Published online Mar 25, 2025. doi: 10.5527/wjn.v14.i1.97373
Revised: September 17, 2024
Accepted: October 28, 2024
Published online: March 25, 2025
Processing time: 236 Days and 13.5 Hours
End-stage renal disease (ESRD) is associated with a multitude of physical, psychological, and social health challenges, including a profound impact on sexual and reproductive health. Among males with ESRD, erectile dysfunction (ED) is highly prevalent due to factors such as underlying comorbidities, including diabetes and hypertension, and the physiological effects of long-term dialysis. Kidney tran
To evaluate the benefits and potential harms of KTx compared to other forms of renal replacement therapy in improving EF in adult males with ESRD, assessed using the international index of EF (IIEF), to survey the prevalence of SexDys in this population, and to assess the correlation between various factors and SexDys through regression analysis.
A systematic search of PubMed, EMBASE, Cochrane Library, Scopus, ClinicalTrials.gov, and Google Scholar was conducted, following the PRISMA 2020 guidelines. Prospective and retrospective cohort studies, as well as cross-sectional studies assessing EF pre- and post-transplantation, were included. These studies used validated tools such as the IIEF to measure EF. Meta-analyses were per
A total of 2419 studies were identified, with 362 abstracts screened and 193 full-text articles reviewed. Ultimately, 11 studies were included for qualitative analysis and 7 for quantitative synthesis. The random effects model for SMD yielded a combined estimate of 0.43 (95%CI: -0.20-1.07), indicating a small but non-significant improvement in EF post-transplantation. The heterogeneity across studies was substantial (I² = 90%), reflecting significant variability in outcomes. Subgroup analysis showed greater improvements in EF among living-donor transplant recipients compared to those receiving organs from deceased donors. Despite this trend, the overall result for changes in EF was not statistically significant (P = 0.15). Additionally, the combined HR from the meta-analysis was 2.87 (95%CI: 1.76-4.69), suggesting that KTx significantly increases the likelihood of improved EF, though variability between studies persisted (I² = 63%).
While KTx offers some promise for improving EF in male ESRD patients, the overall evidence remains inconclusive due to high heterogeneity between studies and a lack of statistical significance in the combined results. Despite this, individual studies suggest that KTx may lead to significant improvements in EF for certain subgroups, parti
Core Tip: Kidney transplantation (KTx) may offer improvements in erectile function (EF) for males with end-stage renal disease, though the overall evidence is inconclusive. This systematic review and meta-analysis found a small, non-significant improvement in EF post-transplantation, with high variability between studies. Living-donor transplant recipients may experience greater EF benefits than deceased-donor recipients. While KTx has the potential to improve sexual function, adjunct therapies like phosphodiesterase type 5 inhibitors may be necessary for persistent erectile dysfunction. Future research should focus on larger, well-designed studies to clarify KTx’s impact on sexual health.
- Citation: Jain J, Singh M, Kumar S, Yadav OK, Shettar A, Navriya SC, Bhirud DP, Choudhary GR, Sandhu AS. Effect of kidney transplantation on sexual dysfunction in patients with end stage renal disease: A systematic review. World J Nephrol 2025; 14(1): 97373
- URL: https://www.wjgnet.com/2220-6124/full/v14/i1/97373.htm
- DOI: https://dx.doi.org/10.5527/wjn.v14.i1.97373
End-stage renal disease (ESRD) profoundly impacts the physical, mental, and social dimensions of a patient's health[1]. Individuals with ESRD who rely on dialysis or undergo kidney transplantation (KTx) experience a remarkable im
Sexual dysfunction (SexDys) is significantly more prevalent in CKD patients compared to those with other chronic illnesses, with this dysfunction primarily manifesting as a loss of sexual interest in both males and females. Erectile dysfunction (ED) is notably higher in males with ESRD, with multiple contributing factors[5]. However, a systematic review and meta-analysis of the available observational studies clearly illustrate the lack of investigation into this critical aspect of CKD patients' lives. There are particularly few studies on sexual function in women with CKD (only 306 patients from 2 studies identified by Navaneethan et al[6]) and nondialysis, nontransplant CKD patients (369 patients from 2 studies). Despite this gap in research, SexDys remains common in CKD patients: 75% of men on dialysis therapy suffer from ED, while 30%-80% of women with CKD report symptoms of SexDys.
This dysfunction often manifests as a loss of sexual interest in both males and females, with ED notably higher in males with ESRD. The high prevalence of ED in this population may be attributed to the underlying causes of CKD, such as diabetes or hypertension, and the direct effects of uremia, particularly on the nervous system. Additionally, psychogenic ED, driven by high levels of anxiety, depression, and poor body image associated with dialysis, plays a crucial role[7-9]. ED profoundly impacts the quality of life in CKD patients, and while the issue is widespread, it remains undervalued and often overlooked by healthcare professionals.
