Copyright
©The Author(s) 2016.
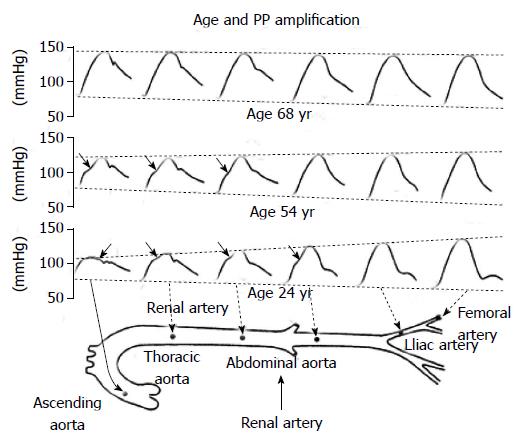
Figure 1 Representative pulse waveforms along the aorta in young, middle-aged and elderly persons.
In younger subjects (age: 24 yr), the rate of propagation is relatively low in arterial vessels, which become progressively narrower and less distensible. Because of the summation of the forward and the backward wave at each point of the arterial tree, peak systolic blood pressure increases markedly from central to peripheral arteries, while end-diastolic blood pressure tends to be reduced and mean arterial pressureremains unchanged. In older subjects (age: 68 yr), because of the more rapid propagation of pressure wave with resulting changes in wave reflections, the amplification of PP disappears, making that central and peripheral BP become identical. At 54 yr of age, the situation is intermediate between younger and older subjects[2].
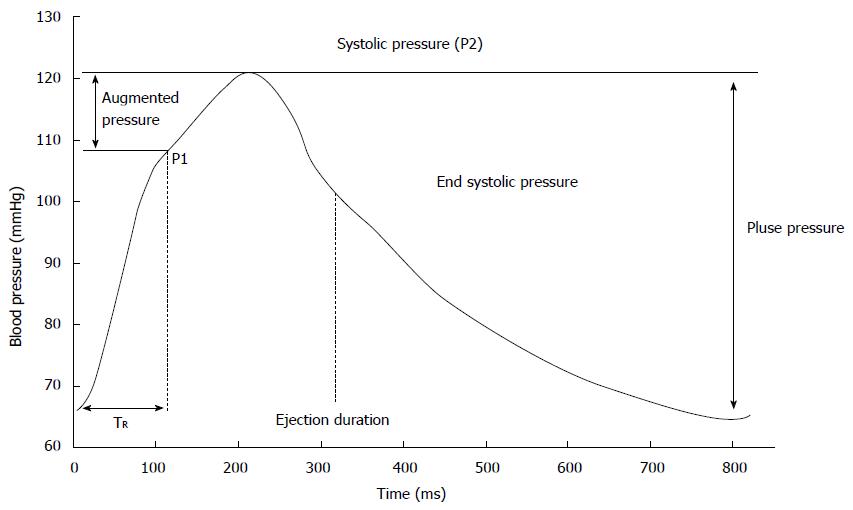
Figure 2 Example central pressure waveform.
TR indicates timing of the reflected pressure wave; P1 and P2 represent the first and second systolic peaks, respectively[3]. Augmentation index is defined as augmented pressure/forwarding pulse pressure (P1).
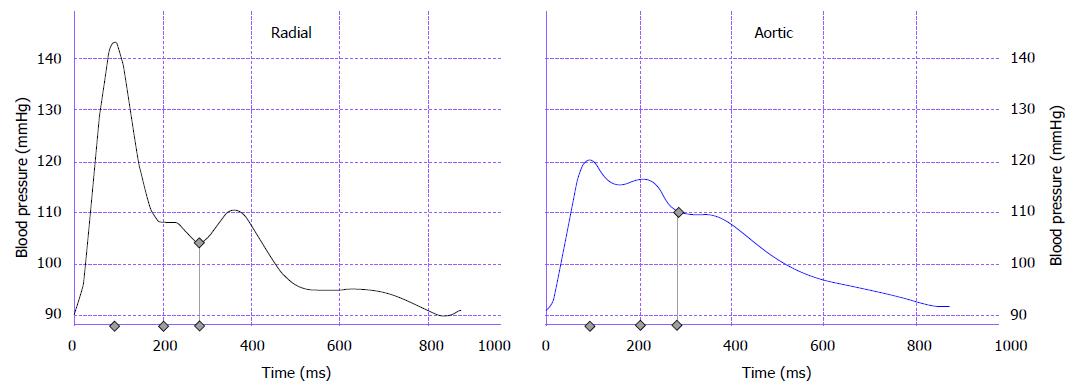
Figure 3 Estimation of central pulse waveform.
Radial tonometry detects radial pulse waveform with high systolic blood pressure over 140 mmHg (left panel). Using this radial waveform, generalized transfer function calculates aortic pulse waveform (right panel). Please note that aortic systolic blood pressure is 120 mmHg (Available from: URL: http://hogimed.fr/?q=sphyg%20p1).
