Published online Jul 6, 2015. doi: 10.5527/wjn.v4.i3.396
Peer-review started: December 18, 2014
First decision: January 20, 2015
Revised: February 25, 2015
Accepted: April 10, 2015
Article in press: April 14, 2015
Published online: July 6, 2015
Processing time: 200 Days and 10.6 Hours
AIM: To analyze the clinical features, diagnostic modalities, and the surgical management of urethral complications after tension-free vaginal tape procedures.
METHODS: This study encompasses a retrospective review of nine patients presented with urethral complications after midurethral sling procedures. The patients underwent the procedures during a period from 1999 to 2012 in three different regional hospitals in the southwest part of Sweden. The time from sling placement to diagnosis, the risk factors, clinical features, diagnosis, surgical management, and functional outcome are presented. The presenting symptoms were described as either early onset (< 12 mo) or late onset (> 12 mo) according to when they were first reported.
RESULTS: Eight cases of urethral erosion and one case of bladder-neck erosion were detected. The mean interval for diagnoses of the erosions ranged from 3 mo to 11 years. The most common presenting symptoms included de novo urgency with or without incontinence (7/9 patients), urinary retention/voiding dysfunction (4/9 patients), urethritis (4/9 patients), relapse of stress-incontinence (3/9 patients), recurrent urinary tract infections (5/9 patients), and hematuria (1/9 patient). In most cases, voiding dysfunction and urethritis occurred early after the operation. The surgical management applied in most cases was transurethral resection of the intraurethral part of the mesh. The removal of the intraurethral mesh resulted in improvement or complete cure of urgency symptoms in 5/7 patients with urgency. Four patients were reoperated with a new stress-incontinence surgery, one with laparoscopic Burch, and three with retropubic tension-free vaginal tape procedures.
CONCLUSION: Urethral complications should be suspected in the case of de novo urgency and relapse of stress-incontinence. Transurethral excision of the intraurethral mesh is the recommended treatment.
Core tip: We present eight cases of urethral erosion and one of bladder neck erosion after tension-free vaginal tape procedures. The mean interval for complication diagnoses ranged from 3 mo to 11 years. The clinical profile of the complications included de novo urgency, voiding dysfunction, urethritis, relapse of stress incontinence, recurrent urinary tract infections, and hematuria. It is important to consider urethral complications in the postoperative follow-up if these symptoms occur. A control urethrocystoscopy is important for the diagnosis. The transurethral excision of the intraurethral part of the mesh is recommended as the treatment of choice.
- Citation: Sergouniotis F, Jarlshammar B, Larsson PG. Urethral complications after tension-free vaginal tape procedures: A surgical management case series. World J Nephrol 2015; 4(3): 396-405
- URL: https://www.wjgnet.com/2220-6124/full/v4/i3/396.htm
- DOI: https://dx.doi.org/10.5527/wjn.v4.i3.396
Stress urinary incontinence (SUI) is a significant and common problem in women. SUI is defined as an involuntary leakage of urine on effort, straining, or coughing[1]. Some of the potential causes of SUI include childbirth, older age, obesity, chronic bronchitis, and chronic constipation[2]. Although relatively mild, symptoms often have a negative effect on the patient quality of life in terms of physical and social well-being.
In 1996, Petros and Ulmsten introduced a new, minimally invasive sling procedure for the treatment of SUI. The new procedure applied a tension-free vaginal tape (TVT) under the mid-urethra. The midurethral sling reinforced the weakened pubourethral ligaments and recreated the “hammock” support of the lax anterior vaginal wall and endopelvic fascia[3-5]. The advantage of the TVT procedure is that it is minimally invasive and can be performed under local or regional anesthesia as outpatient surgery.
The TVT procedure has undergone numerous modifi-cations and improvements since its initial introduction. In 2001, De lorme et al[6] described a surgical approach where the polypropylene suburethral sling was placed between the two obturator foramina. The goal was to maintain the same position of the sling under the mid-urethra while reducing the risk of complications associated with the blind passage in the retropubic space, such as bladder, bowel, and iliac vessel injury. The procedure is an “outside-in” technique. The technique involves a blind percutaneous introduction of a curved trocar lateral to the vagina, around the inferior ischiopubic ramus, through the obturator foramen and into the anterior vaginal wall at the midurethral level.
A later modification of the Delorme technique was described by de Leval[7] in 2003. De Leval designed a trans-obturator inside-out procedure (TVT-O), a technically more convenient method than the outside-in technique. The surgeon does not need to use an index finger to guide the needle coming from the outside. Furthermore, a “wing-guide” is used during the dissection of the paraurethral tunnel in order to protect the urinary tract[5].
In 2006, a third generation of midurethral slings was introduced with the development of single incision mini-slings. The new method applied a shorter polypropylene mesh with a single suburethral incision. Because the technique avoided the need for blind passage through the retropubic or obturator spaces, it aimed to reduce the complications and increase the safety of the procedure[8-11]. An additional benefit of the procedure was that it could also be performed under local anesthesia.
Since 1996 when it was first introduced, the TVT technique has become the gold standard of minimally invasive surgery in the treatment of stress incontinence. The efficacy of the TVT procedure has been comprehensively documented in the literature. However, TVT-associated complications and their management are less well understood[12-15].
Perioperative perforation of the bladder is a common complication associated with retropubic TVT sling procedures. In a Swedish study that evaluated the results of over 700 patients treated with TVT, the frequency rate of bladder perforations was 1.7%[16]. Urethral erosion of the mesh is a rare complication after a sling operation and may present with various symptoms. The complication occurs when the sling placed outside the urinary tract gradually erodes into the urethra[17]. The first described case of urethral erosion after a TVT operation was published in 2001[18]. Since then, there have been a limited number of reports and case series published on this unusual complication[12,19-26].