KTx offers potential improvements in sexual function for both men and women, as it corrects metabolic and endocrine imbalances, normalizes hormonal profiles, and enhances psychological well-being[8,10]. Studies suggest that women tend to experience more consistent improvements in sexual function post-transplant, but the results for men are mixed. While some men report improvements in erectile function (EF), 30%-50% still experience ED or altered ejaculatory function post-transplant. Factors such as comorbidities, changes in body image due to surgery, and the effects of immunosuppressive therapy may hinder sexual recovery. However, one key benefit of KTx is the increase in spare time due to freedom from hemodialysis (HD), which may contribute to better sexual function. Despite these potential benefits, SexDys persists for many post-transplant recipients, negatively impacting their well-being and life satisfaction[11,12]. While KTx can improve sexual function for some, the outcomes remain controversial, particularly in men, warranting fur
Multiple studies with large sample sizes have been conducted to explore the etiogenesis, pathophysiology, and prevalence of ED in ESRD, as well as the effect of KTx on SexDys. These studies include observational studies, rando
This study evaluated the effect of KTx compared to other forms of renal replacement therapy (RRT) for improving SexDys, specifically erectile function, in adult males with ESRD, as assessed by changes in the International Index of Erectile Function (IIEF)[5,13,14].
Inclusion criteria: (1) Population: Adult males with ESRD who have undergone successful KTx; (2) Study design: Prospective or retrospective cohort studies, as well as cross-sectional studies, assessing EF with validated tools pre- and post-transplantation; (3) Single-arm, multi-arm, or comparative studies; (4) Outcome measures: Studies using validated questionnaires to assess SexDys, specifically EF, using tools like the international index of EF (IIEF); (5) Language: Only studies published in English; and (6) Availability: Availability of full text for review.
Exclusion criteria: (1) Study design: Case series, case reports, narrative reviews, editorials, and letters to the editor, as well as meta-analyses and systematic reviews; (2) Population: Studies involving patients under 18 years old and studies on conditions other than ED (e.g., anatomical penis defects or other sexual disorders); (3) Outcome measures: Studies assessing SexDys using non-validated questionnaires or a dichotomous (yes/no) approach and studies measuring sexual function only pre- or post-operatively, without comparative results; and (5) Study redundancy: When multiple records with overlapping populations are identified, only the most recent study was included.
The study adheres to the PRISMA 2020 guidelines, the Methodological Expectations for Cochrane Intervention Reviews when conducting the review[15], and PRISMA 2020 for the reporting[16].
We conducted a systematic literature search in PubMed, EMBASE, Cochrane Library, Scopus, NML-ERMED, ClinicalTrials.gov, and Google Scholar. The preliminary search strategy was formulated using PubMed's advanced search builder[17].
Four authors (Jain J, Kumar S, Shettar A, and Yadav OK) were responsible for the literature search. During an initial face-to-face meeting, all authors agreed on conducting an independent preliminary database search to become familiar with relevant keywords and major subheadings. In a subsequent meeting, kidney transplantation (MeSH) and sexual dysfunction (MeSH) were identified as major headings for the initial search. Using these MeSH terms and the AND operator, an initial search was performed on PubMed. The results were exported as a citation manager file and shared among all authors. The studies were independently reviewed, and suggestions from Singh M, Navriya SC, Bhirud DP, Choudhary GR, Sandhu AS were communicated by Singh M to the team. After discussion, an alternative search strategy involving MeSH subheadings was developed and continuously refined until the final analysis. The final search strategy (Kidney Transplantation AND ["Sexual Dysfunction, Physiological/etiology"[MeSH] OR "Sexual Dysfunction, Physiological/pathology"[MeSH] OR "Sexual Dysfunction, Physiological/physiopathology"[MeSH] OR "Sexual Dysfunction, Physiological/therapy"[MeSH]) was executed on PubMed, and the results were independently reviewed by the four primary authors Jain J, Kumar S, Shettar A, Yadav OK. These searches were then replicated across all selected databases, with results exported as CSV files. The search included all databases from their inception until May 2024. Initial metadata were reviewed to remove duplicates, followed by abstract reviews based on the predefined inclusion and exclusion criteria. A snowball search was conducted to identify additional studies, and reference lists of eligible publications were examined for further relevant studies.
The screening process consisted of: (1) Initial screening: Titles were initially screened to exclude irrelevant articles; (2) Abstract screening: Relevant titles were further screened by abstracts alone. Full articles were reviewed if the abstracts did not show sufficient relevance; and (3) Consensus resolution: Disagreements regarding search results were resolved by consensus among the reviewers.
The inclusion criteria ensure the selection of studies that provide comprehensive data on self-reported EF, using validated tools, in patients undergoing transplants, while being inclusive of various study designs and without language restrictions. The exclusion criteria eliminate studies with insufficient or non-validated EF data, ensuring the reliability and robustness of the study's findings. By focusing on validated measurement tools and excluding less rigorous study designs and reports, the criteria aim to maintain high-quality evidence for the analysis.
All identified records were independently screened for eligibility by four authors (Jain J, Kumar S, Shettar A, and Yadav OK), with any disagreements resolved by consensus. Data were extracted into a predefined Microsoft Excel spreadsheet, capturing study characteristics, patient demographics, renal transplantation (RT) specifics, and sexual function outcomes. Cochrane Collaboration's recommended methods were followed for data extraction from full-text articles, summary tables, and figures. When the standard deviation for the mean change from baseline of the EF domain of the IEF-15 or IIEF-5 was not provided, it was calculated from the standard error, confidence interval (CI), or P value. If these were unavailable, the standard deviation was estimated using correlation coefficients from other included trials. For studies assessing EF at multiple pre- or post-operative time points, data closest to the RT assessment were retrieved. The quality of records was independently assessed by four investigators (Singh M, Navriya SC, Bhirud DP, and Choudhary GR), with discrepancies resolved by consensus. The risk of bias across studies was estimated through visual assessment of funnel plot asymmetry and the Egger's statistical test.
A total of 2419 studies were identified from various databases: 1880 from Google Scholar, 421 from PubMed, and 118 from Scopus. After removing duplicates, 2057 records were discarded. A total of 362 study abstracts were screened. Of these, 169 records were excluded based on the predetermined inclusion and exclusion criteria available in the abstract text. A total of 193 full-text articles were assessed for eligibility. Out of these, 182 studies were excluded due to the following reasons: 20 due to inappropriate population as per the inclusion and exclusion criteria. 72 due to lack of either pre- or post-KTx evaluation, 19 due to full text not being available, and 71 as they did not use the IIEF as an assessment tool.
Eleven studies were included in the qualitative synthesis[18-28] (Table 1), and 7 studies were included in the quantitative synthesis[18,18-22,24,25] (Table 2).
| Ref. | Country | Population | Tool for EF assessment | No. of participants | No. of living donor RTRs | Type of renal transplant anastomosis | Age ± SD | Months of dialysis before RT ± SD | Time point of EF assessment (months after RT) | No. of patients with smoking | No. of patients with hypertension | No. of patients with diabetes | Testosterone prior to RT (ng/dL) |
| Gontero et al[18] | Italy | Adult males on HD undergoing RT | EF domain of IIEF-15 | 22 | NA | End-to-side external iliac artery | 51 ± 10.5 | 11.5 ± 5.5 | 3 | NA | NA | NA | 410 ± 182 |
| Mirone et al[19] | Italy | Adult males on HD undergoing RT | EF domain of IIEF-15 | 78 | 0 | Internal or external iliac artery | NA | NA | 3 | NA | NA | NA | NA |
| Nanjappa et al[27] | India | Adult males on HD undergoing RT | IIEF-5 | NA | NA | NA | NA | NA | NA | 37 | 63 | NA | NA |
| Nassir[20] | Saudi Arabia | Adult males with sexual partners on HD or dialysis | EF domain of IIEF-15 | 25 | NA | NA | 49.2 ± 11.4 | 22 ± 18.8 | NA | NA | NA | NA | NA |
| Pourmand et al[21] | Iran | Adult males on HD undergoing RT | IIEF-5 | 64 | NA | Common iliac artery: 8 | 41.1 ± 8.7 | 41.8 ± 31.9 | NA | NA | NA | NA | NA |
| Pyrgidis et al[28] | Egypt | Hepatitis C virus+ adult males on dialysis | IIEF-5 | 64 | 0 | NA | 50.1 ± 6.1 | 12.8 ± 20.5 | NA | NA | NA | NA | 307 ± 94 |
| Teng et al[22] | China | Adult males on dialysis undergoing RT | EF domain of IIEF-15 | 24 | NA | Internal iliac artery | 44.7 ± 9.8 | NA | NA | NA | NA | NA | NA |
| Javid et al[23] | Iran | Sexually active adult males on MHD | NA | NA | Internal and external iliac artery | 43.24 ± 8.73 | 12 | ||||||
| Pan et al[24] | China | Adult males on maintenance hemodialysis undergoing Ktx who suffered from SARS-COV-2 infection | NA | NA | NA | 40.2 ± 9.7 | 32.5 ± 35.3 | 6 | |||||
| El hennawy et al[25] | Saudi Arabia | Adult males on maintenance hemodialysis undergoing Ktx | 68 | NA | NA | 48.96+/-12.9 | 12 | ||||||
| Mondal et al[26] | India | Adult males on maintenance hemodialysis undergoing Ktx | NA | NA | NA | 40.9 ± 9.9 | 13.6 ± 0.43 | ||||||
| Ref. | No. of patients with SexDys before Ktx | No. of patients with SexDys after Ktx | MEAN IIEF difference with 95%CI | Smoking | HTN | Diabetes | Testosterone prior Ktx | RR | Upper limit RR | Lower limit RR | Weight age for SexDys before and after transplant (565) | Weight age for mean IIEF difference | Pre-KTX IIEF | Post-KTX IIEF | |
| Gontero et al[18] | 65/87 | 42/87 | -4.4 (-6.67, -2.13) | 13 | 19 | 1 | 410 ± 182 | 419 ± 129 | 2.18 | 1.2 | 3.95 | 0.0389 | 0.035889 | 22.5 ± 7.09 | 18.09 ± 6.33 |
| Mirone et al[19] | 68/78 | 71/78 | 0.9 (-1.53, -.27) | 16 | 69 | 7 | NA | NA | 0.67 | 0.24 | 1.86 | 0.138 | 0.12724 | 42.46 | 39.97 |
| Nanjappa et al[27] | 12/16 | 7/16 | 8.00 (4.75, 11.25) | NA | NA | NA | NA | NA | 3.86 | 0.86 | 17.32 | 0.02831 | |||
| Nassir[20] | 96/127 | 71/127 | 1.8 (1.17, 2.43) | NA | NA | NA | 805 ± 170 | 942 ± 216 | 2.44 | 1.43 | 4.17 | 0.22477 | 0.207177 | 17.47 ± 4.3 | 19.26 ± 4.41 |
| Pourmand et al[21] | 5.6 (3.68, 7.52) | NA | NA | NA | NA | NA | NA | NA | Na | Na | 0.104405 | 13.59 | 19.16 | ||
| Pyrgidis et al[28] | 4.8 (3.22, 6.38) | NA | NA | NA | NA | NA | NA | NA | NA | Na | |||||
| Teng et al[22] | 21/24 | 11/24 | 7.3 (5.22, 9.38) | NA | NA | 0 | 307 ± 94 | 654 ± 314 | 8.27 | 1.94 | 35.34 | 0.04247 | 0.039152 | 12.46 ± 8.88 | 19.75 ± 5.93 |
| Javid et al[23] | NA | 72 | 32 | ||||||||||||
| Pan et al[24] | 191/230 | 142/230 | 2 ± 13.6 | NA | 167 | 3.04 | 1.96 | 4.69 | 0.407079 | 0.375204 | 19 ± 7.41 | 21 ± 6.21 | |||
| El hennawy et al[25] | 63/68 | 39/68 | 8.7 | 9.37 | 3.35 | 26.24 | 0.120354 | 0.11093 | 46.8 ± 12.9 | 55.5 ± 13 | |||||
| Mondal et al[26] | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
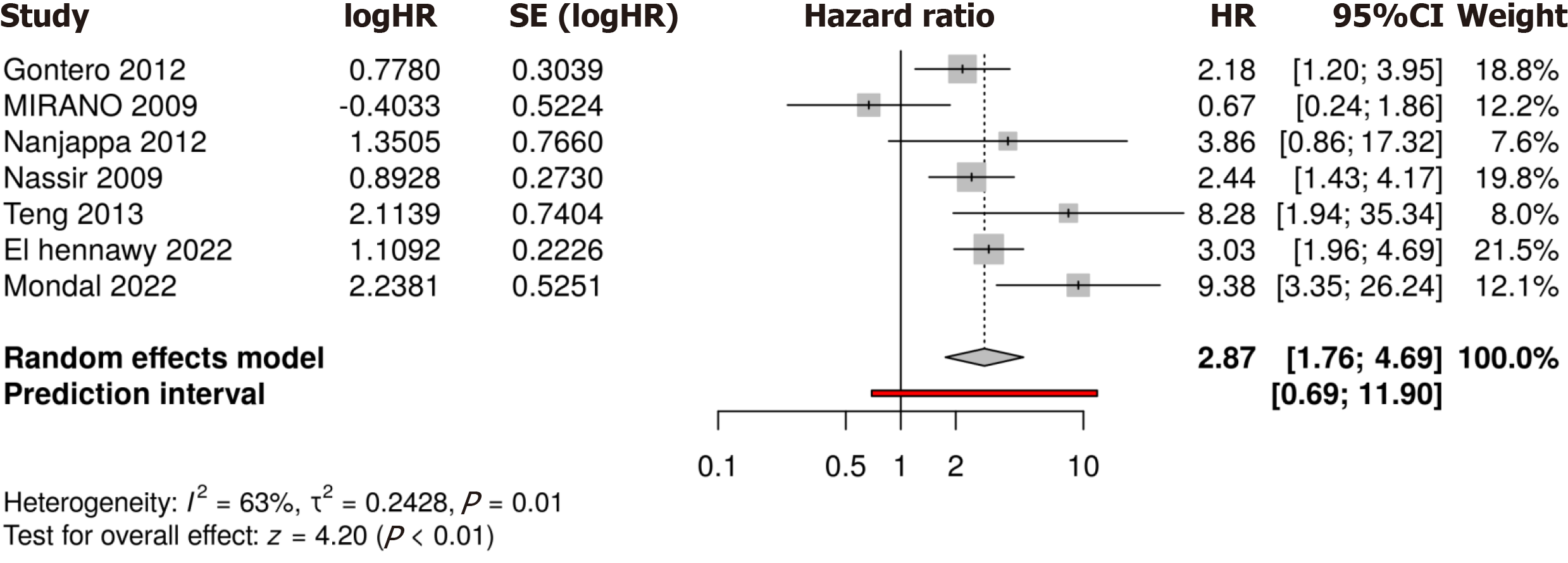
Study-specific results are elicited in Figure 1. Using a random effects model, the combined hazard ratio (HR) from all included studies was 2.87 (95%CI: 1.76-4.69), indicating that, on average, the hazard is almost tripled across the studies. This result is statistically significant, as the CI does not include 1 (Tables 1 and 2).
The I² statistic was 63%, indicating moderate heterogeneity between studies. This suggests that the results across the studies are not completely consistent, and there is some variability in the effects observed.
The τ² statistic was 0.2428, which quantifies the between-study variance in log HRs.
Cochran’s Q test for heterogeneity was significant (P = 0.01), reinforcing the presence of variability in the study outcomes.
The test for overall effect gave Z = 4.20 and a P value < 0.001, indicating that the overall result was highly statistically significant.
The prediction interval of [0.69, 11.90] provides insight into the expected range of effects in a new study. This wide interval suggests that while the overall effect is positive, in some cases (e.g., future studies), the effect might not be as large or could even be protective (HR < 1).
The results suggest a significant overall effect of the treatment or exposure on the hazard being studied, with the combined HR indicating a near tripling of the risk (HR = 2.87). However, there is notable variability across studies, as reflected by the I² statistic of 63%. While most studies indicate a positive hazard (increased risk), some studies, such as that by Mirone et al[19], show non-significant or even protective effects (HR < 1), contributing to the observed heterogeneity.
Given the moderate heterogeneity, the random effects model was appropriate for synthesizing the data, but the prediction interval suggests that future studies may exhibit varying results, ranging from a protective effect (HR < 1) to an extremely high risk (HR > 11). Therefore, while the overall conclusion is strong and statistically significant, caution is warranted when interpreting the generalizability of these findings across all contexts.
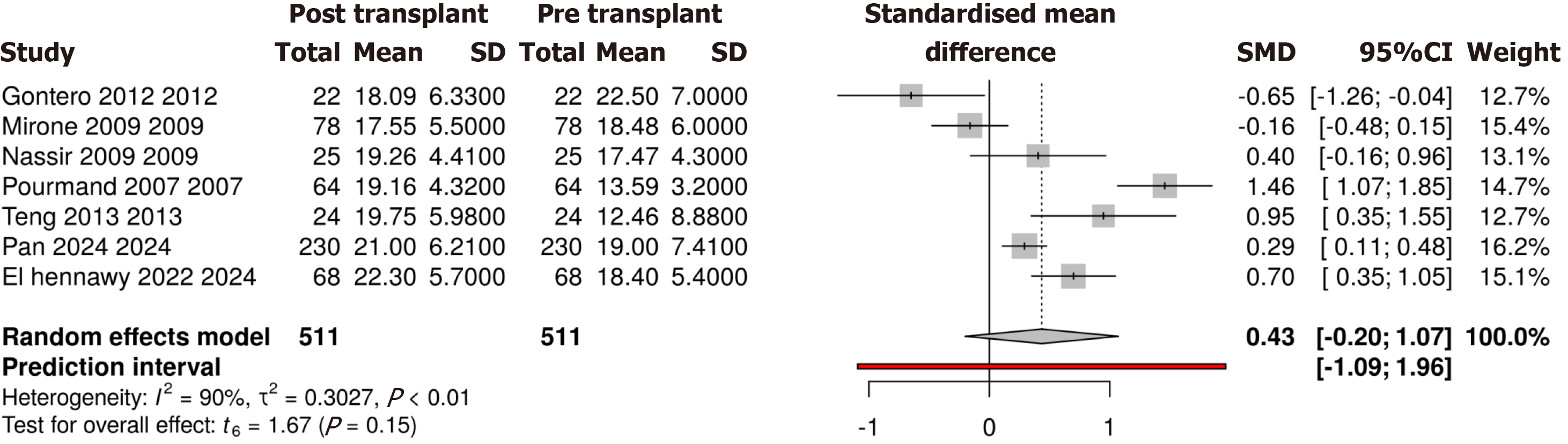
The random effects model yielded a standardized mean difference (SMD) of 0.43 (95%CI: -0.20-1.07). This suggests that the post-transplantation group shows a small overall improvement in the outcome of EF, but the CI crossing zero indicates that the result is not statistically significant. This means that while there appears to be a positive trend, we cannot conclusively say that the intervention (KTx) leads to a statistically significant improvement across all studies included in this analysis (Figure 2).
Test for overall effect: With t6 = 1.67 and a P value of 0.15, the overall effect was not statistically significant. This test further confirms that the combined result does not provide strong evidence that the post-transplantation outcomes are significantly different from pre-transplantation outcomes.
The forest plot summarized the results of several studies by comparing pre-transplant and post-transplant outcomes, using the SMD as the effect measure.
Random effects model: The combined SMD of 0.43 suggests a small positive effect overall, indicating a potential improvement in the outcome post-transplantation. However, due to the wide CI (-0.20-1.07), we cannot conclusively say that this improvement is statistically significant.
Weighting of studies: Studies like those by Pourmand et al[21] and Pan et al[24] have a greater weight (16.2% and 14.7%, respectively), meaning that they contributed more to the overall combined result due to their larger sample sizes or lower standard errors. Smaller studies like those by Gontero et al[18] and Teng et al[22] have smaller weights (12.7% each), contributing less to the overall effect.
The high heterogeneity (I² = 90%) suggests that the studies included in the meta-analysis are not consistent in their findings. This could be due to differences in patient populations, methods of assessing the outcome (e.g., different tools to measure EF), or differences in study design. High heterogeneity reduces confidence in the combined result, as it implies that the effect size varies widely between studies.
This meta-analysis of SMDs across multiple studies suggests a modest overall improvement in outcomes following KTx. However, the combined result (SMD = 0.43) is not statistically significant, and the wide prediction interval (-1.09-1.96) implies that future studies might observe a range of effects, from negative to highly positive. This lack of signifi
In summary, while some studies suggest positive effects of KTx on patient outcomes, the overall evidence is inconclusive due to the variability between studies and the lack of a statistically significant combined effect. Future research should aim to reduce heterogeneity by standardizing study designs and outcome measures, and efforts should be made to include all relevant studies to minimize publication bias.
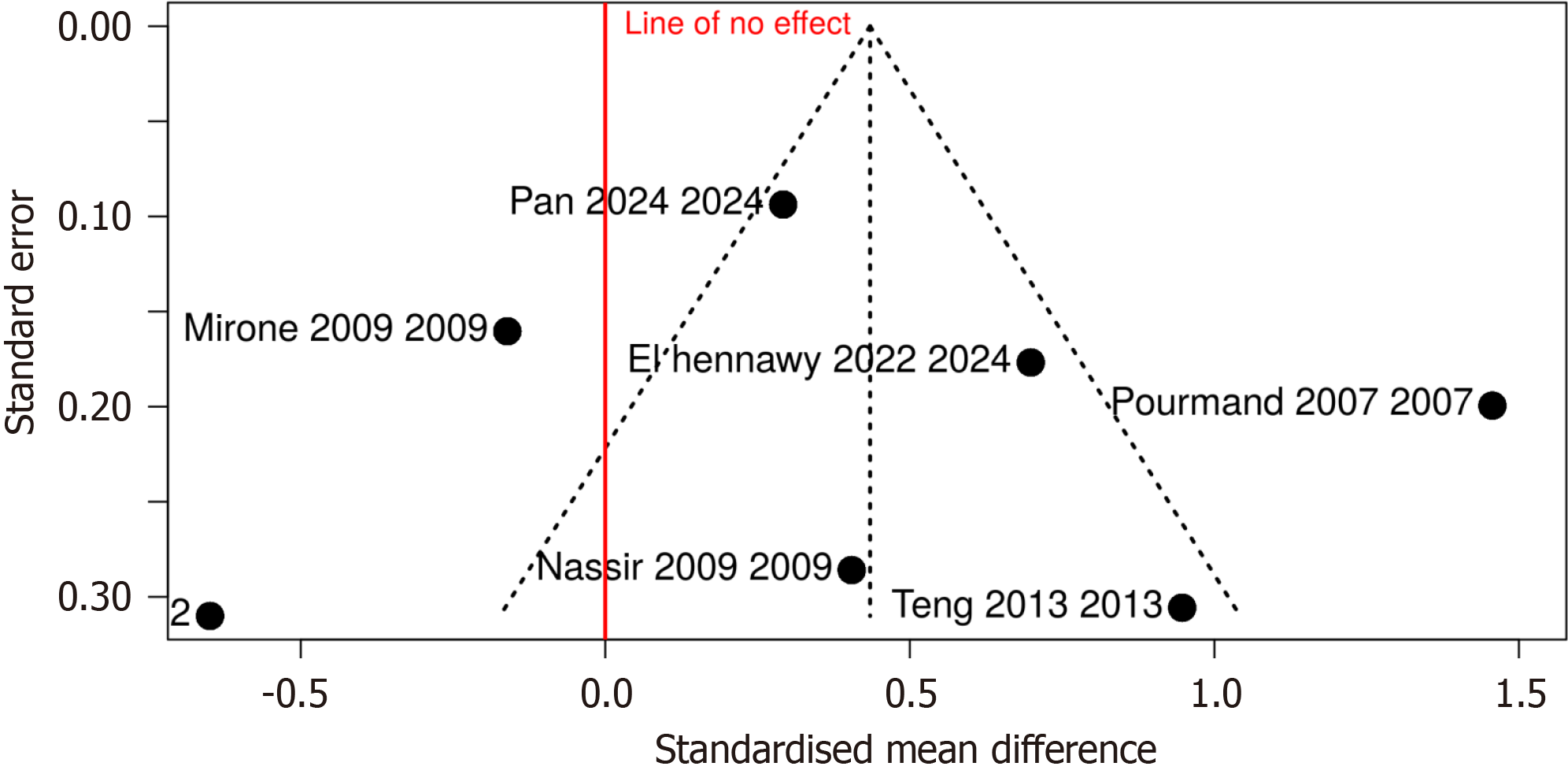
The funnel plot is a visual tool used to detect potential publication bias in meta-analyses, with the X-axis (SMD) representing the treatment effect or SMD for each study and Y-axis (standard error) representing the precision of each study; smaller studies with larger standard errors appear towards the bottom, while larger studies with smaller standard errors appear towards the top.
The plot (Figure 3) appears somewhat asymmetric, with more studies on the right-hand side of the funnel and fewer on the left, which might indicate potential publication bias. Typically, in the absence of bias, studies should be symmetrically distributed around the line of no effect (SMD = 0). Studies like those by Mirone et al[19] and Pan et al[24] appear on the far left, suggesting smaller or negative effects, while studies like those by Pourmand et al[21] and Teng et al[22] are on the far right, showing larger positive effects.
The red vertical line represents no effect (SMD = 0). Studies to the right show a positive effect, while those to the left indicate negative or non-significant effects. Studies clustered near the line of no effect indicate results close to an SMD of zero, meaning no significant difference between the compared groups.
The asymmetric nature of the plot suggests potential publication bias, as studies with larger positive effects (higher SMD) are more represented, especially on the right side. Small studies with null or negative results (potentially located on the left side) might be underreported or unpublished, leading to this asymmetry.
This systematic review and meta-analysis demonstrate that KTx has the potential to significantly improve EF in male patients with ESRD. Our findings align with previous studies, showing that the prevalence of ED decreases after RT. Specifically, patients who underwent KTx experienced a marked improvement in EF, as evidenced by increased scores in validated tools such as the IIEF-5 and IIEF-15. These improvements are likely multifactorial, driven by the restoration of hormonal balance, improved cardiovascular health, and the cessation of long-term dialysis, which is known to impair EF in ESRD patients.
The pathophysiology of ED in patients with ESRD is complex and involves both organic and psychogenic factors. Uremia, long-term dialysis, and associated metabolic disorders such as hypertension and diabetes are known contributors to ED. Moreover, the chronic stress and psychological impact of living with renal disease may also exacerbate SexDys. KTx helps to reverse many of these factors by restoring normal kidney function, reducing uremia, and alleviating the psychological burden associated with chronic illness. However, it is important to note that KTx does not resolve all underlying causes of ED, particularly in patients with vascular abnormalities or severe structural penile defects, where transplantation alone may be insufficient to restore normal EF.
Interestingly, while the overall trend shows improvements in EF post-transplantation, the extent of these im
Despite these positive findings, several studies reported that a subset of patients did not experience significant improvements in EF after KTx. These patients often had pre-existing vascular or neurogenic causes of ED, which were unlikely to be corrected by transplantation. Additionally, the use of immunosuppressive medications, while essential for preventing organ rejection, may contribute to endothelial dysfunction, further complicating the recovery of EF. In such cases, adjunct therapies, such as phosphodiesterase type 5 inhibitors (PDE5i), may offer a viable treatment option. PDE5i have been shown to be both safe and effective in renal transplant recipients, with the added benefit of not interfering with common immunosuppressive medications such as cyclosporine or tacrolimus. For patients who do not respond to PDE5i, alternative treatments such as intracavernosal injections, vacuum devices, or even penile implants may be necessary.
Our findings highlight the importance of addressing ED in male ESRD patients both before and after KTx. Improving EF not only enhances quality of life but also promotes better psychological well-being, which is crucial for long-term post-transplant health. However, it remains essential to approach these improvements with caution, as the quality of evidence supporting our findings is low to moderate. This is largely due to the observational nature of the included studies, the high heterogeneity between them, and the small sample sizes of many of the studies.
Strengths: The strengths of the present study include: (1) Comprehensive data synthesis: Our study is one of the first to synthesize the available literature on the effects of KTx on EF in a systematic and meta-analytical framework, providing valuable insights into the relationship between KTx and sexual function in male ESRD patients; (2) Validated mea
Limitations: This study has the following limitations: (1) High heterogeneity: The included studies exhibited significant heterogeneity in terms of population characteristics (e.g., age and comorbidities), dialysis duration, and the time points at which EF was assessed post-transplantation. This heterogeneity limits the generalizability of our findings and may have affected the robustness of our conclusions; (2) Lack of randomized controlled trials: Due to the life-saving nature of KTx, RCTs comparing transplant recipients to dialysis patients are not feasible. As a result, most of the included studies were observational in nature, which limits our ability to establish causality between KTx and improvements in EF; (3) Short follow-up periods: Many studies assessed EF at short intervals after KTx, sometimes as early as three to six months post-transplantation. This limited follow-up may not capture long-term changes in EF, particularly in patients who experience delayed recovery or complications related to graft function; and (4) Potential bias: Most studies relied on self-reported EF outcomes, which are subject to recall bias and may not fully reflect the objective changes in sexual health. Additionally, the lack of standardization in the time points used for postoperative EF assessment introduces further variability in the data.
In conclusion, our systematic review and meta-analysis suggest that KTx offers a promising avenue for improving EF in male patients with ESRD. While the majority of patients experience some level of improvement in EF post-tran
Despite these limitations, our findings underscore the importance of addressing SexDys as a key component of care for ESRD patients undergoing KTx. Clinicians should be aware of the potential benefits of transplantation on EF, but they must also recognize that additional therapies, such as PDE5i, may be necessary for patients with persistent or severe ED post-transplantation. Furthermore, future research should focus on conducting large-scale, long-term cohort studies to better understand the relationship between KTx and EF, as well as to identify potential risk factors for poor sexual health outcomes post-transplant.
Ultimately, KTx not only restores renal function and improves overall quality of life, but it also has the potential to significantly enhance sexual health in a population burdened by high rates of ED. However, more high-quality studies are needed to validate these findings and to establish evidence-based guidelines for managing ED in renal transplant recipients.
| 1. | Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2024 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney Int. 2024;105:S117-S314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1052] [Article Influence: 1052.0] [Reference Citation Analysis (0)] |
| 2. | Holley JL, Schmidt RJ. Changes in fertility and hormone replacement therapy in kidney disease. Adv Chronic Kidney Dis. 2013;20:240-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 42] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 3. | Holley JL. The hypothalamic-pituitary axis in men and women with chronic kidney disease. Adv Chronic Kidney Dis. 2004;11:337-341. [PubMed] [DOI] [Full Text] |
| 4. | Finkelstein FO, Shirani S, Wuerth D, Finkelstein SH. Therapy Insight: sexual dysfunction in patients with chronic kidney disease. Nat Clin Pract Nephrol. 2007;3:200-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 60] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 5. | Thomas J, Kneale D, McKenzie JE, Brennan SE, Bhaumik S. Chapter 2: Determining the scope of the review and the questions it will address. Cochrane Training. [cited 11 September 2024]. Available from: https://training.cochrane.org/handbook/current/chapter-02. |
| 6. | Navaneethan SD, Vecchio M, Johnson DW, Saglimbene V, Graziano G, Pellegrini F, Lucisano G, Craig JC, Ruospo M, Gentile G, Manfreda VM, Querques M, Stroumza P, Torok M, Celia E, Gelfman R, Ferrari JN, Bednarek-Skublewska A, Dulawa J, Bonifati C, Hegbrant J, Wollheim C, Jannini EA, Strippoli GF. Prevalence and correlates of self-reported sexual dysfunction in CKD: a meta-analysis of observational studies. Am J Kidney Dis. 2010;56:670-685. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 117] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 7. | Kang J, Tian J, Lu Y, Song Y, Liu X. Erectile function after kidney transplantation: a meta-analysis. Transl Androl Urol. 2020;9:1967-1979. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Perri A, Izzo G, Lofaro D, La Vignera S, Brunetti A, Calogero AE, Aversa A. Erectile Dysfunction after Kidney Transplantation. J Clin Med. 2020;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | Abarca-Durán X, Fernández-Medina IM, Jiménez-Lasserrotte MDM, Dobarrio-Sanz I, Martínez-Abarca AL, Fernández-Sola C. Sexuality in Kidney Transplant Recipients: A Qualitative Study. Healthcare (Basel). 2021;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 10. | Steiner T, Wunderlich H, Ott U. [Sexuality after kidney transplantation]. Urologe A. 2009;48:1438-1442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Muehrer RJ, Lanuza DM, Brown RL, Djamali A. Sexual concerns among kidney transplant recipients. Clin Transplant. 2014;28:1294-1302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | Schipper K, Abma TA, Koops C, Bakker I, Sanderman R, Schroevers MJ. Sweet and sour after renal transplantation: a qualitative study about the positive and negative consequences of renal transplantation. Br J Health Psychol. 2014;19:580-591. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 47] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 13. | Cumpston M, Lasserson T, Flemyng E, Page MJ. Chapter III: Reporting the review. Cochrane Training. [cited 11 September 2024]. Available from: https://training.cochrane.org/handbook/current/chapter-iii. |
| 14. | Noyes J, Booth A, Cargo M, Flemming K, Harden A, Harris J, Garside R, Hannes K, Pantoja T, Thomas J. Chapter 21: Qualitative evidence. Cochrane Training. [cited 11 September 2024]. Available from: https://training.cochrane.org/handbook/current/chapter-21. |
| 15. | Higgins JPT, Lasserson T, Thomas J, Flemyng E, Churchill R. How to cite the MECIR Standards. Cochrane Community. [cited 17 September 2024]. Available from: https://community.cochrane.org/mecir-manual/key-points-and-introduction/how-cite-mecir-standards. |
| 16. | Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44932] [Cited by in RCA: 40092] [Article Influence: 10023.0] [Reference Citation Analysis (2)] |
| 17. | PubMed. [cited 2024 September 17]. Advanced Search Results. Available from: https://pubmed.ncbi.nlm.nih.gov/advanced/. |
| 18. | Gontero P, Oderda M, Filippini C, Fontana F, Lazzarich E, Stratta P, Turello E, Tizzani A, Frea B. Does kidney transplantation onto the external iliac artery affect the haemodynamic parameters of the cavernosal arteries? Asian J Androl. 2012;14:621-625. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | Mirone V, Longo N, Fusco F, Verze P, Creta M, Parazzini F, Imbimbo C. Renal transplantation does not improve erectile function in hemodialysed patients. Eur Urol. 2009;56:1047-1053. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 36] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 20. | Nassir A. Sexual function in male patients undergoing treatment for renal failure: a prospective view. J Sex Med. 2009;6:3407-3414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 31] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 21. | Pourmand G, Emamzadeh A, Moosavi S, Mehrsai A, Taherimahmoudi M, Nikoobakht M, Saraji A, Salem S. Does renal transplantation improve erectile dysfunction in hemodialysed patients? Transplant Proc. 2007;39:1029-1032. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 32] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 22. | Teng LC, Wang CX, Chen L. Improved erectile function and sex hormone profiles in male Chinese recipients of kidney transplantation. Clin Transplant. 2011;25:265-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 25] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 23. | Javid A, Saberi N, Behnamfar A, Gharzi H, Gholipour F, Bahrami H. Sexual Function in Renal Transplant Recipients with Internal versus External Iliac Artery Anastomosis: A Randomized Clinical Trial. Urol J. 2024;21:121-125. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 24. | Pan J, Zheng Z, Wang W, Hu D, Yao R, Chen Y, Ding H, Zhong J, Hao Z, Liao G. Time-dependent analysis of erectile dysfunction in kidney transplant recipients: insights from four distinct time periods. BMC Infect Dis. 2024;24:728. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 25. | El Hennawy HM, Safar O, Faifi ASA, Shalkamy O, Alqahtani Y, Nazer WE, Mahedy A, Ali MA, Atta EA, Abdelaziz AA, Malki AA, Mirza N, Fageeh AA, Zaitoun MF, Elatreisy A. Does Kidney Transplantation Help Young Patients on Dialysis With Erectile Dysfunction? A Single-center Study. Urology. 2022;169:120-124. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 26. | Mondal S, Sinha Roy PP, Pal DK. Sexual well-being and fertility in male renal transplant recipients: A study in a tertiary care centre. Urologia. 2022;89:636-640. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 27. | Nanjappa B, Singh S, Mavuduru R, Modi M, Minz M, Mandal A, Sakhuja V. 2132 impact of renal transplant on vasculogenic and neurogenic determinants of erectile dysfunction in patients with chronic renal failure. J Urol. 2012;187:e861-e861. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 28. | Pyrgidis N, Mykoniatis I, Sokolakis I, Minopoulou I, Nigdelis MP, Sountoulides P, Verze P, Hatzichristodoulou G, Hatzichristou D. Renal Transplantation Improves Erectile Function in Patients with End-Stage Renal Disease: A Systematic Review and Meta-Analysis. J Urol. 2021;205:1009-1017. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |