated static access pressures were associated with abnormal Kt/V values, high access recirculation and deviation of the Kt/V profile (Abnormal Kt/V profile) from normally expected values (Normal Kt/V profile).
To hypothesize that static or derived access pressures would correlate with direct intra-access blood flow rates and that clearance (Kt/V) profiles would correlate with measured Kt/V values.
Static access pressures, real-time adequacy of dialysis and intra-access blood flow were investigated in end stage renal disease patients undergoing hemodialysis. Wilcoxon-Mann-Whitney test, chi-square test or Fisher’s exact test was used to investigate differences between the groups; Spearman’s rank correlation test to investigate relationships between static pressures, direct intra-access pressures and Kt/V profiles; and multinomial logistic regression models to identify the independent effect of selected variables on Kt/V profiles. Odds ratio were calculated to measure the association between the variables and Kt/V profiles.
One hundred and seven patients were included for analysis. There were no significant differences between genders, and types of vascular access between the normal vs. abnormal clearance (Kt/V) profile groups. No significant correlation could be demonstrated between static access pressures and Kt/V profiles, static access pressures and intra-access blood flow, intra-access blood flow and Kt/V profiles, measured Kt/V and Kt/V profiles or recirculation and Kt/V profiles.
In this study utilizing measured versus estimated data, we could not validate that dialysis machine generated elevated static pressures predict intra-access blood flow disturbances or that abnormal Kt/V profiles predict access recirculation or inadequate dialysis. These parameters, though useful estimates, cannot be accepted as quality assurance for dialysis adequacy or access function without further evidences.
Core tip: Hemodialysis machine-generated circuit pressures and clearance profiles are potential predictors of quality assurances. We hypothesized that static or derived access pressures would correlate with direct intra-access blood flow rates and that Kt/V profiles would correlate with measured Kt/V values. However, we could not validate that dialysis machine generated elevated static pressures predict intra-access blood flow disturbances or that abnormal Kt/V profiles predict access recirculation or inadequate dialysis. While future larger studies are needed to confirm these findings, we believe our study serves as a basis for them.
- Citation: Koratala A, Dass B, Alquadan KF, Sharma S, Singhania G, Ejaz AA. Static pressures, intra-access blood flow and dynamic Kt/V profiles in the prediction of dialysis access function. World J Nephrol 2019; 8(3): 59-66
- URL: https://www.wjgnet.com/2220-6124/full/v8/i3/59.htm
- DOI: https://dx.doi.org/10.5527/wjn.v8.i3.59
On-line monitoring of ultraviolet (UV) absorption of spent dialysate during routine hemodialysis allows continuous measurement of removed solutes from spent dialysate. The continuous calculation of the clearances-adequacy of dialysis (Kt/V) - throughout therapy is graphically displayed and allows clinicians to monitor the efficacy of the dialysis treatment in real time, the so-called dynamic Kt/V profile. Previously we observed that elevated static access pressures were associated with abnormal Kt/V values, high access recirculation and deviation of the Kt/V profile (Abnormal Kt/V profile) from normally expected values (Normal Kt/V profile). These observations suggested the possibility that dialysis machine-generated real-time Kt/V profiles may provide a non-invasive, inexpensive and quick assessment of adequacy of dialysis and access function in hemodialysis patients. To validate our observations, we performed a larger, prospective observational study. We hypothe-sized that static or derived access pressures would correlate with direct intra-access blood flow rates and that Kt/V profiles would correlate with measured Kt/V values.
