Copyright
©The Author(s) 2019.
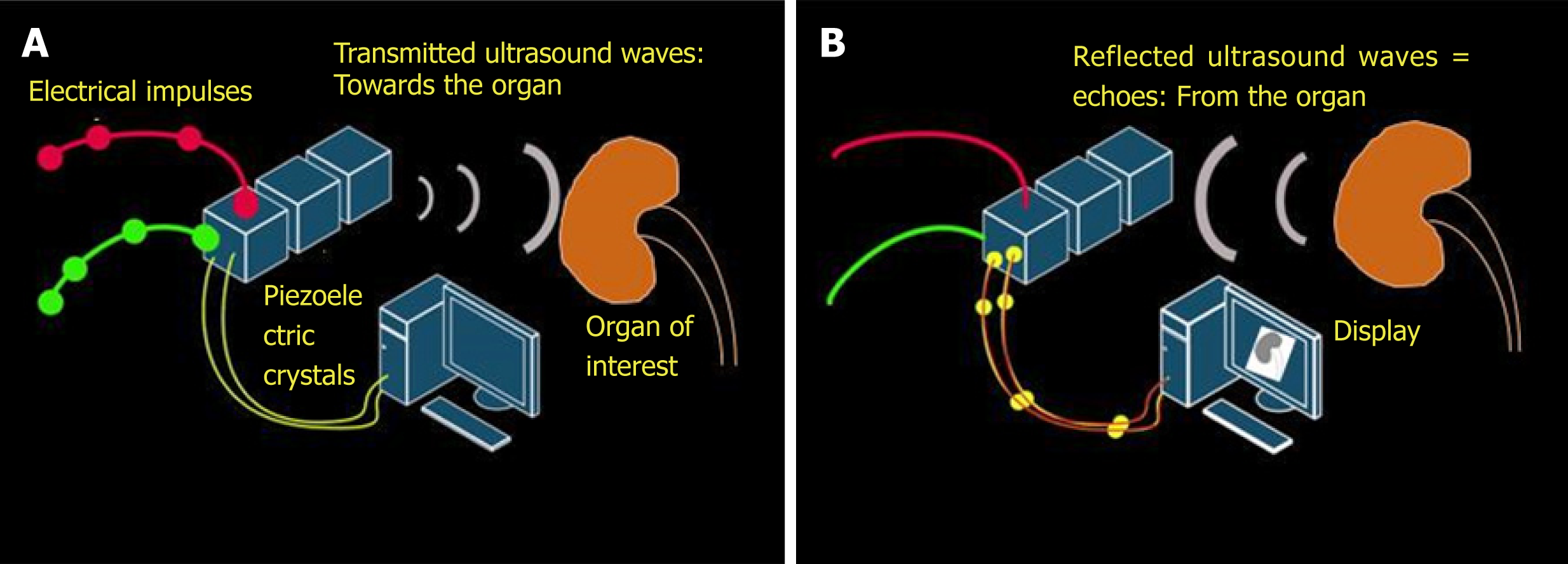
Figure 1 Working principles underlying generation of ultrasound image.
A: Inverse piezoelectric effect – conversion of electrical energy into mechanical energy (ultrasound waves); B: Piezoelectric effect – conversion of mechanical energy into electrical energy by the piezoelectric crystals located in the transducer. These impulses are displayed on the monitor in the image format.
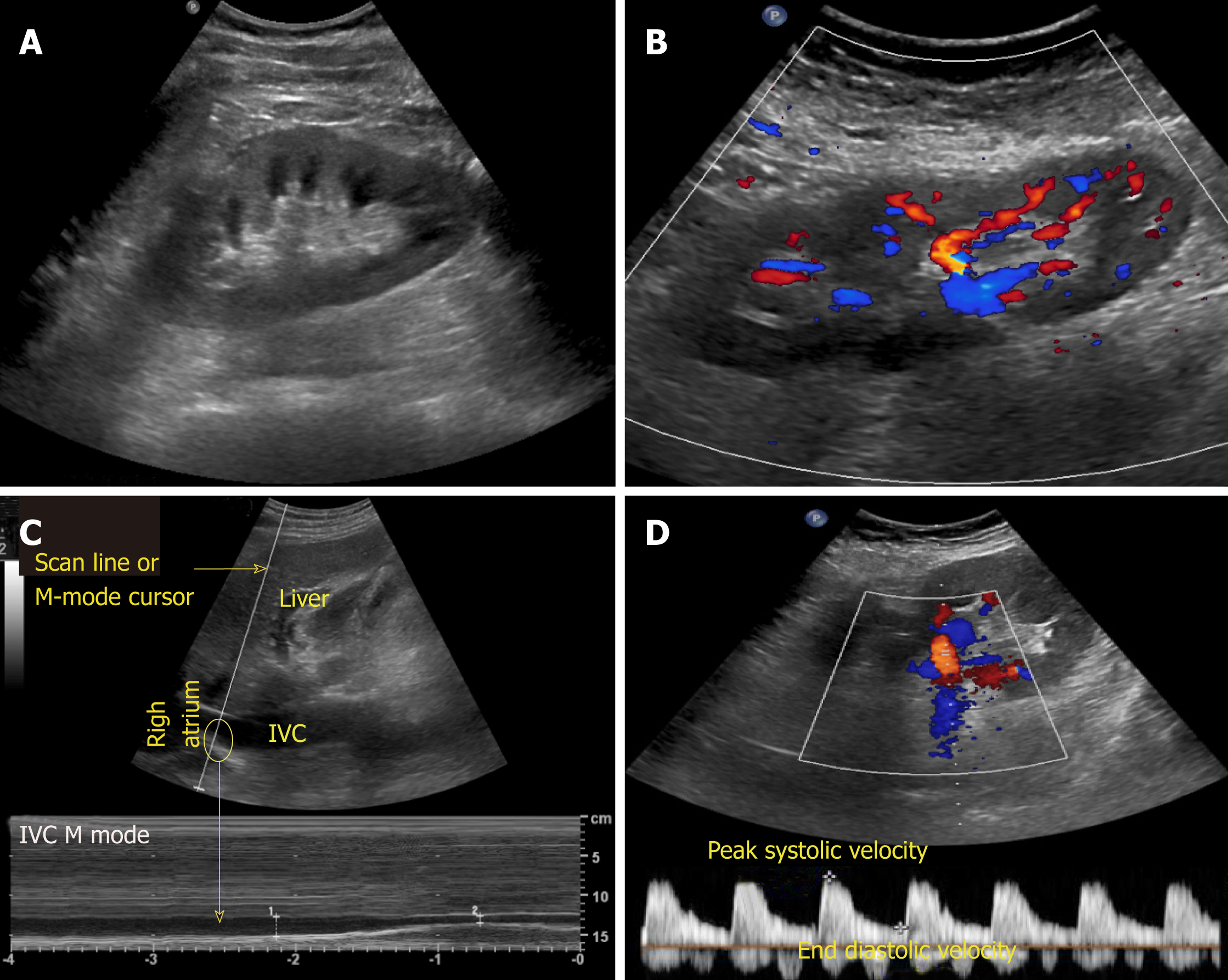
Figure 2 Commonly used modes in nephrology-oriented point of care ultrasonography.
