Published online Dec 17, 2018. doi: 10.5527/wjn.v7.i8.148
Peer-review started: September 3, 2018
First decision: October 8, 2018
Revised: October 25, 2018
Accepted: December 5, 2018
Article in press: December 5, 2018
Published online: December 17, 2018
Processing time: 106 Days and 1.6 Hours
Patients with acute kidney injury (AKI) in the intensive care unit (ICU) are often suitable for palliative care due to the high symptom burden. The role of palliative medicine in this patient population is not well defined and there is a lack of established guidelines to address this issue. Because of this, patients in the ICU with AKI deprived of the most comprehensive or appropriate care. The reasons for this are multifactorial including lack of palliative care training among nephrologists. However, palliative care in these patients can help alleviate symptoms, improve quality of life, and decrease suffering. Palliative care physicians can determine the appropriateness and model of palliative care. In addition to shared decision-making, advance directives should be established with patients early on, with specific instructions regarding dialysis, and those advance directives should be respected.
Core tip: Role of palliative medicine in nephrology is not well defined and the patients with acute kidney injury in the intensive care unit may not receive the most comprehensive care surrounding their illness due to scarcity of established palliative care guidelines and lack of palliative care training among nephrologists. A multidisciplinary approach involving palliative care physician early in the course of illness may help in comfort care of acute kidney injury patients in the intensive care unit. Shared decision-making and advance directives play an important role guiding the physician as to what patient wishes are, and those decisions should be respected.
- Citation: Krishnappa V, Hein W, DelloStritto D, Gupta M, Raina R. Palliative care for acute kidney injury patients in the intensive care unit. World J Nephrol 2018; 7(8): 148-154
- URL: https://www.wjgnet.com/2220-6124/full/v7/i8/148.htm
- DOI: https://dx.doi.org/10.5527/wjn.v7.i8.148
Intensive care unit (ICU) patients with acute kidney injury (AKI) have a high mortality rate and renal replacement therapy is not cost-effective in these patients[1]. Physicians in the ICU often face challenging situations when potentially inappropriate treatment has to be withdrawn in critically ill patients[2]. Various factors make these situations more complex; incapacitated state of ICU patients, the option of temporary dialysis due to reversible nature of AKI, and inadequate knowledge of surrogate decision-makers about the goals of care and prognosis[2]. Palliative medicine has a well-established role in many chronic disease states and principles of palliative care are well established for the management of end-stage disease symptoms. However, the role of palliative medicine in the field of nephrology is not well defined and patients with AKI leading to fluid overload, acidosis, hyperkalemia, acute respiratory distress syndrome, respiratory failure and multisystem organ dysfunction with hypotension and sepsis in the ICU may not receive the most comprehensive or appropriate care surrounding their illness. A multitude of factors contribute to this; lack of palliative care training among nephrologists, lack of epidemiological research on outcomes and scarcity of established palliative care guidelines for management of AKI patients in the ICU results in a substandard level of care. However, a multidisciplinary approach by involving palliative care physician early in the course of illness may help in comfort care of AKI patients in the ICU. In this review, we discuss the use of palliative medicine in this specific patient population.
One of the main reasons why palliative care is rarely offered to AKI patients in the ICU setting is the lack of palliative medicine training in most nephrology programs. As a result, most nephrologists may not feel comfortable or compelled to provide these services at an appropriate time. To help solve this issue, nephrology fellows in the future during their training should receive some exposure to palliative care, especially in the ICU setting. There are well-established prognostic indicators from multitudes of epidemiological research on disease progression and outcomes in end-stage renal disease (ESRD) patients. Due to this, nephrologists frequently consult palliative medicine in situations when it may be appropriate for the ESRD patient to withdraw from chronic dialysis. However, AKI patients on dialysis in the ICU may not have palliative care offered at an appropriate time due to the lack of guidelines/recommendations to make a clinical judgment. The following discussion may serve as a guide to nephrologists for providing palliative care to patients with AKI in the ICU.
Kao et al[3] conducted a retrospective cohort study to investigate in-hospital mortality and long-term survival rates in critically ill patients with AKI or ESRD receiving renal replacement therapy. This study found that overall in-hospital mortality was 66.5% and there was no significant difference in mortality rates between AKI and ESRD groups (adjusted odds ratio: 0.93; 95%CI: 0.84-1.02)[3]. Hypertension was found to be a high-risk factor for in-hospital mortality in patients with AKI while older age, chronic liver disease and history of cancer were found to be independent risk factors for in-hospital mortality in both AKI and ESRD groups[3]. In addition, older age, coronary artery disease, and ICU admissions were found to be risk factors in AKI patients for long-term dialysis dependence[3]. In another study, Bagshaw et al[4] investigated risk factors and outcomes associated with critically ill septic AKI patients in ICU. Compared to non-septic AKI group, septic AKI group had greater severity of illness (P = 0.0001), hypotension (P = 0.0001), tachycardia (P = 0.0001), worse lung function measures (P = 0.0001), higher white cell counts (P = 0.0001) and significant acidemia (P = 0.0001)[4]. Also, septic AKI group was associated with a higher crude mortality rate in the ICU (19.8% vs 13.4%, P ≤ 0.001) and in the hospital (29.7% vs 21.6%, P < 0.001) compared to non-septic AKI group[4]. Furthermore, a recent prospective cohort study involving septic AKI patients undergoing dialysis in the ICU found that norepinephrine use, hepatic failure, medical condition, blood lactate, and pre-dialysis creatinine level were associated with early mortality (seven days)[5].
Palliative care should be considered for all high-risk AKI patients in the ICU determined by the presence risk factors associated with poor outcome or high mortality rates as discussed earlier. Three palliative care models have evolved over two decades with an aim to improve quality of care and reduce suffering in the ill patients[6]. These models of care may be considered in the ICU setting for AKI patients as appropriate.
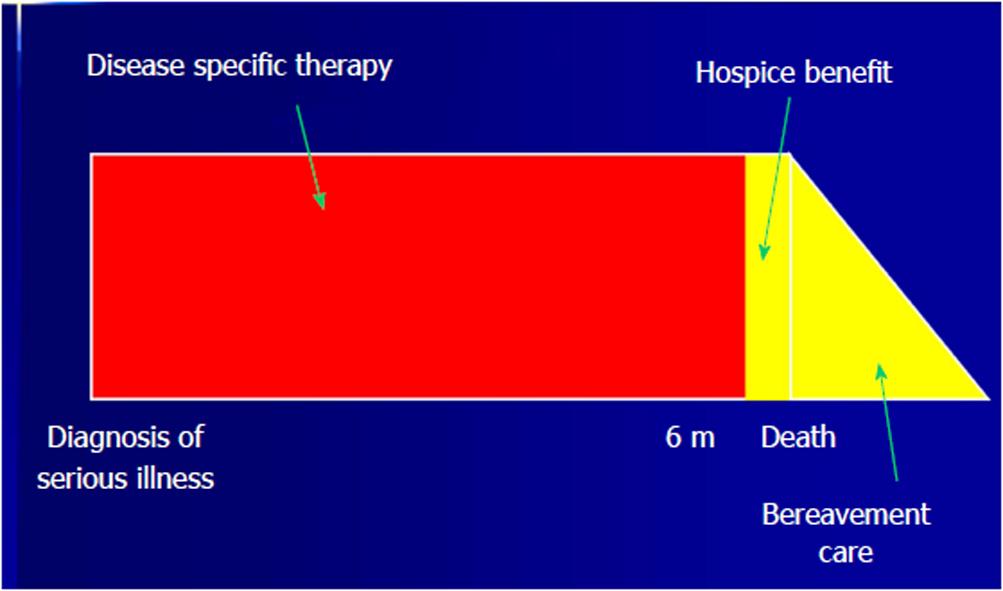
Conventional model of care: This is also called as the traditional dichotomous model of palliative care where ICU patients receive curative or disease-specific care for AKI till it fails following which palliative care will be initiated[7]. This dichotomous model offers AKI patients either curative/disease-specific care or palliative care but not both simultaneously, which leads to a sudden transition from curative to palliative care without enough transition time (Figure 1)[6,7]. The Conventional model of care is suitable for young AKI patients in the ICU without high-risk factors associated with the poor outcome such as septic shock, acidemia, hypertension, coronary artery disease, chronic liver disease and history of malignancy. Given higher resolution rates in this patient population, curative or disease-specific therapy is given first for the management of AKI till it is unsuccessful and then palliative care is initiated.