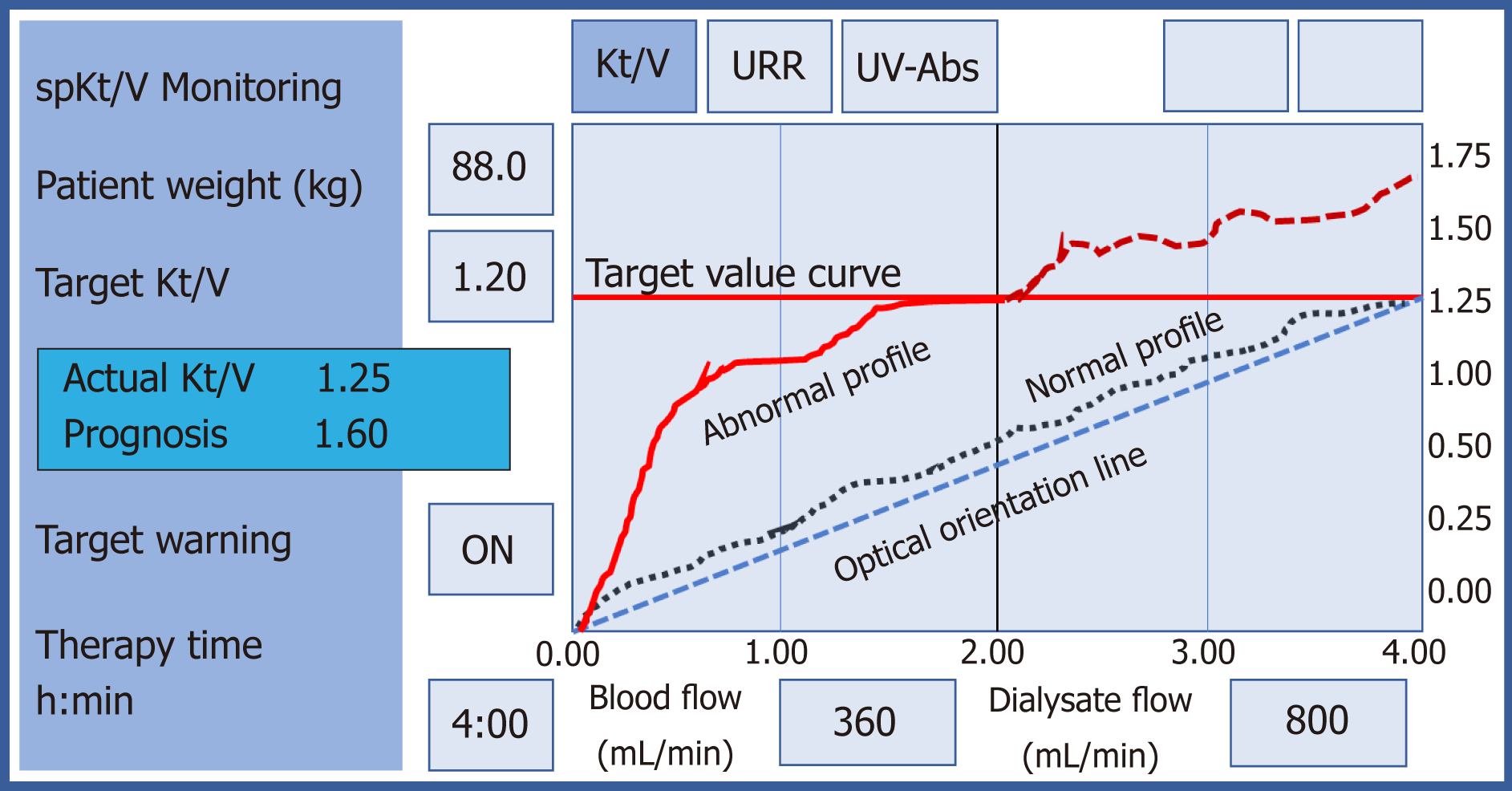
End stage renal disease patients undergoing maintenance hemodialysis at the outpatient dialysis unit of an academic medical center were included in the study. All patients were dialyzed with Dialog (B Braun AG)TM dialysis machine with a built-in UV-Spectrophotometer (Option Adimea, B Braun AGTM). The machine continually calculates the adequacy of dialysis (Kt/V) throughout therapy and graphically displays Kt/V profile and an indication of how close it is to the target (Figure 1). Fluctuations in the predicted curve caused by changes in variables affecting Kt/V are visible at a glance. Abnormal Kt/V profile was defined as major fluctuations from the predicted curve displayed. The standard dialysis prescription was high-flux polysulfone dialyzers (F160; Fresenius, Worcester, MA, United States), blood flow rate of 350-450 mL/min, dialysate flow rate of 500-800 mL/min and ultrafiltration rates of 5-10 mL/kg·h as appropriate. Anticoagulation was not used in patients per divisional protocol. Only patients with functional arteriovenous fistula or graft were included in the study.
The ESRD program in this academic center employed an Access Surveillance Program and the team members included nephrologists, nephrology nurses, technicians, interventional radiologists, surgeons, primary care physicians and patients. Functional access was defined as blood flow > 600 mL/min[1]. Vascular access dysfunction was defined as elevated static or derived venous pressures (PV), elevated negative arterial pre-pump pressures (PA) that prevent increasing to acceptable blood flow rates, or unexplained decreases in the measured amount of hemodialysis delivered (Kt/V). Critical intra-access blood flow was defined as AVF blood flow < 600 mL/min, AVG blood flow < 800 mL/min, or decreased intra-access blood flow by > 20% compared to previous values[2,3]. Direct intra-access flow measurements were performed with ultrasound dilution (Transonic Systems Inc.TM). Clinically significant access recirculation was defined as values more than 5%. The demographic information was obtained from the chart, the static pressures and Kt/V profiles were obtained by direct visualization of the dialysis machine display screen, the Kt/V values obtained from biochemical measurements, and intra-access blood flow data were obtained from Transonic measurement data. The study was approved by the Institutional Review Board at the University of Florida.
Results are presented as mean ± SE with P-value. Wilcoxon-Mann-Whitney test was used to compare independent groups not normally distributed, χ2 test or Fisher’s exact test for comparison between two categorical variables, and P value < 0.05 was considered statistically significant. Associations between static pressures, direct intra-access pressures and Kt/V profiles were investigated using Spearman’s rank correlation test (rs) and regression analysis where applicable. These predictors were included in a univariate and subsequent multinomial logistic regression model to identify their independent effect on Kt/V profiles. The strength of the association of each variable with Kt/V profiles were summarized by calculating an odds ratio (OR) and a corresponding 95%CI. All analyses were conducted using SPSS version 20 (Chicago, IL, United States). The study conception, design, execution, data collection, analysis, and manuscript preparation were formed in its entirety and independently by the investigators. Every author had independent access to the analysis.
The analysis included 107 patients. The baseline characteristics of the patients are shown in Table 1. There were no significant differences between age, gender, types of vascular access, PA, intra-access flow rates or percentage of patients with abnormal access recirculation between the Normal vs. Abnormal Kt/V profile groups. How-ever, the Abnormal Kt/V profile group had significantly lower PV and higher measured Kt/V values. Twenty-one patients underwent access recirculation studies, twelve in the Normal Kt/V group and nine in the Abnormal Kt/V group. Access recirculation test was positive in 12/12 patients studied in the Normal Kt/V profile group and 8/9 patients in the Abnormal Kt/V profile group. The percentages in their respective groups are shown in Table 1.
| Variables | Full cohort (n = 107) | Normal Kt/V profile (n = 68) | Abnormal Kt/V profile (n = 39) | P-value |
| Demographics | ||||
| Age (yr) | 54.9 ± 1.5 | 56.5 ± 1.8 | 52.3 ± 2.8 | 0.210 |
| Male gender (%) | 52.3 | 46.1 | 53.8 | 0.843 |
| Access types | ||||
| AV fistula (%) | 63.5 | 58.8 | 71.8 | 1.000 |
| AV graft (%) | 36.5 | 41.2 | 28.2 | 1.000 |
| Access pressures and flow rates | ||||
| Static PA (mmHg) | -196.7 ± 4.1 (-203)1 | -196.2 ± 4.6 (-202) | -197.5 ± 7.9 (-206) | 0.884 |
| Static PV (mmHg) | 240.8 ± 5.5 (244) | 249.9 ± 7.2 (254) | 224.8 ± 7.9 (235) | 0.021 |
| Intra-access flow rate | 1369.5 ± 82.8 (1070) | 1256.3 ± 87.4 (1035) | 1566.8 ± 165.6 (1170) | 0.103 |
| Adequacy of dialysis | ||||
| Measured Kt/V | 1.42 ± 0.04 (1.46) | 1.40 ± 0.04 (1.44) | 1.45 ± 0.07 (1.51) | < 0.001 |
| Access recirculation > 5% (n = 21) (%) | 18.7 | 17.4 | 20.5 | 0.429 |
No significant association could be demonstrated between PA and Kt/V profile groups, nor between PA and absolute Kt/V values (Table 2). However, significant associations were noted between PV and Kt/V profiles. When analyzed for highest quartile of PV values (PVQTRL), no significant associations were found between PVQTRL and Kt/V profiles or Kt/V values.
| Strength of association | ||
| Variables | rs | P-value |
| Static PA – Kt/V profiles | -0.05 | 0.636 |
| Static PA – Kt/V | -0.14 | 0.155 |
| Static PV – Kt/V profiles | 0.19 | 0.047 |
| Static PVQTRL – Kt/V profiles | -0.17 | 0.078 |
| Static PA – Intra-access blood flow | -0.25 | 0.009 |
| Static PA – Intra-AVF blood flow | -0.22 | 0.069 |
| Static PA – Intra-AVG blood flow | -0.16 | 0.319 |
| Static PV – Intra-access blood flow | 0.04 | 0.666 |
| Intra-access blood flow - Kt/V profile | -0.12 | 0.208 |
| Intra-AVF blood flow - Kt/V profile | 0.17 | 0.174 |
| Intra-AVG blood flow - Kt/V profile | 0.05 | 0.783 |
| Critical intra-access blood flow - PA | 0.24 | 0.226 |
| Critical intra-access blood flow - PV | 0.14 | 0.482 |
| Critical intra-access blood flow – Kt/V profile | 0.01 | 0.962 |
| 20% reduced intra-access blood flow – Static PA | -0.15 | 0.262 |
| 20% reduced intra-access blood flow – Static PV | -0.03 | 0.851 |
| 20% reduced intra-access blood flow – Kt/V profile | 0.14 | 0.294 |
| Access recirculation > 5% - Kt/V profile | 0.20 | 0.389 |
| Kt/V – Kt/V profile | -0.08 | 0.397 |
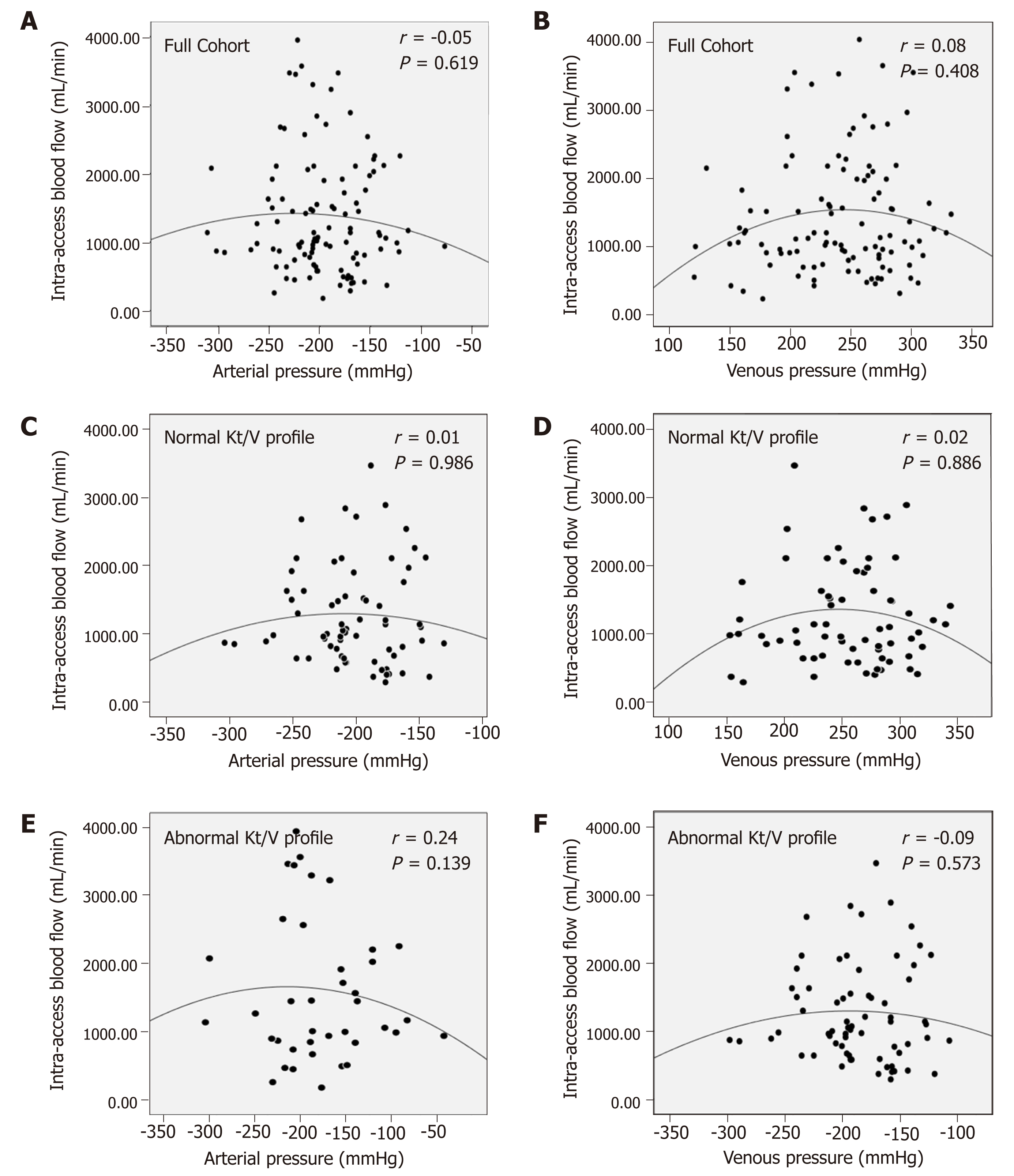
No significant association could be demonstrated between PA or PV and intra-access blood flow, even when analyzed separately for AVF and AVF. When plotted against PA or PV, intra-access blood flow exhibited a quadratic relationship (Figure 2A,B). Similar patterns were revealed when plotted separately for Kt/V profiles (Figure 2C-F) and access types (Figures not shown).
No significant association could be demonstrated between intra-access blood flow and Kt/V profiles.
No significant association could be demonstrated between critical intra-access blood flow and static pressures or Kt/V profiles.
No significant association could be demonstrated between Kt/V and Kt/V profiles.
No significant association could be demonstrated between access recirculation and Kt/V profiles. The odds ratio for positive access recirculation associated with Abnormal Kt/V profile was 2.5 (95%CI: 1-5-4.2; P = 0.429).
In univariate analysis, age (OR = 1.02, 95%CI: 0.99-1.04, P = 0.186), gender (OR = 1.10, 95%CI: 0.50-2.42, P = 0.813), type of access (OR = 1.78, 95%CI: 0.76-4.16, P = 0.182), PA (OR = 1.00, 95%CI: 0.90-1.00, P = 0.874) and intra-access blood flow rates (OR = 1.00, 95%CI: 0.99-1.00, P = 0.075) were not significant risk factors for Abnormal Kt/V profile. However, PV (OR = 1.01, 95%CI: 1.00-1.02, P = 0.033) was a significant risk factor. In the multivariate regression model that included all of these variables irrespective of their statistical significance in the univariate model, none of them were significant predictors of Abnormal Kt/V profile.
UV absorption technology has enabled dynamic monitoring of dialysis efficiency in real time and the potential for non-invasive and quick assessment of access function. In this study we investigated the validity of these observations by analyzing the association between machine-generated data and measured data in patients under-going maintenance dialysis.
The major finding of the study was the lack of significant association between static access pressures and direct intra-access blood flow, Kt/V profiles and direct intra-access blood flow or Kt/V profiles and Kt/V values. The significant associations seen between PV and Kt/V profile and PA and intra-access blood flow could not be demonstrated in the adjusted regression model. The findings are better understood when considering that static access pressures are arterial and venous circuit pressures that are generated by transducers inside the machine. The arterial pump effect is measured as the arterial pressure and is dependent on the blood flow within the tubule, which is dependent on the internal diameter of the tubing segment within the pump. Effective blood flow deviates significantly from calculated blood flow when PA ≤ −150 mmHg and can lead to loss of treatment efficiency[4]. PV are monitored distal to the dialyzers and usually located before the air bubble chamber. Low PV may be due to low PA secondary to poor arterial flow. High PV indicate an obstruction in the venous limb distal to this point and can be due to venous needle blow out or clots in the air trap, kinks in the tubing or a stenosis within the vascular access. Equating elevated static pressures to vascular access problems maybe deceptive as suggested by our findings.
Data was also analyzed according to access types as the sites of stenosis vary accordingly. In AVF, problems occur in the arterial inflow (forearm AVF 55%, upper arm AVF 17%) or between the needles (forearm AVF 19%, upper arm AVF 17%). In contrast, majority of stenosis in AV grafts are in the venous outflow (93%)[5,6]. The validity of the major findings of this study of no significant association between study parameters persisted in this subgroup. This was also true when analyzed for critical intra-access blood flow in the two types of vascular access group. We did not deter-mine absolute static intra-access pressure ratios due to its reported limitations in detecting flow limiting problems on the arterial inflow or between the dialysis needles where most problems occur in AVFs.
Close concordance between the blood-based and UV-based Kt/V values has been reported[7,8], however the relationship between Kt/V profiles and Kt/V has hitherto not been studied. In our investigations we could not demonstrate significant correla-tion between Kt/V profile and Kt/V values. Technical factors including volume of distribution and mass transfer coefficients affect dialysate absorbance and confound clearance results. A dialyzer membrane has different filtration rate for molecules of different compounds and for this reason concentrations of these substances, both in blood and in the dialysis do not change according to one pattern. While the UV-absorbance correlates well to the concentration of small solutes such as urea, creatinine and uric acid in the spent dialysate and in the blood at a fixed wavelength of 285 nm, the lowest correlations exist for sodium, calcium, glucose, vitamin B12 and albumin[9]. Medications and fluid administration during dialysis may therefore affect clearance outputs.
Determining the percentage of access recirculation is used to evaluate adequacy of dialysis clearance. Access recirculation decreases adequacy of dialysis and has been used to indicate access issues. Despite the high percentage of positive access recir-culation present in the patients studied in both groups, no correlation was demonstrated with Kt/V profiles. Thus, in our current investigation utilizing a surveillance measure and a clinical monitoring measure simultaneously, we could not validate that dialysis machine generated elevated static pressures predict intra-access blood flow disturbances or that abnormal Kt/V profiles predict access recirculation or inadequate dialysis. These parameters, though useful estimates, cannot be accepted as quality assurance for dialysis adequacy or access function without further studies.
The monitoring of dialysate ultraviolet absorbance and hemodialysis machine generated clearance profiles is a validated technology to measure dialysis adequacy (Kt/V) and allows for continuous and real-time tracking during each session. The Kt/V profile displayed by the machine includes the delivered-dose curve superimposed on the anticipated trajectory.
In our practice, we noted that that elevated static access pressures were associated with abnormal Kt/V values, high access recirculation and deviation of the Kt/V profile (Abnormal Kt/V profile) from normally expected values (Normal Kt/V profile).
Based on the above observation, we hypothesized that static or derived access pressures would correlate with intra-access blood flow rates and that clearance (Kt/V) profiles would correlate with measured Kt/V values.
We investigated static access pressures, real-time adequacy of dialysis and intra-access blood flow in patients undergoing hemodialysis. Appropriate statistical methods were used to investigate differences between the groups; relationships between static pressures, direct intra-access pressures and Kt/V profiles; and identify the independent effect of selected variables on Kt/V profiles. Odds ratio were calculated to measure the association between the variables and Kt/V profiles.
Among the 107 participants included, no significant correlation could be demonstrated between static access pressures and Kt/V profiles, static access pressures and intra-access blood flow, intra-access blood flow and Kt/V profiles, measured Kt/V and Kt/V profiles or recirculation and Kt/V profiles.
We could not validate that dialysis machine generated elevated static pressures predict intra-access blood flow disturbances or that abnormal Kt/V profiles predict access recirculation or inadequate dialysis.
The investigated hemodialysis machine-generated parameters and access flows, though useful estimates can’t be accepted as quality assurance for dialysis adequacy or access function without further evidences. Larger studies are needed to formulate protocol-driven modifications to treatment parameters, which may serve as valuable nursing tools for optimizing patient therapy outcomes.
Manuscript source: Unsolicited manuscript
Specialty type: Urology and nephrology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mahmoud KM, Nechifor G, Trkulja V S-Editor: Ma YJ L-Editor: A E-Editor: Wang J
| 1. | National Kidney Foundation, Inc. K/DOQI Guidelines–Updates 2006. New York: National Kidney Foundation, Inc; 2001; Available from: http://www.kidney.org/PROFESSIONALS/kdoqi/guideline_upHD_PD_VA/index.htm. |
| 2. | Lee T, Mokrzycki M, Moist L, Maya I, Vazquez M, Lok CE; North American Vascular Access Consortium. Standardized definitions for hemodialysis vascular access. Semin Dial. 2011;24:515-524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 184] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 3. | Hurst FP, Lee RE, Thompson AM, Pullin BD, Silverstein DM. FDA Regulatory Perspectives for Studies on Hemodialysis Vascular Access. Clin J Am Soc Nephrol. 2018;13:513-518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 4. | Twardowski ZJ, Haynie JD, Moore HL. Blood Flow, Negative Pressure, and Hemolysis During Hemodialysis. Home Hemodial Int. 1999;3:45-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Turmel-Rodrigues L, Pengloan J, Baudin S, Testou D, Abaza M, Dahdah G, Mouton A, Blanchard D. Treatment of stenosis and thrombosis in haemodialysis fistulas and grafts by interventional radiology. Nephrol Dial Transplant. 2000;15:2029-2036. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 277] [Cited by in RCA: 233] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 6. | Tessitore N, Bedogna V, Lipari G, Melilli E, Mantovani W, Baggio E, Lupo A, Mansueto G, Poli A. Bedside screening for fistula stenosis should be tailored to the site of the arteriovenous anastomosis. Clin J Am Soc Nephrol. 2011;6:1073-1080. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Castellarnau A, Werner M, Günthner R, Jakob M. Real-time Kt/V determination by ultraviolet absorbance in spent dialysate: technique validation. Kidney Int. 2010;78:920-925. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 42] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 8. | Mohamed A, Davenport A. Comparison of methods to estimate haemodialysis urea clearance. Int J Artif Organs. 2018;41:371-377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 9. | Fridolin I, Magnusson M, Lindberg LG. On-line monitoring of solutes in dialysate using absorption of ultraviolet radiation: technique description. Int J Artif Organs. 2002;25:748-761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 44] [Article Influence: 2.0] [Reference Citation Analysis (0)] |