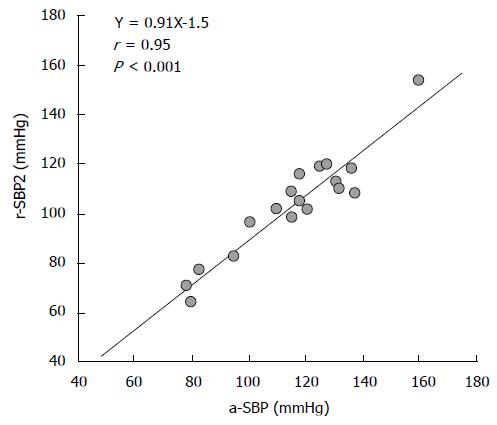
Figure 4 Relationship between radial second peak of systolic blood pressure and aortic systolic blood pressure.
There is a strong positive relation between two[10]. r-SBP2: Radial second peak of systolic blood pressure; a-SBP: Aortic systolic blood pressure.
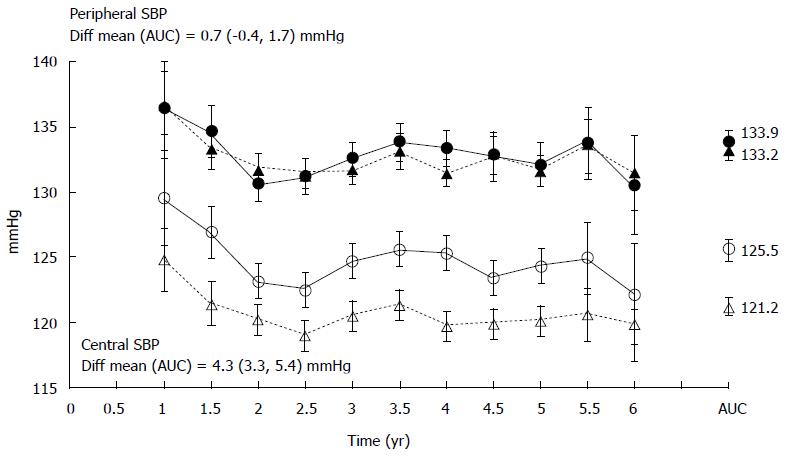
Figure 5 Principal results of ASCOT-CAFÉ study.
Brachial blood pressure was similar between the patients treated with beta-blocker-based medication (close circles) and calcium channel blocker-based treatment (closed triangles). However, central blood pressure was higher in the former (open circles) than the latter group (open triangles)[11]. SBP: Systolic blood pressure.
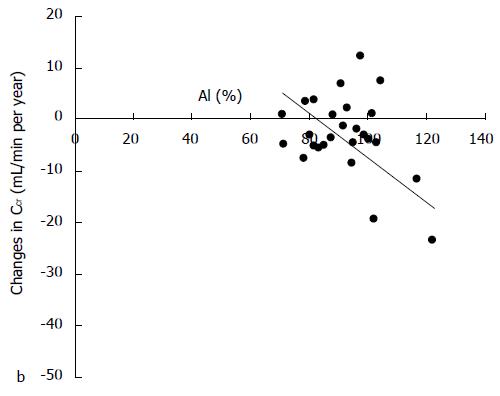
Figure 6 Relationship between annual changes in creatinine clearance and augmentation index.
There is an inverse relation between two[5].
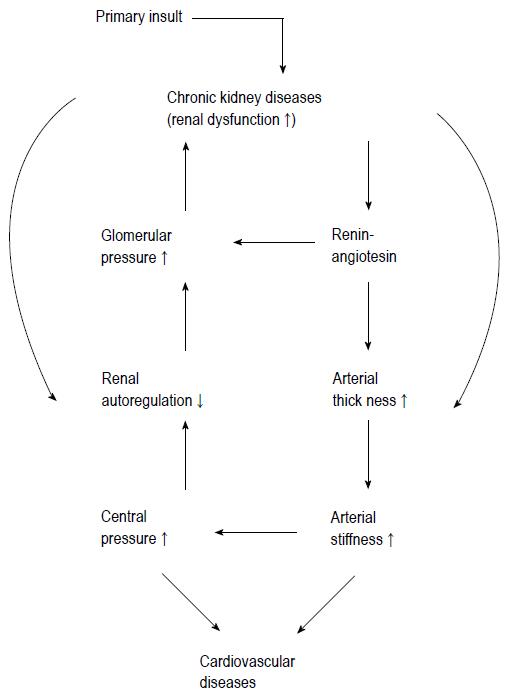
Figure 7 Working hypothesis underlying cardiovascular disease and chronic kidney disease.
Lowering central blood pressure could cut vicious cycle between CVD and CKD[29]. CKD: Chronic kidney disease; CVD: Cardiovascular disease.
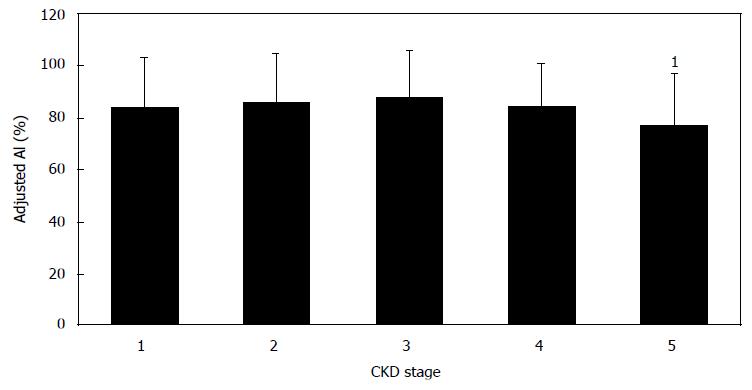
Figure 8 Comparison of augmentation index among all chronic kidney disease stages.
AI was adjusted with confounding factors including age, blood pressure, pulse rate, and vasodilator antihypertensive drugs. 1Indicated significant difference from stage 1[37]. CKD: Chronic kidney disease.
Figure 9 Disparate effects of antihypertensive drugs on central blood pressure.
Differences between brachial systolic blood pressure and central systolic blood pressure (ΔSBP2) were compared between vasodilator (VD) and non-vasosilator (non-VD) antihypertensive medications. ΔSBP2 was adjusted by age, gender, height, BMI, diastolic blood pressure and use of nitrate. The comparison between actual VD and non-VD only regimen was shown in left panel (A). Right panel (B) depicted comparisons among VD(est), non-VD(est) and Mixed combination of VD and non-VD. “(est)” indicated including data derived from mixed combination, for which the effects of VD and non-VD alone on ΔSBP2 were estimated. Non-hypertensive population (non-HT) was used as physiological reference for ΔSBP2. VD antihypertensive drugs included angiotensin receptor blocker, calcium channel blocker, converting enzyme inhibitor and alpha-blocker. Non-VD group includes beta-blocker and diuretics. Mann-Whitney U test was used to compare the means, unless otherwise specified. K-W and G-H described Kruskal-Wallis and Games-Howell multiple comparison test[40].
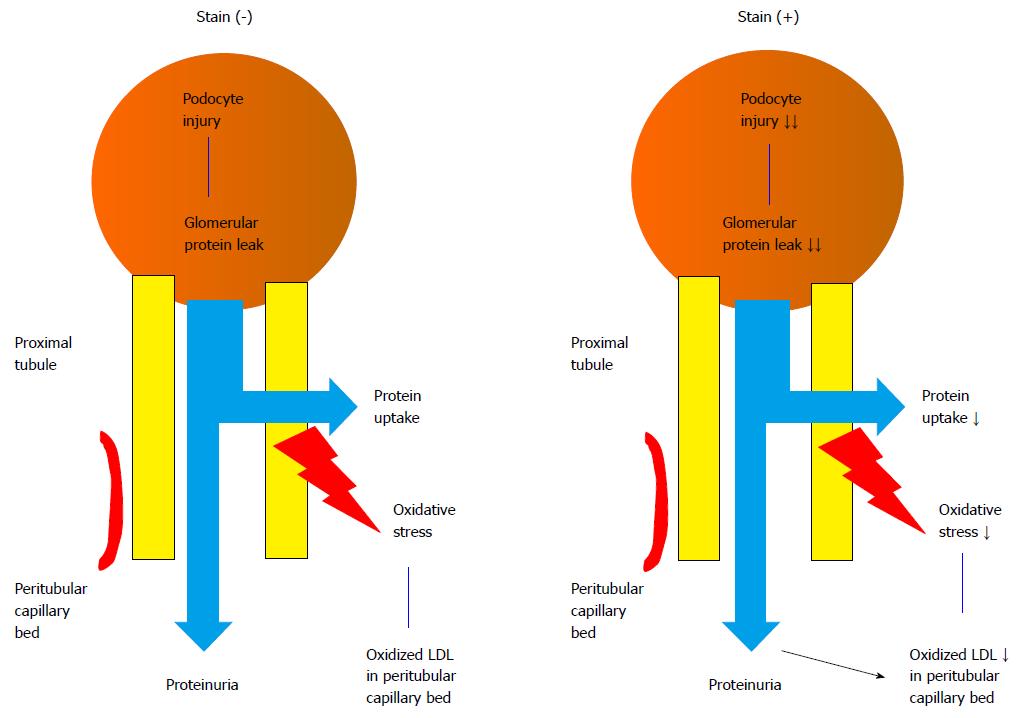
Figure 10 Multiple actions of statin on chronic kidney diseases: Statin decreases proximal tubular uptake of protein leaked from glomeruli, reducing oxidative stress.
Statin also improve podocyte injury, reducing glomerular protein leak[27]. LDL: Low-density lipoprotein.
- Citation: Ohno Y, Kanno Y, Takenaka T. Central blood pressure and chronic kidney disease. World J Nephrol 2016; 5(1): 90-100
- URL: https://www.wjgnet.com/2220-6124/full/v5/i1/90.htm
- DOI: https://dx.doi.org/10.5527/wjn.v5.i1.90