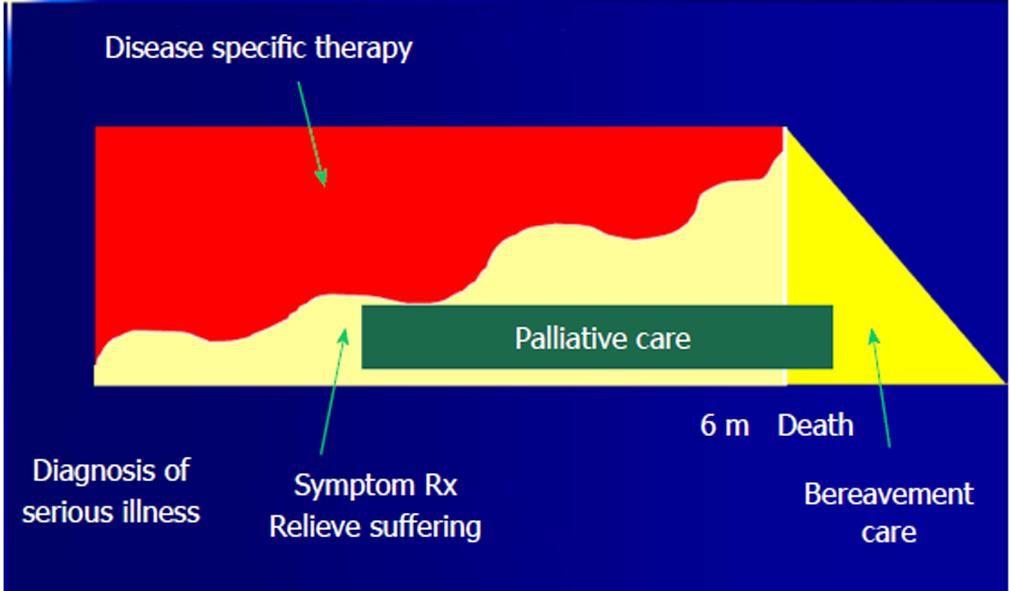
Comprehensive model of care: This is also called as the overlapping model of palliative care where ICU patients receive both curative or disease-specific care for AKI and palliative care simultaneously (Figure 2)[7]. Although this model of care is dichotomous, it offers both curative/disease-specific and palliative care simultaneously to the patients with a gradual increase in palliative care over time and slow withdrawal of curative/disease-specific care[6,7]. However, both of these dichotomous models of care have the disadvantage of providing one model of care at the cost of the other[6]. The Comprehensive model of care is suitable for older AKI patients in the ICU with multiple comorbid conditions in addition to the presence of high-risk factors for the poor outcome such as septic shock, acidemia, hypertension, coronary artery disease, chronic liver disease, history of malignancy and history of prior ICU admissions. Due to the poor outcome and higher mortality rates in this patient population, concurrent initiation of palliative care early in the course of medical management helps to prevent and relieve suffering from pain and other physical, psychological, emotional and spiritual distress[7].
Conceptualization model of care: This is also called as the individualized integrated model of palliative care where ICU patients concurrently receive both palliative care and curative or disease-specific care for AKI, but individualized to suit the needs of the AKI patients and family members[7]. In this model of care, palliative care extends beyond the death of the patient to include bereavement care for the family members[7]. In addition, the intensity of palliative care varies based on the needs of the patient or family member during the course of management[7]. Conceptualization model of palliative care is best suited for poor prognostic AKI patients in the ICU with multiple comorbidities and multi-organ failure. This model of care classifies all the interventions and options of care based on goals allowing more flexible management[6]. Once the palliative care is consulted for the impending death of a family member or friend that entails life-changing events and dynamics, the conceptual model helps in supportive intervention to educate family caregivers about stress coping strategies and creates a perception that they have necessary skills to confront problematic situations. (1) Cure-seeking care: Aim to eliminate the underlying disease/medical problem with medical treatment[6]. For example, treatment of sepsis, hypotension, acidosis, electrolyte imbalance, and underlying connective tissue and immunological disorders in AKI patients; (2) Life-extending care: Aim to prolong life in chronic disease states with the help of medical treatment while also enhancing the quality of life[6]. For examples, AKI patients with long-term dialysis dependence; (3) Quality of life and comfort maximizing care: Aim to improve function, reduce suffering and enhance the quality of life in AKI patients in the ICU, and these interventions may also prolong life[6]; (4) Family supportive care: Aim to address the grief and emotions of the family members from the time of diagnosis to past death[6]. The key variables that should be considered for supportive care interventions for family members are[8]; preparedness of the caregivers for the tasks and demands of the role, mastery to manage stress, competence to adapt more quickly to the situation, self-efficacy to manage a situation with coping behaviors, social support to the caregivers, positive emotions to reframe the stressful situations in a positive way, optimism of caregivers to neutralize some potentially negative aspects of caregiving[8]; (5) Healthcare staff supportive care: Aim to address the grief and emotions related to the management of these AKI patients in the ICU[6].
Patel et al[9] described outcomes and decision-making process for nephrologists in the management of AKI in the ICU setting. Expected outcomes and prognosis for patients with AKI remain poor with the mortality rate of 28%-90%[10]. The highest prognostic indicators for mortality were concomitant multi-organ failure, mechanical ventilation, liver-failure, and malignancy[9,11,12]. These prognostic indicators aid physicians to offer palliative care at an appropriate time in this patient population. Furthermore, the use of the RIFLE (Risk, Injury, Failure, Loss of kidney function, and End-stage kidney disease) criteria to establish predicted mortality was around 80%-85% and that, while not perfect, could still be an acceptable tool to help establish the prognosis for AKI patients in the ICU[9,13]. However, in those patients who survive, 70%-90% have a recovery of kidney function[12,13]. Hence RIFLE criteria can be considered when making clinical decisions regarding the discontinuation of dialysis in AKI patients[12,13]. The Renal Physicians Association/American Society of Nephrology (RPA/ASN) guideline, Shared Decision-Making in the Appropriate Initiation of and Withdrawal from Dialysis, helps to establish general recommendations in certain situations in which dialysis may be discontinued[14]. These situations are: (1) a patient with full capacity for judgment who asks for dialysis to be discontinued; (2) a patient who lacks capacity but previously expressed a desire not to continue dialysis; (3) a patient without capacity but power of attorney asking to withdraw dialysis; (4) a patient who has irreversible, profound neurological impairment; (5) a patient who has a terminal illness (severe cirrhosis, end stage pulmonary disease, advanced stage of cancer) with a life expectancy of ≤ 6 mo. In these situations, it is appropriate to consult palliative care and develop a plan to proceed with the discontinuation of dialysis.
Advance directives also play an important role in clinical decision-making. The presence of an advance directive gives clinicians a guide as to what patient wishes are, and those decisions should be respected[9]. However, one study involving cancer patients in the ICU demonstrated that the presence of an advance directive did not alter decision-making regarding life-supporting interventions[15]. This alone is concerning; however, this issue becomes more complex when it is considered that most advance directives typically do not directly address acute dialysis in the setting of AKI. Nephrologists are often left without a guide for advance directives to determine the continuity of care in this specific setting.
Cost is another factor, which must be considered in these patients. The SUPPORT trial helped to establish the cost-effectiveness of AKI treatment involving 490 patients[1]. This trial determined that overall cost of renal replacement therapy per quality-adjusted-life-year in AKI patients in the ICU was $128200 with $274100 for patients in worst prognostic group and $61900 for patients in the best prognostic group. However, it surpassed the cost-effective limit of $50000 per quality-adjusted-life-year[1]. In another study by Gopal et al[16], the outcomes of 85 survivors of multi-organ failure who required the use of renal replacement therapy in ICU found that the cost of each year of survival was $50000, and the majority of survivors felt that their treatment was worthwhile and their quality of life was satisfactory. With a high mortality rate of up to 90% for ICU patients with AKI[10], the ethical principle of justice and the equitable distribution of resources must be considered when treating these patients. In these situations, a palliative care consult would provide a more cost-effective treatment apart from better symptom management and a better quality of life.