A: B-mode: Grey-scale image of the left kidney; B: Color Doppler mode: Blood flow inside the kidney is indicated by red and blue colors; C: M-mode: Variations in diameter of the inferior vena cava over time at the area of interest (circle); D: Pulsed wave Doppler: Transverse view of the kidney with graphic representation of flow in the renal artery.
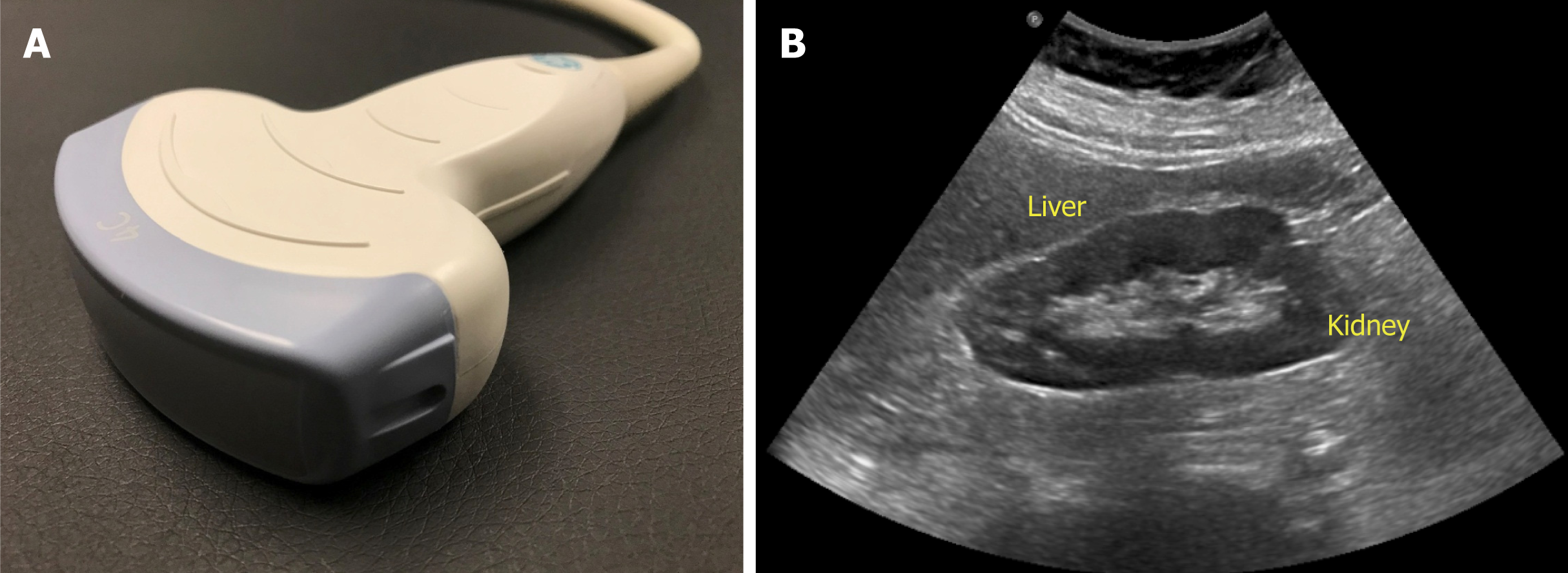
Figure 3 Curvilinear probe (A) used for abdominal applications (B) example of an image obtained using this probe.
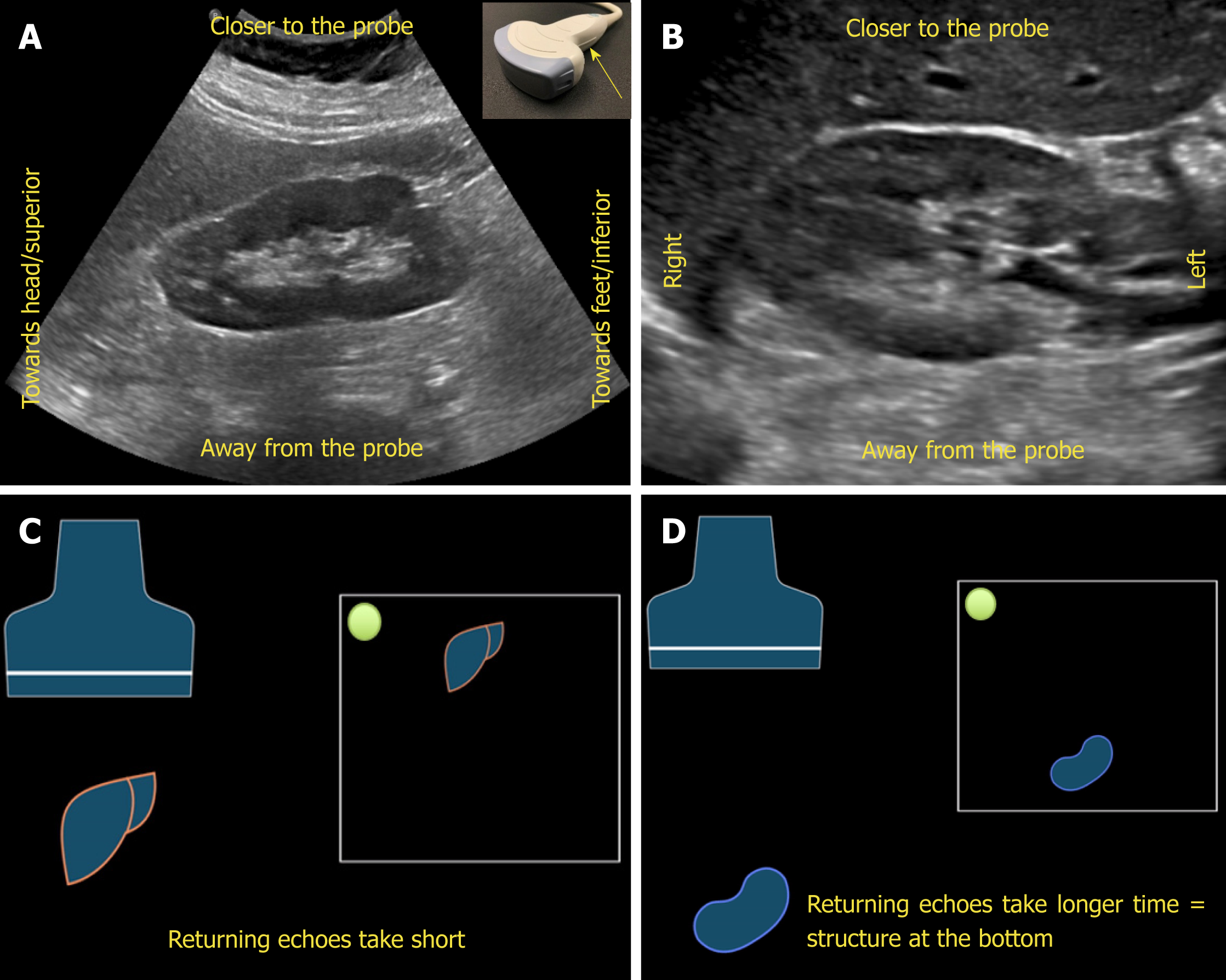
Figure 4 Orientation of the image.
A, B: Ultrasound image of the (A) longitudinal and (B) transverse views of the right kidney demonstrating the image orientation; C, D: Cartoon illustrating that echoes returning from a structure that is farther from the probe take longer time compared to those returning from the structure that is closer to the probe and that farther structure is portrayed at the bottom of the screen and the nearer one on the top. Note that the arrow in Figure 4A points to the probe marker and the green dot represents indicator on the screen.
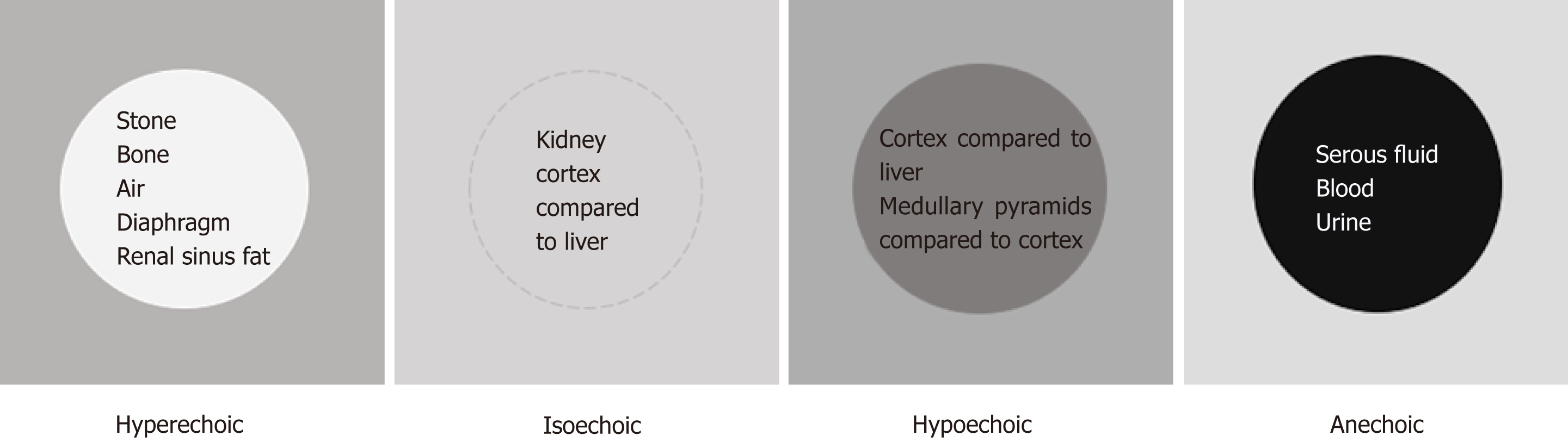
Figure 5 Illustration of “relative echogenicity”.
The circular area in the center is hyperechoic (brighter), isoechoic (similar brightness), hypoechoic (darker) and anechoic (black) compared to the surrounding area respectively. Echogenicity of the commonly encountered structures on renal sonography are listed inside the circles. Note that renal cortex can be either isoechoic or hypoechoic compared to that of normal liver.
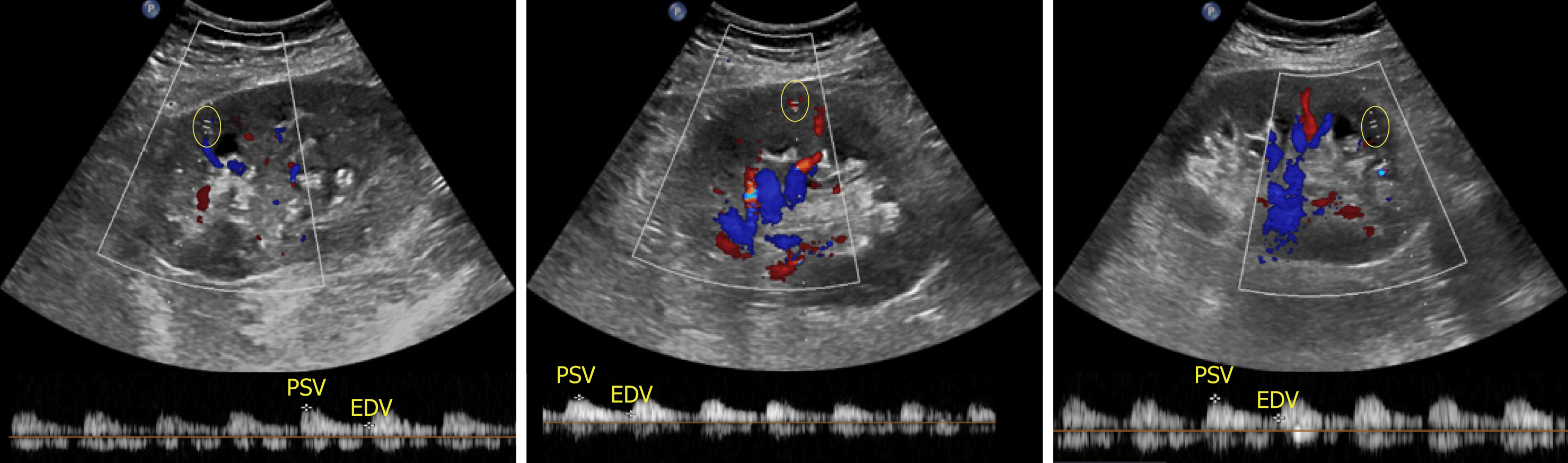
Figure 6 Images of the transplanted kidney demonstrating resistive indices in the superior, middle and inferior arcuate arteries (at corticomedullary junction; sample indicated by yellow circle), which were calculated as 0.
61, 0.64 and 0.60 respectively and EDV = end diastolic velocity.
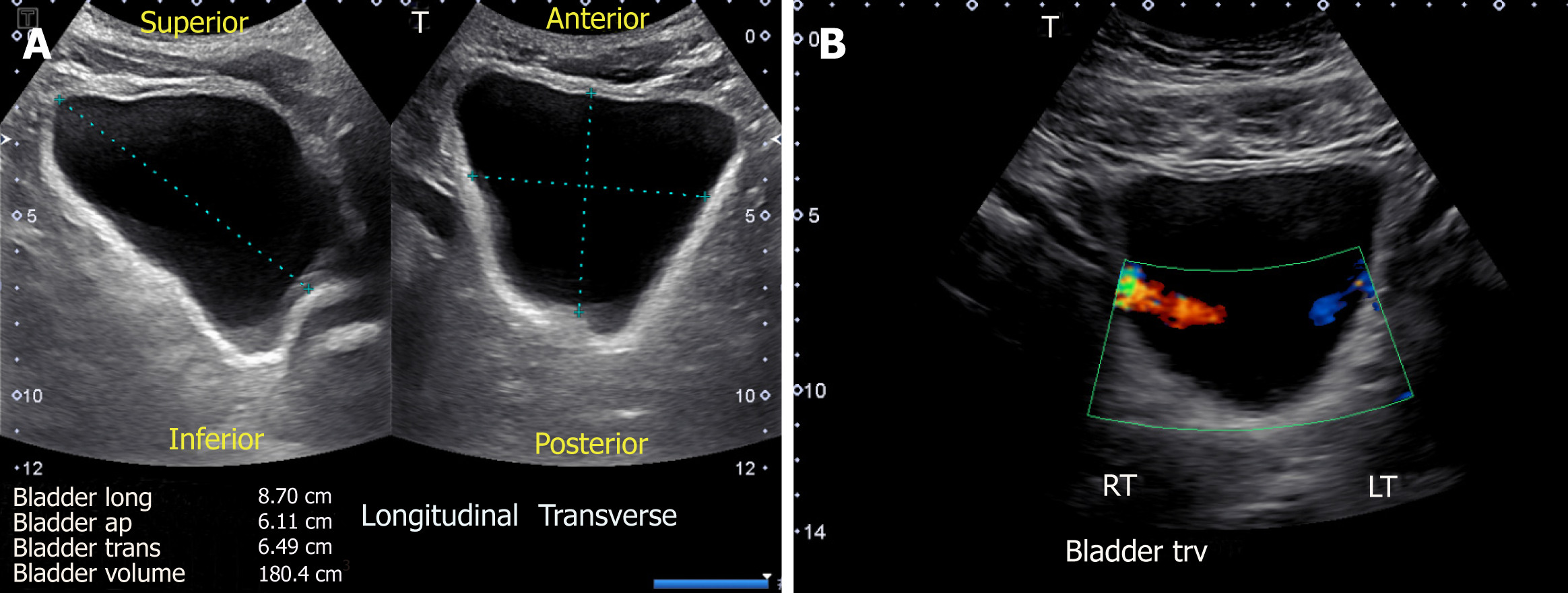
Figure 7 Urinary bladder ultrasound demonstrating (A) bladder volume measurement: Length, antero-posterior and transverse measurements are obtained and multiplied by 0.
52 to obtain the approximate amount of urine volume and (B) color Doppler image of the bladder showing ureteral jets.
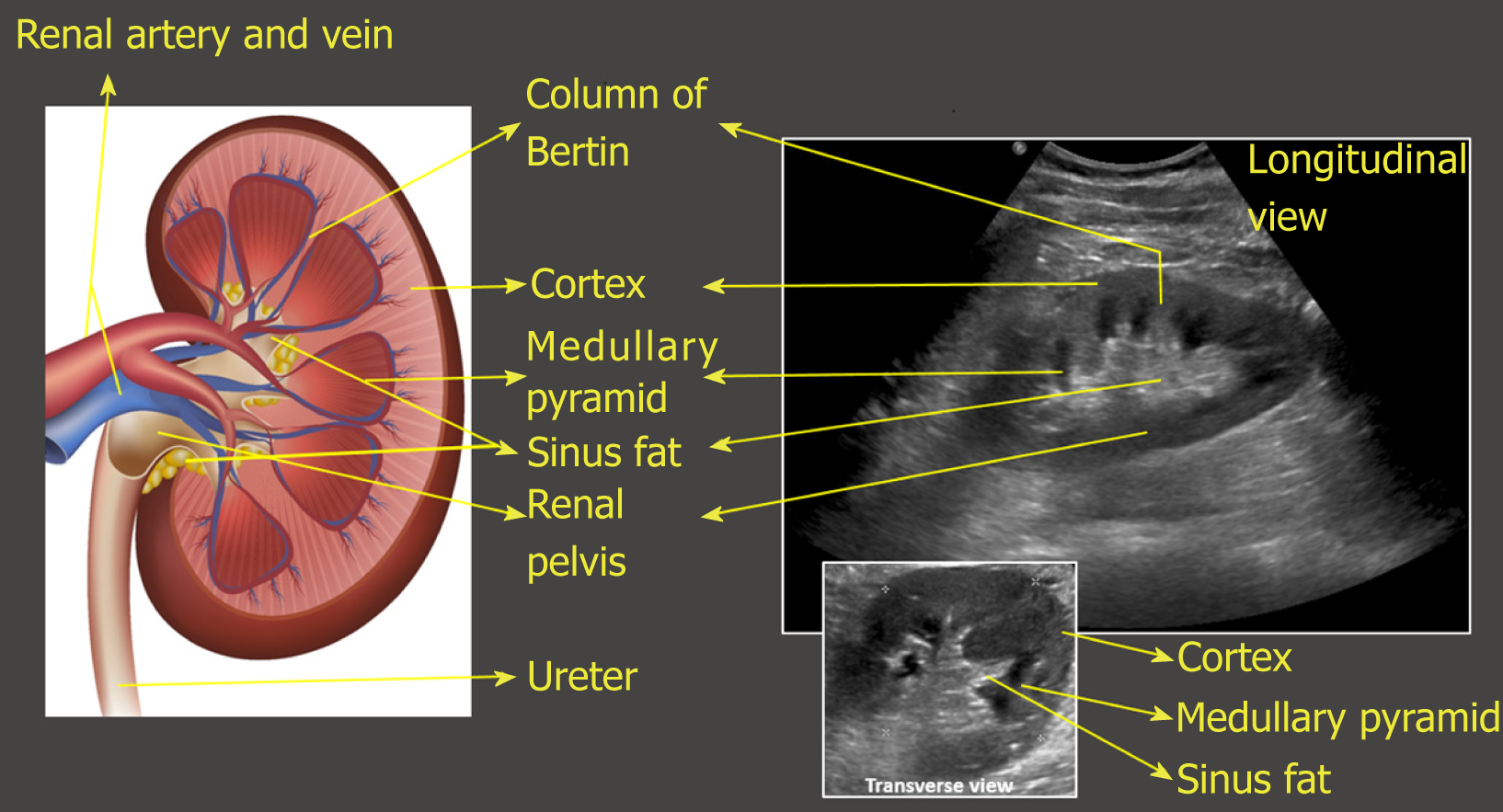
Figure 8 Illustration of longitudinal section of the kidney with corresponding ultrasound image.
Transverse view of the kidney is also shown. Note that the most echogenic part of the kidney is sinus fat, and calyces and ureter are not usually visible unless distended. Renal pelvis is hypoechoic but not usually “black” (anechoic) unless there is hydronephrosis.
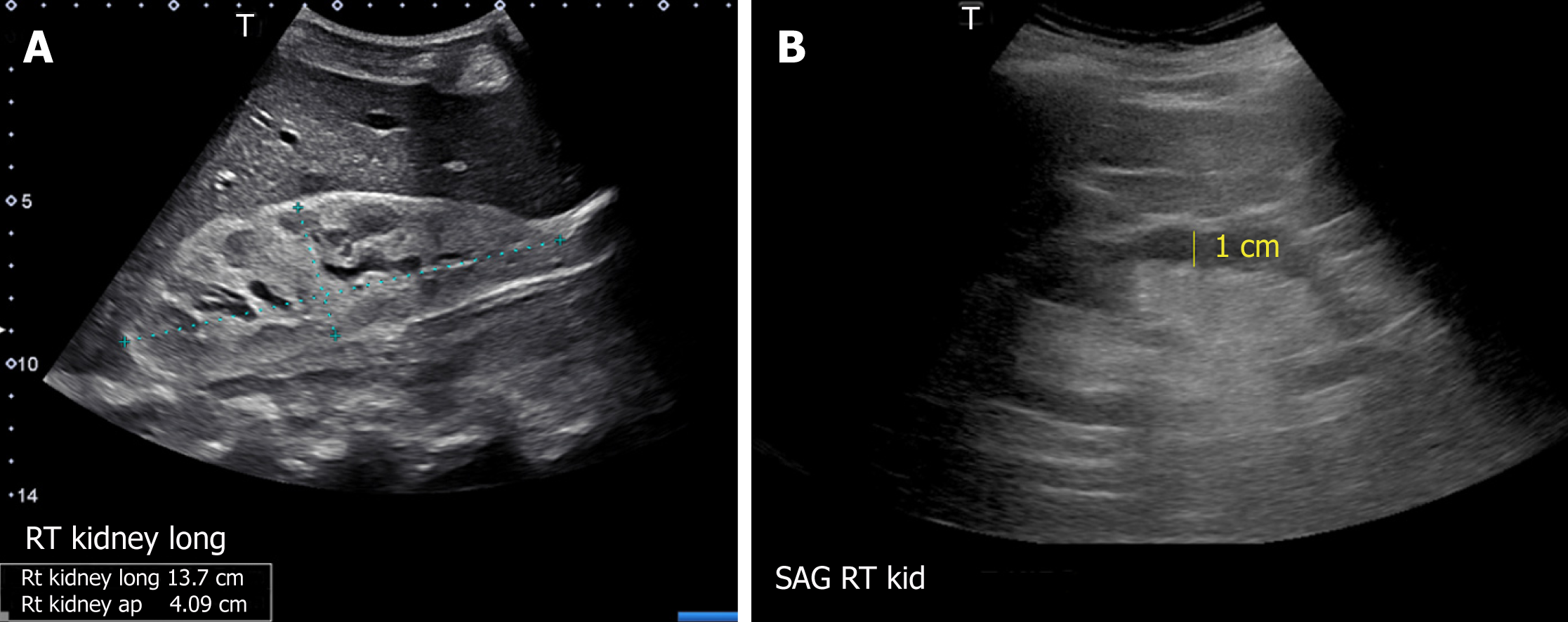
Figure 9 Renal sonogram demonstrating (A) large echogenic kidney in a patient with multiple myeloma and (B) thin parenchyma approximately 1 cm in a patient with chronic kidney disease.
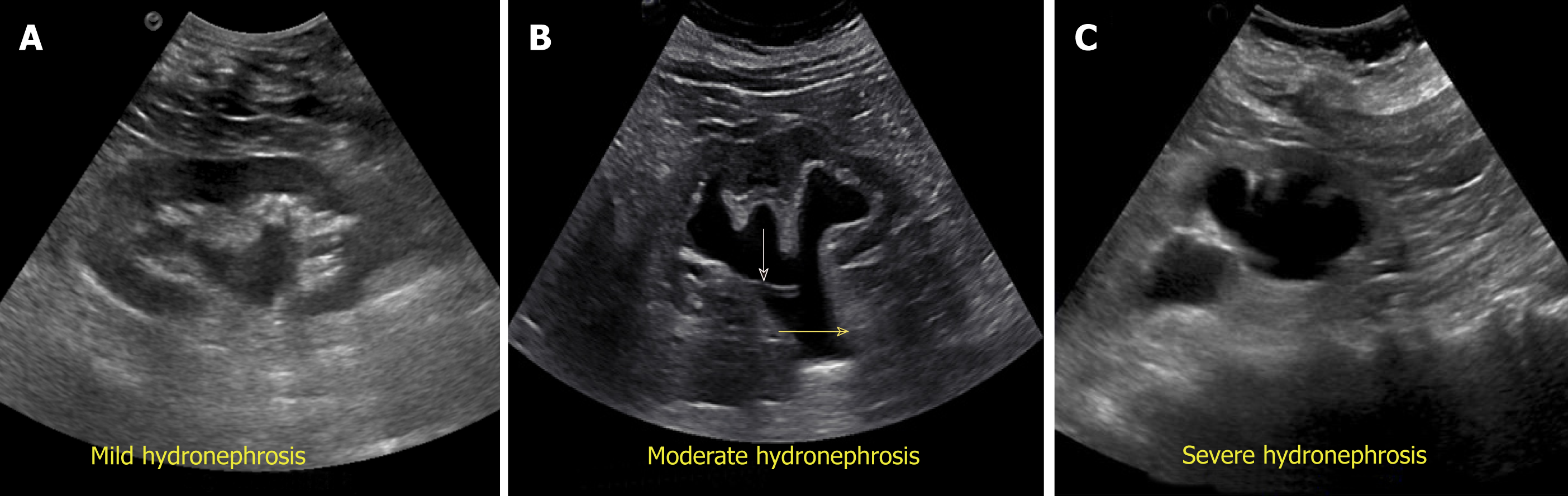
Figure 10 Grading of hydronephrosis.
A: Note that as the severity of hydronephrosis increases, the urine (anechoic structure) moves proximally into the kidney exerting pressure on the parenchyma; B: White arrow points to ureteral stent and yellow arrow indicates dilated proximal ureter.
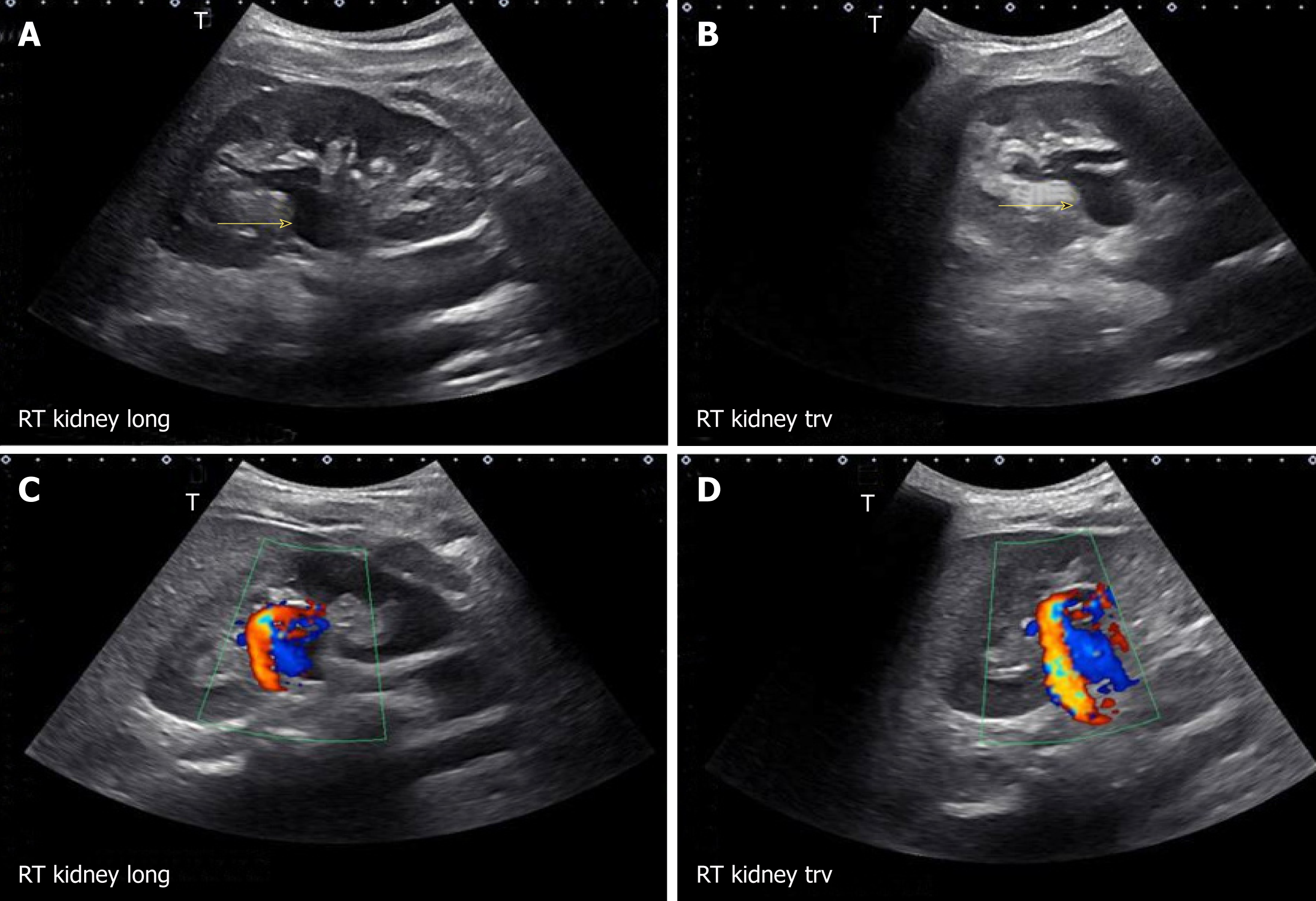
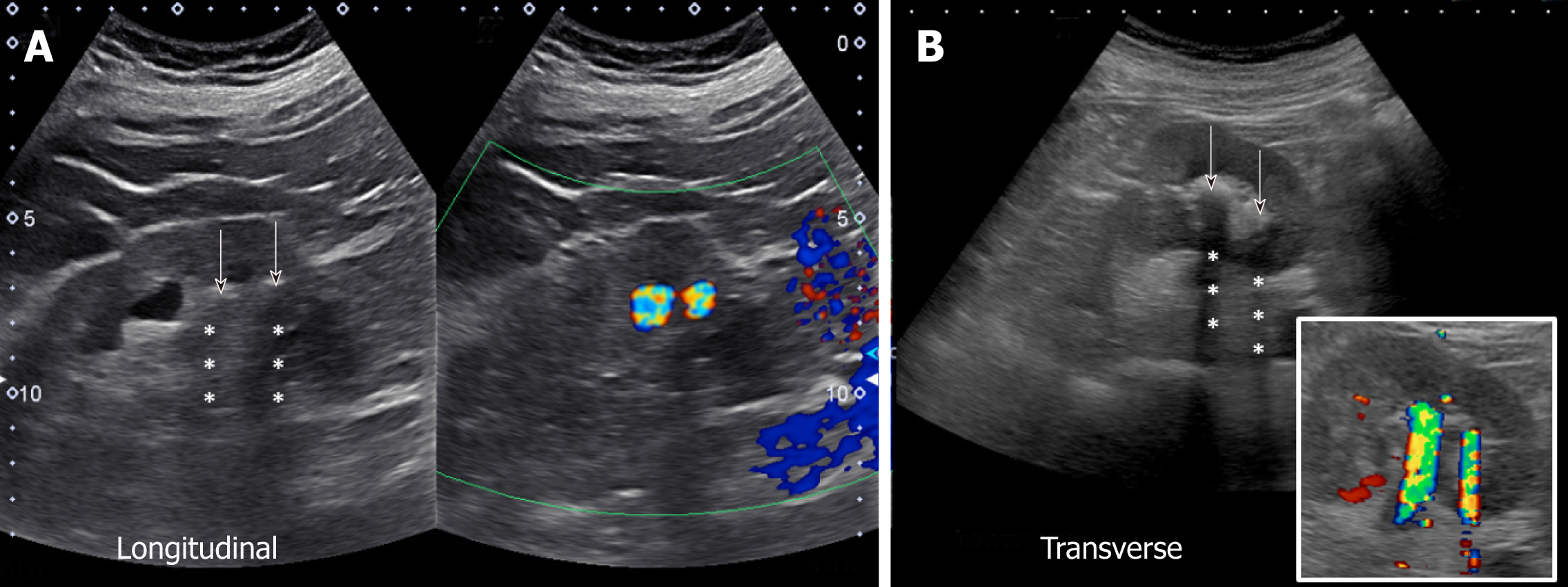
Figure 11 Longitudinal and transverse gray-scale renal ultrasound images demonstrating anechoic region in the mid-kidney suggestive of mild hydronephrosis in the top panel.
Doppler images demonstrating prominent arteriovenous flow suggestive of vascular malformation are shown in the bottom panel. Adapted from reference No. 29, first author’s previous work, published under CC BY-NC 4.0 license.
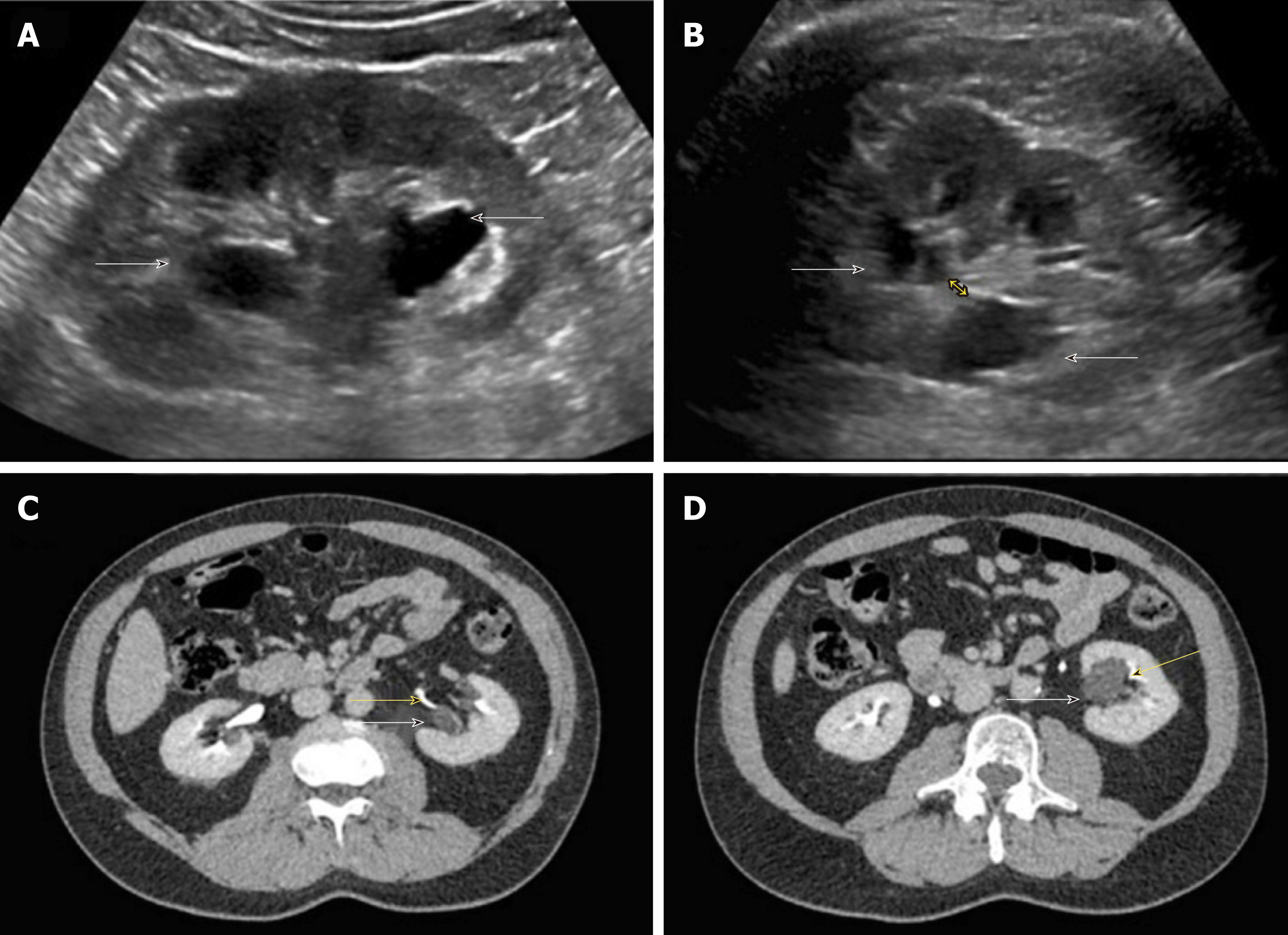
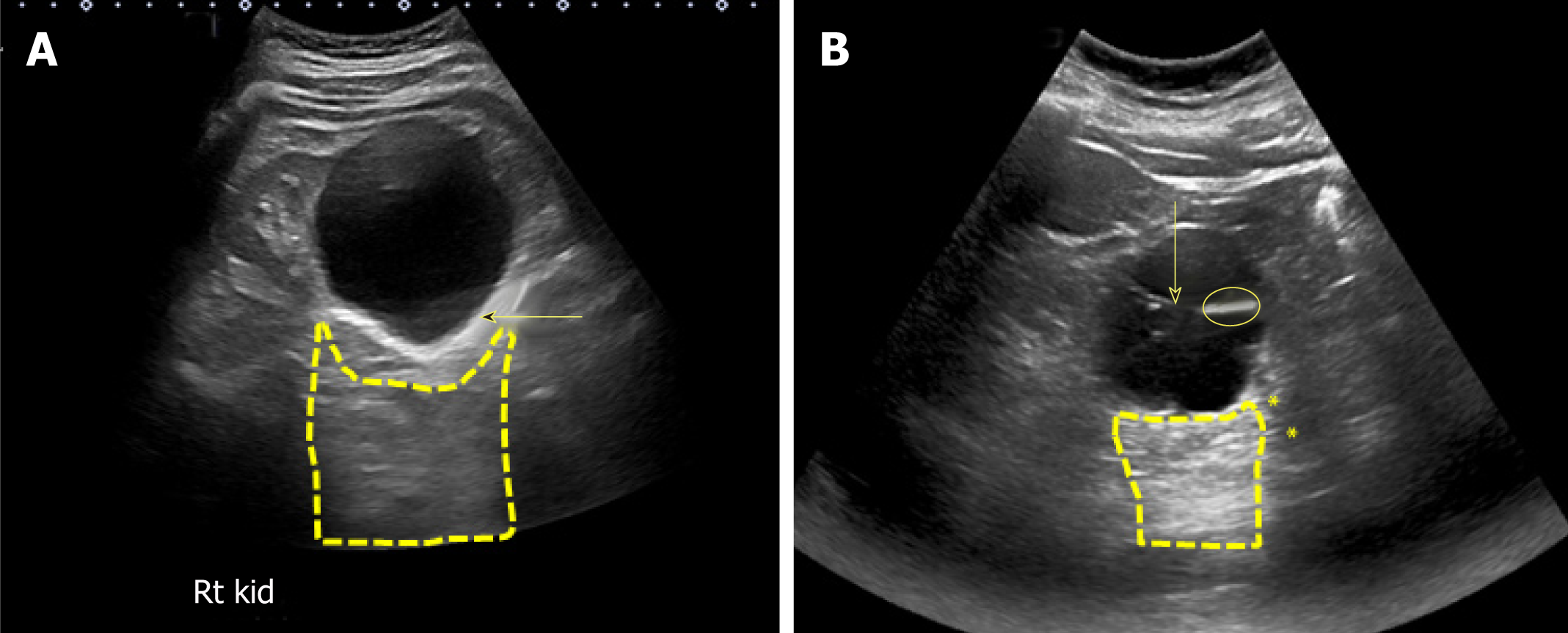
Figure 12 Renal sonogram.
A, B: Sagittal (A) and transverse (B) views of the left kidney showing hypoechoic areas in the pelvic area (arrows) suggestive of hydronephrosis; C, D: However, on the transverse view, these areas do not seem to be connected with one another (double‐headed arrow) and computed tomography (CT) scan with contrast demonstrating (C) and parapelvic cysts (arrows) that are separate from the contrast‐filled collecting system (yellow arrows) (D). Adapted from reference no. 30, first author’s previous work, published under CC BY-NC 4.0 license.
Figure 13 Urinary bladder ultrasound.
A: Enlarged prostate (arrow) compressing the urinary bladder; B: Heterogeneous solid mass (arrow) occupying almost the entire bladder; C: Normal appearance of a decompressed bladder with Foley catheter: The empty bladder with functioning catheter is difficult to visualize, and the hypoechoic/anechoic fluid-filled balloon (arrow) is the only portion visible; D: Distended bladder filled with urine despite the presence of Foley catheter indicating catheter malfunction.
Figure 14 Renal sonogram demonstrating grey-scale (A) and corresponding color Doppler (B) images of the kidney demonstrating acoustic shadowing and twinkling sign respectively, which is diagnostic of stones.
Arrows point to the hyperechoic stones and asterisks indicate shadowing.
Figure 15 Renal sonogram demonstrating a large simple cyst in the lower pole of the right kidney.
A: Arrow points to echogenic far wall and the contained area posterior to the cyst represents acoustic enhancement; B: Example of a complex cyst with septations (arrow). The image shows both acoustic enhancement from the cyst (contained area with yellow outline) and acoustic shadowing (asterisks) from calcifications in the septa (circle).
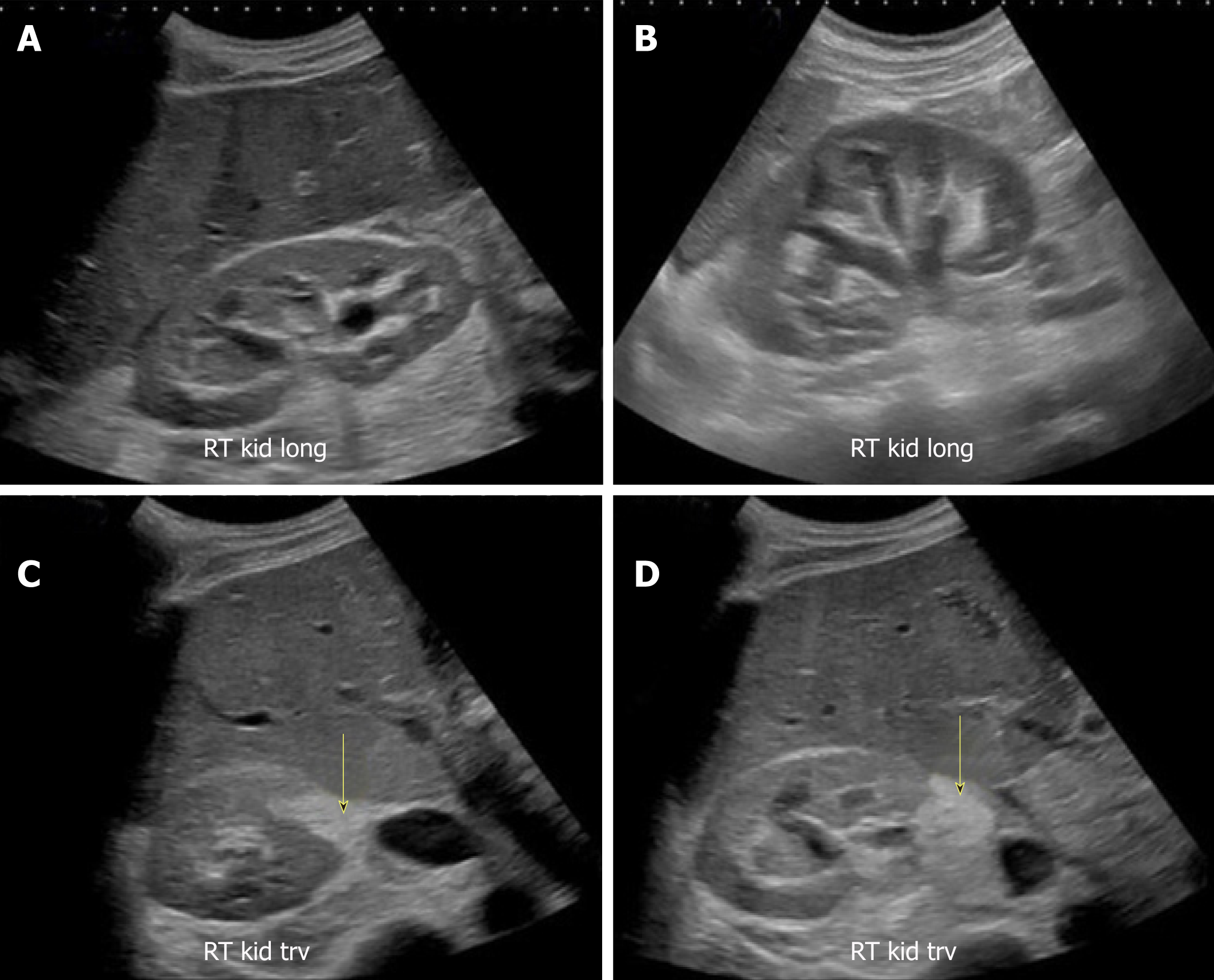
Figure 16 Renal sonogram images.
A, B: Bilateral moderate hydronephrosis and hydroureter; C, D: Transverse views of the right kidney showing echogenic debris (arrows) in the right collecting system in addition to fluid–fluid levels, suggestive of pyonephrosis. Adapted from reference No. 43, first author’s previous work, published under CC BY-NC 4.0 license.
- Citation: Koratala A, Bhattacharya D, Kazory A. Point of care renal ultrasonography for the busy nephrologist: A pictorial review. World J Nephrol 2019; 8(3): 44-58
- URL: https://www.wjgnet.com/2220-6124/full/v8/i3/44.htm
- DOI: https://dx.doi.org/10.5527/wjn.v8.i3.44