Published online Sep 25, 2023. doi: 10.5527/wjn.v12.i4.82
Peer-review started: February 16, 2023
First decision: April 13, 2023
Revised: May 16, 2023
Accepted: June 12, 2023
Article in press: June 12, 2023
Published online: September 25, 2023
Processing time: 215 Days and 18 Hours
The clinical spectrum of immunoglobulin A vasculitis nephritis (IgAVN) ranges from the relatively common transitory microscopic hematuria and/or low-grade proteinuria to nephritic or nephrotic syndrome, rapidly progressive glomerulonephritis, or even renal failure. Clinical and experimental studies have shown a multifactor pathogenesis: Infection triggers, impaired glycosylation of IgA1, complement activation, Toll-like-receptor activation and B cell proliferation. This knowledge can identify IgAVN patients at a greater risk for adverse outcome and increase the evidence for treatment recommendations.
Core Tip: This review summarizes the main mechanisms involved in the pathogenesis of immunoglobulin A vasculitis nephritis and the recent treatment development, in order to decrease the risk of kidney disease progression.
- Citation: Amatruda M, Carucci NS, Chimenz R, Conti G. Immunoglobulin A vasculitis nephritis: Current understanding of pathogenesis and treatment. World J Nephrol 2023; 12(4): 82-92
- URL: https://www.wjgnet.com/2220-6124/full/v12/i4/82.htm
- DOI: https://dx.doi.org/10.5527/wjn.v12.i4.82
Immunoglobulin A (IgA) vasculitis (IgAV), also known as Henoch-Schoenlein purpura (HSP), is the most common systemic vasculitis in children. It is defined by the presence of non-thrombocytopenic palpable purpura or petechiae (mandatory criterion) predominantly located in the lower limbs, plus abdominal pain or IgA deposition in tissue biopsy or arthritis/arthralgia or renal disease[1,2]. 20%-80% of patients with IgAV develop renal involvement, termed IgAV nephritis (IgAVN), which is the key element in affecting long-term outcome[3-5].
According to the European SHARE (Single Hub and Access point for paediatric Rheumatology in Europe) plane[6], all IgAV patients should be investigated for renal involvement at diagnosis and throughout follow-up by measuring blood pressure, determining the presence of haematuria, quantifying albuminuria and/or proteinuria and, finally, estimating glomerular filtration rate (eGFR)[7]. If initial tests are normal, they need to be monitored for at least 6-12 mo[8-12]. The renal biopsy should be performed in the case of impaired eGFR, persistent proteinuria, nephrotic (e.g., severe proteinuria, low serum albumin levels and oedema) or nephritic (e.g., impaired eGFR, hypertension, haematuria/proteinuria) syndrome.
This review summarizes some important current aspects of IgAVN and most importantly the understanding of its pathogenesis and treatment founded on the results of a multitude of clinical and experimental researches.
IgA nephropathy (IgAN) is the most common primary glomerulonephritis in children and adults. Exclusive renal involvement is characterized by a very slow progression, typical of chronic diseases[9]. In contrast, IgAVN is the most common cause of secondary glomerulonephritis in pediatric age; renal involvement tends to have an acute and self-limiting course similar to that of post-infectious glomerulonephritis, but if persistent it can lead to chronic kidney disease and end-stage renal disease approximately 20 years after diagnosis[10,11].
In a retrospective study based on the epidemiological, clinical and laboratory characteristics of IgAV patients, Carucci et al[12] investigated the initial risk factors for IgAVN development, suggesting that age at diagnosis and abdominal pain were associated with a higher risk of onset of the kidney disease in pediatric age. However, additional long-term studies are still needed for the retrospective study type[12].
According to a Japanese study conducted by Komatsu et al[13], IgAVN has two peaks in incidence (1-19 years and 60-69 years), while IgAN has an isolated peak in incidence during the 4th decade. Compared to IgAN, IgAVN is clinically more severe (especially considering the parameters of proteinuria and hypoalbuminemia), and histologically more aggressive, with a higher percentage of proliferative endocapillary glomerulonephritis and crescentic glomerulonephritis[13].
Despite these differences, several studies have shown that the two diseases share the same pathogenesis, namely a defect in IgA1 glycosylation[14-16]. In addition, glomerular histologic findings can be identical, ranging from focal proliferative lesions with diffuse mesangial IgA deposits to extracapillary proliferative lesions with crescent formation, making it sometimes impossible to distinguish IgAN from IgAVN in the absence of extrarenal signs. For this reason, the two entities have recently been considered to be two different manifestations of the same pathology and in 2012, during the Chapel Hill Consensus Conference on the nomenclature of vasculitis, it was decided to replace the definition "HSP" with that of "IgAV", considering it the systemic form of IgAN[17,18].
In an interesting case series by Kamei et al[10], 11% of patients with an initial diagnosis of IgAN subsequently (over a period ranging from 5 mo to 14 years) developed palpable purpura, which allowed the diagnosis to be changed to IgAVN, supporting the hypothesis that IgAN and IgAVN are actually two variants of the same disease. In almost all of these patients, worsening of nephritis was described after the onset of purpura[10]. For this reason, patients diagnosed with IgAN require careful and prolonged follow-up with special attention to the possible appearance of purpura, a sometimes nuanced finding that therefore risks going unnoticed[19].
IgAVN shares many pathophysiological features with IgAN (Table 1). The aim of this review is to update the patho
| No. | Mechanism of IgAVN pathogenesis |
| 1 | Infection triggers (Helicobacter pylori, Streptococcus pneumoniae and Haemophilus Influenzae[22-25] |
| 2 | Genetic factors[26-28] |
| 3 | Impaired glycosylation of IgA1 (Gd-IgA1)[29-41] |
| 4 | Complement activation[42-45] |
| 5 | TLR activation and B cell proliferation[46-48] |
| 6 | AECAs[49-51] |
| 7 | NAPIr[52,53] |
| 8 | Elevated plasma levels of IgE, eosinophil activation, higher levels of ECP and renal α-SMA[54-56] |
Helicobacter pylori[22], Streptococcus pneumoniae and Haemophilus Influenzae[23,24] are the main pathogens associated with the disease. Infections may be involved in the pathogenesis of IgAVN through two mechanisms. The first is due to the presence of N-acetylgalactosamine (GaINAc) on the superficial side of pathogens stimulating the output of cross-reactive IgA and IgG that identify galactose-deficient IgA1 (Gd-IgA1). Alternatively, microbial agents containing antigens similar to structures on the vessel wall generate a cross-reactive autoantibody response[25].
Little is known yet about the role of genetic factors in the IgAVN pathogenesis, although the presence of ethnic and geographical differences in the incidence of IgAV and IgAVN would indicate its involvement[26,27]. Furthermore, several genes involved in cytokine and chemokine production, complement activation, and regulation of endothelium activity have been implicated in IgAV susceptibility[25,28].
Serum levels of Gd-IgA1 are heritable in both IgAN and IgAVN, indicating that the genetic predisposition to develop IgAVN and IgAN is the same[16].
IgAVN and IgAN appear to have identical pathophysiology, with only quantitative differences[29]. High levels of IgA and IgA-containing immune complexes have been observed in both cases. However, this serum abnormality is not a sensitive marker for diagnosis[30]. IgA1, not IgA2, is the main component of IgAN and IgAVN. The IgA1 molecule has a hinge region which contains up to six O-linked glycan chains made up GaINac, typically with β1,3-linked galactose (Gal) attached to it[31,32]. Normally, mono- and di-sialylated Gal-GaINAc disaccharides are present in healthy subjects[33,34]. Elevated levels of Gd-IgA1 have been detected in patients with IgAVN and IgAN, compared with the healthy population and patients with other glomerular diseases[35]. Therefore, Gd-IgA1 now plays a pivotal role in both IgAN and IgAVN pathogenesis[36].
It has been reported that these patients have decreased galactosylation of O-glycans, resulting in reduced β1,3-galactosyltransferase activity in the peripheral B cells of patients. Reduced β1,3-galactosyltransferase activity leads to a lack of terminal β1,3-galactosyl residues in the hinge region of IgA1[15,37].
Gd-IgA1 polimer molecules are known to be anti-glycan IgA1 or IgG, resulting in the formation of circulating immune complexes that are deposited in the renal mesangium and subepithelial and subendothelial space, and which incite glomerular injury. In IgAVN, IgA deposit can be found not just in the kidney, but also in other sides like the skin, and larger immune complexes are found compared to IgAN[15]. Deposition of IgA1-containing immune complexes appears to be mediated by a relationship with mesangial transferrin 1 (CD71) and CD89 receptors, also known as FcαRI, which may occur as a transmembrane receptor in myeloid cells. These receptors on the mesangial surface are more highly expressed than in healthy children.
The monomeric IgA can bind, but without crossbinding with FcαRI, leading to anti-inflammatory reactions[38]. Monovalent FcαRI targeting results in the formation of intracellular structures called "inhibisomes", which obstruct the signaling of nearby activated receptors. This process is referred to as ITAM inhibitory signaling (ITAMi) and results in a downregulation of immune activation. In contrast, IgA immune complexes binding to FcαRI on neutrophils induce activating ITAM signaling, resulting in multiple pro-inflammatory functions. In addition, the activation of FcαRI induces the LTB4 chemoattractant release, resulting in neutrophil migration[39,40].
Consequently, after deposition the mesangial cells start to proliferate and produce other components of the extracellular matrix, and also inflammatory and profibrogenic cells such as cytokines and chemokines[35-41].
The activation of the complement system plays an important role in the pathophysiology of IgAV and IgAVN, including infection triggers and genetics. Indeed, mesangial deposits contain the complement components C3 and C5-C9, which are able to form the attack complex that destroys the membrane of target cells[42]. High levels of C3a, C5a and Bb have also been documented in the serum of pediatric patients with acute IgAV. C5a is a neutrophil chemoattractant that increases during systemic inflammation. C3a and C5a increase interleukin (IL)-8 secretion by endothelial cells, further attracting neutrophils.
More recently, the lectin-related complement activation pathway has also been shown to be involved in IgAVN and IgAN, as IgA can activate mannan-related lectins[43,44]. In contrast, IgA cannot activate the classic pathway and the main activator of the classic pathway, C1q, which is not present in immune complexes[45].
Another mechanism considered to be responsible for IgAV injury is the hyperreactivity of B and T cells in response to specific antigenic triggers. TLR signaling is the first line of defense against microbial infection. Hyperactivated TLR signaling causes cellular inflammatory infiltration that generates cytokines and autoantibodies, leading to autoimmune diseases[46,47].
TLRs are expressed in numerous cells, including kidney cells. There is increasing evidence to support the role for TLRs in autoimmune and inflammatory kidney diseases[22].
Donadio et al[48] showed children with IgAV that had significantly increased expression of mRNA encoding for TLR4, compared with healthy controls. TLR2 mRNA expression showed a borderline increase, while no difference was found in the expression of mRNA encoding for TLR3 and TLR9. Regulatory T cells (Treg) expressing the transcriptional factor FoxP3 play a potent anti-inflammatory role. Defective expression of FoxP3 mRNA and reduced expression of trans
However, it is still unclear if TLR expression is also associated with IgAVN development.
Anti-endothelial cell antibodies (AECAs) are a heterogeneous group of antibodies directed to human endothelial cell antigens. A role of these antibodies in IgAVN has been hypothesized[49]. According to the hypothesis, tumor necrosis factor-α can increase the binding of IgA1 AECAs to endothelial cells. The latter produce IL-8, leading to neutrophil migration[50].
The interaction between IgA1 AECAs and FcαRI on neutrophils results in the release of LTB4, inducing neutrophil recruitment, reactive oxygen species release, neutrophil extracellular traps accompanied by the cell death (NETosis) and antibody-dependent cellular cytotoxicity. All this leads to vascular injury in the final analysis[51].
Other pathogenetic mechanisms underlying IgAVN need to be further investigated. Masuda et al[52] showed that nephritis-associated plasmin receptor, a nephritogenic antigen for acute poststreptococcal glomerulonephritis, might have a pathogenic role in a subgroup of patients with IgAVN[52].
In a study by Davin et al[29], elevated plasma levels of IgE were found more commonly in patients with IgAN, but the pathogenetic role of IgE has not yet been clarified. In fact, mast cells are not usually present in the mesangium[24].
Eosinophil activation, higher levels of eosinophil cationic protein (ECP) in serum, and renal α-smooth muscle (α-SMA) expression have also been proposed as playing a role in the pathogenesis of IgAVN[25].
Observations indicate that enhanced renal α-SMA expression could be an early histological marker of IgAN progression. Similarly, increased expression of α-SMA in the tubule-interstitial region, but not in glomeruli, has been associated with bad prognosis[26].
It is currently not possible to predict and identify which children may develop chronic kidney damage from onset. Some serum and urine markers can identify IgAV patients with or without renal involvement and in predicting the severity of renal inflammation to avoid chronic damage[53,54]. Measuring biomarkers in urine has many advantages: Samples are easy to collect using non-invasive methods; urine reflects damages in renal parenchyma, unlike blood, which comes into contact with many organs and organ systems; the number of different core proteins in the urine is lower than in blood[55]. In a prospective, multicenter study, Pillebout et al[54] identified biomarkers that may identify IgAVN at the onset of the disease: Serum Gd-IgA1 level, urine IgA, IgG, IgM, IL-6, IL-8, IL-10, and IgA-IgG and IgA-sCD89 complex levels[54]. A systematic literature review performed by Sugino et al[56] identifies that some clinical and urinary biomarkers potentially correlate with the presence and severity of IgAVN in children. The most promising preclinical urinary biomarkers in predicting nephritis are: Kidney injury molecule-1 (KIM-1), monocyte chemotactic protein-1 (MCP-1), N-acetyl-β-glucosaminidase (NAG), and angiotensinogen. Urinary KIM-1, MCP-1, and NAG correlate with the disease severity of nephritis (4). However, none of them prove to be established markers of disease. Further studies are needed to verify whether preclinical markers are better than the currently used ones (24-h urinary protein values, urinary protein:creatinine ratio and urinary albumin concentration)[55].
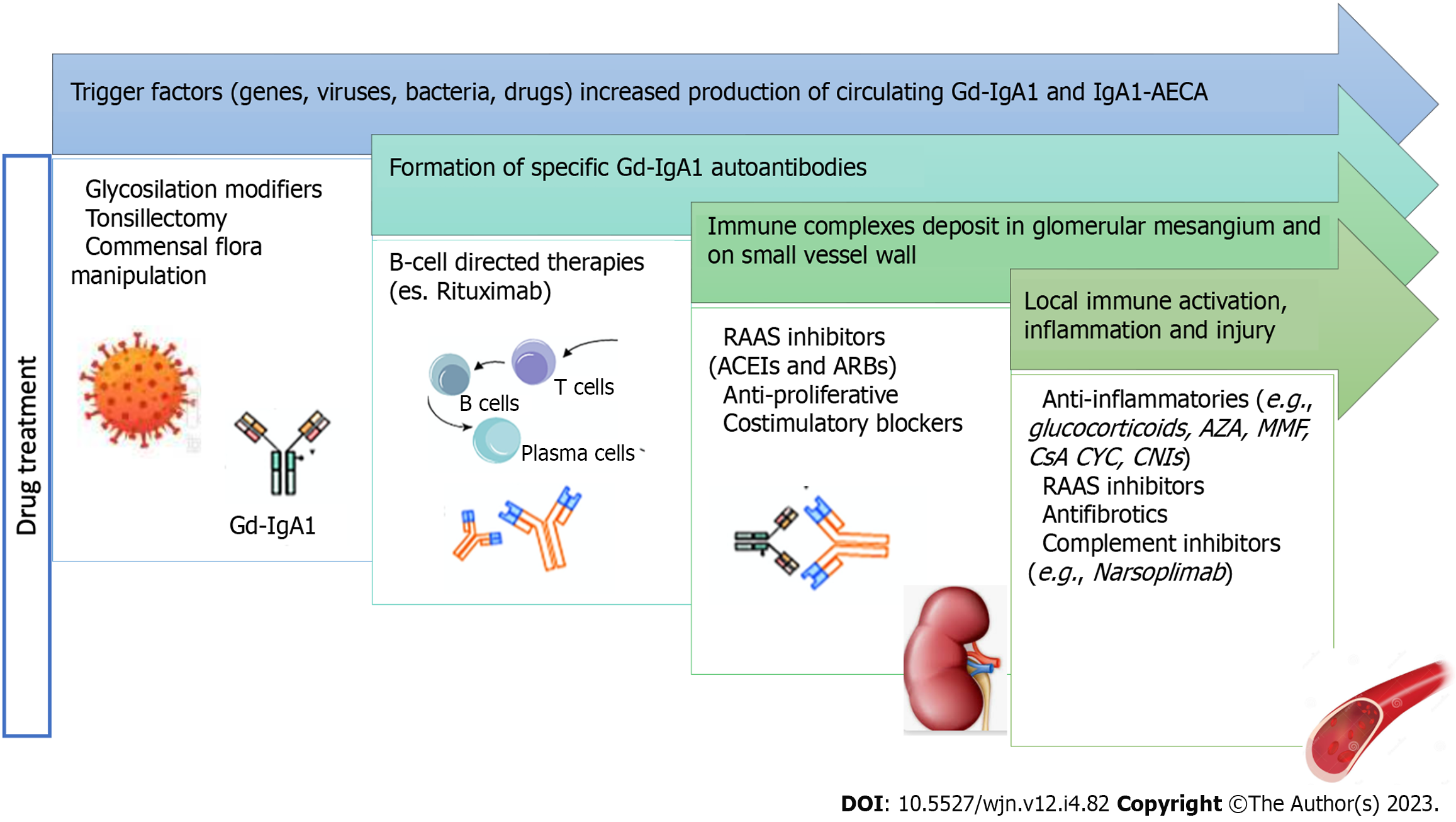
Figure 1 illustrates the integration of the pathogenesis diagram with the drug treatment diagram to reveal the supporting mechanism of the drugs.
Decisions regarding the treatment of IgAVN are challenging due to the large percentage of patients with a positive prognosis and the uncertain clinical progression of single patients. Unfortunately, evidence-based treatment is not yet available even for the most serious event[1]. In several retrospective studies, delayed therapy has been related to a bad outcome. Therefore, despite the risk of spontaneous remission, it may be recommended that severely affected patients be treated as soon as possible.
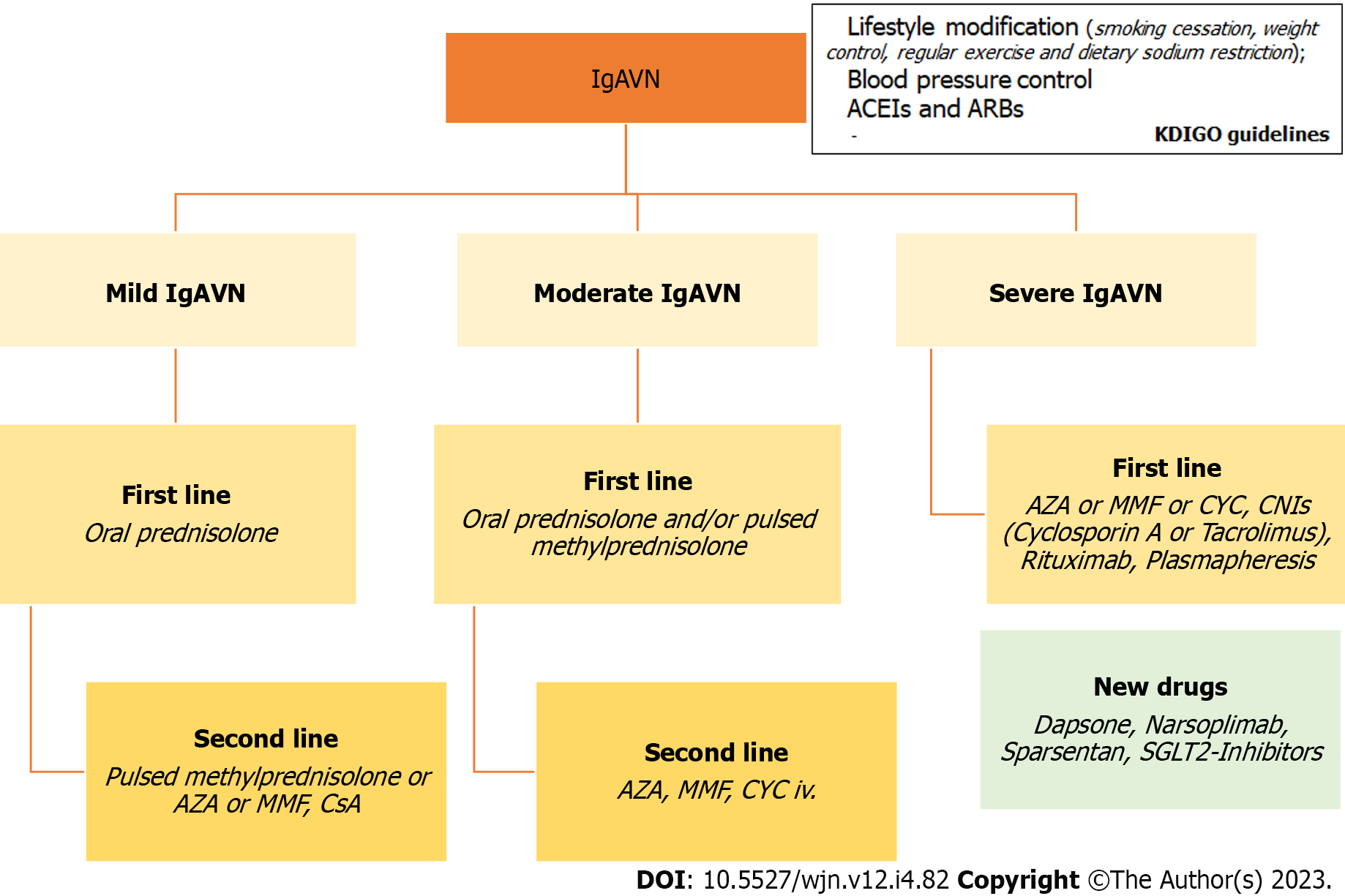
Recently, the Kidney Disease Improving Global Outcomes (KDIGO) guidelines have mainly highlighted that the treatment of IgAVN remains a matter of debate and, in the absence of sufficient long-term data, have recommended that it should be treated in the same way as in patients with non-severe forms of isolated IgAN. However, the KDIGO guidelines do not take into account the more acute onset of IgAVN with more aggressive lesions in renal histology[57]. According to KDIGO guidelines, IgAVN patients should first receive a supporting care including routine modification (smoking cessation, weight control, regular exercise and dietary sodium restriction), blood pressure control and a course of renin-angiotensin system (RAS) blockers without immunosuppressive drugs or steroids. In the opinion of experts, this approach can result in the undertreatment of glomerular inflammation, mainly because acute and potentially aggressive glomerular inflammation goes untouched or its immunosuppressed treatment is postponed for several months.
On the contrary, European treatment guidelines consider IgAN and IgAVN as two distinct entities and suggest oral steroids as a first line therapy in IgAVN. In this regard, the German Society of Pediatric Nephrology has recently suggested an early treatment approach for patients with important kidney involvement. Following this treatment suggestion, IgAVN patients with nephritic syndrome, nephrotic syndrome, or glomerular cellular growths will receive an initial standardized corticosteroid- based treatment regimen for 2 mo, followed by an additional immunosuppression in patients with inadequate response after 3-6 mo from the start of treatment[58].
Corticosteroids, intravenous or oral, are part of most treatment regimens, and there is some evidence of their positive result on the long-term outcome of adult IgAN patients. Similarly, other immunosuppressive therapies, such as azathioprine (AZA), mycophenolate mofetil (MMF), cyclosporine A (CsA), or rituximab, have been shown to be effective in individual cases or in small series of patients. Cyclophosphamide (CYC) has also been used for more severe manifestations of IgAN (Table 2)[6]. In conclusion, given the rare nature of severe IgAVN, there is a necessity to standardize the diagnostic and therapeutic approach at least nationally, but ideally multinationally, in order to gain more expertise and move to evidence-based treatment. Future treatment strategies should be evaluated in large multicenter trials. Figure 2 summarizes the treatments available for IgA vasculitis and nephritis.
| Class of drugs | Ref. | ||
| Mild IgAVN | First line | Corticosteroids: Oral prednisolone | [60-62] |
| Second line (or corticosteroid-sparing agent) | Immunosuppressive therapies: Pulsed methylprednisolone or AZA or MMF, CsA | [6,71,72] | |
| Moderate IgAVN | First line | Corticosteroids: Oral prednisolone and/or pulsed methylprednisolone | [6,60-62] |
| Second line (Cortico-dependent and cortico-resistant forms of IgAVN) | Immunosuppressive therapies: AZA, MMF, CYC iv | [71,72] | |
| Severe IgAVN | First line | Immunosoppresive therapies + corticosteroids: AZA or MMF or CYC, CNIs (Cyclosporin A or Tacrolimus), Rituximab, Plasmapheresis | [64-66,74-77] |
| New drugs: Dapsone, Narsoplimab, Sparsentan | [81,82] | ||
| RAS blockers (ACEIs and ARBs) should be used in IgAVN as soon as possible | [78-80] | ||
Several studies highlight a potential beneficial impact of corticosteroids in IgAVN. Oral prednisolone and/or pulsed methylprednisolone should be used as the earliest treatment in those cases with mild-moderate IgAVN[6]. A randomized, placebo-controlled trial showed that IgAVN was resolved more quickly in children treated with prednisone than in those treated with placebo. However, the study offered outcome data only 6 mo after randomization. Hence, it is unknown whether prednisone treatment reduced the number of cases with persistent IgAVN or simply encouraged a more rapid resolution of the renal disease compared with the placebo[59]. Kim et al[60] showed that corticosteroid exposure significantly reduced serum Gd-IgA1 levels, which are associated with the pathophysiology of IgAVN[60].
However, no evidence has been found that early treatment with steroids could prevent nephritis in IgAV patients and reduce the risk of proteinuria in the following 12 mo[61].
In the cortico-dependent and cortico-resistant forms of IgAVN, other immunosuppressive treatments, such as calcineurin inhibitors (CNIs), AZA, MMF, CYC, rituximab and plasmapheresis can be considered. AZA, MMF or intravenous CYC can be used in the first- or second-line management of moderate-severe IgAVN[6].
CNIs should be considered a hopeful agent for the treatment of severe IgAVN. The two CNIs currently on the market are CsA and tacrolimus. CsA was found to be effective in improving histological lesions and proteinuria in IgAVN patients[62,63]. In a pilot study of 20 IgAVN children, 12 of whom received tacrolimus treatment reached complete remission; eight achieved partial remission at the end of 6 mo[64].
Current data are not in favor of CYC use in IgAVN because no statistically significant differences were found in the group of patients treated with this immunosuppressive drug compared to the group treated with high doses of corticosteroid[65,66]. CsA or oral CYC cannot be routinely recommended in moderate IgAVN. Intravenous CYC with pulsed methylprednisolone and/or oral prednisolone are also required as an earliest treatment in patients with IgAVN[6]. AZA appeared to be an effective steroid-sparing drug. This has allowed all steroid-dependent patients to go steroid-free. No formal guidelines are available for the duration of treatment. In studies no patient has had any adverse events associated with AZA therapy[67,68].
MMF should be suggested patients with IgAVN, especially if proteinuria still remains after an initial steroid course and despite antiproteinuric treatment[69,70]. A current meta-analysis has, in fact, reported results combining eight studies and proposed that patients with IgAN treated with MMF had higher remission than the control group[71]. In association with steroid therapy, AZA and MMF can be used as a maintenance treatment in those patients with severe IgAVN[6].
Data on the use and efficacy of the anti-CD20 monoclonal antibody rituximab in patients with IgAVN are still limited. A few case reports have recommended that rituximab could be successful in IgAVN in both pediatric and adult ages, especially if other oral immunosuppressive treatments have not been able to induce remission[72,73].
Finally, there is plasmapheresis, which can be used as a rescue therapy in cases of rapid progression to renal failure or persistent nephrotic syndrome. Interestingly, early plasmapheresis has been useful in some patients even without additional immunosuppression[74,75].
Numerous data suggest that RAS blockers such as angiotensin-converting enzyme inhibitors/angiotensin receptor blockers should be used in IgAVN and as soon as possible. Prospective randomized trials have shown that the use of these drugs improves long-term renal issues in children and adults and prevents/Limits secondary glomerular injury in patients with persistent proteinuria[76-78].
Dapsone is a drug that could be considered for the treatment of IgAVN because it can suppress the development of toxic-free radicals by neutrophils. It also reduces the output of IgA antibodies, an essential phenomenon in the pathophysiology of IgAVN[79,80].
A phase II study recently demonstrated the safety, tolerability, and efficacy of narsoplimab, a novel Mannan-binding lectin-associated serine proteinase 2 inhibitor. It is a humanized monoclonal antibody that inhibits the lecithin pathway target of the complement system and seems to result in a clinically significant reduction in proteinuria and the stability of renal function as evaluated by eGFR in high-risk patients with IgAN[81].
A clinical trial is being conducted to evaluate the use of sparsentan as a potential first-line treatment in patients with newly diagnosed IgAN who have not received previous treatment with RAS blockers. Treatment response will be based on endpoints of proteinuria and GFR and will be assessed by changes from the baseline compared to another treatment[76].
Many studies have shown the renoprotective role of sodium-glucose cotransporter 2 (SGLT2) inhibitors in early to advanced diabetic kidney disease. Recent evidence show that SGLT2 inhibitors are similarly renoprotective in non-diabetic chronic kidney disease, such as IgAN, in a wide range of eGFR of 25-75 mL/min/1.73 m2 and albumin/creatinine ratio of 200-5000 mg/g[82,83].
According to a recent Cochran study on the prevention and treatment of IgAVN, studies have shown no benefit of prednisone with respect to placebo or no treatment in preventing persistent kidney disease in children without or with little kidney disease at the time of onset[61].
According to the European SHARE initiative, only follow-up is required for patients with microscopic haematuria, no renal disorder and proteinuria, or with non-persistent mild or moderate proteinuria. In the case of severe proteinuria or impaired GFR, a paediatric nephrologist must be consulted and a renal biopsy performed. In the case of mild IgAVN, oral prednisolone should be used as a first-line treatment. In some patients with persistent proteinuria, the addition of AZA or MMF, CsA or pulsed methylprednisolone, may be used as a second-line treatment or as a corticosteroid- sparing agent. For patients with moderate IgAVN, oral prednisolone and/or pulsed methylprednisolone should be used as earliest treatment. Addition of AZA, MMF or intravenous CYC may also be used in the first- or second-line treatment of moderate nephritis, according to the histological findings in the kidney biopsy. For severe IgAVN, intravenous CYC with pulsed methylprednisolone and oral prednisolone should be used as a first-line treatment. AZA/MMF plus steroid therapy can be used as a second life[6].
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Urology and nephrology
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Koukoulaki M, Greece; Miao MS, China; Wang T, China S-Editor: Fan JR L-Editor: A P-Editor: Zhao S
| 1. | Delbet JD, Parmentier C, Herbez Rea C, Mouche A, Ulinski T. Management of IgA Vasculitis with Nephritis. Paediatr Drugs. 2021;23:425-435. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Hastings MC, Rizk DV, Kiryluk K, Nelson R, Zahr RS, Novak J, Wyatt RJ. IgA vasculitis with nephritis: update of pathogenesis with clinical implications. Pediatr Nephrol. 2022;37:719-733. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 42] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 3. | Kliegman RM, Stanton B, St. Geme J, Schor NF, Behrman RE. Pediatria di Nelson (19° edizione). Elsevier. 2013;910-914:1873-1874. |
| 4. | Chen JY, Mao JH. Henoch-Schönlein purpura nephritis in children: incidence, pathogenesis and management. World J Pediatr. 2015;11:29-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 77] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 5. | Pohl M. Henoch-Schönlein purpura nephritis. Pediatr Nephrol. 2015;30:245-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 76] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 6. | Ozen S, Marks SD, Brogan P, Groot N, de Graeff N, Avcin T, Bader-Meunier B, Dolezalova P, Feldman BM, Kone-Paut I, Lahdenne P, McCann L, Pilkington C, Ravelli A, van Royen A, Uziel Y, Vastert B, Wulffraat N, Kamphuis S, Beresford MW. European consensus-based recommendations for diagnosis and treatment of immunoglobulin A vasculitis-the SHARE initiative. Rheumatology (Oxford). 2019;58:1607-1616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 101] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 7. | Salvador CL, Tøndel C, Rowe AD, Bjerre A, Brun A, Brackman D, Mørkrid L. Estimating glomerular filtration rate in children: evaluation of creatinine- and cystatin C-based equations. Pediatr Nephrol. 2019;34:301-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 8. | Goldstein AR, White RH, Akuse R, Chantler C. Long-term follow-up of childhood Henoch-Schönlein nephritis. Lancet. 1992;339:280-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 292] [Cited by in RCA: 235] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 9. | Rajasekaran A, Julian BA, Rizk DV. IgA Nephropathy: An Interesting Autoimmune Kidney Disease. Am J Med Sci. 2021;361:176-194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 122] [Article Influence: 30.5] [Reference Citation Analysis (0)] |
| 10. | Kamei K, Ogura M, Sato M, Ito S, Ishikura K. Evolution of IgA nephropathy into anaphylactoid purpura in six cases--further evidence that IgA nephropathy and Henoch-Schonlein purpura nephritis share common pathogenesis. Pediatr Nephrol. 2016;31:779-785. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 11. | Mao S, Xuan X, Sha Y, Zhao S, Zhu C, Zhang A, Huang S. Clinico-pathological association of Henoch-Schoenlein purpura nephritis and IgA nephropathy in children. Int J Clin Exp Pathol. 2015;8:2334-2342. [PubMed] |
| 12. | Carucci NS, La Barbera G, Peruzzi L, La Mazza A, Silipigni L, Alibrandi A, Santoro D, Chimenz R, Conti G. Time of Onset and Risk Factors of Renal Involvement in Children with Henoch-Schönlein Purpura: Retrospective Study. Children (Basel). 2022;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Reference Citation Analysis (0)] |
| 13. | Komatsu H, Fujimoto S, Yoshikawa N, Kitamura H, Sugiyama H, Yokoyama H. Clinical manifestations of Henoch-Schönlein purpura nephritis and IgA nephropathy: comparative analysis of data from the Japan Renal Biopsy Registry (J-RBR). Clin Exp Nephrol. 2016;20:552-560. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 40] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 14. | Çakıcı EK, Gür G, Yazılıtaş F, Eroğlu FK, Güngör T, Arda N, Orhan D, Özalp Ateş FS, Bülbül M. A retrospective analysis of children with Henoch-Schonlein purpura and re-evaluation of renal pathologies using Oxford classification. Clin Exp Nephrol. 2019;23:939-947. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 15. | Novak J, Moldoveanu Z, Renfrow MB, Yanagihara T, Suzuki H, Raska M, Hall S, Brown R, Huang WQ, Goepfert A, Kilian M, Poulsen K, Tomana M, Wyatt RJ, Julian BA, Mestecky J. IgA nephropathy and Henoch-Schoenlein purpura nephritis: aberrant glycosylation of IgA1, formation of IgA1-containing immune complexes, and activation of mesangial cells. Contrib Nephrol. 2007;157:134-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 79] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 16. | Kiryluk K, Moldoveanu Z, Sanders JT, Eison TM, Suzuki H, Julian BA, Novak J, Gharavi AG, Wyatt RJ. Aberrant glycosylation of IgA1 is inherited in both pediatric IgA nephropathy and Henoch-Schönlein purpura nephritis. Kidney Int. 2011;80:79-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 176] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 17. | Jennette JC, Falk RJ, Bacon PA, Basu N, Cid MC, Ferrario F, Flores-Suarez LF, Gross WL, Guillevin L, Hagen EC, Hoffman GS, Jayne DR, Kallenberg CG, Lamprecht P, Langford CA, Luqmani RA, Mahr AD, Matteson EL, Merkel PA, Ozen S, Pusey CD, Rasmussen N, Rees AJ, Scott DG, Specks U, Stone JH, Takahashi K, Watts RA. 2012 revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum. 2013;65:1-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4416] [Cited by in RCA: 4208] [Article Influence: 350.7] [Reference Citation Analysis (0)] |
| 18. | Mittal A, Dijoo M, Sabhikhi A, Gulati S. Henoch Schönlein Purpura Nephritis Developing in a Child with Known IgA Nephropathy. Indian J Pediatr. 2018;85:808-809. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 19. | Yamabe H, Kaizuka M, Tsunoda S, Nagasawa T, Nomura K, Shimada M. Henoch-Schönlein Nephritis Manifesting with Purpura 15 years after Diagnosis of IgA Nephropathy. Case Rep Nephrol. 2019;2019:1042648. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 20. | Suzuki H, Kiryluk K, Novak J, Moldoveanu Z, Herr AB, Renfrow MB, Wyatt RJ, Scolari F, Mestecky J, Gharavi AG, Julian BA. The pathophysiology of IgA nephropathy. J Am Soc Nephrol. 2011;22:1795-1803. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 429] [Cited by in RCA: 591] [Article Influence: 42.2] [Reference Citation Analysis (0)] |
| 21. | Lau KK, Suzuki H, Novak J, Wyatt RJ. Pathogenesis of Henoch-Schönlein purpura nephritis. Pediatr Nephrol. 2010;25:19-26. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 102] [Cited by in RCA: 102] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 22. | Xiong LJ, Tong Y, Wang ZL, Mao M. Is Helicobacter pylori infection associated with Henoch-Schonlein purpura in Chinese children? a meta-analysis. World J Pediatr. 2012;8:301-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 26] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 23. | Senior BW, Woof JM. The influences of hinge length and composition on the susceptibility of human IgA to cleavage by diverse bacterial IgA1 proteases. J Immunol. 2005;174:7792-7799. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 43] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 24. | Wang L, Li X, Shen H, Mao N, Wang H, Cui L, Cheng Y, Fan J. Bacterial IgA protease-mediated degradation of agIgA1 and agIgA1 immune complexes as a potential therapy for IgA Nephropathy. Sci Rep. 2016;6:30964. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 25. | Rigante D, Castellazzi L, Bosco A, Esposito S. Is there a crossroad between infections, genetics, and Henoch-Schönlein purpura? Autoimmun Rev. 2013;12:1016-1021. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 87] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 26. | Galla JH, Kohaut EC, Alexander R, Mestecky J. Racial difference in the prevalence of IgA-associated nephropathies. Lancet. 1984;2:522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 45] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 27. | Gardner-Medwin JM, Dolezalova P, Cummins C, Southwood TR. Incidence of Henoch-Schönlein purpura, Kawasaki disease, and rare vasculitides in children of different ethnic origins. Lancet. 2002;360:1197-1202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 527] [Cited by in RCA: 455] [Article Influence: 19.8] [Reference Citation Analysis (0)] |
| 28. | Yu HH, Liu PH, Yang YH, Lee JH, Wang LC, Chen WJ, Chiang BL. Chemokine MCP1/CCL2 and RANTES/CCL5 gene polymorphisms influence Henoch-Schönlein purpura susceptibility and severity. J Formos Med Assoc. 2015;114:347-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 29. | Davin JC, Ten Berge IJ, Weening JJ. What is the difference between IgA nephropathy and Henoch-Schönlein purpura nephritis? Kidney Int. 2001;59:823-834. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 170] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 30. | de Almeida JL, Campos LM, Paim LB, Leone C, Koch VH, Silva CA. Renal involvement in Henoch-Schönlein purpura: a multivariate analysis of initial prognostic factors. J Pediatr (Rio J). 2007;83:259-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 31. | Renfrow MB, Mackay CL, Chalmers MJ, Julian BA, Mestecky J, Kilian M, Poulsen K, Emmett MR, Marshall AG, Novak J. Analysis of O-glycan heterogeneity in IgA1 myeloma proteins by Fourier transform ion cyclotron resonance mass spectrometry: implications for IgA nephropathy. Anal Bioanal Chem. 2007;389:1397-1407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 82] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 32. | Tarelli E, Smith AC, Hendry BM, Challacombe SJ, Pouria S. Human serum IgA1 is substituted with up to six O-glycans as shown by matrix assisted laser desorption ionisation time-of-flight mass spectrometry. Carbohydr Res. 2004;339:2329-2335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 83] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 33. | Field MC, Dwek RA, Edge CJ, Rademacher TW. O-linked oligosaccharides from human serum immunoglobulin A1. Biochem Soc Trans. 1989;17:1034-1035. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 70] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 34. | Baenziger J, Kornfeld S. Structure of the carbohydrate units of IgA1 immunoglobulin. II. Structure of the O-glycosidically linked oligosaccharide units. J Biol Chem. 1974;249:7270-7281. [PubMed] |
| 35. | Amore A, Cirina P, Conti G, Brusa P, Peruzzi L, Coppo R. Glycosylation of circulating IgA in patients with IgA nephropathy modulates proliferation and apoptosis of mesangial cells. J Am Soc Nephrol. 2001;12:1862-1871. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 96] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 36. | Lau KK, Wyatt RJ, Moldoveanu Z, Tomana M, Julian BA, Hogg RJ, Lee JY, Huang WQ, Mestecky J, Novak J. Serum levels of galactose-deficient IgA in children with IgA nephropathy and Henoch-Schönlein purpura. Pediatr Nephrol. 2007;22:2067-2072. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 90] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 37. | Allen AC, Willis FR, Beattie TJ, Feehally J. Abnormal IgA glycosylation in Henoch-Schönlein purpura restricted to patients with clinical nephritis. Nephrol Dial Transplant. 1998;13:930-934. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 125] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 38. | Berthelot L, Papista C, Maciel TT, Biarnes-Pelicot M, Tissandie E, Wang PH, Tamouza H, Jamin A, Bex-Coudrat J, Gestin A, Boumediene A, Arcos-Fajardo M, England P, Pillebout E, Walker F, Daugas E, Vrtosvnik F, Flamant M, Benhamou M, Cogné M, Moura IC, Monteiro RC. Transglutaminase is essential for IgA nephropathy development acting through IgA receptors. J Exp Med. 2012;209:793-806. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 121] [Cited by in RCA: 142] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 39. | Moura IC, Centelles MN, Arcos-Fajardo M, Malheiros DM, Collawn JF, Cooper MD, Monteiro RC. Identification of the transferrin receptor as a novel immunoglobulin (Ig)A1 receptor and its enhanced expression on mesangial cells in IgA nephropathy. J Exp Med. 2001;194:417-425. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 207] [Cited by in RCA: 199] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 40. | Heineke MH, Ballering AV, Jamin A, Ben Mkaddem S, Monteiro RC, Van Egmond M. New insights in the pathogenesis of immunoglobulin A vasculitis (Henoch-Schönlein purpura). Autoimmun Rev. 2017;16:1246-1253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 212] [Article Influence: 26.5] [Reference Citation Analysis (0)] |
| 41. | Moura IC, Benhamou M, Launay P, Vrtovsnik F, Blank U, Monteiro RC. The glomerular response to IgA deposition in IgA nephropathy. Semin Nephrol. 2008;28:88-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 44] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 42. | Yang YH, Tsai IJ, Chang CJ, Chuang YH, Hsu HY, Chiang BL. The interaction between circulating complement proteins and cutaneous microvascular endothelial cells in the development of childhood Henoch-Schönlein Purpura. PLoS One. 2015;10:e0120411. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 37] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 43. | Roos A, Rastaldi MP, Calvaresi N, Oortwijn BD, Schlagwein N, van Gijlswijk-Janssen DJ, Stahl GL, Matsushita M, Fujita T, van Kooten C, Daha MR. Glomerular activation of the lectin pathway of complement in IgA nephropathy is associated with more severe renal disease. J Am Soc Nephrol. 2006;17:1724-1734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 298] [Cited by in RCA: 332] [Article Influence: 17.5] [Reference Citation Analysis (0)] |
| 44. | Hisano S, Matsushita M, Fujita T, Iwasaki H. Activation of the lectin complement pathway in Henoch-Schönlein purpura nephritis. Am J Kidney Dis. 2005;45:295-302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 71] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 45. | Wyatt RJ. The complement system in IgA nephropathy and Henoch-Schönlein purpura: functional and genetic aspects. Contrib Nephrol. 1993;104:82-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 46. | Gluba A, Banach M, Hannam S, Mikhailidis DP, Sakowicz A, Rysz J. The role of Toll-like receptors in renal diseases. Nat Rev Nephrol. 2010;6:224-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 150] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 47. | Amura CR, Renner B, Lyubchenko T, Faubel S, Simonian PL, Thurman JM. Complement activation and toll-like receptor-2 signaling contribute to cytokine production after renal ischemia/reperfusion. Mol Immunol. 2012;52:249-257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 36] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 48. | Donadio ME, Loiacono E, Peruzzi L, Amore A, Camilla R, Chiale F, Vergano L, Boido A, Conrieri M, Bianciotto M, Bosetti FM, Coppo R. Toll-like receptors, immunoproteasome and regulatory T cells in children with Henoch-Schönlein purpura and primary IgA nephropathy. Pediatr Nephrol. 2014;29:1545-1551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 56] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 49. | Legendre P, Régent A, Thiebault M, Mouthon L. Anti-endothelial cell antibodies in vasculitis: A systematic review. Autoimmun Rev. 2017;16:146-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 50. | Yang YH, Huang YH, Lin YL, Wang LC, Chuang YH, Yu HH, Lin YT, Chiang BL. Circulating IgA from acute stage of childhood Henoch-Schönlein purpura can enhance endothelial interleukin (IL)-8 production through MEK/ERK signalling pathway. Clin Exp Immunol. 2006;144:247-253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 53] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 51. | Otten MA, Bakema JE, Tuk CW, Glennie MJ, Tutt AL, Beelen RH, van de Winkel JG, van Egmond M. Enhanced FcαRI-mediated neutrophil migration towards tumour colonies in the presence of endothelial cells. Eur J Immunol. 2012;42:1815-1821. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 52. | Masuda M, Nakanishi K, Yoshizawa N, Iijima K, Yoshikawa N. Group A streptococcal antigen in the glomeruli of children with Henoch-Schönlein nephritis. Am J Kidney Dis. 2003;41:366-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 58] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 53. | Williams CEC, Toner A, Wright RD, Oni L. A systematic review of urine biomarkers in children with IgA vasculitis nephritis. Pediatr Nephrol. 2021;36:3033-3044. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 54. | Pillebout E, Jamin A, Ayari H, Housset P, Pierre M, Sauvaget V, Viglietti D, Deschenes G, Monteiro RC, Berthelot L; HSPrognosis group. Biomarkers of IgA vasculitis nephritis in children. PLoS One. 2017;12:e0188718. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 70] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 55. | Jelusic M, Sestan M, Giani T, Cimaz R. New Insights and Challenges Associated With IgA Vasculitis and IgA Vasculitis With Nephritis-Is It Time to Change the Paradigm of the Most Common Systemic Vasculitis in Childhood? Front Pediatr. 2022;10:853724. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 21] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 56. | Sugino H, Sawada Y, Nakamura M. IgA Vasculitis: Etiology, Treatment, Biomarkers and Epigenetic Changes. Int J Mol Sci. 2021;22. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 38] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 57. | Rovin BH, Adler SG, Barratt J, Bridoux F, Burdge KA, Chan TM, Cook HT, Fervenza FC, Gibson KL, Glassock RJ, Jayne DRW, Jha V, Liew A, Liu ZH, Mejía-Vilet JM, Nester CM, Radhakrishnan J, Rave EM, Reich HN, Ronco P, Sanders JF, Sethi S, Suzuki Y, Tang SCW, Tesar V, Vivarelli M, Wetzels JFM, Lytvyn L, Craig JC, Tunnicliffe DJ, Howell M, Tonelli MA, Cheung M, Earley A, Floege J. Executive summary of the KDIGO 2021 Guideline for the Management of Glomerular Diseases. Kidney Int. 2021;100:753-779. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 260] [Cited by in RCA: 443] [Article Influence: 110.8] [Reference Citation Analysis (0)] |
| 58. | Butzer S, Hennies I, Gimpel C, Gellermann J, Schalk G, König S, Büscher AK, Lemke A, Pohl M. Early clinical course of biopsy-proven IgA vasculitis nephritis. BMC Pediatr. 2022;22:570. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 59. | Ronkainen J, Koskimies O, Ala-Houhala M, Antikainen M, Merenmies J, Rajantie J, Ormälä T, Turtinen J, Nuutinen M. Early prednisone therapy in Henoch-Schönlein purpura: a randomized, double-blind, placebo-controlled trial. J Pediatr. 2006;149:241-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 223] [Cited by in RCA: 184] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 60. | Kim MJ, Schaub S, Molyneux K, Koller MT, Stampf S, Barratt J. Effect of Immunosuppressive Drugs on the Changes of Serum Galactose-Deficient IgA1 in Patients with IgA Nephropathy. PLoS One. 2016;11:e0166830. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 61. | Hahn D, Hodson EM, Willis NS, Craig JC. Interventions for preventing and treating kidney disease in Henoch-Schönlein Purpura (HSP). Cochrane Database Syst Rev. 2015;2015:CD005128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 30] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 62. | Jauhola O, Ronkainen J, Autio-Harmainen H, Koskimies O, Ala-Houhala M, Arikoski P, Hölttä T, Jahnukainen T, Rajantie J, Ormälä T, Nuutinen M. Cyclosporine A vs. methylprednisolone for Henoch-Schönlein nephritis: a randomized trial. Pediatr Nephrol. 2011;26:2159-2166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 54] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 63. | Shin JI, Park JM, Shin YH, Kim JH, Lee JS, Jeong HJ. Henoch-Schönlein purpura nephritis with nephrotic-range proteinuria: histological regression possibly associated with cyclosporin A and steroid treatment. Scand J Rheumatol. 2005;34:392-395. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 64. | Zhang DF, Hao GX, Li CZ, Yang YJ, Liu FJ, Liu L, Yuan XY, Li RH, Dong L, Dong Q, Jacqz-Aigrain E, Zhao W. Off-label use of tacrolimus in children with Henoch-Schönlein purpura nephritis: a pilot study. Arch Dis Child. 2018;103:772-775. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 65. | Pillebout E, Alberti C, Guillevin L, Ouslimani A, Thervet E; CESAR study group. Addition of cyclophosphamide to steroids provides no benefit compared with steroids alone in treating adult patients with severe Henoch Schönlein Purpura. Kidney Int. 2010;78:495-502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 109] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 66. | Tarshish P, Bernstein J, Edelmann CM Jr. Henoch-Schönlein purpura nephritis: course of disease and efficacy of cyclophosphamide. Pediatr Nephrol. 2004;19:51-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 106] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 67. | Singh S, Devidayal, Kumar L, Joshi K, Minz RW, Datta U. Severe Henoch-Schönlein nephritis: resolution with azathioprine and steroids. Rheumatol Int. 2002;22:133-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 40] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 68. | Sarcina C, Tinelli C, Ferrario F, Pani A, De Silvestri A, Scaini P, Del Vecchio L, Alberghini E, Buzzi L, Baragetti I, Pozzi C. Changes in Proteinuria and Side Effects of Corticosteroids Alone or in Combination with Azathioprine at Different Stages of IgA Nephropathy. Clin J Am Soc Nephrol. 2016;11:973-981. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 40] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 69. | Ren P, Han F, Chen L, Xu Y, Wang Y, Chen J. The combination of mycophenolate mofetil with corticosteroids induces remission of Henoch-Schönlein purpura nephritis. Am J Nephrol. 2012;36:271-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 45] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 70. | Han F, Chen LL, Ren PP, Le JY, Choong PJ, Wang HJ, Xu Y, Chen JH. Mycophenolate mofetil plus prednisone for inducing remission of Henoch-Schönlein purpura nephritis: a retrospective study. J Zhejiang Univ Sci B. 2015;16:772-779. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 71. | Du B, Jia Y, Zhou W, Min X, Miao L, Cui W. Efficacy and safety of mycophenolate mofetil in patients with IgA nephropathy: an update meta-analysis. BMC Nephrol. 2017;18:245. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 72. | Fenoglio R, Naretto C, Basolo B, Quattrocchio G, Ferro M, Mesiano P, Beltrame G, Roccatello D. Rituximab therapy for IgA-vasculitis with nephritis: a case series and review of the literature. Immunol Res. 2017;65:186-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 40] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 73. | Maritati F, Fenoglio R, Pillebout E, Emmi G, Urban ML, Rocco R, Nicastro M, Incerti M, Goldoni M, Trivioli G, Silvestri E, Mohammad AJ, Jayne D, Eriksson P, Segelmark M, Novikov P, Harris H, Roccatello D, Vaglio A. Brief Report: Rituximab for the Treatment of Adult-Onset IgA Vasculitis (Henoch-Schönlein). Arthritis Rheumatol. 2018;70:109-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 58] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 74. | Shenoy M, Ognjanovic MV, Coulthard MG. Treating severe Henoch-Schönlein and IgA nephritis with plasmapheresis alone. Pediatr Nephrol. 2007;22:1167-1171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 66] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 75. | Augusto JF, Sayegh J, Delapierre L, Croue A, Tollis F, Cousin M, Subra JF. Addition of plasma exchange to glucocorticosteroids for the treatment of severe Henoch-Schönlein purpura in adults: a case series. Am J Kidney Dis. 2012;59:663-669. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 27] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 76. | Ninchoji T, Kaito H, Nozu K, Hashimura Y, Kanda K, Kamioka I, Shima Y, Hamahira K, Nakanishi K, Tanaka R, Yoshikawa N, Iijima K, Matsuo M. Treatment strategies for Henoch-Schönlein purpura nephritis by histological and clinical severity. Pediatr Nephrol. 2011;26:563-569. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 38] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 77. | Praga M, Gutiérrez E, González E, Morales E, Hernández E. Treatment of IgA nephropathy with ACE inhibitors: a randomized and controlled trial. J Am Soc Nephrol. 2003;14:1578-1583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 228] [Cited by in RCA: 212] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 78. | Coppo R, Peruzzi L, Amore A, Piccoli A, Cochat P, Stone R, Kirschstein M, Linné T. IgACE: a placebo-controlled, randomized trial of angiotensin-converting enzyme inhibitors in children and young people with IgA nephropathy and moderate proteinuria. J Am Soc Nephrol. 2007;18:1880-1888. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 177] [Cited by in RCA: 165] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 79. | Lee KH, Hong SH, Jun J, Jo Y, Jo W, Choi D, Joo J, Jung G, Ahn S, Kronbichler A, Eisenhut M, Shin JI. Treatment of refractory IgA vasculitis with dapsone: a systematic review. Clin Exp Pediatr. 2020;63:158-163. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 80. | Iqbal H, Evans A. Dapsone therapy for Henoch-Schönlein purpura: a case series. Arch Dis Child. 2005;90:985-986. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 26] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 81. | Lafayette RA, Rovin BH, Reich HN, Tumlin JA, Floege J, Barratt J. Safety, Tolerability and Efficacy of Narsoplimab, a Novel MASP-2 Inhibitor for the Treatment of IgA Nephropathy. Kidney Int Rep. 2020;5:2032-2041. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 106] [Article Influence: 21.2] [Reference Citation Analysis (0)] |
| 82. | Tesař V. SGLT2 inhibitors in non-diabetic kidney disease. Adv Clin Exp Med. 2022;31:105-107. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 83. | Wheeler DC, Toto RD, Stefánsson BV, Jongs N, Chertow GM, Greene T, Hou FF, McMurray JJV, Pecoits-Filho R, Correa-Rotter R, Rossing P, Sjöström CD, Umanath K, Langkilde AM, Heerspink HJL; DAPA-CKD Trial Committees and Investigators. A pre-specified analysis of the DAPA-CKD trial demonstrates the effects of dapagliflozin on major adverse kidney events in patients with IgA nephropathy. Kidney Int. 2021;100:215-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 240] [Article Influence: 60.0] [Reference Citation Analysis (0)] |