The objective of this study was to evaluate the clinical features, physical findings, and diagnostic procedures of postoperative urethral complications. Furthermore, the effectiveness of our management approach in controlling the condition, as well as the outcomes after treatment, were addressed.
Our first case of urethral complication was noted in 2006. We had examined a woman via urethrocystoscopy due to postoperative urinary tract discomfort, including dysuria and frequency and voiding dysfunctions. The urethrocystoscopy revealed an intraurethral section of the displaced mesh. Following the initial case, all women with dysuria, frequency and voiding dysfunctions, and de novo urgency after TVT-procedures underwent urethrocystoscopy.
Herein, we performed an analysis of women with urethral complications after synthetic midurethral sling procedures. The patients’ medical records were reviewed retrospectively. The time between sling placement to diagnosis, risk factors, presenting symptoms, diagnostic procedures, surgical management, and postoperative outcomes were recorded. A control urethrocystoscopy was performed on the patients with remaining symptoms.
Five different surgeons from three different regional hospitals in the southwest part of Sweden had performed the sling procedures over a 13-year period (1999-2012) in women diagnosed with intraurethral displaced tape. The presenting symptoms were described as either early onset (< 12 mo postoperatively) or late onset (> 12 mo postoperatively), based on when the symptoms were first reported.
The manufacturers’ standard recommendations were followed when placing the mesh, so that the mesh laid tension-free under the urethra. All the surgeons were very experienced and had performed more than 200 TVT procedures. Vaginal sonography was applied as part of the routine postoperative control.
In the period from 1999-2012, nine cases of intraurethrally displaced mesh after midurethral sling procedures were identified. In all nine cases, the mesh was surgically removed at our clinic.
A 46-year-old woman was operated upon with TVT-O for genuine SUI in May 2006. The patient was 2-para, had a hormone intrauterine device (IUD; Mirena®) and a body mass index (BMI) of 23.0. The patient also had a medical history of chronic cough, appendectomy, and her mother was operated on with Burch-plastic. During the procedure, the band was doubled with an Allis clamp in a little loop in order to avoid tension of the sling.
Postoperatively, the patient developed urinary retention and had to use intermittent catheterization. The patient complained of pain in the urethra and was treated for urinary tract infection (UTI). An urethrocystoscopy performed 19 d after the surgery showed swelling over the bladder neck; hence, a suprapubic catheter was applied. Two weeks later, the patient had spontaneous voiding, and the suprapubic catheter was removed.
Five months after the surgery, the patient complained of de novo urgency, voiding dysfunction, urethral pain, and dyspareunia. An urethrocystoscopy showed an erosion of the sling directly across the urethra. A second surgery, 5.5 mo after the primary TVT operation, was performed using a transvaginal urethroplasty, and the tape was removed to restore the urethra. A suprapubic catheter was applied for three weeks.
At the three-month short-term follow-up, the patient had improved voiding, no urgency, fewer frequency symptoms, and little vaginal pain. Over the long-term, the patient had a relapse of SUI and de novo urge incontinence. The former was first treated with two paraurethral silicon injections and then with laparoscopic Burch colposuspension. The latter was treated with anticholinergics.
A 55-year-old postmenopausal woman underwent a TVT-O for mixed incontinence. The patient was 2-para, obese with a BMI of 40.7, and on medication for hypertension and type II diabetes. The TVT-O procedure was performed without complications. Perioperatively, it was noticed that she had a short urethra. The mesh was placed approximately 1 cm from meatus.
During the first postoperative month, the patient experienced worsening of her urgency symptoms, together with urethral pain. The patient was treated with antibiotics for urethritis and had two urethrocystoscopy procedures without any signs of erosion. Due to voiding difficulties, the patient received urethral dilatations with a slight reduction in her symptoms, and she was scheduled for further dilatations. After urethrocystoscopy, 3 mo postoperatively, it was noticed that the patient had urethral erosion.
The patient was reoperated upon 3 mo and 9 d after the sling application. The sling was cut outside the urethra, excised transurethrally, and the defect in the urethra was closed. A suprapubic catheter was applied for three weeks.
During the short-term follow-up, the patient developed a local vaginal infection and UTI; however, the urgency symptoms improved. Over the long-term follow-up, the patient had a worsening of her urgency and slight relapse of SUI. The patient was treated with anticholinergics for her urgency. During this time, the patient underwent an operation for disc herniation in the lower spine and had a gastric bypass. The patient was later offered polyacrylamide injection treatment for the stress component of her incontinence but felt that she needed no further operative treatment.
A 60-year-old woman, 3-para, with a normal BMI of 24.1, ulcerative colitis, and cardiac arrhythmia underwent a TVT-O in 2005 for genuine SUI with no complication. The cardiac arrhythmia was later treated with a pacemaker. The patient had voiding dysfunction shortly after the TVT-O operation and used intermittent catheters for 1 mo.
Twenty months after the TVT-O procedure, the patient developed de novo urge incontinence and local vaginal pain, and was prescribed antibiotics for her UTI. An urethrocystoscopy showed a small part of the mesh in the urethra. A new operation was performed two years postoperatively, with transurethral excision of the intraurethral part of the mesh. No urethroplasty was needed. A suprapubic catheter was placed for 10 d, and antibiotics were given for two weeks.
In the long-term follow-up, the patient had no urgency symptoms, no vaginal pain, and no SUI.
A 43-year-old woman, 2-para, with a normal BMI of 26.1 and no previous surgery, underwent a mini-sling TVT-Secur operation for genuine SUI in 2009. After the application of the sling, the perioperative urethrocystoscopy was normal.
A short time after the operation, the patient developed de novo urgency with leakage, urethral pain, local vaginal pain, and dyspareunia, but her SUI had been cured. An urethrocystoscopy was performed 2 mo postoperatively. The procedure showed a small erosion of two loops of the TVT mesh in the urethra at the 5 o’clock position. The patient was treated conservatively and received antibiotics for urethritis.
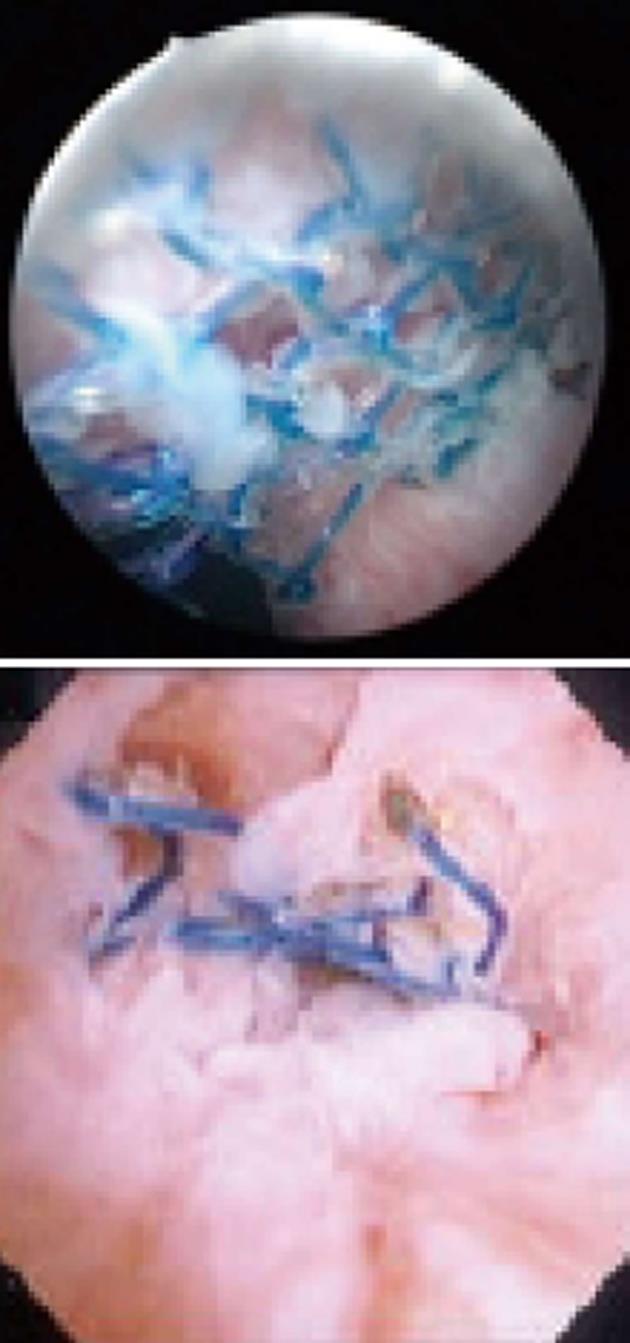
The mesh continued to erode into the urethra, and the next urethrocystoscopy, conducted 6 mo postoperatively, showed progression of the erosion and visible passing of the sling right through the urethra between the 3 o’clock and 9 o’clock positions. The patient was followed conservatively for 1.5 years, but the sling did not progress further through the urethra. A transurethral excision of the intraurethral part of the mesh was performed 20 mo postoperatively. The patient was then treated with antibiotics for 1 mo.
Three months after the operation the patient had no urethral pain, less dyspareunia and vaginal pain, and improved urgency symptoms. However, the patient’s SUI relapsed. Therefore, a TVT-retropubic procedure was performed two years after the first sling placement. This dissection was somewhat more difficult due to the presence of the scar tissue.
In the long-term follow-up, the patient had no stress incontinence, slight vaginal pain, and began anticholinergic treatment.
A 38-year-old woman underwent a retropubic TVT for genuine SUI in 1999. The patient was 5-para, with a BMI of 36.2, had been sterilized with a laparoscopic procedure, and then re-sterilized with a new laparoscopy because of an ectopic pregnancy. The TVT procedure was uncomplicated, but the patient did have a voiding dysfunction and irritative urinary symptoms after the operation. An urethrocystoscopy 3 mo postoperatively was normal.
In 2004, five years after the first operation, the patient had a relapse of her SUI, and a TVT-O operation was performed in 2005. No preoperative urethrocystoscopy was done at this procedure. With the exception of mild voiding problems, the patient was satisfied. The patient had also undergone a vaginal hysterectomy after the second sling procedure.
In 2010, the patient experienced a macroscopic hematuria. An urethrocystoscopy was performed 11 years and 1 mo after the first TVT. This procedure revealed a 1 cm horizontal erosion of the white TVTclassic mesh into the urethra. This tape used in 1999 was undyed, whereas the tape used in 2005 was dyed blue. A transurethral extirpation of the intraurethral part of the mesh was performed 12 years and 3 mo after the first TVT. The patient was treated with antibiotics for three weeks postoperatively.
In the long-term follow-up, the patient had no voiding problems, little urgency, and experienced improvement of her incontinence after all procedures.
In 2011, a 47-year-old woman was operated upon with the MiniArcTM single-incision sling system for genuine SUI. The patient was 4-para, obese with a BMI of 35.3, had asthma, fibromyalgia, and irritable bowel syndrome. She was previously sterilized laparoscopically. The preoperative cystoscopy was normal, and the MiniArcTM procedure was uncomplicated. Postoperatively, the patient had voiding difficulties and did not experience any improvement in her incontinence.
In a follow-up, 8 mo after the operation, the patient had a worsening of her SUI and was treated with antibiotics because of a UTI. The urethrocystoscopy showed that the mesh had eroded 0.5 cm into the urethra. A reoperation was performed 10 mo after placement of the sling. Transurethrally, the intraurethral mesh was cut on both sides, a catheter was placed, and local antibiotics were applied in the urethra. The patient was treated with oral antibiotics postoperatively.
At the three-month follow-up, the patient had unchanged SUI and recurrent UTIs. However, the urethrocystoscopy was normal. The patient later had a successful retropubic TVT. The postoperative follow-up was uncomplicated with the exception of a UTI.
A 44-year-old woman was operated upon with retropubic TVT for genuine SUI in 2002. The patient was 3-para, had a BMI of 29.7, and an appendectomy in her medical history. There were no preoperative complications. In the long-term, the patient complained of recurrent UTIs, de novo urgency without incontinence, nocturia, and minor voiding dysfunctions. An urethrocystoscopy, nine years after the primary operation, showed one part of the mesh eroded into the urethra at the right side near the bladder neck.
A reoperation was conducted 1 mo later, and the intraurethral mesh was cut and removed. The excision was performed transurethrally, and urethroplasty was not needed. Antibiotics were given for prophylaxis.
Three months after the reoperation, the patient had a slight relapse of her SUI. The urgency symptoms and voiding problems did improve, and the patient no longer had the nocturia. The urethrocystoscopy was normal at 3 mo. However, a year later during the follow-up urethrocystoscopy, a small section of threads from the mesh was noticed at the 3 o’clock position. As the patient was symptom free, it was handled conservatively, and an urethrocystoscopy was planned for the following year.
A 40-year-old woman underwent a retropubic TVT for genuine SUI in 2004. The patient was 1-para, healthy, and had a BMI of 21.3. There were no perioperative complications, and the patient was asymptomatic for 6.5 years. She had also undergone an abdominal salpingo-oophorectomy and total hysterectomy due to a large ovarian cyst. Five days later, the patient was reoperated upon because of an adherent ileus of the small intestine.
Seven years and 8 mo after the sling placement, the patient had an examination due to a relapse of her SUI and minor de novo urgency. An urethrocystoscopy showed erosion of the tape into the urethra. A transurethral procedure was performed seven years and 9 mo postoperatively. Local antibiotics were applied in the urethra along with systemic antibiotic prophylaxis.
In the follow-up 5 mo later, the symptoms of SUI with minor urgency remained. The urethrocystoscopy was normal, and there was a slight detrusor contraction while filling the bladder. However, there was no need for anticholinergics. The patient was operated upon with a new retropubic TVT, and at the one-year follow-up she had no SUI or urgency.
A 66-year-old woman, 2-para, with a BMI of 26.0, and a medical history of hypertension and gastritis underwent a TVT-retropubic procedure for SUI in 2010. She was operated upon at a perimenopausal age for an abdominal hysterectomy because of a fast-growing, but benign myoma. The patient had also previously undergone a vaginal operation for pelvic organ prolapse in the form of a rectocele and enterocele.
The patient developed SUI after her pelvic organ prolapse operation. Therefore, the previously mentioned TVT retropubic procedure was performed in 2010. The mesh was doubled with Allis forceps, and no leakage was observed. The perioperative urethrocystoscopy was normal.
Five months after the operation, the patient was examined for severe urgency symptoms. However, her SUI had been cured. The urethrocystoscopy showed that the mesh had eroded to the left side of the bladder neck.
A reoperation was performed 8 mo after the TVT procedure. The mesh had eroded from the bladder neck into the bladder making it difficult to cut the mesh transurethrally. Using a suprapubic trocar (laparoscopic trocar) from the abdomen to the bladder, the mesh was excised using laparoscopic scissors under the guidance of a cystoscope. The patient had a suprapubic catheter for 1 d and bladder catheter for 2 d. Antibiotics were given for one week.
In the long-term, the patient had an improvement in her urgency and no incontinence symptoms. An urethrocystoscopy performed 5 mo postoperatively was normal.
The patient had to undergo later a laparoscopic lysis of pelvic adhesions due to a chronic dyspareunia. These adhesions were caused by the previous hysterectomy.
Pertinent patient characteristics are presented in Table 1. The mean patient age at the primary operation was 48.9 years (range: 38-66 years). Six of the patients were premenopausal, and three were postmenopausal. The median BMI was 29.2 (range: 21.3-40.7), and three patients had a BMI > 30. Only one patient had a medical history of a pelvic organ prolapse operation before the primary incontinence procedure. Two patients had medical records of chronic asthma, and three patients had physically demanding work. Four of the patients had undergone other surgical procedures after the primary TVT operation. There were no obvious common predisposing factors for urethral erosion.
| Case | Age (yr) | Parity | BMI | Menopause | Previous operations | Postoperative medical history | Primary operation |
| Case 1 | 46 | 2 | 23.0 | Hormone IUD (Mirena®) | Appendectomy | No | TVT-O, Gynecare® |
| Case 2 | 55 | 2 | 40.7 | Yes | No | Gastric by-pass | TVT-O, Gynecare® |
| Case 3 | 60 | 3 | 24.1 | Yes | No | Pacemaker | TVT-O, Gynecare® |
| Case 4 | 43 | 2 | 26.1 | No | No | No | TVT-Secure, Gynecare® |
| Case 5 | 38 | 5 | 36.2 | No | Laparoscopic sterilization, Re-sterilization because of ectopic pregnancy | Hysteroscopy, vaginal hysterectomy | TVT-retropubic, Gynecare® |
| Case 6 | 48 | 4 | 35.3 | No | Laparoscopic sterilization | No | MinArcTM, AMS® |
| Case 7 | 44 | 3 | 29.7 | No | Appendectomy | No | TVT-retropubic, Gynecare® |
| Case 8 | 40 | 1 | 21.3 | No | No | Abdominal total hysterectomy and bilateral salpingo-oophorectomy for ovarian mass, re-laparotomy because of ileus | TVT-retropubic, Gynecare® |
| Case 9 | 66 | 2 | 26.0 | Yes | Abdominal hysterectomy, pelvic organ prolapse procedure | Laparoscopic operation of adhesions | TVT-retropubic, Gynecare® |
Eight of the patients were operated upon for genuine SUI and one for mixed incontinence. The type of primary operation varied from TVT-retropubic to TVT-obturator and mini-slings (Table 1). Therefore, no obvious correlations with the types of operations were found. We do not have data on the number of different TVT operations performed since 1999 in the three hospitals. Therefore, the frequency of the urethral erosion by the mesh cannot be calculated.
In two cases, the sling was doubled preoperatively to make the sling tension-free. Finally, postoperatively, four of the nine patients used intermittent catheterization because of voiding difficulties.
Eight of the presented cases had urethral erosions, and one had erosion of the mesh in the bladder neck. The mean interval for diagnosing the erosions was 42 mo (range: 3-133 mo). Four patients were diagnosed within the first year after the operation and five later, up to 11 years after the primary procedure (Table 2). The presenting symptoms were divided into an early-onset (< 12 mo postoperatively) and late-onset (> 12 mo) group according to when they were first reported. It is not clear if all symptoms were directly related to the described complications, but they might be a useful indicator of suspected erosion. Seven patients had clear clinical symptoms less than 12 mo after their operation. The list of early-onset symptoms for each patient is listed in Table 2. Four patients had new symptoms reported after 12 mo postoperatively.
| Case | Interval for diagnosis | Early-onsetsymptoms(< 12 mo) | Late-onset symptoms(> 12 mo) | Interval forsurgicalmanagement | Outcome aftersurgicalmanagement | Further treatment |
| Case 1 | 5 mo | Urinary retention/voiding dysfunction, UTI, urethral pain (urethritis), de novo urgency, dyspareunia | _ | 5 mo | Improved urgency, voiding dysfunction resolved, relapse of SUI | Anticholinergic, incontinence pad, electric stimulation, two macroplasty procedures, laparoscopic Burch |
| Case 2 | 3 mo | Urethral pain (urethritis), worsening of urgency | _ | 3 mo | Worsening of urge incontinence, relapse of SUI, recurrent urethritis | Anticholinergic, local antibiotics into the urethra, no further SUI treatments |
| Case 3 | 1 yr 8 mo | Urinary retention/voiding dysfunction | De novo urgency, recurrent UTI, vaginal pain | 1 yr 11 mo | Urgency resolved, vaginal pain resolved | No further SUI treatments |
| Case 4 | 2 mo | De novo urgency, urethral pain (urethritis), vaginal pain, dyspareunia | _ | 1 yr 8 mo | Improved urgency, urethral pain resolved, relapse of SUI | Anticholinergic, retropubic TVT |
| Case 5 | 11 yr 1 mo | Urinary retention/voiding dysfunction, UTI, voiding pain (urethritis) | Relapse of SUI, hematuria after TVT-O | 12 yr 2 mo | Recurrent minor SUI (patient already had second incontinence operation), improved urgency, urethral pain, voiding dysfunction resolved | No further SUI treatments |
| Case 6 | 8 mo | Urinary retention/voiding dysfunction, direct relapse of SUI, UTI | _ | 10 mo | Same as before the surgical management | Retropubic TVT |
| Case 7 | 9 yr 1 mo | _ | Recurrent UTI, de novo urgency, nocturia | 9 yr 2 mo | Slight relapse of SUI, improved urgency and voiding dysfunction | Local estrogens, no further SUI treatments |
| Case 8 | 7 yr 8 mo | _ | Relapse of SUI, minor de novo urgency, nocturia | 7 yr 9 mo | Same as before surgical management | Retropubic TVT |
| Case 9 | 4 mo | De novo urgency | _ | 7 mo | Improved urgency, cured SUI, no relapse after the surgical management | No further SUI treatments |
Overall, the majority of patients (77.7%) had some grade of de novo urgency with or without urge incontinence and recurrent UTIs (55.5%). The most common early-onset symptoms included urinary retention and voiding dysfunctions, urethritis, and vaginal pain. The late-onset symptoms were more often recurrent UTIs and recurrence of SUI.
The median interval between the diagnosis and surgical treatment was 1.5 mo (range: 10 d to 3 mo) for seven cases of urethral erosion. There were two cases with an interval of 13 mo and 18 mo, which were first treated conservatively.
The first case required transvaginal excision of the intraurethral mesh followed by transvaginal urethroplasty. This was a rather complicated and time-consuming operation, which led us to change our approach to transurethral resection of the intraurethral part of the mesh.
The best position for identifying and removing the intraurethral mesh was to have the patient in the lithotomy position under general or regional anesthesia. Using a regular cystoscope [Karl Storz Gmbh, Tuttlingen, Germany; Charrière (Ch) 22, 0° or 30° optics, with a deflecting mechanism with Albarran lever, and a working channel with two ports] the intraurethral mesh was identified (Figure 1), and a 5 Ch “open-end” ureteral catheter was inserted into the urethra. A 0-0 monofilament thread was then introduced through a loop in the central part of the mesh, and a good portion of the thread was pushed through the mesh into the bladder. Then, the cystoscope was retracted, and the thread position in the urethra was secured by grasping it at the meatus. The ureteral catheter was removed from the cystoscope, which was reintroduced into the bladder, and the distal part of the thread was located and grasped with cystoscopic pincers and extracted through the urethra. This created a thread loop through the mesh allowing the application of tension on the mesh while cutting.
To avoid cutting the loop by mistake, it is recommended to use a monofilament thread that is a different color than the mesh. It can be technically challenging to insert the monofilament thread into one of the loops of the TVT mesh. The procedure is easier when using a child cystoscope (Ch 10, one port channel, with an optic of 0°). The small cystoscope is more easily handled in the urethra and does not require a ureteral catheter to pass the monofilament thread through the instrument and the mesh. After placing the thread, the procedure is continued as described above with a normal cystoscope. From our experience, the monofilament thread of 0-0 size is the most convenient to use.
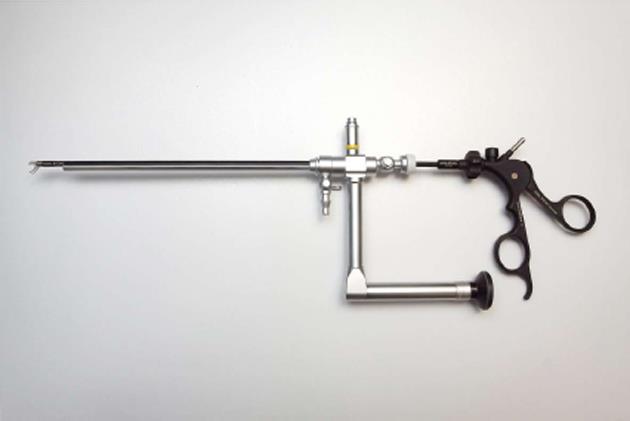
The next step was to carefully dilate the urethra to Hegar pin number 10. A nephroscope (Storz S27092 AMA, 0° optic and an operating sheath 27093BN, Ch 28 with a working channel of 5 mm) (Figure 2) has been the most convenient instrument to use when cutting the mesh. The regular cystoscope was not the best choice, as the small scissors used through a cystoscope were too weak to cut the mesh and easily broke. With a video technique, it was possible for the assistant to manipulate the urethra with one finger in the vagina. Through the working channel of the nephroscope, laparoscopic scissors (Storz, Metzenbaum scissor 5 mm, 34210 MW or Hak scissor, 34210 EH) were used to cut the mesh. It was easy to cut the mesh at the first side, and with the monofilament suture, it was possible to keep the mesh tensioned while cutting the other side. Cutting of the mesh at the mucosal level did not require suturing.
As much as possible of the visible mesh should be cut. If some small part remains, it will probably disappear. Only one case had small remains of the mesh at the control cystoscopy performed a couple of months after surgery. This patient will be followed-up with a new urethrocystoscopy after one year.
Preoperative antibiotics and intraurethral antibiotics were given as prophylaxis. Additionally, we have postoperatively left a suprapubic catheter in place for 7 d. During this time, oral antibiotics were given.
Under the ideal circumstances, the procedure took 30 min or less.
Four patients had relapses of their SUI after the intraurethral mesh was removed (Table 2). For five patients, no further SUI treatment was necessary after the removal of the intraurethral tape. Five out of seven patients patients with urgency experienced improvements or cures of their symptoms after the removal of the intraurethral mesh. Only three out of seven patients with de novo urgency were in need of anticholinergics after the last follow-up. Three patients also experienced improvements or cures of their voiding difficulties.
The exact pathophysiology behind erosion of the sling materials is not fully understood[3,17]. Various factors may predispose a patient to erosion. Factors associated with the pelvic anatomy include urogenital atrophy, poorly estrogenized tissue, previous pelvic radiation, previous vaginal surgery, or concomitant procedure and local infection, as well as a high body weight[13,17,27,28]. Our series had only one patient with a previous pelvic procedure, so these risk factors could not be verified.
Predisposing factors associated with the surgical technique include excessive tensioning of the sling and placement of the mesh too close to the urethra, which is the most feasible explanation, but it is not possible to extract this information from the medical records. When operating with mini-slings, it has been suggested to put the sling closer to the urethra than with traditional slings. This could explain our two cases of urethral complication after mini-sling procedures. Other possible explanations are inadequate vaginal tissue coverage and improper dissecting near the urethra, which might damage the urethral tissue and its vascularity[3,13,17,27]. Two of our cases had the sling doubled under the urethra perioperatively to ensure a tension-free application of the mesh. Four of our cases suffered from tight placement of the sling under the urethra; two patients had to use intermittent catheterization and two experienced voiding difficulties postoperatively.
The surgical manuals on retropubic TVT procedures recommend a rigid catheter guide inserted into the indwelling catheter for contralateral displacement of the bladder to minimize the risk of perforation. The urethra is then pulled towards the TVT needle, potentially increasing the risk of perforating the edge of the urethra. This might explain cases of urethral perforations and erosions in retropubic TVTs, but not in the other methods, as there was no displacement of the urethra during the operation.
More than one million TVT procedures have been performed worldwide since 1996 when the method was introduced[3,19]. In Sweden, about 4000-5000 women are operated on annually for SUI, most of whom receive the retropubic technique[16].
Urethral complications might be more common than reported, but that does not mean that the TVT procedures should be restricted. Urethral injury is still a rare complication, while the TVT procedures have a high success rate and a great improvement in the quality of life of the operated patients.
Urethral erosion may present with various symptoms. These include postoperative urinary retention, voiding dysfunction, hematuria, urethral or pelvic pain, recurrent UTIs, relapse of SUI, and de novo urgency[15].
There are only sporadic case reports referring to the clinical profile of erosions after sling procedures. As it seems in our study, the clinical profile of urethral complications might vary depending on the early or late onset of the symptoms after the operation. In the early period, we should expect voiding difficulties and urethritis symptoms, whereas in the later stage, it is more common with the relapse of SUI. De novo urgency (with or without leakage) and recurrent UTIs are also common symptoms that might appear early or late in the postoperative process.
In a review of 376 women with adverse events after suburethral sling procedures, Petri et al[28] analyzed the most common complications. De novo urgency with or without leakage was presented in 54% of the cases, voiding dysfunction in 48%, vaginal erosion in 19%, and urethral and vaginal pain in 14%. A total of 17 (4.5%) cases of urethral and bladder base perforation were found in their study, and most often the complications had occurred peroperatively. However, urethral and bladder base perforations might be associated with severe morbidity, and even lead to urethravaginal fistulae if undetected. Our study describes similar clinical symptoms secondary to urethral erosions.
A majority (77.7%) of our cases had de novo urgency. Postoperative de novo urgency has been reported in 10% of TVT procedures. If urethrocystoscopy is implemented postoperatively, the number of undiagnosed urethral erosions could considerably be reduced.
There has been a variety of approaches to the surgical management of urethral complications after sling procedures. The transvaginal excision of the intraurethral part of the sling with urethroplasty was the first approach to be used[18]. We used this method for our first case, but the transurethral excision of the mesh has become the preferred method for the majority of the patients in our series.
Another alternative is the conservative approach. In case 3, only one small loop of the mesh was seen in the urethra during the first cystoscopy. Cystoscopies were performed every 6 mo as a follow-up, and the mesh migrated directly across the urethra, but did not progress further after that.
We tried conservative treatment after receiving a report from colleagues who found a part of the mesh in the urethra but did not remove it. Therefore, we believe that urethral erosion might be a much common complication, at least in Sweden, where gynecologists perform TVT procedures, but do not routinely carry out urethrocystoscopy.
We also introduced preoperative urethrocystoscopy to all pubovaginal sling procedures. Including urethrocystoscopy in the preoperative investigation had many advantages. First, filling the bladder with 300 mL of saline solution without any detrusor contraction made cystometry unnecessary. Second, conducting a preoperative pad test with 300 mL in the bladder, with the patient exercising for 1 min and coughing ten times, would be much faster, if it is done at the same time as the urethrocystoscopy. Third, it would make urethrocystoscopy a standard and familiar procedure for the gynecologist.
Urethral complications after sling procedures might be more common than previously thought. One of the reasons is that the urethrocystoscopy is not included routinely in the postoperative follow-up of patients with residual or new symptoms from the urinary or vaginal tracts. This makes it difficult to identify complications because of the wide variation in the clinical profile and the timing of the presenting symptoms. It is important to suspect urethral complications if symptoms, such as urgency, voiding dysfunction, recurrent UTIs, or relapse of SUI occur after sling procedures.
We recommend the transurethral approach for the excision of the intraurethral mesh as the treatment of choice for urethral erosion.
We are grateful to all the patients who participated in the study.
Introduction of the tension-free vaginal tape (TVT) operations in 1996 to treat stress incontinence changed the surgical management of the condition. Instead of being an abdominal operation with one week of hospitalized postoperative care, TVT became a minimal invasive outpatient surgery, with same-day discharge. This meant many more women could be operated upon with this minimally invasive technique improving the patient’s quality of life tremendously. However, even the minimally invasive procedures have associated complications with a unique set of symptoms.
Mesh erosions are very serious complications, especially in prolapse surgery, with a high patient morbidity rate. In TVT operations, very few complications have been reported, mostly referring to perforation of the bladder. Urethral complications have been reported very sporadically.
The authors have performed routine urethrocystoscopy on women with some voiding difficulties after a TVT operation. Nine cases of urethral mesh erosions were identified. The initially used method required removal of the tape with an intravaginal approach, a rather long and complicated operation. The authors made a necessary modification with an intraurethral removal of the tape using a nephroscope. This device is normally used in kidney operations and not in vaginal procedures.
As much as 10% of reported cases of de novo urgency occur after a TVT operation. Many of these women might have urethral erosion that can be easily operated upon, if identified during urethrocystoscopy.
Stress incontinence is leakage of urine during coughing, laughing, and running. Urge incontinence is leakage after a strong feeling of need to void. De novo urge is a symptom of urgency that develops after the stress incontinence procedure. TVT procedures are minimally invasive operations with placing of a small tape under the urethra. Cystoscopy is a diagnostic procedure where a small instrument with a camera is introduced into the bladder and identifies the inside. Urethrocystoscopy is the same procedure that also includes examining of the urethra. It is not always performed during a routine cystoscopy.
This article is very interesting for individuals involved in the treatment of stress incontinence. Authors present their experience in the treatment of urethral erosion after tension-free vaginal tape procedures. The diagnostic and therapeutic approach is clearly explained. Also, an unusual and rare but very interesting operation of transurethral excision of the intraurethral part of the mesh was performed.
P- Reviewer: Friedman EA, Markic D, Taheri S, Trkulja V S- Editor: Ma YJ L- Editor: A E- Editor: Yan JL
| 1. | Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, van Kerrebroeck P, Victor A, Wein A. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Am J Obstet Gynecol. 2002;187:116-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 737] [Cited by in RCA: 749] [Article Influence: 32.6] [Reference Citation Analysis (0)] |
| 2. | Altman D, Falconer C, Zetterstro?m , J . Urogynekologi. Lund: Studentlitteratur. Print 2010; . |
| 3. | Brophy MM, Klutke JJ, Klutke CG. A review of the tension-free vaginal tape procedure: outcomes, complications, and theories. Curr Urol Rep. 2001;2:364-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Ulmsten U, Henriksson L, Johnson P, Varhos G. An ambulatory surgical procedure under local anesthesia for treatment of female urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 1996;7:81-85; discussion 85-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1252] [Cited by in RCA: 1160] [Article Influence: 40.0] [Reference Citation Analysis (0)] |
| 5. | Long CY, Hsu CS, Wu MP, Liu CM, Wang TN, Tsai EM. Comparison of tension-free vaginal tape and transobturator tape procedure for the treatment of stress urinary incontinence. Curr Opin Obstet Gynecol. 2009;21:342-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 64] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 6. | Delorme E. [Transobturator urethral suspension: mini-invasive procedure in the treatment of stress urinary incontinence in women]. Prog Urol. 2001;11:1306-1313. [PubMed] |
| 7. | de Leval J. Novel surgical technique for the treatment of female stress urinary incontinence: transobturator vaginal tape inside-out. Eur Urol. 2003;44:724-730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 554] [Cited by in RCA: 518] [Article Influence: 24.7] [Reference Citation Analysis (0)] |
| 8. | Walsh CA. TVT-Secur mini-sling for stress urinary incontinence: a review of outcomes at 12 months. BJU Int. 2011;108:652-657. [PubMed] |
| 9. | Abdel-Fattah M, Ford JA, Lim CP, Madhuvrata P. Single-incision mini-slings versus standard midurethral slings in surgical management of female stress urinary incontinence: a meta-analysis of effectiveness and complications. Eur Urol. 2011;60:468-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 115] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 10. | Oliveira R, Silva C, Dinis P, Cruz F. Suburethral single incision slings in the treatment of female stress urinary incontinence: what is the evidence for using them in 2010? Arch Esp Urol. 2011;64:339-346. [PubMed] |
| 11. | Molden SM, Lucente VR. New minimally invasive slings: TVT Secur. Curr Urol Rep. 2008;9:358-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 44] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 12. | Morton HC, Hilton P. Urethral injury associated with minimally invasive mid-urethral sling procedures for the treatment of stress urinary incontinence: a case series and systematic literature search. BJOG. 2009;116:1120-1126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 29] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 13. | Siegel AL. Urethral necrosis and proximal urethro-vaginal fistula resulting from tension-free vaginal tape. Int Urogynecol J Pelvic Floor Dysfunct. 2006;17:661-664. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | Karram MM, Segal JL, Vassallo BJ, Kleeman SD. Complications and untoward effects of the tension-free vaginal tape procedure. Obstet Gynecol. 2003;101:929-932. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 132] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 15. | Deffieux X, Bonnet K, Chevalier N, Gervaise A, Frydman R, Fernandez H. [Urinary complications in sub-urethral sling procedures]. J Gynecol Obstet Biol Reprod (Paris). 2005;34:745-756. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 16. | Ankardal M, Heiwall B, Lausten-Thomsen N, Carnelid J, Milsom I. Short- and long-term results of the tension-free vaginal tape procedure in the treatment of female urinary incontinence. Acta Obstet Gynecol Scand. 2006;85:986-992. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 40] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 17. | Clemens JQ, DeLancey JO, Faerber GJ, Westney OL, Mcguire EJ. Urinary tract erosions after synthetic pubovaginal slings: diagnosis and management strategy. Urology. 2000;56:589-594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 113] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 18. | Koelbl H, Stoerer S, Seliger G, Wolters M. Transurethral penetration of a tension-free vaginal tape. BJOG. 2001;108:763-765. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | Deng DY, Rutman M, Raz S, Rodriguez LV. Presentation and management of major complications of midurethral slings: Are complications under-reported? Neurourol Urodyn. 2007;26:46-52. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 171] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 20. | Sweat SD, Itano NB, Clemens JQ, Bushman W, Gruenenfelder J, McGuire EJ, Lightner DJ. Polypropylene mesh tape for stress urinary incontinence: complications of urethral erosion and outlet obstruction. J Urol. 2002;168:144-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 70] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 21. | Baracat F, Mitre AI, Kanashiro H, Montellato NI. Endoscopic treatment of vesical and urethral perforations after tension-free vaginal tape (TVT) procedure for female stress urinary incontinence. Clinics (Sao Paulo). 2005;60:397-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 22. | McLennan MT. Transurethral resection of transvaginal tape. Int Urogynecol J Pelvic Floor Dysfunct. 2004;15:360-362. [PubMed] |
| 23. | Powers K, Lazarou G, Greston WM. Delayed urethral erosion after tension-free vaginal tape. Int Urogynecol J Pelvic Floor Dysfunct. 2006;17:422-425. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 24. | Velemir L, Amblard J, Jacquetin B, Fatton B. Urethral erosion after suburethral synthetic slings: risk factors, diagnosis, and functional outcome after surgical management. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19:999-1006. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 43] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 25. | Wijffels SA, Elzevier HW, Lycklama a Nijeholt AA. Transurethral mesh resection after urethral erosion of tension-free vaginal tape: report of three cases and review of literature. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20:261-263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 26. | Quiroz LH, Cundiff GW. Transurethral resection of tension-free vaginal tape under tactile traction. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20:873-875. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 27. | Daneshgari F, Kong W, Swartz M. Complications of mid urethral slings: important outcomes for future clinical trials. J Urol. 2008;180:1890-1897. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 194] [Cited by in RCA: 197] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 28. | Petri E, Ashok K. Complications of synthetic slings used in female stress urinary incontinence and applicability of the new IUGA-ICS classification. Eur J Obstet Gynecol Reprod Biol. 2012;165:347-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 1.4] [Reference Citation Analysis (0)] |