AKI in ICU patients has a host of symptoms, including pain, pruritus, anorexia, sleep disturbances, fatigue, sexual dysfunction, and others[17]. The appropriateness of palliative care in AKI patients in the ICU will be judged based on the complications and prognosis. However, a study done by Aslakson et al[18] establishes the role of palliative care in the ICU and determined that “palliative care is increasingly accepted as an essential component of comprehensive care for critically ill patients, regardless of diagnosis or prognosis”. AKI in the ICU comes with a host of complications regarding treatment decisions. Among the most difficult decisions a physician must make is whether to withdraw dialysis from these patients. Due to difficulty in establishing the prognosis, this decision may not come lightly. Following is a list of recommendations and justifications for the palliative care in these critically ill AKI patients: (1) Palliative care is appropriate in patients with AKI in the ICU: Patients with AKI in the ICU are often appropriate for palliative care due to the multitudes of symptoms they can experience. These patients have historically not been provided this service due to multifactorial reasons. However, palliative care in these patients can help to alleviate problematic symptoms, improve quality of life, and decrease suffering. Palliative care physicians, with the teamwork of the patient’s nephrologist, are equipped with the appropriate training and knowledge to make determinations regarding the appropriateness of palliative care for individual patients. Depending on the clinical situation and the presence of risk factors for poor outcome, one of the three models of care is recommended; (2) Establish an advance directive with patients early on, with specific instructions regarding dialysis, and respect those advance directives[9]: This will help to establish patient wishes early on, and with the ethical respect of these wishes, a physician can make a sound clinical judgment regarding the withdrawal of dialysis as well as the establishment of palliative care in that patient; (3) Discontinuation of dialysis should occur in the situations outlined by the RPA/ASN guidelines[14]: The RPA/ASN guidelines help to establish evidence-based ethical considerations when making the clinical decision to withdraw dialysis. Clinicians can use these guidelines combined with informed consent to educate patients and patient advocates about the risks, benefits, outcomes, and prognosis for each patient’s condition.
AKI in the elderly population has been shown to be associated with significant morbidity and mortality[19]. Furthermore, dialysis is associated with poor outcomes, suffering, and limited life prolongation at the cost of dignity and quality of life in the elderly AKI patients admitted to ICU with multiple comorbidities[19]. Expectations of today’s society about the standard of care have lead to indisputable provisions of dialysis in this patient population necessitating the reevaluation of these approaches[19]. Although RPA/ASN guidelines are applicable in the acute care setting, there are few factors that may limit its use in AKI patients in the ICU[20]. Shared decision-making is often difficult given decisions are urgent and physicians have not known patients and their family members prior to ICU admission in most cases[20]. In contrast, shared decision making in chronic kidney disease patients progressing to ESRD is much easier due to the long-standing relationship between caregiver, patients and their family members[20]. Some clinical scenarios may challenge caregivers with ethical and legal issues as few patients and their relatives may demand initiating or continuing dialysis even after it is considered futile[2]. In such situations, informed decision-making plays a crucial role in proving the legality of withholding or withdrawing dialysis[2]. All the discussions and communications with the patient and his/her family members or surrogate decision makers should be properly documented at all the times during the entire course of management[2]. In addition, a multidisciplinary approach involving palliative care team, nephrologists, intensivists, and institutional ethics committee may help to settle conflicts between the caregivers, and the patient and family members[2].
AKI patients in the ICU have a host of symptoms and most often suitable for palliative care that can help relieve symptoms, improve quality of life and reduce suffering. The appropriateness of palliative care in this patient population is determined with the teamwork of the patient’s nephrologist and palliative care physician. Shared decision-making and advance directives play an important role in the management and guide the physician as to what patient wishes are, and those decisions should be respected. Either comprehensive or conceptualization model of palliative care is recommended for these patients.
Manuscript source: Unsolicited manuscript
Specialty type: Urology and Nephrology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Nechifor G, Trimarchi H, Yorioka N S- Editor: Wang XJ L- Editor: A E- Editor: Bian YN
| 1. | Hamel MB, Phillips RS, Davis RB, Desbiens N, Connors AF Jr, Teno JM, Wenger N, Lynn J, Wu AW, Fulkerson W, Tsevat J. Outcomes and cost-effectiveness of initiating dialysis and continuing aggressive care in seriously ill hospitalized adults. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. Ann Intern Med. 1997;127:195-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 134] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 2. | Jawed Y. Acute Kidney Injury in Critical Patients and the Role of Palliative Care,. Available from: URL: https://www.kidneynews.org/kidney-news/special-sections/acute-kidney-injury-in-critical-patients-and-the-role-of-palliative-care. |
| 3. | Kao CC, Yang JY, Chen L, Chao CT, Peng YS, Chiang CK, Huang JW, Hung KY. Factors associated with poor outcomes of continuous renal replacement therapy. PLoS One. 2017;12:e0177759. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 4. | Bagshaw SM, George C, Bellomo R; ANZICS Database Management Committee. Early acute kidney injury and sepsis: a multicentre evaluation. Crit Care. 2008;12:R47. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 405] [Cited by in RCA: 476] [Article Influence: 28.0] [Reference Citation Analysis (0)] |
| 5. | da Hora Passos R, Ramos JG, Mendonça EJ, Miranda EA, Dutra FR, Coelho MF, Pedroza AC, Correia LC, Batista PB, Macedo E. A clinical score to predict mortality in septic acute kidney injury patients requiring continuous renal replacement therapy: the HELENICC score. BMC Anesthesiol. 2017;17:21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 39] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 6. | Feudtner C. Collaborative communication in pediatric palliative care: a foundation for problem-solving and decision-making. Pediatr Clin North Am. 2007;54:583-607, ix. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 212] [Cited by in RCA: 162] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 7. | Lanken PN, Terry PB, Delisser HM, Fahy BF, Hansen-Flaschen J, Heffner JE, Levy M, Mularski RA, Osborne ML, Prendergast TJ. An official American Thoracic Society clinical policy statement: palliative care for patients with respiratory diseases and critical illnesses. Am J Respir Crit Care Med. 2008;177:912-927. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 506] [Cited by in RCA: 510] [Article Influence: 30.0] [Reference Citation Analysis (0)] |
| 8. | Hudson P. A conceptual model and key variables for guiding supportive interventions for family caregivers of people receiving palliative care. Palliat Support Care. 2003;1:353-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 68] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 9. | Patel SS, Holley JL. Withholding and withdrawing dialysis in the intensive care unit: benefits derived from consulting the renal physicians association/american society of nephrology clinical practice guideline, shared decision-making in the appropriate initiation of and withdrawal from dialysis. Clin J Am Soc Nephrol. 2008;3:587-593. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 10. | Metnitz PG, Krenn CG, Steltzer H, Lang T, Ploder J, Lenz K, Le Gall JR, Druml W. Effect of acute renal failure requiring renal replacement therapy on outcome in critically ill patients. Crit Care Med. 2002;30:2051-2058. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 629] [Cited by in RCA: 565] [Article Influence: 24.6] [Reference Citation Analysis (0)] |
| 11. | A controlled trial to improve care for seriously ill hospitalized patients. The study to understand prognoses and preferences for outcomes and risks of treatments (SUPPORT). The SUPPORT Principal Investigators. JAMA. 1995;274:1591-1598. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1959] [Cited by in RCA: 1797] [Article Influence: 59.9] [Reference Citation Analysis (0)] |
| 12. | Chertow GM, Christiansen CL, Cleary PD, Munro C, Lazarus JM. Prognostic stratification in critically ill patients with acute renal failure requiring dialysis. Arch Intern Med. 1995;155:1505-1511. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 252] [Cited by in RCA: 231] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 13. | Abosaif NY, Tolba YA, Heap M, Russell J, El Nahas AM. The outcome of acute renal failure in the intensive care unit according to RIFLE: model application, sensitivity, and predictability. Am J Kidney Dis. 2005;46:1038-1048. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 210] [Cited by in RCA: 179] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 14. | Galla JH. Clinical practice guideline on shared decision-making in the appropriate initiation of and withdrawal from dialysis. The Renal Physicians Association and the American Society of Nephrology. J Am Soc Nephrol. 2000;11:1340-1342. [PubMed] |
| 15. | Kish Wallace S, Martin CG, Shaw AD, Price KJ. Influence of an advance directive on the initiation of life support technology in critically ill cancer patients. Crit Care Med. 2001;29:2294-2298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 51] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 16. | Gopal I, Bhonagiri S, Ronco C, Bellomo R. Out of hospital outcome and quality of life in survivors of combined acute multiple organ and renal failure treated with continuous venovenous hemofiltration/hemodiafiltration. Intensive Care Med. 1997;23:766-772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 77] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 17. | Cohen LM, Moss AH, Weisbord SD, Germain MJ. Renal palliative care. J Palliat Med. 2006;9:977-992. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 70] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 18. | Aslakson RA, Curtis JR, Nelson JE. The changing role of palliative care in the ICU. Crit Care Med. 2014;42:2418-2428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 227] [Cited by in RCA: 214] [Article Influence: 19.5] [Reference Citation Analysis (0)] |
| 19. | Akbar S, Moss AH. The ethics of offering dialysis for AKI to the older patient: time to re-evaluate? Clin J Am Soc Nephrol. 2014;9:1652-1656. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 20. | Gabbay E, Meyer KB. Identifying critically ill patients with acute kidney injury for whom renal replacement therapy is inappropriate: an exercise in futility? NDT Plus. 2009;2:97-103. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |